1 Department of Geriatrics, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, 200025 Shanghai, China
2 Department of Endocrine and Metabolic Diseases, Shanghai Institute of Endocrine and Metabolic Diseases, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, 200025 Shanghai, China
3 Department of Biomedical Sciences, Faculty of Medicine, Health and Human Sciences, Macquarie University, 2109 Sydney, Australia
4 Department of Cardiovascular Medicine, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, 200025 Shanghai, China
†These authors contributed equally.
Abstract
Background: Carotid-femoral pulse wave velocity (cfPWV) and ejection duration (ED) have different impacts on target organ damage (TOD). The aim of this study was to determine the relationship of cfPWV and ED with TOD. Methods: A total of 1254 patients (64.27% males) from Ruijin Hospital were enrolled in this study from December 2018 to August 2022. Medical records, blood samples and urine samples were collected. The cfPWV was measured and ED was generated using SphygmoCor software (version 8.0, AtCor Medical, Sydney, Australia). TOD including left ventricular hypertrophy (LVH), microalbuminuria, chronic kidney disease (CKD), and abnormality of carotid intima-media thickness (CIMT) were evaluated. Results: Multiple stepwise linear regression models of cfPWV and ED (individually or together) showed that cfPWV was positively correlated with left ventricular mass index (LVMI) (
Keywords
- carotid-femoral pulse wave velocity
- ejection duration
- target organ damage
- renal damage
- left ventricular hypertrophy
Carotid-femoral pulse wave velocity (cfPWV) is a gold standard measure of arterial stiffness. cfPWV is associated with target organ damage (TOD) such as left ventricular hypertrophy (LVH), chronic kidney disease (CKD), microalbuminuria, abnormality in carotid intima-medium thickness (CIMT), as well as cardiovascular events [1, 2, 3].
Ejection duration (ED) is defined as the time interval from opening to closure of the aortic valve [4], and is closely related to cardiac physiology and function [5]. The methods used to measure ED have changed over the years [6, 7, 8]. The main factor that shortens left ventricular ejection time (LVET) is the relative lengthening of the pre-ejection period (PEP), thereby delaying the onset of ejection. Further shortening of the LVET is associated with a decrease in stroke volume [4]. ED is associated with impairment of cardiac function and is a strong predictor of cardiovascular outcomes in certain patients, including those with hypertension [9], heart failure [10, 11], or other ischemic cardiac diseases [12, 13]. It has also been shown that ED is an independent predictor of incident heart failure [14]. When the arterial elastic modulus is constant, LVET has a dominant effect on the calculated PWV compared to the heart rate (HR) and to peripheral resistance [15]. Moreover, LVET but not HR is independently correlated with aortic PWV [16]. However, clinical applications of ED measurement in the general population that is free of cardiac diseases remains unclear, and the interaction of ED and/or cfPWV with TOD and cardiovascular events requires further investigation.
Therefore, in the present study we analyzed the associations of cfPWV and/or ED with TOD. This allowed exploration of the interaction between arterial stiffness and LVET, with the long-term goal of achieving individualized clinical management of ED and cfPWV in general patients.
