1 State Key Laboratory of Pathogenesis, Prevention, Treatment of Central Asian High Incidence Diseases, 830054 Urumqi, Xinjiang, China
2 Department of Cardiology, Xinjiang Medical University Affiliated First Hospital, 830054 Urumqi, Xinjiang, China
†These authors contributed equally.
Abstract
Background: The C-reactive protein–albumin–lymphocyte (CALLY) index
is a novel inflammatory biomarker, and its association with the prognosis of
coronary artery disease (CAD) after percutaneous coronary intervention (PCI) has
not previously been studied. Therefore, this study aimed to investigate the
effect of using the CALLY index on adverse outcomes in CAD patients undergoing
PCI. Methods: From December 2016 to October 2021, we consecutively
enrolled 15,250 CAD patients and performed follow-ups for primary endpoints
consisting of all-cause mortality (ACM) and cardiac mortality (CM). The CALLY
index was computed using the following formula: (albumin
Keywords
- CRP–albumin–lymphocyte index
- coronary artery disease
- percutaneous coronary intervention
- prognosis
- biomarker
Since percutaneous coronary intervention (PCI) was introduced over five decades ago, the prognosis for patients with coronary artery disease (CAD) has improved significantly [1, 2]. However, despite great advancements in the treatment of CAD, the morbidity and mortality from cardiovascular diseases in China continue to rise [3]. Inflammation occurs during the occurrence and development of atherosclerosis and has an important impact on triggering cardiovascular diseases [4]. Several new humoral biomarkers of inflammation have been established to predict the long-term outcomes of CAD patients. However, few reports have verified the practical application value of these markers in daily diagnosis and treatment processes. Therefore, there is a need for the identification of novel biomarkers regarding the risk assessment of clinical outcomes in patients after PCI.
The C-reactive protein–albumin–lymphocyte (CALLY) index, which consists of the C-reactive protein (CRP), albumin, and lymphocytes, combines the markers of inflammation, immunity, and nutrition. Iida et al. [5] initially proposed the CALLY index and reported that a low CALLY index was related to poor survival in hepatocellular carcinoma patients after hepatectomy. However, the significance of the CALLY index as a predictor has since been discovered in different cancers [6, 7, 8, 9, 10], although few data have been reported on the relationship between the CALLY index and cardiovascular events. Considering that it is easy to access and has a high quality–price ratio, the CALLY index may provide doctors with useful evidence for risk stratification in the prognosis of CAD patients undergoing PCI. In addition, since inflammatory, immunological, and nutritional conditions are commonly reported to be highly involved in cardiovascular events [11, 12, 13, 14], it is sensible to assess the predictive performance of the CALLY index in patients with CAD. Thus, using a cohort of real-world patients, we aimed to evaluate the effect of the CALLY index on the risk of long-term outcomes in patients undergoing PCI.
From December 2016 to October 2021, 15,250 consecutive CAD patients were
hospitalized at Xinjiang Medical University Affiliated First Hospital. These
details are available at http://www.chictr.org.cn (Identifier: NCT05174143).
