1 Department of Cardiology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, 200011 Shanghai, China
†These authors contributed equally.
Abstract
Background: Lipid profiles differ naturally between individuals and
between populations. So far, the data relating to non-fasting lipid profiles has
been derived predominantly from studies on Western population. The
characteristics and clinical significance of non-fasting lipids in Chinese
patients with coronary heart disease (CHD) in response to traditional Chinese
diets remain poorly understood. Methods: A total of 1022 Chinese CHD
patients with coronary artery luminal stenosis
Keywords
- lipid
- non-fasting state
- coronary heart disease
- major adverse cardiovascular events
- coronary artery stenosis
A fasting lipid profile is typically used to assess cardiovascular risk, even though humans are mostly in a non-fasting state during the 24-hour period of each day [1, 2]. Numerous observational studies have in fact demonstrated that normal food intake has minimal effect on lipid and lipoprotein levels [3, 4, 5, 6, 7]. Non-fasting lipid measurement would not only facilitate blood lipid testing by laboratories and clinicians, but also increase patient compliance. Furthermore, various large-scale prospective studies have demonstrated that the association of non-fasting lipid profiles with the risk of cardiovascular diseases is similar to that observed with measurements taken during fasting [3, 4, 8, 9, 10]. A meta-analysis from the Emerging Risk Factors Collaboration have found that non-fasting non-high-density lipoprotein cholesterol (non-HDL-C) and non-fasting calculated low-density lipoprotein cholesterol (LDL-C) were even better for cardiovascular risk prediction than those evaluated in the fasting state [11]. Therefore, non-fasting lipid profiles have been accepted as the clinical standard in Denmark since 2009, based on recommendations from the Danish Society for Clinical Biochemistry [12]. Subsequently, the UK National Institute for Health and Care Excellence (NICE) clinical guideline CG181 endorsed the use of non-fasting lipid profiles for cardiovascular primary prevention [13]. In 2016, the joint consensus statement from the European Atherosclerosis Society (EAS) and the European Federation of Clinical Chemistry also recommended the use of non-fasting blood samples for lipid testing in routine clinical practice [14].
Lipid profiles differ naturally between individuals and between populations. So far, the data relating to non-fasting lipid profiles has been derived predominantly from studies on Western population. The characteristics and clinical significance of non-fasting lipids in Chinese patients with coronary heart disease (CHD) in response to traditional Chinese diets remain poorly understood. Therefore, we conducted a prospective observational study on Chinese CHD patients that examined both their fasting and non-fasting lipid profiles. In addition, we evaluated the predictive value of non-fasting lipid profiles for the risk of cardiovascular events during a 5-year follow-up period.
This prospective observational study was carried out at the Shanghai Ninth
People’s Hospital, Shanghai JiaoTong University School of Medicine. The study was
approved by the hospital ethics review board (2016-256-T191) and conducted in
compliance with the declaration of Helsinki. All participants signed a consent
form prior to entering the study. A total of 1203 patients with acute or stable
chest discomfort and at least one cardiovascular risk factor was screened from
January 2015 to April 2017. All participants underwent elective coronary artery
angiography after admission. Finally, 1022 patients with intermediate or severe
coronary stenosis were enrolled. A total of 181 patients were excluded because
they had mild stenosis (
Anti-platelet drugs, statins and/or other lipid-lowering drugs, angiotensin
converting enzyme inhibitor (ACEI) or angiotensin II receptor blocker (ARB),
Elective coronary angiography (Judkin’s technique) was performed on all
participants after admission. Two independent interventional experts who were
blind to the clinical information separately quantified the severity of stenosis
in the coronary artery. Luminal stenosis with a diameter narrowing of
Blood samples were collected after a 12-hour overnight fast and 4 hours after a
daily breakfast according to the participant’s dietary habit. Plasma levels of
triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol
(HDL-C) and low-density lipoprotein cholesterol (LDL-C) were assayed by an
automated biochemistry analyzer (Siemens Advia 2400, Siemens Healthcare
Diagnostics Inc., Deerfield, IL, USA). LDL-C was calculated using the Friedewald
equation [LDL-C = TC – (HDL-C) – (TG / 2.2)] when TG was
All patients visited their doctors every three months in our outpatient clinic. Patients were interviewed by telephone if they could not attend their scheduled clinic appointment. They were followed up for 5 years and any major adverse cardiovascular events (MACE) during this time were recorded. MACE was defined as the composite of all cause death, cardiac death, myocardial infarction, unscheduled coronary revascularization, and stroke. Patient follow-up was 100% complete.