A total of 1358
subjects who attended the Ruijin Hospital (affiliated with the Shanghai Jiao Tong
University School of Medicine) from December 2018 to August 2022 were included in
this study. The inclusion criteria were health
assessment, age
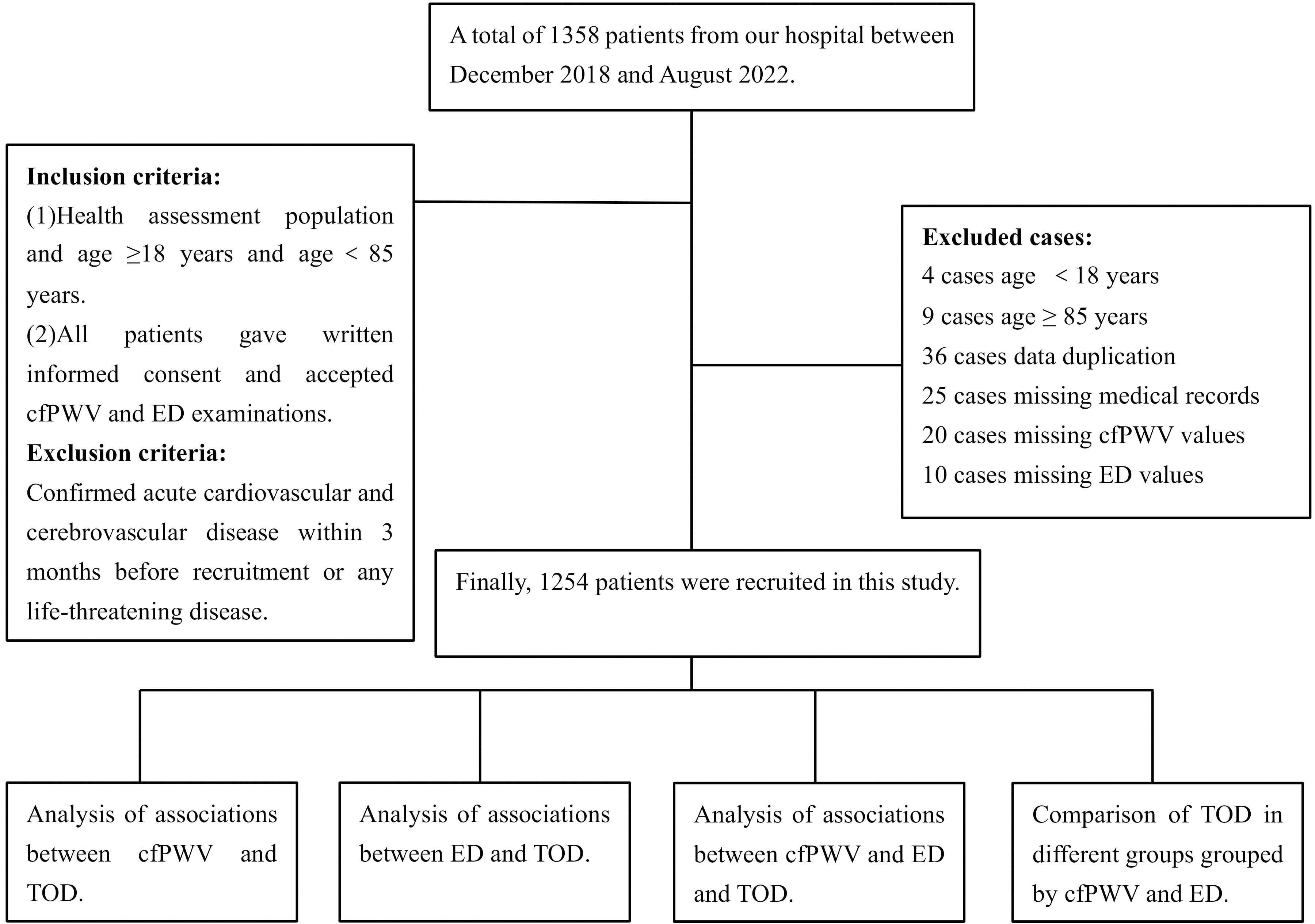 Fig. 1.
Fig. 1.Flowchart of the research protocol.
A high-fidelity SPT-304 micromanometer (20172216993, Millar Instruments, Houston, TX,
USA) interfaced with a laptop computer was used to obtain radial waveforms and pulse wave analysis measurements by
applanation tonometry. SphygmoCor software (version 8.0, AtCor Medical, Sydney, Australia) was used to generate a
reconstructed aortic pulse waveform from radial waveforms using a transfer
function [18]. ED, subendocardial viability
ratio (SEVR) and other hemodynamic indices including the
central augmentation index (cAIx), cAIx adjusted to a heart rate of 75 bpm (beats
per minute) (AIx@HR75), central diastolic blood pressure (cDBP), central systolic
blood pressure (cSBP) and central mean arterial blood pressure (cMAP) were
derived from the reconstructed aortic waveform. For
calibrating radial waveforms, triplicate recordings of left brachial blood
pressure and a 10-s sample of brachial pulse waves were measured by a validated
Omron 705 CP oscillometric
device (HEM-705cp, Omron, Kyoto, Japan) [19]. For this measurement, the subject
was in the supine position in a quiet room with stable
temperature for at least 10 minutes of rest, and without
caffeine, smoking or exercise for 30 minutes prior to examination [20]. ED was
reported in milliseconds (ED ms) and as a percentage of the cardiac cycle (ED%).