Coronary artery disease was diagnosed as
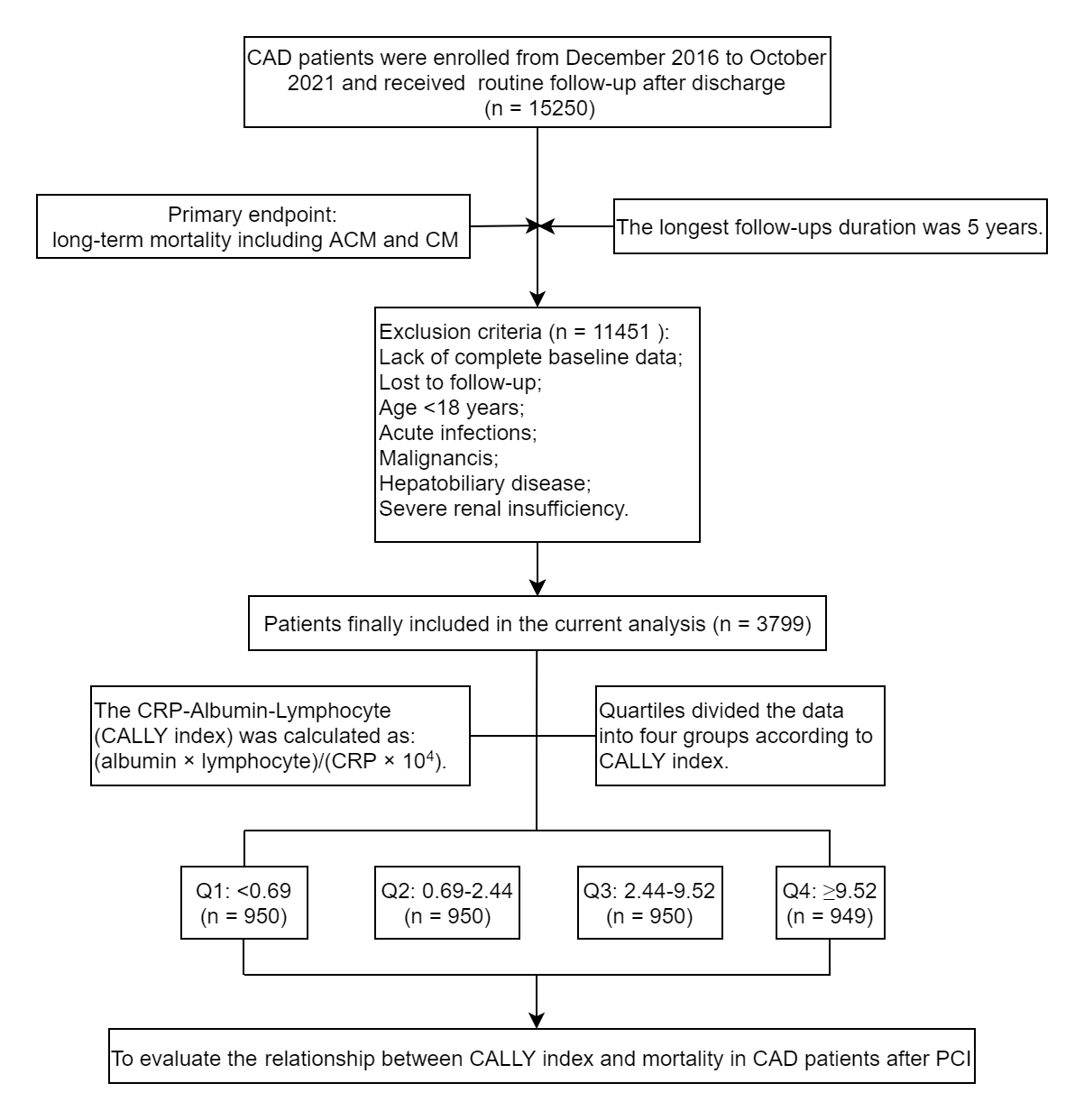 Fig. 1.
Fig. 1.Flowchart of the study. CAD, coronary artery disease; PCI, percutaneous coronary intervention; CALLY, C-reactive protein–albumin–lymphocyte; ACM, all-cause mortality; CM, cardiac mortality; CRP, C-reactive protein.
Demographic data, cardiovascular risk factors, and laboratory data were documented for all patients. We recorded cardiovascular risk factors, such as sex, age, smoking status, drinking status, and history of hypertension and diabetes. We also collected information on medications. Fasting blood samples were collected within 24 h of admission and stored in –80 °C refrigerators until testing. Serum concentrations of creatinine (Cr), uric acid (UA), triglyceride (TG), total cholesterol (TC), high-density lipoprotein-C (HDL-C), low-density lipoprotein-C (LDL-C), lymphocyte count, albumin, and CRP were measured in the Clinical Laboratory Department of Xinjiang Medical University First Affiliated Hospital using chemical analysis equipment. The severity of the coronary artery stenosis was also collected in SCAD patients and ACS patients.