IBM SPSS Statistics 23.0 (IBM Corp., Armonk, NY, USA) software was used to
perform statical analysis. The distribution of lipid profiles was confirmed by
the Shapiro-Wilk and Kolmogorov-Smirnov tests. Some lipid parameters in the
fasting and non-fasting states were not normally distributed, hence mostly
non-parametric statistical analysis was used in this study. Categorical variables
were expressed as a percentage, while continuous variables were presented as the
median [first quartile, third quartile]. Mann-Whitney U test was used to compare
continuous variables between two independent groups. The chi-square test was used
to compare categorical variables. Differences between fasting and non-fasting
lipid profiles within a single group was compared by the Wilcoxon signed-rank
test. Multivariate logistic regression analysis (forward conditional) was
performed to identify independent factors associated with the severity of
coronary artery stenosis. Lipid profiles and clinical characteristics with a
p value
Table 1 shows the baseline characteristics of the study participants. A total of
1022 CHD patients with angiographically-determined coronary artery stenosis of
| Intermediate stenosis (n = 486) | Severe stenosis (n = 536) | p value | ||
| Age (years) | 66 [60, 73] | 68 [61, 75] | 0.006 | |
| Male | 252 (51.9%) | 374 (69.8%) | ||
| BMI (kg/m |
24.49 [22.27, 26.57] | 24.75 [22.49, 26.81] | 0.316 | |
| Type of CHD | ||||
| ACS | 33 (6.8%) | 134 (25.0%) | ||
| Non-ACS | 453 (93.2%) | 402 (75.0%) | ||
| Revascularization | ||||
| PCI | 0 (0%) | 420 (78.4%) | ||
| CABG | 0 (0%) | 11 (2.1%) | ||
| Other |
486 (100%) | 105 (19.6%) | ||
| Medical history | ||||
| Smoker |
165 (34.0%) | 260 (48.5%) | ||
| Hypertension | 323 (66.5%) | 381 (71.1%) | 0.120 | |
| Diabetes mellitus | 108 (22.2%) | 202 (37.7%) | ||
| Prior history of CHD |
114 (23.5%) | 290 (54.1%) | ||
| History of atrial fibrillation | 61 (12.6%) | 72 (14.6%) | 0.710 | |
| COPD | 32 (6.6%) | 40 (7.5%) | 0.626 | |
| Family history of CVD | 260 (53.5%) | 277 (51.7%) | 0.573 | |
| Medications | ||||
| Aspirin and/or thienopyridine | 465 (95.7%) | 509 (96.8%) | 0.408 | |
| Anticoagulants | 60 (12.3%) | 72 (14.6%) | 0.641 | |
| Beta blocker | 115 (23.6%) | 133 (24.9%) | 0.715 | |
| ACEI/ARB | 129 (26.5%) | 153 (28.7%) | 0.484 | |
| CCB | 68 (14.0%) | 65 (12.1%) | 0.403 | |
| Statins | 356 (73.2%) | 446 (83.2%) | ||
| Other lipid-lowering drugs |
28 (5.8%) | 45 (9.1%) | 0.114 | |
| Laboratory variables | ||||
| Troponin I (ng/mL) | 0.00 [0.00, 0.01] | 0.01 [0.00, 0.05] | ||
| BNP (pg/mL) | 49 [24.75, 98.50] | 66 [33.00, 182.00] | ||
| CRP (mg/L) | 1.28 [1.28, 4.29] | 1.81 [1.28, 6.50] | ||
| Creatine level (µmol/L) | 78.00 [67.00, 93.00] | 81.00 [67.00, 97.00] | 0.118 | |
Values are expressed as percentage or median [first quartile, third quartile].