It was defined as beginning with the initial upstroke of the forward wave and
ending with occurrence of the dicrotic notch [21]. Peripheral mean arterial blood pressure (pMAP) was calculated
using the following formula: pMAP = peripheral diastolic blood pressure (pDBP) +
1/3 [peripheral systolic blood pressure (pSBP) – pDBP].
Recordings were discarded if the diastolic or systolic
variability of consecutive waveforms exceeded 5%, or if the raw amplitude of the
recorded pulse wave signal was
The carotid-femoral pulse
wave velocity (cfPWV) was calculated using the formular: cfPWV
(m/s) = [(the distance of the suprasternal notch to the femoral artery — the
distance from the suprasternal notch to the carotid artery) (m)/the transit time
of the pulse wave (s)]. Shortly after the measurement of office blood pressure,
the right side carotid and femoral arterial waveforms were derived by
applanation tonometry. Patients fasted overnight and no
caffeine beverage or smoking was allowed within 3 hours of the measurement.
PWV was measured using SphygmoCor (version 8.0, AtCor Medical,
Sydney, Australia). For this study, “normal cfPWV” was
defined as cfPWV
LVH was defined as a left ventricular mass index (LVMI)
Spot morning urine samples obtained from participants were used to measure the
urinary albumin-creatinine ratio (ACR). Abnormal albuminuria
was defined as urine ACR
Carotid intima-media thickness was assessed bilaterally by high-resolution
Doppler ultrasound (HD11EX Ultrasound, Philips Medical
Systems, Andover, MA, USA) with a broadband linear array transducer,
preferentially at frequencies
All analyses were performed using SPSS 24.0 for Windows (SPSS Inc, Chicago, IL,
USA). A two-sided p value of
A total of 1254 patients (mean age 53.13
| Variable | Overall | Male | Female | p value |
|---|---|---|---|---|
| N = 1254 | N = 806 | N = 448 | ||
| Age (years) | 53.13 |
52.11 |
54.95 |
|
| Sex, n (%) | NA | 806/1254 (64.27) | 448/1254 (35.73) | NA |
| Height (cm) | 167.41 |
171.41 |
160.22 |
|
| BMI (Kg/m |
25.32 |
25.93 |
24.23 |
|
| Smoking history, n (%) | 215/1254 (17.15) | 199/806 (24.69) | 16/448 (3.57) | |
| Antihypertensive agents, n (%) | 391/1254 (31.18) | 291/806 (36.10) | 100/448 (22.32) | |
| Serum uric acid ( |
365.19 |
394.99 |
311.68 |
|
| TG (mmol/L) | 1.93 |
2.09 |
1.64 |
|
| TC (mmol/L) | 4.81 |
4.71 |
4.99 |
|
| HDL-c (mmol/L) | 1.15 |
1.08 |
1.27 |
|
| LDL-c (mmol/L) | 3.13 |
3.08 |
3.22 |
0.005 |
| FBG (mmol/L) | 5.78 |
5.85 |
5.65 |
0.055 |
| HbA1c (%) | 6.16 |
6.17 |
6.12 |
0.556 |
| pSBP (mmHg) | 130.68 |
131.45 |
129.28 |
0.058 |
| pDBP (mmHg) | 76.71 |
78.14 |
74.14 |
|
| pMAP (mmHg) | 94.70 |
95.91 |
92.52 |
|
| cSBP (mmHg) | 119.68 |
119.95 |
119.19 |
0.492 |
| cDBP (mmHg) | 77.81 |
79.23 |
75.26 |
|
| cMAP (mmHg) | 95.52 |
96.53 |
93.71 |
0.001 |
| cAP | 12.61 |
11.58 |
14.46 |
|
| cAIX | 28.81 |
27.13 |
31.83 |
|
| cAIX@HR75 | 25.31 |
23.54 |
28.49 |
|
| HR (beat/min) | 69.24 |
69.20 |
69.32 |
0.837 |
| cfPWV (m/s) | 8.24 |
8.35 |
8.05 |
0.012 |
| LVMI (g/m |
103.44 |
106.45 |
96.88 |
|
| eGFR (mL/min/1.73 m |
90.28 |
92.44 |
86.39 |
|
| LogACR (mg/mmol) | 0.39 |