Enrolled patients underwent follow-ups at 1 month, 6 months, 1 year, 3 years, and 5 years after discharge. The well-trained research coordinators evaluated the patients by office visits, telephone contact, or examination of medical records, as necessary. The occurrence of all-cause mortality (ACM) and cardiac mortality (CM) was the primary endpoint. The secondary endpoint was to assess major adverse cardiac events (MACEs), which is the combination of ACM, CM, non-fatal myocardial infarction, and unplanned coronary revascularization, alongside major adverse cardiac and cerebrovascular events (MACCEs), which were defined as MACEs plus stroke [15].
Statistical analyses were performed using SPSS 26.0 (SPSS Inc., Chicago, IL,
USA). Continuous variables are presented as either the mean (SD) or median (IQR).
Categorical data are reported as numbers and percentages. We employed the
t-test or analysis of variance and Chi-square tests or Fisher’s exact
test to compare continuous and categorical variables, respectively. The
Kaplan–Meier method was used to estimate the cumulative survival probabilities.
Univariate and multivariate Cox regression models were used to assess hazard
ratios (HRs) and corresponding 95% confidence intervals (CIs). Finally, we
plotted the restricted cubic spline between the CALLY index and adverse clinical
outcomes. A value of p
Table 1 displays the baseline characteristics of the cohort. Of the 3799 CAD
participants who had undergone PCI, most patients were men (73.0%), while the
mean age was 61.78
| Variables | Q1 | Q2 | Q3 | Q4 |
| ( |
(0.69–2.44) | (2.44–9.52) | ( | |
| Male, n (%) | 725 (76.3) | 671 (70.6) | 674 (70.9) | 704 (74.2) |
| Age, mean (SD), years | 63.52 |
62.47 |
60.86 |
60.27 |
| Smoking, n (%) | 411 (43.3) | 373 (39.3) | 348 (36.6) | 353 (37.2) |
| Drinking, n (%) | 244 (25.7) | 217 (22.8) | 203 (21.4) | 192 (20.2) |
| Hypertension, n (%) | 646 (68.0) | 670 (70.5) | 664 (69.9) | 625 (65.9) |
| Diabetes, n (%) | 686 (72.2) | 630 (66.3) | 534 (56.2) | 501 (52.8) |
| SCAD, n (%) | 258 (27.2) | 287 (30.2) | 318 (33.5) | 363 (38.3) |
| SCr, median (IQR), µmol/L | 78.7 [66.0–97.0] | 74.0 [62.4–90.0] | 72.1 [62.0–85.4] | 73.0 [62.0–86.0] |
| UA, median (IQR), mmol/L | 372.0 [299.0–482.3] | 354.7 [295.8–448.2] | 344.8 [287.1–416.7] | 335.0 [280.0–403.0] |
| HbA1c, mean (SD), mmol/L | 6.85 |
6.90 |
6.65 |
6.45 |
| TG, median (IQR), mmol/L | 1.2 [0.9–1.8] | 1.4 [1.0–2.1] | 1.6 [1.1–2.3] | 1.5 [1.1–2.2] |
| TC, mean (SD), mmol/L | 3.74 |
3.86 |
3.87 |
3.84 |
| HDL-C, mean (SD), mmol/L | 0.99 |
1.01 |
1.06 |
1.09 |
| LDL-C, mean (SD), mmol/L | 2.44 |
2.50 |
2.48 |
2.44 |
| Lymphocytes, mean (SD), |
1.95 |
2.19 |
2.28 |
2.36 |
| Albumin, mean (SD), g/L | 37.77 |
