The aim of the present investigation was to evaluate the efficacy of an
antibacterial coating of implant-abutment prosthetic junctions by real time
measurement of Volatile Organic Compounds (VOCs). A total of 20 patients and 40
internal prosthetic junction implants were evaluated in the present
investigation: 20 fixtures with antibacterial internal coating (Test) and 20
without treatment (Control). The VOCs measurements were evaluated at the baseline
(T
Although implant rehabilitation represents a highly successful treatment, it is not free from complications that can undermine its long-term success. Among these, the loss of crestal bone surrounding an implant not only affects implant stability but also the aesthetic outcome, because it influences the shape and contour of the overlying soft tissue [1]. The healthy peri-implant soft tissues are characterized by connective tissue core with a keratinized epithelium surface. The endosseous portion of the implant produce a contact interface with mineralized bone tissues, while subsequently with bone marrow, vascular component and fibrous tissue [2].
Peri-implantitis is the most common cause of peri-implant bone loss, affecting 9.25% of implants and 19.83% of subjects [3].
Peri-implantitis is “an inflammatory process in peri-implant soft and hard tissues, that causes a clinically progressive crestal bone loss, after the adaptive phase following prosthetic loading” [4, 5, 6, 7].
It develops with a pathogenetic mechanism similar to periodontitis, even though peri-implantitis sites often have larger inflammatory lesions than periodontitis sites [8].
Moreover, the oral flora differs in completely edentulous patients; specifically it showed a toning of bacteria microbiota to aerobic species of the salivary microbiome [9].
The perimplantitis is supported by gram-negative anaerobic periopathogens including Porphyromonas gingivalis and Tannerella forsythia, opportunistic pathogens such as Pseudomonas aeruginosa and Staphylococcus aureus, fungal organisms and viruses [8, 10, 11].
The implant-abutment connection (IAC) is one of the causal factors of peri-implant tissues.
Two-piece implants are composed of two components: the fixture (intraosseous component with an internal hollow portion) and the abutment (or a healing screw). Even after connection and screw tightening, a microgap remains at the IAC, favouring bacterial leakage and acting as a bacterial reservoir, where toxins and products of bacterial metabolism cause inflammation of the peri-implant tissues, osteoclastic activation and bone resorption [1].
The bacterial contamination of IAC can occur not only when the implant abutment is disconnected (for impressions or prosthetic phases) but it is powered by the chewing load that causes micro-oscillations of the abutment [12]. The spatial relationship between gap and bone level can affect the extent of inflammation and bone resorption. Broggini et al. [13] demonstrated that peri-implant neutrophil infiltration increased progressively as the IAC depth increased, i.e., subcrestal IAC promoted a significantly greater density of neutrophils than did supracrestal IAC. Animal experimental studies found that bone loss decreased when the microgap moved coronally, while if the gap was moved in an apical direction, closer to bone level, a greater amount of bone loss was observed [14, 15, 16]. Multifactorial conditions influence bacterial leakage, such as the torque forces used to connect the components, the loading forces during masticatory function and, moreover, the type of connection and the precision fit between fixture, abutment and clamping screw [12].
The penetration and proliferation of bacteria in the IAC (or implant-healing screw connection) is confirmed in clinical practice by the common finding of malodour, when healing screw or abutment are removed. This is the result of the release of volatile sulphide compounds, produced by bacterial metabolism [17].
Knowing the importance of IAC and its influence on peri-implant tissue health, research has been focused on improving the connections in order to reduce the gap and the bacterium leakage. A recent technology provides for the lining of the IAC surface with an antibacterial coating [17].
The VOCs are small molecular mass substances (
Among VOCs produced by oral bacteria, responsible of halitosis and related with oral infections, should be mentioned: methanethiol, also known as methyl mercaptan, produced by enzymatic degradation of L-methionine, acetone, isoprene, sulphur containing compounds like dimethyl sulphide and hydrogen sulphide [19].