0.39 |
0.38 |
0.685 |
| CIMT (mm) | 0.74 |
0.75 |
0.73 |
0.036 |
| LVH, n (%) | 298/836 (35.65) | 173/573 (30.19) | 125/263 (47.53) | |
| CKD, n (%) | 36/1191 (3.02) | 17/765 (2.22) | 19/426 (4.46) | 0.031 |
| ACR abnormality, n (%) | 129/754 (17.11) | 94/520 (18.08) | 35/234 (14.96) | 0.293 |
| CIMT abnormality, n (%) | 386/791 (48.80) | 270/524 (51.53) | 116/267 (43.45) | 0.032 |
| ED (ms) | 318.68 |
314.83 |
325.62 |
|
| SEVR (%) | 144.72 |
148.89 |
137.21 |
Data shown are the mean
Pearson correlation analysis showed that cfPWV was positively correlated with
LVMI (r = 0.325, p
| Variable | LVMI | eGFR | LogACR | CIMT | ||||
|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | |
| cfPWV | 0.325** | –0.234 | 0.188** | 0.283** | ||||
| ED | –0.132** | –0.045 | 0.118 | –0.052 | 0.184 | –0.015 | 0.672 | |
cfPWV, carotid-femoral pulse wave velocity; ED, ejection duration; LVMI, left ventricular myopathy index; eGFR, estimated glomerular filtration rate; ACR, albumin–creatinine ratio; CIMT, carotid intima-media thickness.
**, Significant at 0.01 level (two tailed).
cfPWV and ED were added separately into
multiple stepwise linear regression models with risk factors. The results of this
analysis showed that cfPWV was significantly associated with age, pMAP, FBG, HR,
height, antihypertensive treatment (yes or no) and BMI (p
| Variable | B | SE | t | p value | 95% CI | VIF | |||
|---|---|---|---|---|---|---|---|---|---|
| LL | UL | ||||||||
| cfPWV | Constant | –6.648 | 1.129 | –5.890 | 0.000 | –8.863 | –4.433 | ||
| Age | 0.081 | 0.004 | 0.504 | 20.589 | 0.000 | 0.073 | 0.089 | 1.173 | |
| pMAP | 0.053 | 0.004 | 0.343 | 14.282 | 0.000 | 0.045 | 0.060 | 1.130 | |
| FBG | 0.114 | 0.026 | 0.102 | 4.346 | 0.000 | 0.062 | 0.165 | 1.071 | |
| HR | 0.018 | 0.004 | 0.093 | 4.013 | 0.000 | 0.009 | 0.027 | 1.063 | |
| Height | 0.017 | 0.006 | 0.071 | 2.942 | 0.003 | 0.006 | 0.029 | 1.135 | |
| Antihypertensive treatment | 0.220 | 0.099 | 0.052 | 2.222 | 0.026 | 0.026 | 0.415 | 1.072 | |
| BMI | 0.027 | 0.013 | 0.053 | 2.181 | 0.029 | 0.003 | 0.052 | 1.172 | |
| ED | Constant | 438.901 | 6.736 | 65.158 | 0.000 | 425.684 | 452.118 | ||
| HR | –1.620 | 0.054 | –0.644 | –30.024 | 0.000 | –1.726 | –1.514 | 1.034 | |
| Sex | 8.700 | 1.227 | 0.159 | 7.090 | 0.000 | 6.292 | 11.107 | 1.123 | |
| BMI | –0.425 | 0.152 | –0.063 | –2.799 | 0.005 | –0.722 | –0.127 | 1.148 | |
| HDL-c | 5.632 | 1.835 | 0.068 | 3.070 | 0.002 | 2.032 | 9.232 | 1.119 | |
| pMAP | –0.123 | 0.045 | –0.062 | –2.750 | 0.006 | –0.211 | –0.035 | 1.130 | |
| FBG | –0.646 | 0.315 | –0.044 | –2.052 | 0.040 | –1.263 | –0.028 | 1.044 | |
Risk factors of carotid-femoral pulse wave velocity (cfPWV) and ejection duration (ED) were analysed by multivariable linear regression analysis. Only variables that remained statistically significant in the final model were presented. pMAP, peripheral mean arterial pressure; FBG, fasting blood glucose; HR, heart rate (beats per minute); BMI, body mass index; HDL-c, high-density lipoprotein cholesterol; CI, confidence interval; LL, lower limit; UL, upper limit; VIF, variance inflation factor.