ACS, acute coronary syndrome; ACEI, angiotensin converting enzyme inhibitor; ARB,
angiotensin II receptor blocker; BNP, B-type natriuretic peptide; CABG, coronary
artery bypass graft; CHD, coronary heart disease; COPD, chronic obstructive
pulmonary disease; CRP, C-reaction protein; CVD, cardiovascular disease; PCI,
percutaneous coronary intervention; BMI, body mass
index; CCB, calcium channel blocker.
Lipoproteins are spherical particles that have a central core containing cholesterol esters and triglycerides, surrounded by free cholesterol, phospholipids, and apolipoproteins. They are divided mainly into five types, chylomicrons, very low-density lipoprotein (VLDL), intermediary density lipoprotein (IDL), low-density lipoprotein (LDL), and high-density lipoprotein (HDL), based on their relative size and densities. Different types of lipoproteins contain different apolipoproteins, which facilitate their function in cholesterol transportation and lipid metabolism. Table 2 shows the fasting and non-fasting lipid profiles in the study population. Four hours after normal breakfast intake, patients with intermediate or severe stenosis experienced an apparent increase in the levels of TG, RC and Apo A1 compared to the fasting state, but a significant decrease in the levels of TC, LDL-C, non-HDL-C, Apo B and Apo E (Table 2). Compared to the fasting state, the non-fasting level of HDL-C decreased significantly in the severe stenosis group but not in the intermediate stenosis group. After adjusted the baseline characteristics (age, gender, smoking and diabetes), the alterations of lipid profiles from fasting to non-fasting states in both groups remained almost unchanged (Supplementary Table 1).
| Intermediate stenosis (n = 486) | Severe stenosis (n = 536) | |||||
| Fasting | Non-fasting | p value |
Fasting | Non-fasting | p value | |
| TC (mmol/L) | 4.18 [3.61, 4.86] | 4.08 [3.52, 4.69] | 0.001 | 3.93 [3.23, 4.64] | 3.68 [3.12, 4.33] | |
| TG (mmol/L) | 1.45 [1.07, 2.02] | 1.63 [1.19, 2.25] | 1.52 [1.12, 2.14] | 1.65 [1.20, 2.31] | ||
| LDL-C (mmol/L) | 2.36 [1.87, 2.94] | 2.21 [1.72, 2.72] | 2.16 [1.62, 2.81] | 1.89 [1.45, 2.46] | ||
| HDL-C (mmol/L) | 1.02 [0.87, 1.23] | 1.01 [0.87, 1.22] | 0.703 | 0.92 [0.77, 1.11] | 0.90 [0.77, 1.08] | |
| RC (mmol/L) | 0.66 [0.49, 0.91] | 0.74 [0.54, 1.02] | 0.69 [0.50, 0.97] | 0.75 [0.55, 1.05] | ||
| Non-HDL-C (mmol/L) | 3.14 [2.55, 3.73] | 3.00 [2.48, 3.61] | 2.97 [2.31, 3.66] | 2.72 [2.21, 3.32] | ||
| Apo A1 (g/L) | 1.11 [0.99, 1.25] | 1.17 [1.04, 1.30] | 1.05 [0.93, 1.18] | 1.08 [0.97, 1.22] | ||
| Apo B (g/L) | 0.83 [0.69, 1.00] | 0.80 [0.68, 0.96] | 0.82 [0.65, 1.00] | 0.75 [0.63, 0.91] | ||
| Apo E (mg/dL) | 4.13 [3.38, 5.03] | 4.02 [3.40, 4.96] | 0.008 | 3.85 [3.11, 4.86] | 3.69 [2.97, 4.64] | |
Values are expressed as median [first quartile, third quartile]. CHD, coronary
heart disease; Apo, apolipoprotein; HDL-C, high density lipoprotein cholesterol;
LDL-C, low density lipoprotein cholesterol; RC, remnant cholesterol; TC, total
cholesterol; TG, triglyceride.