40.25 |
42.16 |
43.38 |
| CRP, median (IQR), g/L | 28.6 [16.2–63.0] | 6.5 [4.6–8.9] | 1.8 [1.3–2.7] | 0.3 [0.2–0.6] |
| Multivessel disease, n (%) | 867 (91.3) | 835 (87.9) | 816 (85.9) | 786 (82.8) |
| ACEI/ARB, n (%) | 388 (40.8) | 460 (48.4) | 414 (43.6) | 396 (41.7) |
| 509 (56.3) | 559 (60.8) | 521 (58.0) | 492 (54.6) | |
| Other lipid-lowering drugs, n (%) | 540 (59.7) | 649 (70.5) | 625 (69.5) | 634 (70.3) |
| Aspirin, n (%) | 890 (93.7) | 897 (94.4) | 905 (95.3) | 913 (96.2) |
| Statin, n (%) | 855 (90.0) | 856 (90.1) | 866 (91.2) | 883 (93.0) |
| Anticoagulation after PCI, n (%) | 136 (14.3) | 93 (9.8) | 116 (12.2) | 139 (14.6) |
| PPI, n (%) | 72 (7.6) | 42 (4.4) | 47 (4.9) | 35 (3.7) |
| Clopidogrel, n (%) | 477 (50.2) | 480 (50.5) | 460 (48.4) | 504 (53.1) |
Note: SCr, serum creatinine; UA, uric acid; HbA1c, hemoglobin A1c; TG, triglycerides; TC, total cholesterol; HDL-C, high-density lipoprotein-C; LDL-C, low-density lipoprotein-C; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; CRP, C-reactive protein; PPI, proton pump inhibitors; SCAD, stable coronary artery disease.
Among all patients, there were 216 cases of ACM during the follow-up (Table 2).
The incidence of ACM in the Q1 quartile was 105 (11.1%), while Q2 was 65
(6.8%), Q3 was 24 (2.5%), and Q4 was 22 (2.3%). The incidence of ACM was lower
in the Q3 and Q4 quartiles than in Q1 (p
| Outcomes | Q1 | Q2 | Q3 | Q4 | Chi-square or t | p-value | |
| ( |
(0.69–2.44) | (2.44–9.52) | ( | ||||
| All patients (n = 3799) | |||||||
| ACM, n (%) | 105 (11.1) | 65 (6.8) | 24 (2.5) | 22 (2.3) | 91.149 | ||
| CM, n (%) | 78 (8.2) | 53 (5.6) | 18 (1.9) | 16 (1.7) | 67.527 | ||
| MACEs, n (%) | 117 (12.3) | 95 (10.0) | 80 (8.4) | 70 (7.4) | 15.257 | 0.002 | |
| MACCEs, n (%) | 125 (13.2) | 102 (10.7) | 85 (8.9) | 78 (8.2) | 14.962 | 0.002 | |
| SCAD patients (n = 1226) | |||||||
| ACM, n (%) | 25 (9.7) | 15 (5.2) | 6 (1.9) | 9 (2.5) | 25.098 | ||
| CM, n (%) | 13 (5.0) | 14 (4.9) | 3 (0.9) | 5 (1.4) | 15.720 | 0.001 | |
| MACEs, n (%) | 23 (8.9) | 26 (9.1) | 18 (5.7) | 17 (4.7) | 7.294 | 0.063 | |
| MACCEs, n (%) | 27 (10.5) | 26 (9.1) | 21 (6.6) | 20 (5.5) | 6.533 | 0.088 | |
| ACS patients (n = 2573) | |||||||
| ACM, n (%) | 80 (11.6) | 50 (7.5) | 18 (2.8) | 13 (2.2) | 63.864 | ||
| CM, n (%) | 65 (9.4) | 39 (5.9) | 15 (2.4) | 11 (1.9) | 49.902 | ||
| MACEs, n (%) | 94 (13.6) | 69 (10.4) | 62 (9.8) | 53 (9.0) | 8.188 | 0.042 | |
| MACCEs, n (%) | 98 (14.2) | 76 (11.5) | 64 (10.1) | 58 (9.9) | 7.466 | 0.058 | |
ACM, all-cause mortality; CM, cardiac mortality; MACEs, major adverse cardiovascular events; MACCEs, major adverse cardiac and cerebrovascular events; ACS, acute coronary syndrome; SCAD, stable coronary artery disease.