This study aims to evaluate the efficacy of antibacterial coating in reducing bacterial proliferation, by using real time Volatile Organic Compounds (VOCs) analysis. The null hypothesis stated that test and control implants showed the same effectiveness in terms of VOCs evidences.
In the study 20 patients (9 males and 11 females, age ranging from 29 to 74
years, mean age 41
The clinical protocol was performed according to the Declaration of Helsinki and the Good Clinical Practice Guidelines. The study protocol received the approval of the Inter-institutional Ethics Committee of Faculdade Ingá, UNINGÁ, PR, BRAZIL, No. 153455/2018; CAEE 04609518.6.0000.5220. The subjects were treated at the Oral Implantology Unit of the University of UNINGÁ, PR, BRAZIL. The inclusion criteria were healthy subject with no periodontal disease but requiring implant rehabilitation in at least two single sites. To evaluate the tissue health, the following clinical parameters were detected: presence or absence of bleeding on probing (BOP) probing depth (PD) in millimeters (mm), and plaque index (PI). When the site exhibited a PI equal to 1, a PD of 3 or fewer mm and absence of BOP, it was considered clinically healthy. The exclusion criteria were serious systemic diseases (gastrointestinal disorders, diabetes mellitus, respiratory dysfunction, neoplasia, various carcinomas, treatment with chemotherapy drug etc.), smoking more than 5 cigarettes a day, lactating or pregnancy, history of non-steroidal anti-inflammatory or antibiotics drugs in the previous four months. Also, patients who needed bone regeneration procedures, who had less than 18 teeth, orthodontic appliances or untreated teeth and caries, and a fissured tongue were excluded. Pre-operative radiograph evaluation was carried out with Cone Beam Tomography (CT) scans to quantify bone height and thickness together with a clinical inspection. The investigational devices were tapered titanium screw-shaped implants with sand-blasted acid-etched surfaces with internal prosthetic connections (Edierre srl, Genova, Italy). A total of 40 implants with internal connection and four cams as anti-rotation system were placed in this study, 20 with antibacterial internal coating (PIXIT) (Test Group) and 20 without PIXIT treatment (Control Group) (Edierre srl, Genova, Italy). The implant diameter was 4 mm, while the length of the implant was chosen by the dentist according to the bone dimension limits with no difference of the internal implant chamber dimension between the screws.
The antibacterial internal coating of the implant chamber was provided by a PIXIT (Edierre Implant System, Genova, Italy) is a solution containing chlorhexidine gluconate at 1% and an alcoholic solution of polysiloxane oligomers that bind the titanium through a protocol as described in a previously study [20]. The particular structure of PXT, containing both hydroxyl functionalities and branched alkyl chains, allows to simultaneously bind the titanium surface and the antimicrobial active chlorhexidine. The product is fixed to the surface through covalent bonds between the superficial OH groups and those present on the siloxane units and at the same time the branched alkyl chains containing carbon and hydrogen trap the Chlorhexidine through Van der Waals interactions. The PXT implant surface treatment has been proposed as antimicrobial coating for dental implant in contrast to the bacterial proliferation and biofilm adhesion (Patent: PCT/IT2015/000142) [21].
The subjects received preventative antibiotic therapy: 2 g of amoxicillin (or
clindamycin 600 mg if allergic to penicillin) an hour and a half before implant
surgery and were instructed to use a mouth rinse with chlorhexidine 0.2%
(Curasept, Saronno Italy) for 2 minutes. The perioral and facial skin was
decontaminated with chlorhexidine 0.2% solution (Curasept, Saronno Italy). All
patients were treated under local anesthesia by means of 2% articaine with 1:100.000 epinephrine (Pierrel S.p.A, Milan, Italy). The implant bed was prepared
with drills having an increasing diameter, as recommended by the implant
manufacturer. The fixtures were placed 1 mm under the alveolar bone level the
internal implant hole was sealed with a cover screw with no treatment in each
group. Three/four months later the implants were exposed, and the cover screw was
replaced with healing abutments (Fig. 1) and internal chamber was washed with 1
mL saline solution at all VOCs measurement time points (Fig. 2), and dried with
absorbent paper points n
 Fig. 1.
