1 Department of Cardiology, Fujian Heart Medical Center, Fujian Medical University Union Hospital, Fujian Institute of Coronary Artery Disease, Fujian Institute of Geriatrics, 350001 Fuzhou, Fujian, China
†These authors contributed equally.
Academic Editors: George Dangas, Christian Hengstenberg and Gianluca Rigatelli
Abstract
Background: A simple stenting strategy with provisional
side-branch (SB) stenting or crossover stenting has been recommended as the
default approach for most coronary bifurcation lesions (CBLs). The proximal
optimization technique (POT) and POT-associated techniques (POTAs) were
introduced to optimize the ostium of SB. However, these techniques are unable to
remove the jailed struts or completely diminish vessel damage. In this study we
developed a novel branch ostial optimization technique (BOOT) and assessed its
efficacy and safety by a propensity score matching comparison (PSM) with
POT-associated techniques (POTA). Methods: From June 2016 to March 2018,
a total of 203 consecutive patients with true CBLs were treated with BOOT (50
patients) or POTA stenting (153 patients). We performed PSM to correct for
confounders from clinical and lesion characteristics. The primary endpoint was
cumulative major adverse cardiac events (MACE) at 12 months including cardiac
death, non-fatal myocardial infarction, and target vessel/lesion
revascularization (TVR/TLR) or target vessel/lesion thrombosis (ST).
Results: After PSM, there were 43 patients in each group.
Follow-up coronary angiography was performed in 77 (89.5%) patients. At 12
months, the angiographic restenosis rate was significantly different between the
BOOT group and the POTA group after PSM (proximal main branch: 20.01
Keywords
- coronary bifurcation lesions
- percutaneous coronary intervention
- provisional stenting
- proximal optimization technique
Though a simple stenting strategy with provisional side-branch (SB) stenting or crossover stenting has been recommended as the default approach for most coronary bifurcation lesions (CBLs) [1, 2, 3], it is still debatable whether final kissing balloon dilation (FKBD) is necessary after main-vessel (MV) stenting [4, 5, 6, 7, 8]. Theoretically, FKBD is able to remove jailed struts and reduce ostial residual stenosis or restenosis [9, 10]. However, previous studies showed no benefits or even harm from routine FKBD [6, 7, 8]. The explanation for this discrepancy is that FKBD may damage ostial SB and deform the MV stent when removing the jailed struts [11, 12, 13]. Hence, a proximal optimization technique (POT) was introduced to facilitate restoration of fractal bifurcation anatomy, apposition of proximal struts onto the proximal MB wall, reorientation of jailing struts toward ostial SB, facilitation of distally rewiring, and partial relief of ostial SB compromise, resulting in a series of POT-associated techniques (POTAs) comprising POT-alone, SB dilation-POT (S-POT), POT-SB dilation-rePOT (POT-S-POT), kissing dilation-POT (K-POT), and POT-kissing dilation-rePOT (POT-K-POT) [1, 2, 13]. Nevertheless, these techniques remain unable to remove the jailed struts or completely diminish vessel damage [14, 15] particularly, when not rewiring SB distally [16]. We proposed a novel technique, the branch ostial optimization technique (BOOT), which can allow distal rewiring of SB and completely remove the struts across the SB ostium onto its proximal side-wall without distortion of the bifurcated vessel/stent, yielding the so-called “1-stent implantation with 2-stent effects”. Nevertheless, the efficacy of BOOT needs to be validated clinically.
This study sought to investigate whether BOOT is clinically feasible and superior to POTA when using a simple strategy for treatment of true or complex CBLs.
From June 2016 to March 2018, 203 consecutive patients with true CBLs (Medina’s
type 1,1,1; 0,1,1; 1,0,1) treated with a simple stenting strategy in our center
were considered eligible for enrollment. Patients with ST-segment elevation acute
myocardial infarction within 24 hours, life expectancy
BOOT: the procedural steps of BOOT include: (A) wiring the SB and MV and pretreating either branch as indicated; (B) performing sequentially snuggling balloon-stent dilation (SBSD) by the following steps: pre-staying a compliance balloon in the SB with its proximal maker in the bifurcation core and then properly positioning of the MV stent; first inflating the SB balloon and then the stent balloon, followed by first deflating the stent balloon and then SB balloon; (C) conducting the proximal optimization technique (POT) at the operator’s discretion; (D) rewiring the SB closest to the carina; (E) performing sequentially kissing or snuggling balloon dilation (SKBD/SSBD) with preference to the latter: placing 2 non-compliance balloons with mini-juxtaposition or snuggling-position in the bifurcation core and sequentially inflating the SB and MB balloons with simultaneous deflation; (F) finalizing the procedure with (re)-POT (Fig. 1).