When cfPWV and ED were added separately to the multivariate stepwise linear
regression model, cfPWV was found to be positively correlated with LVMI (0.131
| Variable | Covariates + cfPWV | Covariates + ED | Covariates + cfPWV and ED | |||||
|---|---|---|---|---|---|---|---|---|
| cfPWV ( |
p value | ED ( |
p value | cfPWV ( |
p value | ED ( |
p value | |
| LVMI | 0.131 |
0.002 | –0.244 |
0.131 |
0.002 | –0.239 |
||
| eGFR | NA | 0.115 |
0.003 | NA | 0.115 |
0.003 | ||
| LogACR | 0.123 |
0.004 | NA | 0.123 |
0.004 | NA | ||
| CIMT | NA | NA | NA | NA | ||||
cfPWV, carotid-femoral pulse wave velocity; ED, ejection duration; TOD, target organ damage; LVMI, left ventricular myopathy index; eGFR, estimated glomerular filtration rate; ACR, albumin–creatinine ratio; CIMT, carotid intima-media thickness; NA, none. All variables were adjusted for age, sex (male or female), height, body mass index, smoking history (yes or no), antihypertensive drugs (yes or no), high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, fasting blood glucose, peripheral mean arterial pressure; heart rate (beats per minute).
When cfPWV and ED were evaluated separately by multivariate
logistic regression analysis and after adjusting for covariates, cfPWV was
found to be significantly associated with CKD (OR = 1.240, 95%
CI 1.055–1.458, p = 0.009
| Variable | B | SE | Wals | df | p value | OR | 95% CI | |||
|---|---|---|---|---|---|---|---|---|---|---|
| LL | UL | |||||||||
| Covariates + cfPWV | ||||||||||
| CKD | cfPWV | 0.215 | 0.083 | 6.806 | 1.000 | 0.009 | 1.240 | 1.055 | 1.458 | |
| Covariates + ED | ||||||||||
| LVH | ED | –0.017 | 0.005 | 14.005 | 1.000 | 0.000 | 0.983 | 0.975 | 0.992 | |
| Covariates + cfPWV + ED | ||||||||||
| LVH | ED | –0.017 | 0.005 | 14.005 | 1.000 | 0.000 | 0.983 | 0.975 | 0.992 | |
| CKD | cfPWV | 0.215 | 0.083 | 6.806 | 1.000 | 0.009 | 1.240 | 1.055 | 1.458 | |
cfPWV, carotid-femoral pulse wave velocity; ED, ejection duration; TOD, target organ damage; CKD, chronic kidney disease; LVH, left ventricular hypertrophy; OR, odds ratio; CI, confidence interval; LL, lower limit; UL, upper limit.
All variables were adjusted for age, sex (male or female), height, body mass index, smoking history, antihypertensive drugs (yes or no), high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, fasting blood glucose, peripheral mean arterial pressure; heart rate (beats per minute).
After adjusting for the covariates of age, sex, height, BMI, smoking history (yes or no), antihypertensive drugs (yes or no), HDL-c, LDL-c, FBG, pMAP and HR, LVH was found to be significantly greater in Group (high cfPWV, low ED) (OR = 6.799, 95% CI 1.305–35.427, p = 0.023), but significantly lower in Group (high ED) (OR = 0.574, 95% CI 0.374–0.882, p = 0.011) compared with Group (control). However, eGFR abnormality, ACR abnormality and CIMT thickness showed no significant differences between the different groups defined by cfPWV and ED levels (Table 6).