Fig. 1.Internal chamber of the implant of untreated (front) and treated (read) with PIXIT.
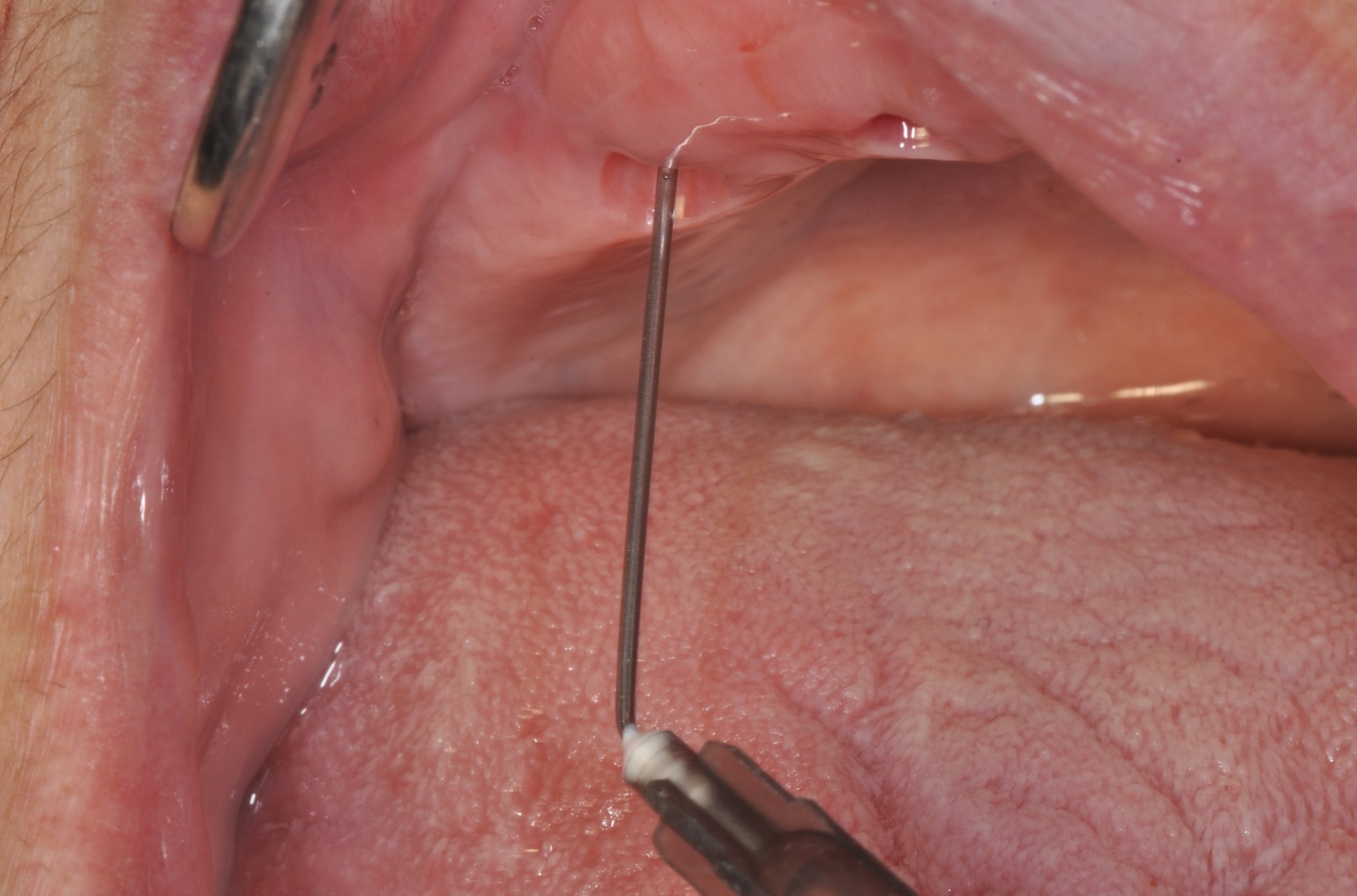 Fig. 2.