Univariate logistic regression analysis was performed to identify potential
factors associated with the severity of coronary artery stenosis. Various
clinical features (age, male, smoker, diabetes, prior history of CHD), fasting
and non-fasting levels of TC, lipoproteins (LDL-C and HDL-C) and apolipoproteins
(Apo A1, Apo B and Apo E) were significantly associated with the severity of
coronary artery stenosis (Supplementary Tables 2,3). The levels of Apo B
and non-HDL-C were highly correlated with LDL-C, while HDL-C was strongly
associated with Apo A1 (Supplementary Fig. 1). Therefore, lipoproteins
and apolipoprotein levels were entered separately into multivariate logistic
regression models. The non-HDL-C level was not included in multivariate
regression analysis. In the fasting state, multivariate logistic regression model
1 and 3 found that HDL-C (OR 0.262, 95% CI 0.158–0.436, p
During the 5-year follow-up period, 43 patients (8.85%) in the intermediate
stenosis group and 113 patients (21.08%) in the severe stenosis group
experienced a MACE. Multivariate Cox regression models that were adjusted for
non-lipid classical risk factors (age, male, smoking, diabetes and stenosis
severity) found that fasting levels of lipoproteins (LDL-C and HDL-C) and
apolipoproteins (Apo A1 and Apo B) were strongly associated with the risk of MACE
(Supplementary Tables 4,5). Multivariate Cox regression models also
showed that non-fasting levels of LDL-C, HDL-C, Apo A1 and Apo B had similar
associations with MACE (Supplementary Tables 4,5). LDL-C and Apo B in
either the fasting (LDL-C: HR 1.592, 95% CI 1.349–1.878; Apo B: HR 6.538, 95%
CI 3.614–11.827; both p
Both non-fasting and fasting levels of lipoproteins (LDL-C and HDL-C) and apolipoproteins (Apo A1 and Apo B) were included in multivariate Cox regression analysis in order to compare their prognostic value. As shown in Table 3, fasting LDL-C and Apo B as well as non-fasting HDL-C and Apo A1 were found to be independent predictors for MACE during the 5-year follow-up. This was in addition to the traditional risk factors of older age, diabetes, smoking and stenosis severity of coronary artery.
| Multivariate Cox regression | ||||
| HR | 95% CI | p value | ||
| Model 1 (Lipoproteins) | ||||
| Coronary artery stenosis severity | 1.646 | 1.137–2.383 | 0.008 | |
| Age | 1.023 | 1.007–1.040 | 0.005 | |
| Smoker |
1.455 | 1.054–2008 | 0.023 | |
| Diabetes mellitus | 1.852 | 1.343–2.554 | ||
| Fasting LDL-C (mmol/L) | 1.628 | 1.380–1.921 | ||
| Non-fasting HDL-C (mmol/L) | 0.138 | 0.064–0.296 | ||
| Model 2 (Apolipoproteins) | ||||
| Coronary artery stenosis severity | 1.777 | 1.232–2.563 | 0.002 | |
| Age | 1.024 | 1.008–1.041 | 0.003 | |
| Diabetes mellitus | 1.838 | 1.333–2.532 | ||
| Fasting Apo B (g/L) | 6.038 | 3.352–10876 | ||
| Non-fasting Apo A1 (g/L) | 0.111 | 0.045–0.274 | ||
Values are expressed as hazard ratio (HR) and 95% confidence intervals (CI).
Apo, apolipoprotein; HDL-C, high density lipoprotein cholesterol; LDL-C, low
density lipoprotein cholesterol; MACE, major adverse cardiovascular events.