| Variable | B | SE | Wals | df | p value | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|
| LL | UL | ||||||||
| LVH | Age | 0.051 | 0.008 | 43.228 | 1.000 | 0.000 | 1.052 | 1.036 | 1.068 |
| Sex | 1.054 | 0.195 | 29.344 | 1.000 | 0.000 | 2.869 | 1.959 | 4.201 | |
| BMI | 0.049 | 0.023 | 4.426 | 1.000 | 0.035 | 1.050 | 1.003 | 1.099 | |
| HDL-c | –0.658 | 0.322 | 4.181 | 1.000 | 0.041 | 0.518 | 0.276 | 0.973 | |
| pMAP | 0.020 | 0.007 | 8.206 | 1.000 | 0.004 | 1.020 | 1.006 | 1.034 | |
| HR | –0.046 | 0.011 | 17.716 | 1.000 | 0.000 | 0.955 | 0.935 | 0.976 | |
| Group (control) | 15.464 | 5.000 | 0.009 | ||||||
| Group (low ED) | 0.728 | 0.406 | 3.219 | 1.000 | 0.073 | 2.071 | 0.935 | 4.588 | |
| Group (high ED) | –0.555 | 0.219 | 6.420 | 1.000 | 0.011 | 0.574 | 0.374 | 0.882 | |
| Group (high PWV) | 0.234 | 0.332 | 0.496 | 1.000 | 0.481 | 1.263 | 0.659 | 2.422 | |
| Group (high PWV low ED) | 1.917 | 0.842 | 5.180 | 1.000 | 0.023 | 6.799 | 1.305 | 35.427 | |
| Group (high PWV high ED) | –0.016 | 0.349 | 0.002 | 1.000 | 0.963 | 0.984 | 0.497 | 1.950 | |
| CKD | Age | 0.073 | 0.016 | 19.393 | 1.000 | 0.000 | 1.075 | 1.041 | 1.111 |
| ACR abnormality | Antihypertensive treatment | 0.754 | 0.222 | 11.490 | 1.000 | 0.001 | 2.126 | 1.375 | 3.288 |
| FBG | 0.145 | 0.047 | 9.392 | 1.000 | 0.002 | 1.157 | 1.054 | 1.269 | |
| pMAP | 0.038 | 0.008 | 20.506 | 1.000 | 0.000 | 1.039 | 1.022 | 1.056 | |
| CIMT abnormality | Age | 0.085 | 0.008 | 102.612 | 1.000 | 0.000 | 1.089 | 1.071 | 1.107 |
| Sex | –0.696 | 0.189 | 13.499 | 1.000 | 0.000 | 0.499 | 0.344 | 0.723 | |
| BMI | –0.062 | 0.025 | 6.296 | 1.000 | 0.012 | 0.940 | 0.896 | 0.987 | |
| Antihypertensive treatment | 0.582 | 0.176 | 10.970 | 1.000 | 0.001 | 1.789 | 1.268 | 2.524 | |
| FBG | 0.114 | 0.056 | 4.183 | 1.000 | 0.041 | 1.121 | 1.005 | 1.250 | |
| pMAP | 0.016 | 0.007 | 4.980 | 1.000 | 0.026 | 1.016 | 1.002 | 1.030 | |
TOD, target organ damage; cfPWV, carotid-femoral pulse wave velocity; ED, ejection duration; LVH, left ventricular hypertrophy; CKD, chronic kidney disease; ACR, albumin–creatinine ratio; CIMT, carotid intima-media thickness; BMI, body mass index; HDL-c, high-density lipoprotein cholesterol; pMAP, peripheral mean arterial pressure; HR, heart rate (beats per minute); FBG, fasting blood glucose; OR, odds ratio; CI, confidence interval; LL, lower limit; UL, upper limit.
All variables were adjusted for age, sex (male or female), height, BMI, smoking history, antihypertensive drugs (yes or no), HDL-c, low-density lipoprotein cholesterol, FBG, pMAP, HR.
The aim of this study was to investigate the correlations of cfPWV and ED with TOD, so as to inform the possible clinical application of ED in general patients. Whether analyzed separately or together in regression models, we found that cfPWV and ED were associated with specific TOD. Multivariate stepwise linear regression showed that cfPWV was positively correlated with LVMI and LogACR, whereas ED was negatively correlated with LVMI and positively correlated with eGFR. This was observed regardless of whether cfPWV and ED were analyzed separately or in combination. Multivariate stepwise logistic regression analysis showed that cfPWV was only associated with eGFR abnormality, whereas ED was associated with LVH after adjusting for covariates and when analyzed either individually or in combination with cfPWV. The association of ED with LVH was statistically significant when cfPWV was in the normal range. With low ED, elevated cfPWV appeared to significantly affect LVH.