Fig. 2.During wash of internal champer with saline solution.
 Fig. 3.
Fig. 3.
During the drying of the internal chamber with
absorbent paper points n
The real-time Volatile Organic Compounds measurements were conducted between
9:00 AM and 12:00 AM in the same position of the operative room in standardized
temperature condition (21
 Fig. 4.
Fig. 4.Graphical representation of the Real Time VOCs measurement. (A) Built-in sensor device and pump. (B) Detail of the calibration of the VOCs measurement computational unit used for the present investigation. (C) Clinical application of the device. (D) Detail of the VOCs measurements at the level of the implant site.
The sample size was evaluated by the analytical software (G Power,
Heinrich-Heine-Universität Düsseldorf, Germany). The optimal sample size
for a statistical significance of the study variable was 20 implants for each
group (effect size: 0.82,
The normality distribution of the study data was evaluated by the
Kolmogorov-Smirnov test and the mean study variables of test and control groups
evaluated by the one way- ANOVA followed by the Tukey’s post-hoc test. The level
of significance was set for p
The use of real time recording of VOCs in the present study has the aim of
evaluating the efficacy or antibacterial activity of PIXIT. The parameter
analyzed was VOCs max peak amplitude in implants coated with
PIXIT (Test) and uncoated implant (Control) at the baseline (T
| VOCs | T |
T |
T | |
| MAX PEAK | (baseline) | (7 days) | (14 days) | |
| Test | Mean (SD) | 2.15 |
2.26 |
2.29 |
| 95% CI | (1.81–2.49) | (1.89–2.62) | (1.94–2.62) | |
| Interquartile range | (1.47–2.84) | (1.52–2.98) | (1.58–3.01) | |
| Control | Mean (SD) | 2.21 |
3.15 |
3.65 |
| 95% CI | (1.88–2.54) | (2.74–3.56) | (3.21–4.08) | |
| Interquartile range | (1.54–2.7) | (2.5–3.6) | (2.76–4.54) | |
| p value | p |
p |
p | |
 Fig. 5.
Fig. 5.Chart of the VOCs max peak comparison between Test and Control
group at T
The scope of the present investigation was to evaluate the early VOC emissions correlated to the early dental implants transmucosal second stage. The uncovering of submerged dental implant represents a critical phase where the fixture is exposed to the oral cavity after the osseointegration healing period [22, 23, 24]. During this phase, the peri implant hard and soft tissues are not already functionalized that could influence the local response, with a lower percentage of lamellar bone at the interface bone-implant interface [22, 25]. In this way the implant uncovering and the positioning of the healing abutment could represent a potential medium for the biofilm adhesion and bacteria aggregation [26, 27]. In fact, several studies reported that the higher dental implants marginal bone loss occurs during the first year at early [28, 29, 30], in particular after the screw positioning and implant uncovering [23, 24].
The outcome of the present study demonstrates a statistically significant reduction of VOC emission in the implant coated with PIXIT and the null hypothesis has been rejected. As demonstrated in a previous study, the high emission of VOC from the internal chamber is correlated with a high microbiological colonization. In fact, the VOC device is also able to detect the fermentation sub-products and could be used for the oral and digestive tract measurements through a built-in real time sensor [31, 32]. This cost effective method has been proposed as a breath-borne biomarker for the diagnosis of several different pathologies such as gastric diseases, nutritional disorders, lung neoplasms, colon and gastric cancer [31, 32]. In the present study the authors aimed to evaluate a representative pooling samples of the patients elected for dental implant positioning affected by partial or total edentulism. If applicable, also the periodontal status was considered as a inclusion criteria in order to avoid any possible bias for VOC measurements induced by concomitant local infections.