Kaplan–Meier curves for the CALLY index and outcomes are shown in Fig. 2. In total, patients in high-CALLY quartiles (Q2, Q3, and Q4) showed a significantly decreased risk of ACM, CM, MACEs, and MACCEs compared with patients in the low-Q1 quartile.
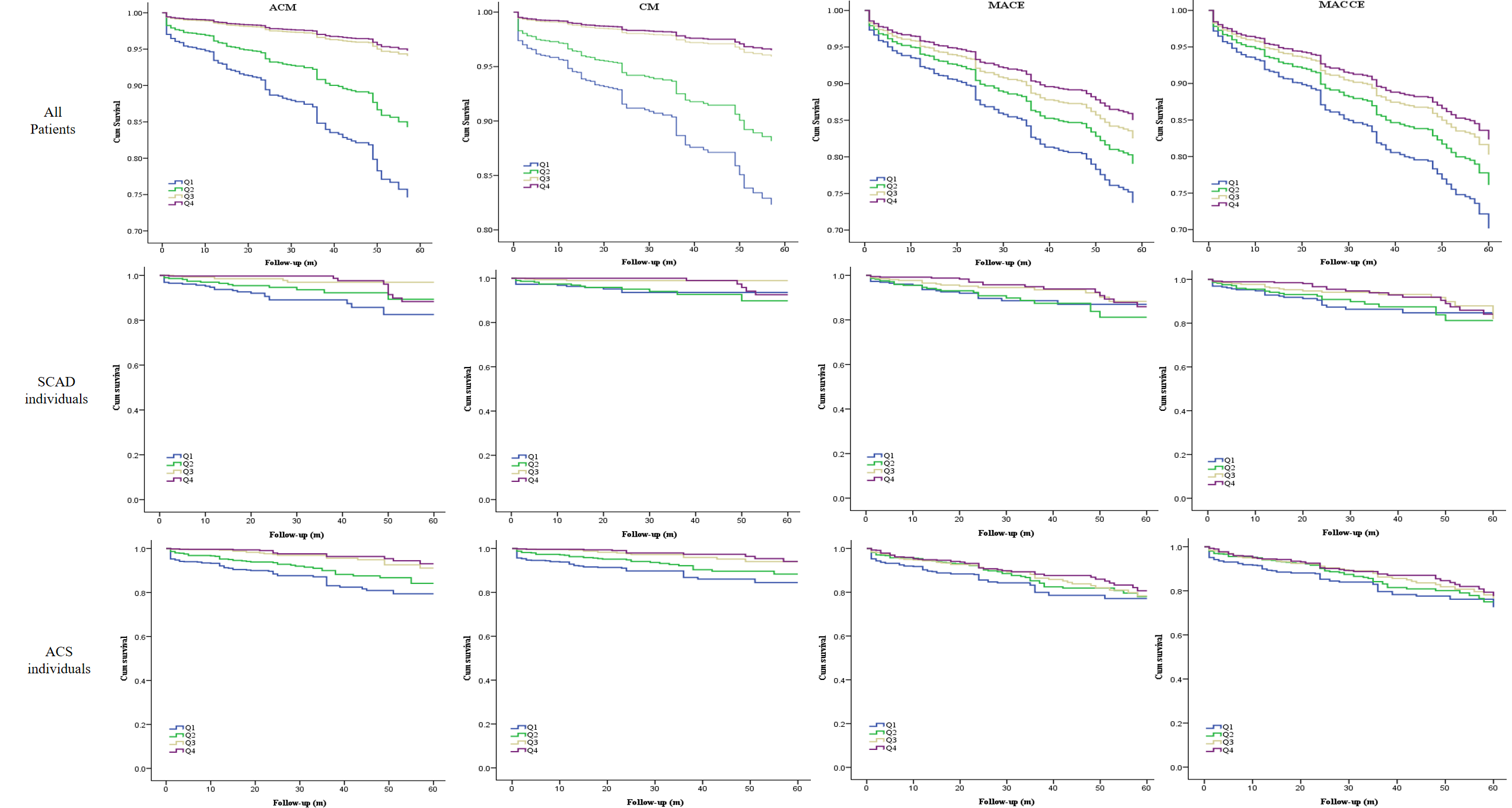 Fig. 2.