In this study, cfPWV and ED were entered either separately or together into the regression models with the covariates. Since both cfPWV and ED were generated by pulse wave analysis, they were entered separately into the regression models to avoid multicollinearity. However, both cfPWV and ED were associated with TOD, hence they were entered into the same regression model with the covariates in order to evaluate and compare their impacts on TOD. The TOD in different patient groups defined by cfPWV and ED status was also analyzed in this study to help elucidate the possible interactions of cfPWV and ED with TOD. With this approach, the associations of cfPWV and/or ED with TOD could be comprehensively assessed.
The results of this study suggest that the observed association between cfPWV
with renal damage was the same using either multivariate stepwise linear or
logistic regression analysis, whereas the association between cfPWV and LVMI was
not. In contrast, ED was correlated with LVMI and eGFR by
multivariate stepwise linear regression analysis, but was only
associated with LVH by multivariate stepwise logistic regression analysis. It has
been reported in earlier studies that cfPWV was associated with cardiovascular
events and TOD [3, 27, 28, 29]. In our previous study, cfPWV showed a significant
negative association with eGFR, and the association between arterial stiffness
and CKD suggested that cfPWV may be a potential hemodynamic index to evaluate
cardiovascular risk in CKD patients with primary hypertension [30]. Moreover, a
review of arterial stiffness and CKD reported that pulse wave velocity in
patients with CKD is much higher in those with diabetes compared to patients of
similar age but without diabetes [31]. The present study showed
that cfPWV was correlated with LogACR and was associated with eGFR. These
findings concur with previous research showing that cfPWV was significantly
associated with CKD and microalbuminuria, suggesting that cfPWV
is a vessel-related and renal-related biomarker [32]. However, other studies have
shown that arterial stiffness correlates with albuminuria but not with
mild-to-moderate CKD [33], thus indicating the need to further investigate the
relationship between cfPWV and CKD. In the current study, ED was found to be
associated with LVH. ED is defined as the time in the cardiac cycle during which
the left ventricle actively ejects blood through the aortic valve and into the
circulation [34]. ED has demonstrated value for CVD risk assessment in
longitudinal studies [14] and for the progression of heart failure [35]. A
proportional relationship was demonstrated between the duration of left
ventricular ejection time (LVET), which is a component of systolic function, and
overall external myocardial efficiency [36]. A shorter LVET is known to worsen
external efficiency. LVET is also directly correlated with the
left ventricular ejection fraction (LVEF) and with stroke volume. It is shortened
in heart failure with reduced ejection fraction (HFrEF) [37]. In the present
study, ED was negatively correlated with LVMI and also with LVH (OR
After adjusting for covariates, we found that LVH was significantly higher in Group (high cfPWV, low ED) patients, but significantly lower in Group (high ED) patients. Previous studies have reported an association between arterial stiffness and left ventricular systolic function [39, 40]. In the present study, shorter ED and elevated cfPWV increased the risk of LVH, whereas normal cfPWV and increased ED was correlated with a significantly lower risk of LVH. Increased cfPWV suggests an increase in arterial stiffness, thereby contributing to dysfunction of cardiac systolic function and thus affecting ED. A previous study showed that cfPWV was significantly associated with LVH in CKD patients [39]. Central PP (pulse pressure), Aix and aortic PWV are key measures of arterial function and are susceptible to left ventricular performance [40]. ED is reported in milliseconds (ED ms) and as a percentage of the cardiac cycle (ED%). Biering-Sørensen et al. [14] found that a shorter LVET (ED ms) was associated with younger age, male sex, higher diastolic blood pressure (BP), higher incidence of diabetes, higher heart rate, higher blood glucose levels and worse fractional shortening (FS), while a lower LVET (ED%) was associated with a significantly increased risk for all events. Although the interactions between ED in combination with cfPWV and LVH are still unverified, the present study suggests there may be dependent or independent associations between ED and arterial stiffness with LVH. This requires further research before individualized management of patients can be achieved.