Moreover, to avoid the interference of antibacterial agents on VOC emission, the patients were told to avoid the use of antibacterials (mouthwash and antibiotics) between placement of the healing screw and final record of VOC.
The studies concerning the internal chamber of the implant found Prevotella intermedia, Porphyromonas gingivalis, and Aggregatibacter actinomycetemcomitans that are also present in peri-implant disease [33, 34, 35, 36]. Scarano et al. [37] reported in a histological study on retrieved implants that screw-retained abutments are correlated to a microgap of 40–60-micron that could represent a critical factor for the bacteria colonization. Multiple in vitro and in vivo studies have demonstrated the presence of bacteria in the abutment-implant gap of all screw-retained connection types, while there is a trend for implants with internal conical connections which exhibit reduced risk of bacterial penetration [1]. Cemented retained implants seem to be hermetic to bacterial infiltration because the gap is filled by cement, but it must be considered that its incomplete removal can negatively affect the peri-implant soft tissues [12, 38].
The gap between implant and abutment probably exists also between implant and healing screw and the inflammatory process begins with the positioning of the healing screw [39].
Very few studies in literature investigated if healing screws are able to provide a complete seal on the implant: in a previous study we demonstrated the presence of activated osteoclasts around unloaded implants with healing screws [40, 41]. In another study we demonstrated, via VOCs emission test, that the microgap existing between implant and healing screw could promote bacterial penetration, underling the importance of evaluating the precision between implant and healing screws [39]. In the last years, the analysis of VOCs released from the human body emerged as a new method of disease diagnosis because some compounds exhibited robust correlations with health or pathological conditions [42]. It is used for screening procedures to diagnose and observe the diseases of the lung [43, 44]. Several recent studies have analysed the correlation between the VOCs in exhaled breath and different forms of lung cancer: abnormal metabolic processes related to pathological types of cancer tissue processes [31, 45].
Preventing microbial leakage in IAC could be useful for long term success of dental implant rehabilitation, reducing peri-implantitis occurrence. Biphasic dental implants are composed of two components: the fixture placed in the bone and the abutment, that supports the prosthetic structure. Even though this study tried to optimize the sealing among implant and abutment, a microgap persists and can promote bacterial leakage, moreover during prosthetic rehabilitation and when healing screw and abutment are removed [46]. Once colonized the bacterial present in the inner portion of the fixture, may represent a bacterial reservoir with the possibility to contaminate implant surroundings and undermine periimplant tissues health [47, 48]. Others common risk factors of peri-implantitis are characterized by periodontal disease accompanied by high plaque/bleeding score, smoke, diabetes, obesity, poor maintenance, fixture malposition and wrong prosthetic rehabilitations, excesses of cement [8].
The close proximity of IAC and microgap to crestal bone causes inflammation and bone resorption, therefore the passage of pathogenic bacteria in the adjacent peri-implant tissues may cause peri-implantitis with an immuno-mediated mechanism similar to periodontitis.
Covering IAC surfaces with antimicrobial coatings, to hinder bacterial proliferation in the internal chamber of the fixture, could reduce inflammation of peri-implant tissues and bone loss [13, 49, 50, 51]. So all kinds of implant abutment connections have a microleakage and bacteria represent a danger for the health of soft and hard tissues around the implant, especially in external connections [52], while conical connections showed low gap and leakage at the IAC interface with reduceding bacterial colonization, thus this connection does not warrant a total seal of the interface [53, 54]. The Pixit implant, tested in this study, has the internal chamber of the fixture coated with a polysiloxane-titanate oligomer that binds a titanium surface via OH groups, and chlorhexidine molecules through Van Der Waals interactions.