Fig. 2.Cumulative Kaplan–Meier estimates of the time for clinical outcomes to occur in all patients according to the CALLY index quartile. ACM, all-cause mortality; CM, cardiac mortality; MACEs, major adverse cardiovascular events; MACCEs, major adverse cardiac and cerebrovascular events; SCAD, stable coronary artery disease; ACS, acute coronary syndrome; CALLY, C-reactive protein–albumin–lymphocyte.
Then, we performed univariate and multivariate regression analyses and found
that the CALLY index has good predictive value for poor prognoses of CAD patients
(Table 3). After adjusting for traditional risk factors, including the history of
smoking and drinking, sex, age, Cr, UA, HbA1C, TG, and HDL-C, the risks of ACM,
CM, MACEs, and MACCEs were decreased by 77.2% (HR: 0.228, 95% CI: 0.121–0.427,
p
| Outcomes | HR | (95% CI) | p-value | adjusted HR | (95% CI) | p-value | |
| ACM (Q1 as reference) | |||||||
| Q2 | 0.584 | 0.429–0.796 | 0.001 | 0.725 | 0.488–1.076 | 0.111 | |
| Q3 | 0.209 | 0.134–0.326 | 0.228 | 0.121–0.427 | |||
| Q4 | 0.183 | 0.116–0.291 | 0.263 | 0.147–0.468 | |||
| CM (Q1 as reference) | |||||||
| Q2 | 0.648 | 0.457–0.918 | 0.015 | 0.844 | 0.537–1.327 | 0.462 | |
| Q3 | 0.214 | 0.128–0.358 | 0.252 | 0.122–0.524 | |||
| Q4 | 0.183 | 0.107–0.314 | 0.294 | 0.150–0.579 | |||
| MACEs (Q1 as reference) | |||||||
| Q2 | 0.771 | 0.588–1.011 | 0.060 | 0.899 | 0.635–1.275 | 0.552 | |
| Q3 | 0.630 | 0.474–0.838 | 0.001 | 0.671 | 0.456–0.986 | 0.042 | |
| Q4 | 0.532 | 0.395–0.716 | 0.626 | 0.422–0.929 | 0.020 | ||
| MACCEs (Q1 as reference) | |||||||
| Q2 | 0.770 | 0.593–1.001 | 0.051 | 0.887 | 0.636–1.237 | 0.481 | |
| Q3 | 0.621 | 0.471–0.818 | 0.001 | 0.639 | 0.442–0.924 | 0.017 | |
| Q4 | 0.549 | 0.413–0.729 | 0.585 | 0.401–0.856 | 0.006 | ||
ACM, all-cause mortality; CM, cardiac mortality; MACEs, major adverse cardiovascular events; MACCEs, major adverse cardiac and cerebrovascular events; HR, hazard ratio; CI, confidence interval.