The significance of non-fasting HDL-C was then investigated in this study,
because the clinical relevance of fasting LDL-C and Apo B in CHD is already
well-established. The entire cohort was divided into three groups according to
tertiles of non-fasting HDL-C. The baseline clinical characteristics and
laboratory test results for the three groups are shown in Supplementary
Table 6. A total of 353 (34.5%), 335 (32.8%), and 334 (32.7%) patients were
categorized into 1st tertile (non-fasting HDL-C
During the 5-year follow-up period, 89 (25.2%), 39 (11.6%) and 22 (6.6%) MACE
were recorded in the 1st, 2nd and 3rd tertile groups, respectively. The MACE-free
survival rate in the 1st tertile group was significantly lower than that observed
in the 3rd tertile group (Fig. 1). After adjustment for baseline clinical
characteristics (age, gender, BMI and fasting lipids), patients in the 1st
tertile group showed a significant higher risk of MACE during the 5-year
follow-up period compared to that in the 3rd tertile group (1st tertile: 2.786,
95% CI [1.808, 4.293], p
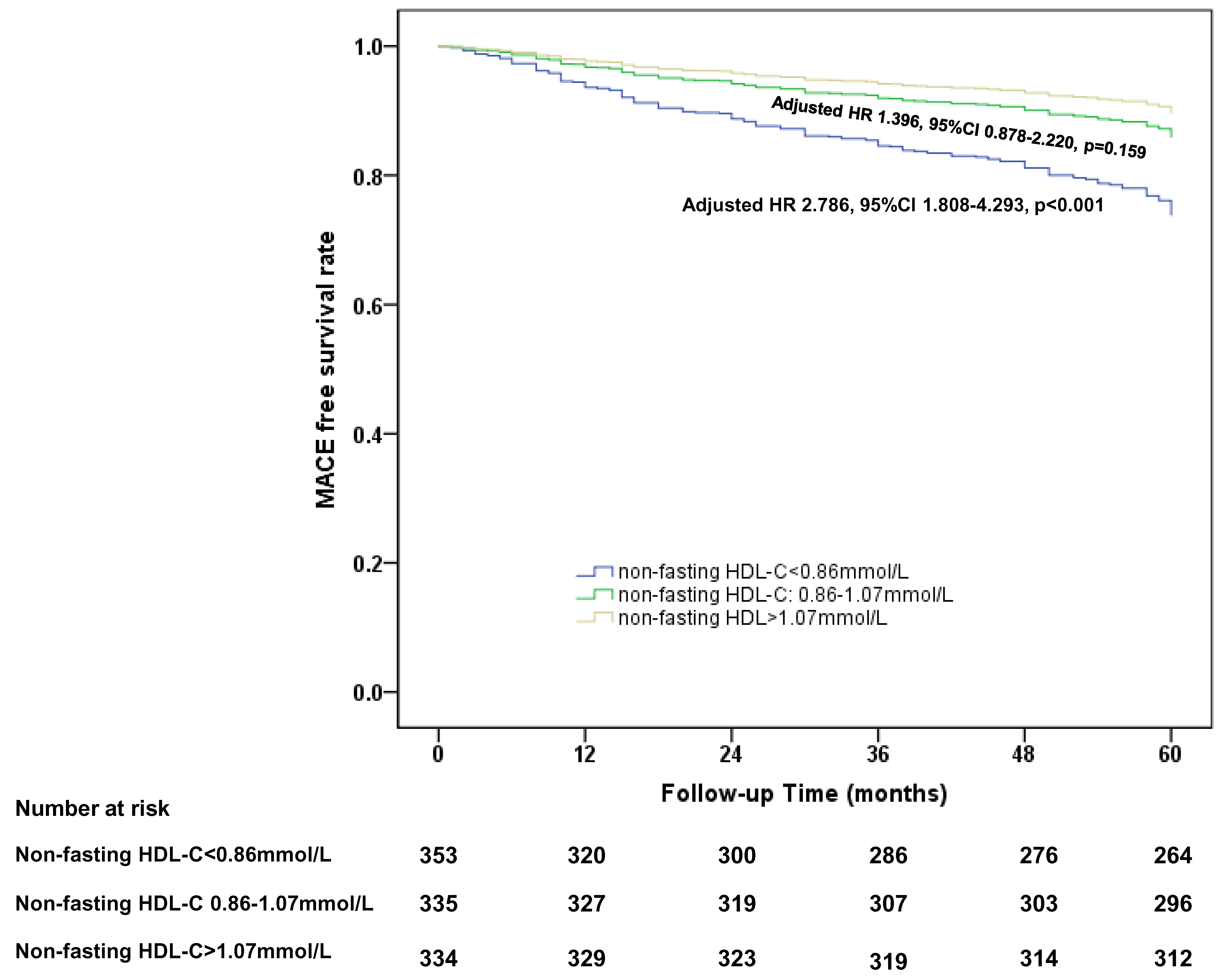 Fig. 1.
Fig. 1.Cox proportional hazards regression analysis of 5-year MACE free survival rate in CHD patients divided by the tertiles of non-fasting HDL-C level. HDL-C, high density lipoprotein cholesterol; HDL, high-density lipoprotein; CHD, coronary heart disease; MACE, major adverse cardiovascular events; HR, hazard ratio; CI, confidence intervals.