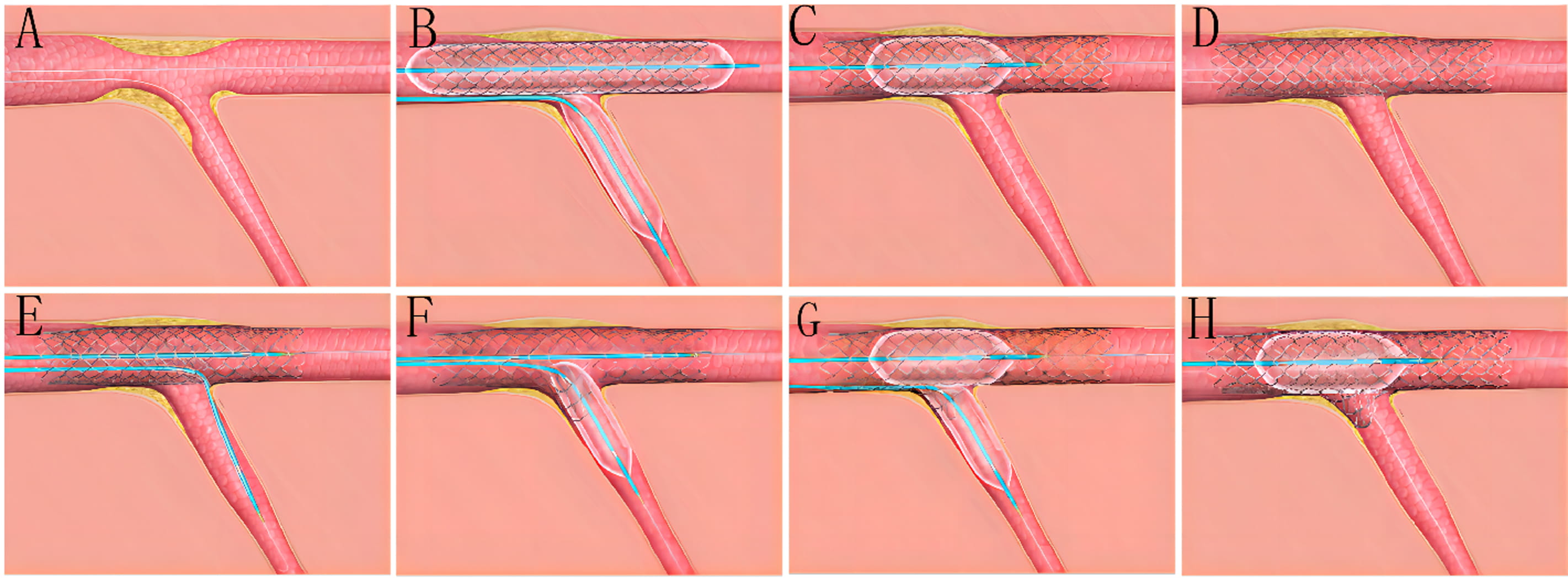 Fig. 1.
Fig. 1.The procedural steps of BOOT. (A) Wiring the SB and MV and pretreating either branch as indicated. (B) Performing sequentially snuggling balloon-stent dilation (SBSD) by following steps: pre-staying a compliance balloon in the SB with its proximal maker in the bifurcation core and then properly positioning of the MV stent; first inflating the SB balloon and then stent balloon, followed by first deflating the stent balloon and then SB balloon. (C) Conducting proximal optimization technique (POT) at operator’s discretion. (D) Rewiring the SB closest to the carina. (E–G) Performing sequentially kissing or snuggling balloon dilation (SKBD/SSBD) with preferred the latter: placing 2 non-compliance balloons with mini-juxtaposition or snuggling-position in the bifurcation core and sequentially inflating the SB and MB balloons with simultaneous deflation. (H) Finalizing the procedure with (re)-POT.
POTA: Briefly, after MV stenting, at least one of the POTAs (e.g., POT-alone, POT-S-POT, POT-K-POT) were used at the discretion of the operators. A clinical example and final results using the BOOT and POTA for treating an unstable angina patient with a severe LAD-D1 TCBL are shown by coronary angiography in Figs. 2,3, respectively.