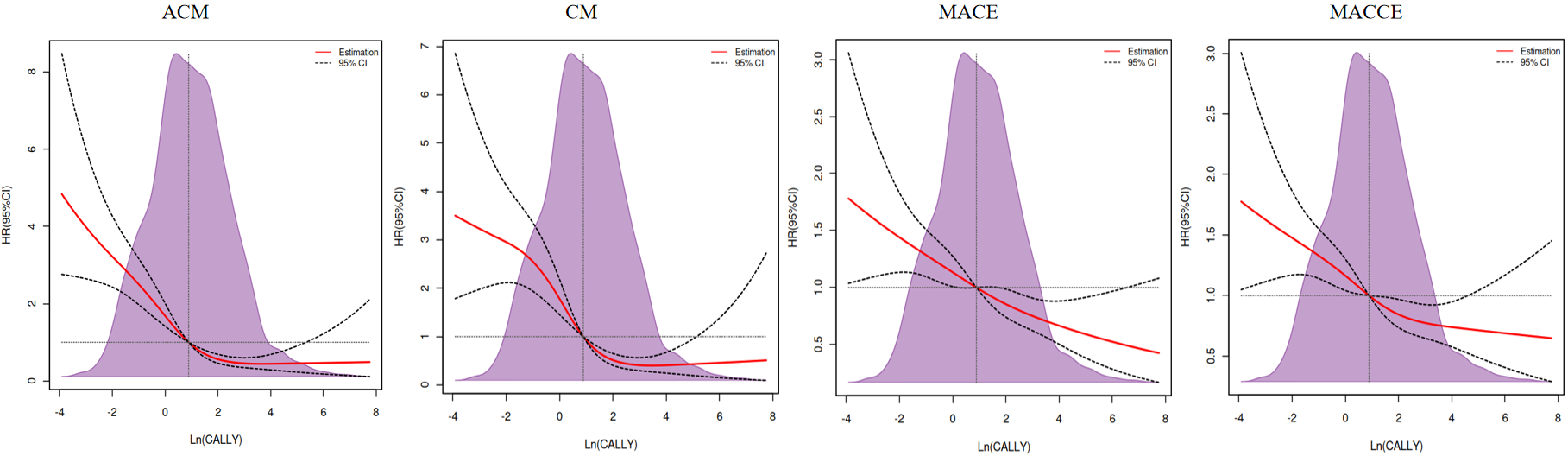 Fig. 3.
Fig. 3.Restricted cubic spline plots for mortality and ischemic events according to Ln (CALLY) continuous scale. The shaded (light purple color) area represents the percentage of the density distribution in the study population after using the CALLY index. Solid red lines are multivariable-adjusted hazard ratios (HRs), with black dotted ribbons showing 95% confidence intervals (CIs) derived from restricted cubic spline regressions with four knots. The horizontal dotted lines represent an HR of 1.0. ACM, all-cause mortality; CM, cardiac mortality; MACEs, major adverse cardiovascular events; MACCEs, major adverse cardiac and cerebrovascular events; CALLY, C-reactive protein–albumin–lymphocyte.
To our knowledge, this is the first real-world, prospective, observational cohort study to investigate the prognosis of CAD patients undergoing PCI using different CALLY index levels. We analyzed the CALLY index in 3799 CAD patients who underwent PCI. We found that patients with the lowest CALLY index had the highest incidence of mortality, MACEs, and MACCEs. There were differences in sex, age, drinking status, smoking status, diabetes history, Cr, UA, HbA1c, TG, HDL-C, lymphocytes, albumin, CRP, ACEI/ARB, and PPI among the four quartiles. Considering the influence of these confounding factors, we conducted a multivariate Cox regression analysis, in which, we found that a low CALLY index was associated with poor prognosis in CAD patients who had undergone PCI. Therefore, the results were reliable and could not be contingent.