Stratified analysis of the association between non-fasting HDL-C and MACE was
conducted according to the baseline clinical characteristics. As shown in Table 4, the association between non-fasting HDL-C and MACE was independent of male,
older age, BMI, stenosis severity and a prior history of CHD. The cutoff value of
non-fasting HDL-C level associated with MACE-free survival during the 5-year
follow-up period was
| Subgroup | n | 3rd Tertile | 1st Tertile | 2nd Tertile | p value for interaction | |||
| Adjusted HR (95% CI) | p value | Adjusted HR (95% CI) | p value | |||||
| Age | 0.058 | |||||||
| 450 | Ref | 2.487 (1.356–4.563) | 0.003 | 0.680 (0.302–1.531) | 0.352 | |||
| 572 | Ref | 2.504 (1.435–4.370) | 0.001 | 1.887 (1.063–3.352) | 0.030 | |||
| Gender | 0.076 | |||||||
| Male | 626 | Ref | 2.369 (1.455–3.859) | 0.001 | 1.078 (0.614–1.894) | 0.793 | ||
| Female | 396 | Ref | 2.432 (1.138–5.198) | 0.022 | 1.889 (0.857–4.162) | 0.115 | ||
| BMI | 1022 | Ref | 2.609 (1.730–3.933) | 1.387 (0.876–2.194) | 0.163 | 0.690 | ||
| Stenosis | 0.067 | |||||||
| Intermediate | 486 | Ref | 3.249 (1.500–7.040) | 0.003 | 1.700 (0.763–3.785) | 0.194 | ||
| Severe | 536 | Ref | 1.757 (1.081–2.855) | 0.023 | 1.055 (0.603–1.843) | 0.852 | ||
| Prior history of CHD | 0.919 | |||||||
| Yes | 404 | Ref | 2.535 (1.356–4.739) | 0.004 | 1.237 (0.595–2.537) | 0.568 | ||
| No | 616 | Ref | 2.407 (1.397–4.149) | 0.002 | 1.341 (0.742–2.423) | 0.331 | ||
HDL-C, high density lipoprotein cholesterol; CHD, coronary heart disease; MACE, major adverse cardiovascular events; HR, hazard ratio; CI, confidence intervals; BMI, body mass index.
This prospective observational study investigated the clinical significance of
fasting and non-fasting lipid profiles in Chinese CHD patients. All participants
had
For many years, most guidelines or statements for the assessment of cardiovascular risk have recommended measurement of lipid profiles in a fasting state. This may be due to the dynamic changes observed in some lipid components, especially triglyceride during a postprandial test (high-fat tolerance). In fact, people eat much less fat in daily life and are mostly in a non-fasting state during 24-hour period of each day. Several large-scale, population-based studies that included men, women, children and diabetic patients have compared the fasting and non-fasting lipid levels in response to daily food intake [3, 4, 5, 6, 7]. These found a slight increase in non-fasting TG levels (0.1–0.3 mmol/L, or 10–21% increase from the fasting state) [3, 4, 5, 6, 7], and small decreases in non-fasting TC levels (0.1–0.3 mmol/L, or a 1–8% reduction from the fasting state) and LDL-C (0.1–0.3 mmol/L, or 4–9% reduction from the fasting state) [3, 4, 6, 7]. However, the changes observed between fasting and non-fasting HDL-C levels were inconsistent. Based on the Copenhagen General Population Study, the maximum mean changes at 1–6 h after habitual meals were –0.1 mmol/L for HDL-C [3]. Some studies showed the non-fasting HDL-C level remained unchanged in children aged 12 years or older, as well as in a large community-based cohort [6, 7]. Taken together, these studies suggest that lipids and lipoproteins changed only slightly in response to normal food intake in men, women and children.