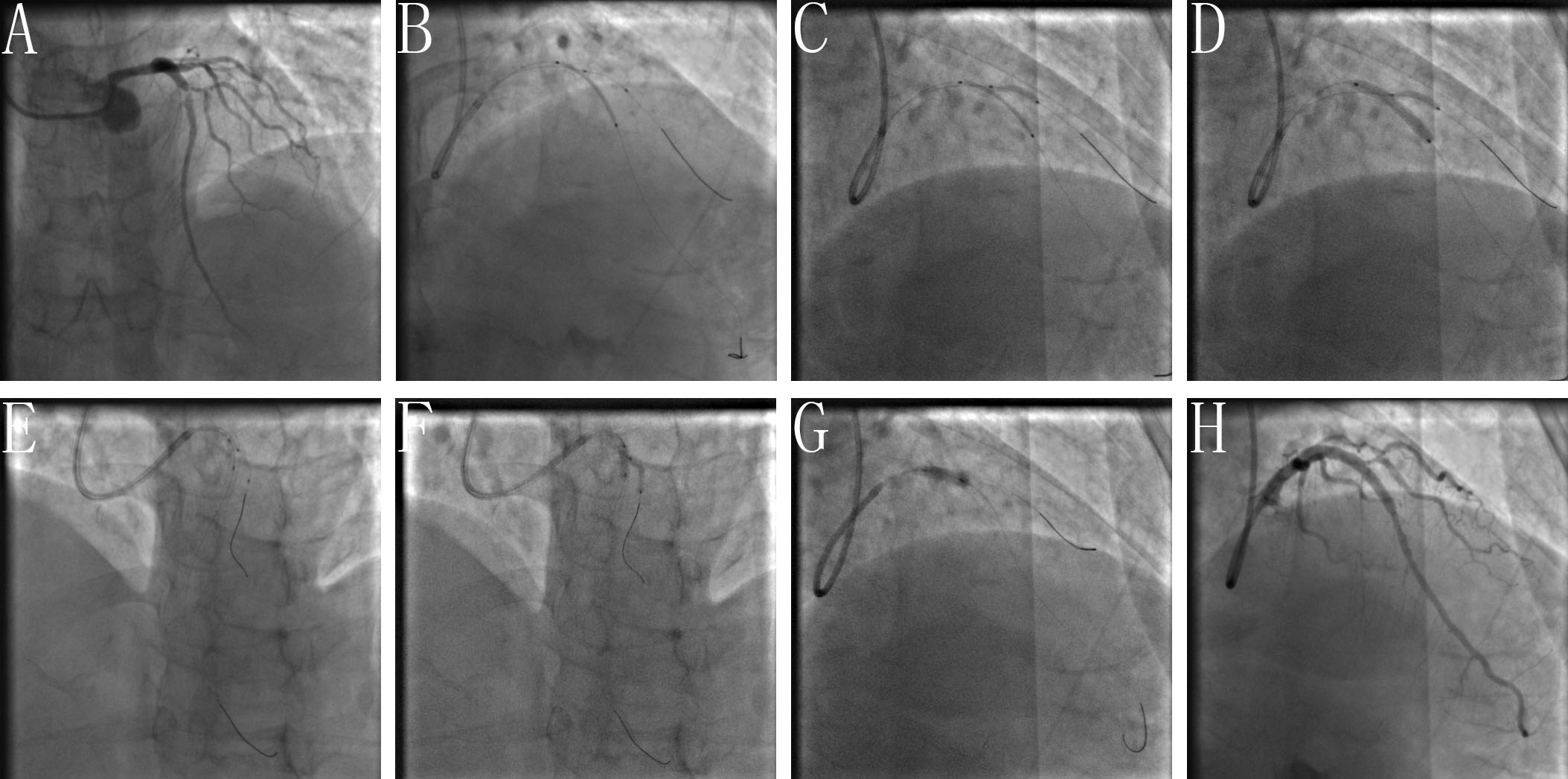 Fig. 2.
Fig. 2.Clinical practice of the BOOT technique. (A) Baseline angiogram with significant stenosis of the left anterior descending (LAD)/first diagonal bifurcation (D1) (medina classification: 1, 1, 1). (B) SBSD: pre-staying a compliance balloon in the D1 with its proximal maker in the bifurcation core and then properly positioning of the LAD stent. (C) SBSD: First inflating the D1 balloon and then stent balloon, followed by first deflating the stent balloon and then D1 balloon. (D) Snuggling balloon-stent dilation. (E) After rewiring the SB closest to the carina withdraw the pre-imbedding D1 balloon and guidewire, then placing 2 non-compliance balloons with mini-juxtaposition or snuggling-position in the bifurcation core. (F) Sequentially inflating the SB and MB balloons with simultaneous deflation. (G) Finalizing the procedure with (re)-POT. (H) Final angiogram result.
