Background: The prognostic value of coronary artery calcium (CAC)
combined with risk factor burdens in middle-aged and elderly patients with
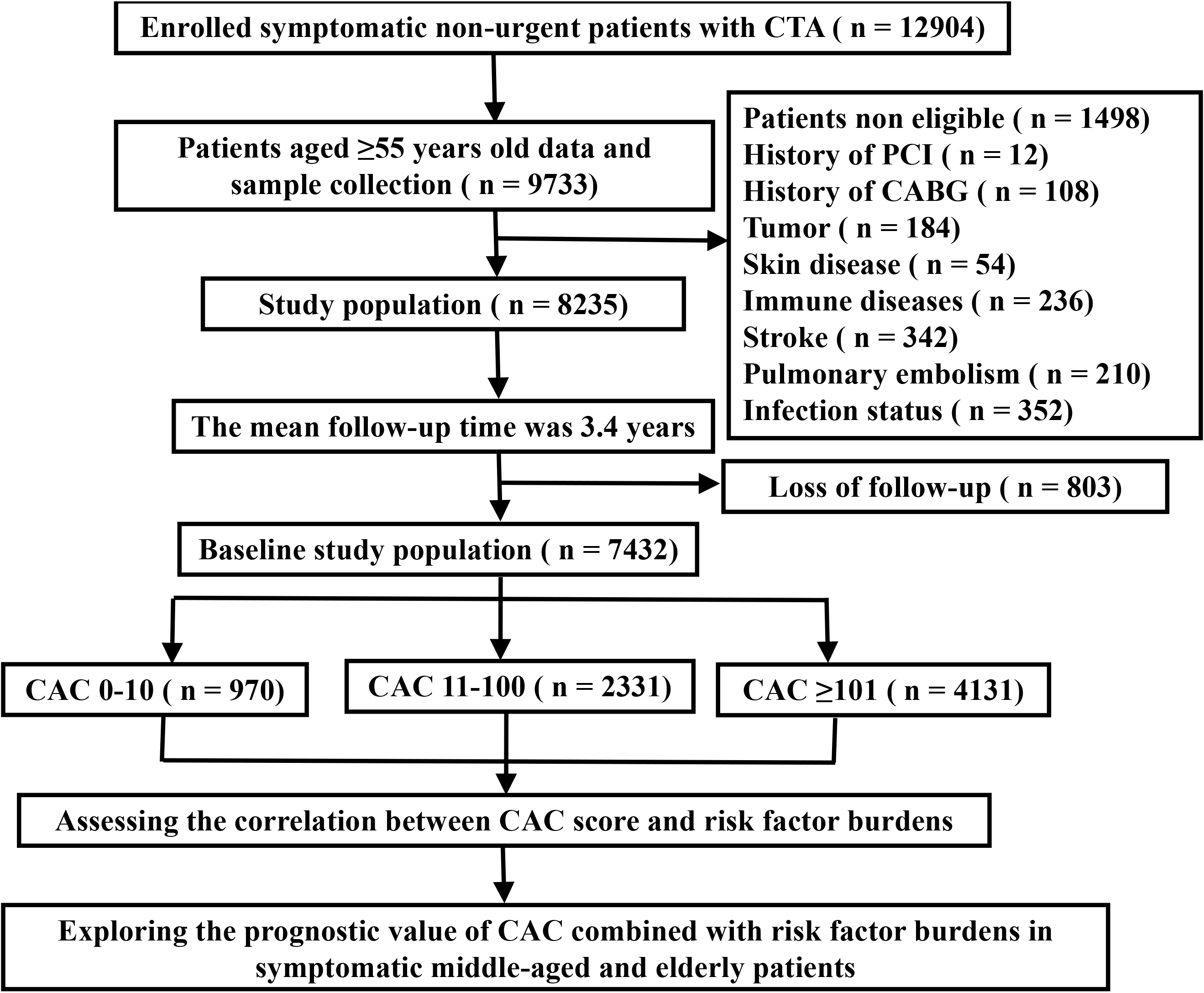
symptoms is unclear. Methods: A cohort study comprising 7432 middle-aged
and elderly symptomatic patients (aged above 55 years) was conducted between
December 2013 and September 2020. All patients had undergone coronary computed
tomography angiography, and the Agatston score were used to measure CAC scores.
The primary outcome was major adverse cardiac and cerebrovascular events (MACCE),
which was defined as a composite outcome of nonfatal myocardial infarction,
revascularization (percutaneous coronary intervention or coronary artery bypass
graft), stroke, and cardiovascular death. Congestive heart failure, cardiogenic
shock, malignant arrhythmia, and all-cause mortality were defined as the
secondary outcomes. Results: There are 970 (13%) patients with CAC
0–10, 2331 (31%) patients with CAC 11–100, and 4131 (56%) patients with CAC
101. The proportion of patients aged 55–65 years, 65–75 years and
75 years was 40.7%, 38.1% and 21.2%, respectively. The total number of
MACCEs over the 3.4 years follow-up period was 478. The percentage of CAC
101 was higher among the 75-year-old group than the 55–65-year-old
group, increasing from 46.5% to 68.2%. With the increase in the CAC score, the
proportion of patients aged 75 years increased from 12.9% to 25.8%,
compared to those aged 55–65 years. The number of risk factors gradually
increased as the CAC scores increased in the symptomatic patients aged over 55
years and the similar tendencies were observed among the different age subgroups.
The proportion of non-obstructive coronary artery disease (CAD) was comparable between the three age groups
(53.5% vs 51.9% vs 49.1%), but obstruction CAD increased
with age. The incidence of MACCE in the group with CAC 101 and 4
risk factors was 1.71 times higher (95% confidence interval (CI) 1.01–2.92;
p = 0.044) than the rate in the group with CAC 101 and 1 risk
factor. In the CAC 0–10 group, the incidence of MACCE in patients aged 75
years was 12.65 times higher (95% CI: 6.74–23.75; p 0.0001) than
that in patients aged 55–65 years. By taking into account the combination of CAC
score, age, and risk factor burden, the predictive power of MACCE can be
increased (area under the curve (AUC) = 0.614). Conclusions: In symptomatic patients aged 55 or above, a rise in age, CAC scores, and risk factor burden was linked to a considerable
risk of future MACCE. In addition, combining CAC scores, age and risk factors can
more accurately predict outcomes for middle-aged and elderly patients with
symptoms.