The effect of daily food intake on plasma lipids has been extensively investigated in Western-population-based studies. However, the changes in non-fasting lipids in the Chinese CHD population following the intake of traditional Chinese food intake have rarely been investigated. Previous studies showed the overall levels of TC and LDL-C gradually decreased from 1 to 4 hours following normal food intake compared with fasting levels, while TG levels increased for up to 6 hours after the last meal [3, 15]. Therefore, the non-fasting blood samples used for lipid measurement in the present study were collected 4 hours after breakfast. CHD patients with intermediate or severe stenosis showed significant reductions in the levels of non-fasting TC, LDL-C and non-HDL-C compared to the fasting state. An obvious increase in the non-fasting levels of TG and RC was observed only in CHD patients with intermediate stenosis, whereas a significant reduction in non-fasting HDL-C was observed in the severe, but not intermediate stenosis group. Thus, in the present study the overall changes in lipoprotein levels observed between the fasting and non-fasting states are in line with those reported in previous large-scale, cohort studies of Western populations [3, 4, 5, 6, 7]. Alterations in lipoproteins after food intake may be attributed to overproduction and decreased catabolism of triglyceride-rich lipoproteins and their remnants, especially in patients with hypertriglyceridemia, metabolism syndrome or diabetes [16, 17]. Transfer of triglycerides from triglyceride-rich lipoproteins to HDL and LDL particles in exchange for cholesteryl esters leads to reduced HDL-C and LDL-C levels in the non-fasting state [18].
Of note, the present study found that significant changes in apolipoprotein levels between fasting and non-fasting states were observed in CHD patients with either intermediate or severe stenosis. However, the Danish general population study, the Copenhagen General Population Study, and the Copenhagen City Heart Study showed that Apo B and Apo A1 do not change in response to normal food intake [3]. This discrepancy with the current findings may be due to different study populations and dietary habits.
The current study also evaluated the significance of non-fasting lipoproteins
and apolipoproteins in terms of the long-term risk of MACE in CHD patients. Both
the fasting and non-fasting levels of lipoproteins (LDL-C and HDL-C) and
apolipoproteins (Apo A1 and Apo B) were identified by multivariate Cox
proportional hazards analysis as being independent predictors of MACE during
5-year follow-up. To compare their prognostic value, non-fasting and fasting
levels of LDL-C, HDL-C, Apo A1 and Apo B were simultaneously included in
multivariate Cox regression models. Only fasting LDL-C and Apo B as well as
non-fasting HDL-C and Apo A1 remained to be independent predictors for MACE risk.
This was in addition to the traditional risk factors (older age, diabetes,
smoking) and the stenosis severity of coronary artery. Our findings are
consistent with those of several large-scale prospective studies with long-term
follow-up that found non-fasting lipid levels were equally robust as predictors
of cardiovascular risk and mortality as fasting lipid profiles [3, 4, 8, 9, 10]. A
meta-analysis from the Emerging Risk Factors Collaboration assessed 68 long-term
prospective studies involving
In addition to lipoproteins, the present study investigated the predictive value of fasting and non-fasting apolipoprotein levels for MACE risk. Fasting Apo B and non-fasting Apo A1 were found to provide additive information for the prediction of MACE risk during a 5-year follow-up in Chinese CHD patients. The AMORIS (the apolipoprotein mortality risk) study similarly analyzed Apo A1 and Apo B as predictors of cardiac risk in large healthy populations. Apo B, Apo A1 and the Apo B/Apo A1 ratio were found to provide additional information for predicting the risk of fatal myocardial infarction to that of LDL-C alone [19]. The case-control INTERHEART (a large case-control study of acute myocardial infarction in 52 countries and sponsored by the World Health Organization) study found that the non-fasting Apo B/Apo A1 ratio was better than all other lipid parameters for predicting the risk of acute myocardial infarction in different ethnic, gender, and age groups, and therefore proposed its use in worldwide clinical practice [20]. Taken together, these findings indicate that non-fasting apolipoprotein levels may be quite valuable for cardiovascular risk management, and thereby warranting further investigation.