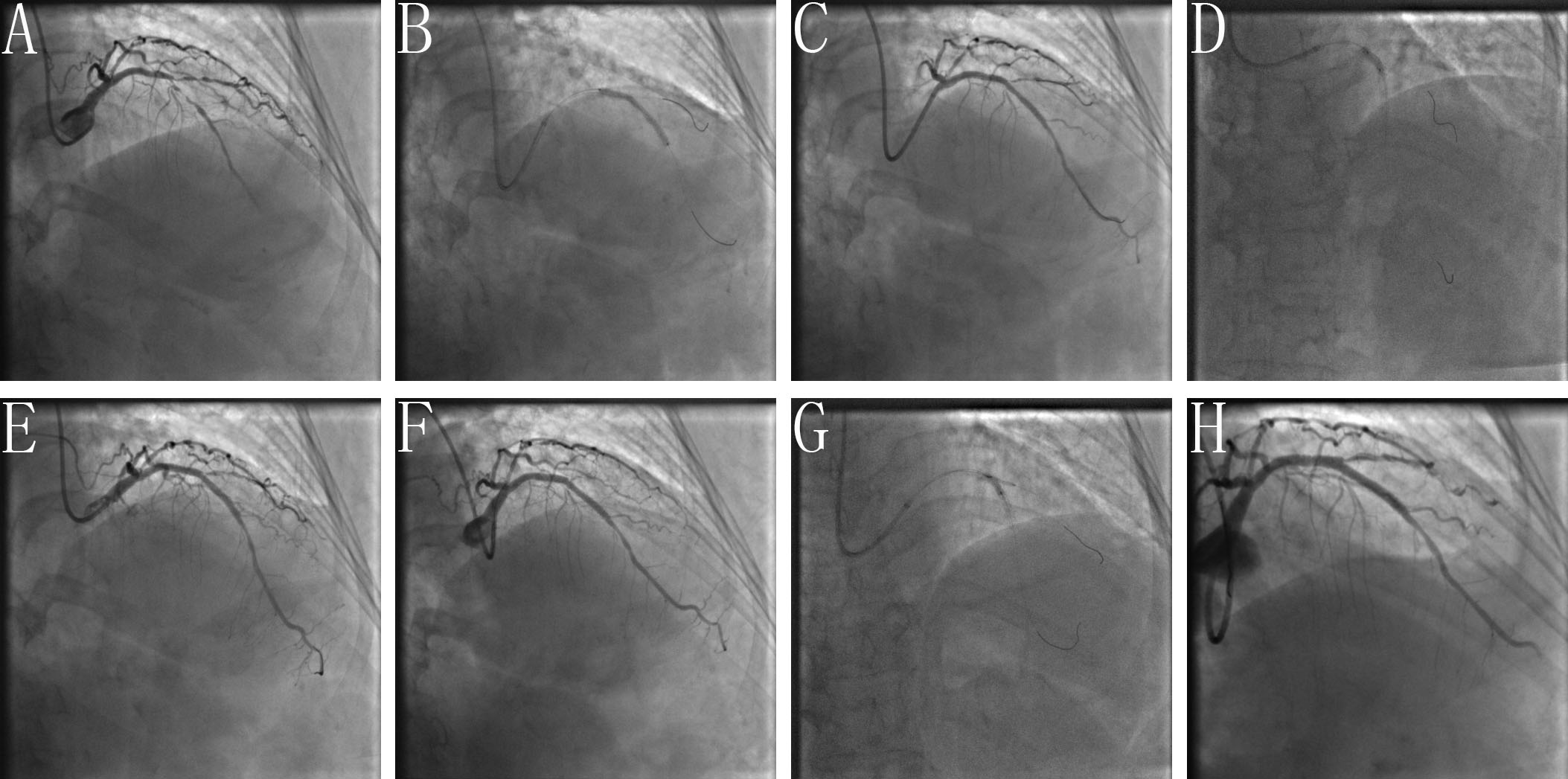 Fig. 3.
Fig. 3.Clinical practice of the POTA technique. (A) Baseline angiogram with significant stenosis of the left anterior descending (LAD)/second diagonal bifurcation (D1) (medina classification: 1, 1, 1). (B) After pre-dilation of LAD and D1, the stent is positioned covering the lesion of proximal-mid LAD with pre-imbedding a guidewire to avoid the D1 acute occlusion. (C) Rewiring the D1 through the most distal cell of the LAD stent facing the SB. (D) Performing POT with NC balloon after rewiring. (E) Angiogram shown TIMI 3 blood flow of D1 with non-dissection. (F) Acute occlusion of D1 after guide wire withdrawal. (G) Performing FKBD after rewiring LAD and D1. (H) Final angiogram shown TIMI 3 blood flow of LAD with non-residual in-stent stenosis, but type B dissection of proximal D1 with TIMI 3 blood flow.
Pre-procedurally, all patients received pretreatment with aspirin and the P2Y12 inhibitors clopidogrel or ticagrelor, with a loading dose as indicated. Intra-procedurally, non-fractionated heparin, 70–100 U/kg, was intravenously injected with a supplemental bolus of 1000 U given per hour to maintain an activated clotting time of 250–300 seconds. Post-procedure, aspirin was used indefinitely, and clopidogrel or ticagrelor for 12 months routinely. Peri-procedural glycoprotein IIb/IIIa inhibitors were left to the operator’s discretion.
Coronary angiography was performed pre-, post-procedurally, and at follow-up
after intracoronary injection of 200ug nitroglycerin, with
The reference vessel diameter (RVD), minimal lumen diameter (MLD), and lesion
length (LL) in 3 bifurcation segments were directly measured by QCA. The late
lumen loss (LLL) was calculated by the difference between the post-procedural MLD
and follow-up MLD, the diameter stenosis percent (%DS) by (RVD-MLD)/RVD
Clinical data was collected during the hospital stay and by hospital visit or
telephone contact at 1-, 3-, 6-, 9-, 12-months after discharge. Follow-up
coronary angiography was planned at 12-month (12
The major cardiac adverse events (MACEs) were composed of cardiac death,
non-fatal myocardial infarction (MI), target vessel/lesion revascularization
(TVR/TLR) or target vessel/lesion thrombosis (ST). Angiographic success was
defined as residual diameter stenosis
Non-Q-wave MI was defined by elevation of cTn values
All analyses were performed with statistical software packages (SSPS 20.0,
Chicago, IL, USA). Data were expressed as mean
Propensity score matching (PSM) was used to reduce treatment selection bias and potential impact of confounding factors from baseline clinical and lesion characteristics. Baseline clinical and lesion characteristics that could affect outcomes on univariate analysis were deemed as candidate variables. The reliability of the model was evaluated using the Hosmer-Lemeshow test. Based on the nearest match algorithm, we created case-matched pairs without replacement at a ratio of 1:1.