In literature, several methods have been used to measure microleakage: scanning electron microscopy microgap analysis [55, 56]; fluid microleakage testing [38]; microbial leakage analysis [37]; micro-ct leakage analysis [57]; dynamic loading fluid leakage [58]. All these methods present important limitations in clinical use, besides the fact that they are time consuming and expensive. For these reasons, in this study we evaluated the efficacy of antibacterial coating in reducing bacterial proliferation in IAC, by using real time Volatile Organic Compounds (VOCs) analysis, an approach that is quick and clinically applicable. The limit of the present investigation is determined by a indirect quantification of the Volatile Organic Compounds without a qualitative bacteria evaluation and semiquantitative quantification. In operative dentistry, the VOCs measurement device could be take advantage from the wide bioaerosols produced during the clinical procedures that could produce a decrease of the indoor air quality and provoke infections to the patients and the dental workers [59].
Several studies demonstrated that profiling of VOCs in exhaled breath can help in identifying pathologies like respiratory diseases, oral infection, i.e., periodontitis and candidiasis [60], oxidative stress and aging processes [61] and neurodegenerative diseases [31]. Recently VOCs emission was used for a screening that might contribute to the decision to test suspected cases or guide quarantine instructions in subjects with Covid-19 disease [62, 63].
VOCs are also responsible of foul smells at the opening of abutment or healing screw, often found in clinical practice. Sterer et al. [17] demonstrated an association between transmucosal depth and malodour, measuring volatile sulphide compounds levels with a sulphide monitor (Halimeter). A significant increase in severity of malodour parameters was observed with the increase in transmucosal depth.
If antibacterial coating is able to reduce the bacterial population within the implant-abutment interface, a reduction of malodour production and VOCs can be expected.
As demonstrated in a previous study by Carinci et al. [64], the results of the present investigation are in agreement with the capacity of the the bacterial proliferation control of the PIXIT implant internal chamber of in vivo at 6 months, via amplification of a targeted bacterial DNA with PCR analysis.
The chlorhexidine digluconate is an effective antiseptics due to a wide broad-spectrum antibacterial property and residual capacity to remain in the oral cavity [65]. Moreover, it was demonstrated that locally the chlorhexidine application is able to reduce the breath odour and sulphides and organoleptic volatile compounds [65]. The total amount of bacteria was significantly lower in treated implants. Moreover, the coating influenced the quality of microbiota, because a lower quantity of bacteria was also obtained when the amount of Corinebacterium rectus and Fusobacterium nucleatum was investigated, bacterial species of the cluster related to peri-implantitis.
Lauritano et al. [66] demonstrated, via microbiological tests, that after immersion in a medium infected by genetic modified Tannerella forsythia (TF) and Porphyromonas Gingivalis (PG), living bacteria were not found either in the internal part of the treated implants nor in the external culture medium, while for untreated implants the internal part was on average 90% lower than that detected in the external culture medium.
Also, PCR analysis on coated vs uncoated implants indicated a remarkable decrease of the bacterial count both in the internal part and in the external medium. The bacterial reduction also in the external culture medium can be justified by the release of chlorhexidine [66].
In conclusion, the antibacterial internal coating of the implant prosthetic junction chamber is effective to decrease the microbial VOCs activity and resist the bacterial penetration. The PXT surface treatment should be considered as an effective tool for a long-term maintenance of the health of peri-implant tissues.
AS, PS, FL designed the research study. AS, FL PS, LL, FC, FF performed the research. AS, FF, FC, FL, LL analyzed the data. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
The study protocol was conducted in accordance to the revised Declaration of Helsinki and received the approval of the Inter-institutional Ethics Committee of Faculdade Ingá, UNINGÁ, PR, BRAZIL, No. 153455/2018; CAEE 04609518.6.0000.5220. The subjects involved submitted the informed consent to participate to the present investigation.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