This study has several potential limitations. Due to its cross-sectional study design and relatively small sample size, the results need further verification in prospective studies. The study was conducted in an Asian population, and hence it is not known whether the results also apply to other ethnic groups. Furthermore, the associations between cfPWV and/or ED with TOD were studied in a general population sample, and comparison of genders should be further investigated. Despite the statistical differences observed for the interactions of cfPWV and ED with LVH, the intrinsic mechanisms involved require further investigation. Although the effects of ED on TOD were discussed in this study, the relationships between pre-ejection period (PEP)/LVET, cardiovascular outcomes and TOD remain unexplored and should be investigated in future studies. The ankle-brachial index (ABI) is defined as the ratio of systolic blood pressure between the ankle and the arm [41]. The ABI is of great significance in screening for peripheral artery disease (PAD) and for predicting cardiovascular disease [42, 43]. A low ABI is an indicator of atherosclerosis, and cfPWV is known to increase as arterial stiffness increases. In an elderly Chinese cohort, the upstroke time per cardiac cycle in the lower extremities showed a significantly stronger association with vascular and renal damage compared with the ABI [44]. Although ABI was not evaluated in the current study, the pathophysiological associations between ABI, cfPWV and ED warrant further research. Finally, the subendocardial viability ratio (SEVR) is an index of myocardial oxygen supply and demand that can be evaluated noninvasively using applanation tonometry. Low SEVR has been associated with reduced coronary flow reserve in patients with hypertension [45]. Although in the current study SEVR was compared between males and females, our focus was on the interaction between cfPWV and ED. Further studies on SEVR should therefore be considered in future research.
In conclusion, cfPWV was more strongly associated with renal damage, whereas ED was more strongly associated with LVH. cfPWV and ED affect each other and have a combined effect on LVH. Clinically, more attention should be paid to LVH in patients with high cfPWV and low ED. However, patients with low cfPWV and high ED are likely to have a lower risk of LVH.
cfPWV, carotid-femoral pulse wave velocity; ED, ejection duration; TOD, target organ damage; LVMI, left ventricular mass index; ACR, albumin-creatinine ratio; eGFR, estimated glomerular filtration rate; CKD, chronic kidney disease; LVH, left ventricular hypertrophy; CIMT, carotid intima-medium thickness; BMI, body mass index; UA, uric acid; Cr, creatinine; TC, total cholesterol; LDL-c, low-density lipoprotein cholesterol; HDL-c, high-density lipoprotein cholesterol; FBG, fasting blood glucose; HbA1c, hemoglobinA1c; cSBP, central systolic blood pressure; cDBP, central diastolic blood pressure; cMAP, central mean arterial blood pressure; cAIx, central augmentation index; cAIx@HR75, cAIx adjusted to heart rate of 75 bpm (beats per minute); SEVR, subendocardial viability ratio; pMAP, peripheral mean arterial blood pressure; K/DOQI, Kidney Disease Outcomes Quality Initiative; MDRD, Modification of Diet in Renal Disease; HR, heart rate; IMT, intima-Media Thickness; TG, total triglycerides; pDBP, peripheral diastolic blood pressure; cDBP, central diastolic blood pressure; cMAP, central mean arterial blood pressure; pSBP, peripheral systolic blood pressure; cAP, central augmentation pressure; CVD, cardiovascular disease; LVET, left ventricular ejection time; LVEF, left ventricular ejection fraction; HFrEF, heart failure with reduced ejection fraction; bPEP, brachial pre-ejection period; bET, brachial ejection time; BP, blood pressure; FS, fractional shortening; PEP, pre-ejection period.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
YYB and JLZ designed the research study. HYJ performed the research. YQ and AA provided help and advice on YYB analyzed the data. YYB, HYJ and JLZ wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
The studies involving human participants were reviewed and approved by Ethics Committee of Ruijin Hospital (Ethics No. 2011-30). The patients/participants provided their written informed consent to participate in this study.
We gratefully acknowledge the invaluable assistance of the physicians of the Department of Geriatrics, Department of Cardiovascular Medicine and Department of Endocrine and Metabolic Diseases of Ruijin Hospital, Shanghai Jiaotong University School of Medicine. This study would not have been possible without their support.
This project was supported by the National Natural Science Foundation of China (Grant No. 81500190), Clinical Science and Shanghai Municipal Hospital New Frontier Technology Joint Project (SHDC12019X20), and Shanghai Municipal Commission of Health and Family Planning (Grant No. 2020YJZX0124).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