Among 203 eligible patients, 50 received BOOT and 153 received POTA, among them 43 pairs of patients were matched for baseline clinical and lesion characteristics by PSM. Matching was performed, based on age, hypertension, diabetes, RVD of proximal and distal main branch (MB), diameter stenosis of proximal and distal MB, LL of proximal and distal MB, RVD, diameter stenosis and LL of SB, with a caliper width equal to 0.1. Before PSM, 46 patients of the BOOT group and 134 patients of the POTA group underwent angiographic follow-up, respectively. After PSM, there were 39 patients of the BOOT group and 38 patients of the POTA group who underwent angiographic follow-up, respectively. Except for shorter lesion length and less diameter stenosis of the SB in the BOOT group before PSM, there were no differences in the baseline clinical and lesion characteristics or in the MV stent length and number between the two groups before or after PSM (Table 1).
| Before PSM | After PSM | ||||||
| BOOT (n = 50) | POTA (n = 153) | p values | BOOT (n = 43) | POTA (n = 43) | p values | ||
| Male, n (%) | 47 (94.0) | 127 (83.0) | 0.054 | 40 (93.0) | 39 (90.7) | 1.000 | |
| Age (years) | 63.5 |
66.2 |
0.115 | 63.4 |
61.9 |
0.522 | |
| Hypertension, n (%) | 34 (68.0) | 91 (59.5) | 0.282 | 28 (55.1) | 34 (79.1) | 0.149 | |
| Hypercholesterolemia, n (%) | 26 (52.0) | 87 (56.9) | 0.548 | 16 (37.2) | 18 (41.9) | 0.659 | |
| Diabetes, n (%) | 14 (28.0) | 51 (33.6) | 0.466 | 13 (30.2) | 18 (41.9) | 0.261 | |
| Smoking, n (%) | 25 (50.0) | 76 (49.7) | 0.968 | 21 (48.8) | 19 (43.2) | 0.597 | |
| Prior PCI, n (%) | 8 (16.0) | 33 (21.6) | 0.394 | 6 (14.0) | 6 (14.0) | 1.000 | |
| Prior MI, n (%) | 7 (14.0) | 22 (14.4) | 0.947 | 4 (9.3) | 8 (18.6) | 0.351 | |
| LVEF (%) | 60.7 |
60.4 |
0.86 | 61.4 |
63.2 |
0.366 | |
| Coronary artery disease, n (%) | |||||||
| Stable angina pectoris | 27 (54.0) | 95 (62.1) | 0.310 | 27 (62.8) | 29 (67.4) | 0.651 | |
| Unstablem angina pectoris | 17 (34.0) | 39 (25.5) | 0.242 | 12 (27.9) | 11 (25.6) | 0.808 | |
| NSTEMI | 6 (12.0) | 19 (12.4) | 0.938 | 4 (9.3) | 3 (7.0) | 1.000 | |
| Antiplatelet therapy, n (%) | |||||||
| Aspirin | 50 (100) | 153 (100) | 1.000 | 43 (100) | 43 (100) | 1.000 | |
| Clopidogrel/Ticargrelor | 50 (100) | 153 (100) | 1.000 | 43 (100) | 43 (100) | 1.000 | |
| GP IIb/IIIa inhibitors | 8 (16.0) | 25 (16.3) | 0.955 | 5 (11.6) | 4 (9.3) | 1.000 | |
| Data are presented as mean Abbreviations: BOOT, branch ostial optimization technique; POTA, POT-associated technique; PSM, propensity score matching; MI, myocardial infarction; PCI, percutaneous coronary intervention; NSTEMI, non-ST elevation MI; LVEF, left ventricular ejection fraction. | |||||||
Before PSM, angiographic success was significantly higher in the BOOT group than
in the POTA group (78.0% vs. 47.1%, p
| Before PSM | After PSM | ||||||
| BOOT (n = 50) | POTA (n = 153) | p values | BOOT (n = 43) | POTA (n = 43) | p values | ||
| Lesion locations, n (%) | 0.145 | 0.289 | |||||
| LM-CBLs | 12 (24.0) | 23 (15.0) | 7 (16.3) | 11 (25.6) | |||
| Non-LM-CBLs | 38 (76.0) | 130 (85.0) | 36 (83.7) | 32 (74.4) | |||
| Lesion length (mm) | |||||||
| Proximal MB | 15.82 |
13.28 |
0.114 | 14.55 |
16.52 |
0.413 | |
| Distal MB | 16.09 |
15.66 |
0.630 | 15.72 |
16.63 |
0.437 | |
| SB | 10.52 |
12.64 |
0.014 | 12.35 |
12.21 |
0.797 | |
| Reference vessel diameter (mm) | |||||||
| Proximal MB | 3.41 |
3.32 |
0.098 | 3.40 |
3.39 |
0.854 | |
| Distal MB | 2.74 |
2.64 |
0.052 | 2.96 |
2.93 |
0.994 | |
| SB | 2.30 |
2.26 |
0.361 | 2.29 |
2.27 |
0.751 | |
| Diameter stenosis (%) | |||||||
| Proximal MB | 78.17 |
79.58 |
0.145 | 79.09 |
77.69 |
0.310 | |
| Distal MB | 80.33 |
78.75 |
0.121 | 80.52 |
79.19 |
0.379 | |
| SB | 74.41 |
76.58 |
0.031 | 75.04 |