Apo A5 is important in TG metabolism because it activates lipoprotein lipase
(LPL)-mediated triacylglycerol lipolysis [21, 22]. Various single nucleotide
polymorphisms (SNPs) in Apo A5 have been identified in Chinese population,
including for example rs2075291 c.553G
To further investigate the clinical significance of non-fasting HDL-C in CHD patients, we divided the study population into three groups according to tertiles of the non-fasting HDL-C level. After 5-year follow-up, the risk of MACE in CHD patients with lower levels of non-fasting HDL-C was approximately 2.5 times higher than that of patients with the highest tertile (1st tertile group, adjusted HR: 2.786). The predictive value of non-fasting HDL-C for MACE was independent of the severity of coronary artery stenosis and of other conventional risk factors. Our findings shed new light on the significance of non-fasting HDL-C as a predictor of MACE in Chinese CHD patients with statin therapy. However, whether a quantitative elevation of plasma HDL-C is beneficial for cardiovascular disease prevention continues to be debatable. Concomitant diseases, drugs, dietary habit and exercise also influence the serum levels of HDL-C. HDL has several structural or functional properties, including reverse cholesterol transport, anti-inflammation, antioxidant effect, or inhibition of platelet aggregation [25]. Functional HDL is likely to be as important as HDL-C level in reducing CHD risk. Some patients with atherosclerotic cardiovascular disease (ASCVD) may have normal or even high HDL-C level but dysfunctional HDL [26]. Therefore, more research is indispensable to evaluate the association of HDL functionality with cardiovascular risk. Potential new treatment based on HDL function may improve the clinical outcome in CHD when added to statin therapy.
In 2009, the Danish Society of Clinical Biochemistry made an official recommendation on the use of lipid measurements in the non-fasting state for cardiovascular risk prediction [12]. Subsequently, the American Heart Association (AHA) [27], the National Institute for Health and Care Excellence (NICE) [13], the European Atherosclerosis Society and the European Federation of Clinical Chemistry [28], the Canadian Cardiovascular Society [29, 30] and other societies [31] updated their guidelines to recommend the use of non-fasting lipid profiles for cardiovascular risk prediction. Moreover, some major statin trials have also used non-fasting blood samples for lipid assessment, including the Heart Protection Study [32], the Anglo-Scandinavian Cardiac Outcomes Trial [33], and the Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine [34]. Although prospective studies have demonstrated the advantages and clinical significance of non-fasting lipids for cardiovascular risk prediction, studies on its cost-effectiveness are still lacking [35, 36, 37]. Driver et al. [38] noted that clinicians should carefully consider the clinical scenarios (initial cardiovascular risk assessment, residual risk of CHD, diagnosis of familial hyperlipidemia or metabolic syndrome, etc.) when choosing between the use of fasting and non-fasting lipids.
Currently in China, lipid levels in the fasting state are still used routinely
for cardiovascular risk assessment. Our study has provided preliminary evidence
of the value of non-fasting lipoproteins and apolipoproteins for cardiovascular
risk assessment of Chinese CHD patients. Lin et al. [15] have also
suggested the non-fasting LDL-C level could be used to guide the treatment of
Chinese CHD patients if the fasting LDL-C level is
This study has some limitations that should be acknowledged. Firstly, we
investigated CHD patients with intermediate or severe stenosis, most of whom
received statin therapy. Therefore, our findings cannot be applied to newly
diagnosed CHD patients who have yet to receive standard treatment. Secondly, the
lipid profiles were not regularly monitored and hence the percentage of patients
who reached the target LDL-C level (
The present study demonstrated that in addition to classical risk factors and the severity of coronary artery stenosis, the lipoprotein and apolipoprotein levels in both fasting and non-fasting states were independent predictors of the long-term risk of MACE in Chinese CHD patients. Measurement of the lipid profile in the non-fasting state may therefore be a rational and feasible approach for the management of cardiovascular risk in Chinese CHD patients. Non-fasting HDL-C level may provide additional information for CHD risk management in routine clinical practice in China, in addition to fasting LDL-C.
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
JZ and ZT enrolled, managed and followed up the participants, as well as acquired their clinical data. JJ and SH measured the lipid profiles and analyzed the data. HZen and CW performed coronary angiography. CW and HZha designed the study and interpreted the data. HZha drafted the manuscript. JZ, ZT, JJ, SH, HZen and CW reviewed the draft critically for important intellectual content. JG interpreted the data and substantively revised the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was approved by Shanghai Ninth People’s Hospital, Shanghai JiaoTong University School of Medicine Ethnics Review Board (2016-256-T191). Informed consent was obtained from all the participants.
Not applicable.
This work was supported by Natural Science Foundation of Shanghai (Grant No. 21ZR1438000) and Clinical Research Program of 9th People’s Hospital, Shanghai Jiao Tong University School of Medicine (Grant No. JYLJ202014).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