However, the mechanisms of action between the CALLY index and poor outcomes after PCI remain unclear. We noticed that patients with the lowest CALLY index in our study had the highest CRP, lowest albumin, and lowest lymphocyte levels. Both CRP and albumin were produced mainly in the liver and could reflect the inflammation grade. However, their acute phase response to inflammation was the opposite, with CRP levels rising and albumin levels decreasing [16]. Thus, CRP appears to act as a downstream biomarker that provides a function of overall upstream cytokine activation. It directly affects vascular disease through the binding and activation of complement and plays an important role in triggering immunity in plaque deposition [17, 18]. In 1994, Liuzzo et al. [19] first underlined that a higher CRP could predict poor prognosis in ACS patients. Subsequently, several investigators have focused on the predictive value of CRP in the risk of cardiovascular disease and adverse outcomes after PCI [20, 21, 22], and have finally drawn conclusions similar to those presented by Liuzzo et al. [19]. Albumin is the predominant serum protein and is associated with nutrition status and inflammatory conditions. Albumin participates in many physiological processes, such as binding various compounds, maintaining the colloidal osmotic pressure, and decreasing platelet aggregation [23]. Hypoalbuminemia is usually considered to be caused by malnutrition, inflammation, or cachexia [24]. Previous studies have shown that a low serum albumin concentration is a risk factor for poor prognosis among patients with MI, heart failure, and CAD undergoing PCI [25, 26, 27]. Importantly, Wada et al. [28] indicated that low serum albumin and high CRP had a cooperative effect on increasing long-term ischemic risk in patients after PCI. Lastly, the lymphocytic count can reportedly be used as an early marker of physiologic “stress” and systemic failure, secondary to myocardial ischemia [29, 30]. Alternatively, low lymphocyte levels represent immunodeficiency status and could predict adverse outcomes in CAD patients [31, 32]. These findings were consistent with our results and provided theoretical and clinical support for our conclusions. Therefore, the CALLY index, based on CRP, albumin, and lymphocyte levels, is a powerful and effective prognostic biomarker for CAD patients who have undergone PCI.
The limitations of our study should be mentioned. Firstly, we only collected baseline data on CRP, albumin, and lymphocyte levels at admission. No information on the effects of changes in the CALLY index with time is available. The effect of dynamic changes in the CALLY index cannot be analyzed. Secondly, this study had a single cohort design. Our results need to be confirmed in the future by a multicenter study. Finally, the mechanism of action between the CALLY index and outcomes after PCI also requires further study.
In conclusion, this study suggests that the baseline CALLY index can be used as a novel, powerful, and inexpensive prognostic biomarker for CAD patients after PCI. The categorization of patients with a decreased CALLY index could provide valuable evidence for the risk stratification of CAD patients after PCI. However, this needs further validation.
Data of this study were available from the corresponding author upon request.
YP and TTW made substantial contributions to the conception and design of the work and drafted the manuscript. CJD, ZHJ, TY, YJF, XGH, YY and SW revised manuscript critically for important intellectual content and made substantial contributions to the acquisition, analysis, and interpretation of data for the work. YYZ and XX made substantial contributions to the conception of the work and revised manuscript critically. Each author had pa rticipated sufficiently in the work to take public responsibil ity for ap-propriate portions of the content. All authors ag reed to be accountable for all aspects of the work in ensurin g that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolv ed. All authors had read and agreed to the final version.
The protocol was performed in accordance with the Declaration of Helsinki, and approved by the ethics committee of Xinjiang Medical University Affiliated First Hospital (Y101310008). Informed consent was obtained from all patients before the intervention. Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
The authors acknowledged all nurses and doctors in the Heart Centre of Xinjiang Medical University Affiliated First Hospital. In addition, we acknowledged all patients of blood samples.
This work was supported by State Key Laboratory of Pathogenesis, Prevention, Treatment of Central Asian High Incidence Diseases Fund (SKL-HIDCA-2021-52) and National Natural Science Foundation of China (grant No. 82170345).
The authors declare no conflict of interest. Xiang Xie and Ying-Ying Zheng are serving as Guest Editors of this journal. We declare that Xiang Xie and Ying-Ying Zheng had no involvement in the peer review of this article and have no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to Filippos Triposkiadis.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.rcm2504111.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.