76.64 |
0.268 | |
| POT, n (%) | 50 (100) | 148 (96.7) | 0.442 | 43 (100) | 43 (100) | 1.000 | |
| MV stenting | |||||||
| Stent length (mm) | 33.44 |
31.20 |
0.291 | 31.86 |
35.56 |
0.220 | |
| Stent numbers (n) | 1.24 |
1.18 |
0.382 | 1.19 |
1.30 |
0.214 | |
| Residual stenosis |
|||||||
| MB | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| SB | 12 (24.0) | 94 (61.4) | 11 (25.6) | 26 (60.5) | 0.001 | ||
| TIMI flow |
|||||||
| MB | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| SB | 1 (2.0) | 15 (9.8) | 0.126 | 0 (0.0) | 9 (20.9) | 0.002 | |
| SB dissection |
2 (4.0) | 12 (7.8) | 0.525 | 1 (2.3) | 7 (15.9) | 0.058 | |
| SB bailout stenting*, n (%) | 2 (4.0) | 17 (11.1) | 0.169 | 1 (2.3) | 7 (15.9) | 0.058 | |
| SB angiographic success, n (%) | 39 (78.0) | 72 (47.1) | 31 (72.1) | 12 (27.9) | 0.005 | ||
| Procedural time (min) | 31.22 |
30.70 |
0.194 | 31.24 |
31.56 |
0.552 | |
| Fluoroscopy time (min) | 20.64 |
20.28 |
0.286 | 20.67 |
21.20 |
0.184 | |
| Contrast volume (mL) | 129.44 |
126.69 |
0.020 | 128.84 |
127.63 |
0.407 | |
| Data are presented as mean Abbreviations: LM-CBLs, left main coronary bifurcation lesions; MB, main-branch; MV, main-vessel; POT, proximal optimization technique; SB, side-branch; TIMI, thrombolysis in myocardial infarction. * Bailout stenting was indicated only when TIMI flow | |||||||
At baseline, RVD, MLD, %DS and LL were comparable in all segments of the
proximal MB, distal MB and SB between the groups; immediately post-procedure,
comparing BOOT versus POTA groups, there was larger MLD and less %DS in each
bifurcated segment, particularly in SB (MLD: 2.10
| Proximal MB | Distal MB | SB | ||||||||
| BOOT | POTA | p values | BOOT | POTA | p values | BOOT | POTA | p values | ||
| (n = 39) | (n = 38) | (n = 39) | (n = 38) | (n = 39) | (n = 38) | |||||
| Baseline | ||||||||||
| RVD (mm) | 3.40 |
3.39 |
0.854 | 2.96 |
2.93 |
0.994 | 2.29 |
2.27 |
0.751 | |
| MLD (mm) | 0.71 |
0.76 |
0.273 | 0.60 |
0.61 |
0.365 | 0.57 |
0.53 |
0.203 | |
| %DS | 79.09 |
77.69 |
0.310 | 80.52 |
79.19 |
0.379 | 75.04 |
76.64 |
0.268 | |
| LL (mm) | 14.55 |
16.52 |
0.413 | 15.72 |
16.63 |
0.437 | 12.35 |
12.21 |
0.797 | |
| Post-procedure | ||||||||||
| RVD (mm) | 3.41 |
3.38 |
0.812 | 2.97 |
2.95 |
0.73 | 2.32 |
2.34 |
0.820 | |
| MLD (mm) | 2.89 |
2.80 |
0.722 | 2.73 |
2.64 |
0.156 | 2.10 |
1.90 |
0.031 | |
| %DS | 16.24 |
18.98 |
0.011 | 8.11 |
10.33 |
14.00 |
18.61 |
0.004 | ||
| Follow-up | ||||||||||
| RVD (mm) | 3.45 |
3.43 |
0.672 | 3.01 |
2.94 |
0.372 | 2.42 |
2.42 |
0.954 | |
| MLD (mm) | 2.78 |
2.57 |
0.029 | 2.46 |
2.26 |
0.012 | 1.84 |
1.48 |
||
| %DS | 20.01 |
26.81 |
0.003 | 18.07 |
23.44 |
0.006 | 23.53 |
39.01 |
||
| LLL (mm) | 0.13 |
0.22 |
0.040 | 0.26 |
0.37 |
0.050 | 0.16 |
0.43 |
||
| Restenosis rate, n (%) | 0 (0.0) | 3 (7.9) | 0.115 | 0 (0.0) | 3 (7.9) | 0.115 | 1 (2.6) | 9 (23.7) | 0.007 | |
| Data are presented as mean Abbreviations: DS, diameter stenosis; LL, lesion length; LLL, late lumen loss; MLD, minimal lumen diameter; MV, main-branch; RVD, reference vessel diameter; SB, side-branch. * Before PSM, 46 patients of the BOOT group and 134 patients of the POTA group underwent angiographic follow-up, respectively. After PSM, there were 39 patients of the BOOT group and 38 patients of the POTA group who underwent angiographic follow-up, respectively. | ||||||||||
During hospitalization, MACE was rare and similar between BOOT and POTA groups before PSM (2.0% vs. 3.9%, p = 1.000) and after PSM (0.0% vs. 4.7%, p = 0.494). At 12 months follow-up, MACE was similar before PSM (8.0% vs. 11.8%, p = 0.604) between the groups and less frequent after PSM (4.7% vs. 23.3%, p = 0.026) in the BOOT group than in the POTA group, due mainly to TVR/TLR (2.3% vs. 20.9%, p = 0.015) (Table 4).
| Before propensity score matching | After propensity score matching | ||||||
| BOOT (n = 50) | POTA (n = 153) | p values | BOOT (n = 43) | POTA (n = 43) | p values | ||
| MACE in hospital, n (%) | 1.000 (2.0) | 6 (3.9) | 1.000 | 0 (0.0) | 2 (4.7) | 0.494 | |
| Non-Cardiac death, n (%) | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| Cardiac death, n (%) | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| Non-Q-wave MI, n (%) | 1 (2.0) | 6 (3.9) | 1.000 | 0 (0.0) | 2 (4.7) | 0.494 | |
| Q-wave MI, n (%) | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| Stent thrombosis, n (%) | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| Urgent TVR/TLR, n (%) | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| MACE at follow-up, n (%) | 4 (8.0) | 18 (11.8) | 0.604 | 2 (4.7) | 10 (23.3) | 0.026 | |
| Non-cardiac death, n (%) | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| Cardiac death, n (%) | 0 (0.0) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 | |
| Non-Q-wave MI, n (%) | 1 (2.0) | 2 (1.3) | 1.000 | 1 (2.3) | 0 (0.0) | 1.000 | |
| Q-wave MI, n (%) | 0 (0.0) | 1 (0.7) | 1.000 | 0 (0.0) | 1 (2.3) | 1.000 | |
| Stent thrombosis, n (%) | 1 (2.0) | 3 (2.0) | 1.000 | 1 (2.3) | 1 (2.3) | 1.000 | |
| TVR/TLR, n (%) | 2 (4.0) | 13 (8.5) | 0.368 | 1.000 (2.3) | 9 (20.9) | 0.015 | |
| Abbreviations: MACE, major adverse cardiovascular event; MI, myocardial infarction; TVR/TLR, target vessel/ lesion revascularization. | |||||||
An optimal treatment of a pinched SB is still in debate when using a simple stenting strategy [1]. This study compared POTA versus BOOT for optimization of ostial SB in treatment of true or complex CBLs with provisional SB stenting or crossover stenting. Our major findings were (1) BOOT significantly improved immediate angiographic success by reducing residual stenosis, abnormal TIMI flow, severe dissection and bailout stenting of SB; (2) BOOT significantly reduced MLD, LLL, %DS and restenosis rate at 1-year angiographic follow-up in each bifurcated segment especially in SB; (3) BOOT also significantly reduced cumulative MACE mainly by reducing TVR/TLR.
When using a simple stenting strategy for treatment of CBLs, routine FKBD is inadvisable due to its undesirable effects and inconsistent clinical outcomes [4, 5, 6, 7, 8, 19, 20, 21]; whereas POT is recommended because of its technically simplicity, but also multiply benefits, such as restoration of fractal bifurcation anatomy, apposition of proximal struts onto the proximal MB wall, prevention of wrong-way wiring, reorientation of jailing struts toward the ostial SB, facilitation of distally rewiring, and partial relief of ostial SB compromise [1, 2, 13, 16, 22]. Nevertheless, POT-alone can only partially relieve ostial SB compromise because it provides only reorientation but not complete apposition of the jailing struts onto the proximal side-wall of ostial SB, likely leaving the struts jailed in the midportion of the SB ostium [14, 15]. A recent multicenter registry investigated the efficacy of POT on crossover stenting under optical coherence tomography (OCT) guidance and showed that pre-POT (POT before MV stenting) provided no benefits such as reduction of incomplete strut apposition around the bifurcation or no increased success of guide wire re-crossing into the optimal cell [23]. In addition to POT-alone, POT can be used before or/and after FKBD or isolated SB dilation in different sequences, resulting in several combinations of POTAs (e.g., S-POT, K-POT, POT-S-rePOT, POT-K-rePOT), all of which, especially the re-POT, have been well accepted and recommended by the 11th and 12th consensuses of the European Bifurcation Club [1, 2]. However, despite the fact that S-POT and K-POT can more fully open the ostial SB, they may also cause problematic deformation of the MV stent or/and the MV itself in and beyond the bifurcation core [1, 2, 13], which can be corrected by adding a final POT to S-POT/K-POT (POT-S-rePOT or POT-K-rePOT), indicating that the re-POT is a crucial step of POTAs [13, 24].
Nevertheless, the actual results of POT-K-rePOT and POT-S-rePOT were still questioned. Our previous study showed that despite well-apposition of the struts onto the proximal vascular wall of a bifurcation, POTAs remained unable to completely remove the ostial jailed struts, even after adding a final re-POT. Conversely we also noted that displacing the jailing struts by FKBD or SB dilation frequently turned back after a final POT, leaving the struts jailed in the mid-portion of the ostial SB [14, 15]. Additionally, several previous studies also found detrimental effects due to the proximal overstretch induced by simultaneous kissing inflation of juxtaposing balloons [19, 20, 21]. Finally, currently, there are no large scale randomized clinical trials to confirm the clinical efficacy of POTAs [1, 2].
Unlike POTAs, BOOT, as shown in our previous bench testing [14, 15], is characterized by 2 crucial steps of SBSD and SKBD/SSBD (Fig. 1), SBSD enables us to distally rewire the SB closer to the carina (a key prerequisite for subsequent high quality BOOT) because it can actively prevent carina and/or plaque shifting; and SKBD/SSBD can effectively displace the jailing struts opposing onto the proximal side-wall of the SB ostium without inducing stent distortion and luminal asymmetry in the bifurcation core, resulting in the so called “lip-like ectropion of ostial struts” or “1-stent implantation with 2-stent effects”. Such favorable results observed in bench testing can also be translated into the improvement of the immediate angiographic success, follow-up angiographic results, and clinical outcomes at 1-year follow-up as demonstrated in our study.
As we have noted, POTAs were not powerful enough to correct SB compromise and MV stent distortion. A pinched SB may cause myocardial ischemia and will affect intra-procedural passage of devices (drug-coated balloon, IVUS, OCT etc.) or future SB-downstream lesion intervention. Conversely, BOOT, by its ability to fully open ostial SB without extra damage of the bifurcated vessel and/or stent, will benefit PSS or crossover stenting in several aspects: (1) affording an active protection to prevent intra-procedural SB occlusion by SSBD, securing safe application of simple stenting techniques as the initial strategy for CBLs; (2) facilitating distal rewiring of SB by SBSD, thereby avoiding intra-procedural use of OCT for guidance of distal rewiring; (3) efficiently displacing and opposing the jailing struts onto the proximal side-wall of the ostial SB by SKBD/SSBD. Overall, BOOT enables us to effectively optimize ostial SB, to finally achieve the goal of “1-stent implantation with 2-stent effects” in the majority of clinical situations, ultimately avoiding complex 2-stent techniques.
Although PSM was used to reduce selection and treatment bias and potential cofounders that may impact clinical outcomes, our study still had several limitations. First, this study was an observational, single-center study with a limited sample size. Second, pre-staying a balloon in the SB and performing SSBD may induce a potential risk of damaging the stent polymer layer or the stent itself. Third, the procedural steps may be unfamaliar for inexperienced operators. Fourth, due to the inadequate power of clinical endpoints, the conclusions of our study should be interpreted with caution. Therefore, we are conducting a randomized clinical study to confirm our observations.
When using a simple stenting strategy for CBLs, BOOT is feasible for optimization of the SB ostium and may be superior to POTAs in terms of the immediate angiographic success, QCA measurements and long-term clinical outcomes at one-year follow-up. Randomized clinical studies will be required to further validate our findings. When using a simple stenting strategy for CBLs, BOOT is feasible for optimization of the SB ostium and may be superior to POTAs in terms of the immediate angiographic success, QCA measurements and long-term clinical outcomes at one-year follow-up. Randomized clinical studies will be necessary to further validate our findings.
SB, side-branch; CBLs, coronary bifurcation lesions; FKBD, final kissing balloon dilation; MV, main-vessel; POT, proximal optimization technique; POTAs, POT-associated techniques; S-POT, SB dilation-POT; POT-S-POT, POT-SB dilation-rePOT; K-POT, kissing dilation-POT; POT-K-POT, POT-kissing dilation-rePOT; BOOT, branch ostial optimization technique; SBSD, sequentially snuggling balloon-stent dilation; SKBD/SSBD, sequentially kissing or snuggling balloon dilation; RVD, reference vessel diameter; MLD, minimal lumen diameter; LL, lesion length; LLL, late lumen loss; %DS, diameter stenosis percent; MACEs, major cardiac adverse events; MI, non-fatal myocardial infarction; TVR/TLR, target vessel/lesion revascularization; ST, target vessel/lesion thrombosis; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; PSM, propensity score matching; MB, main branch; OCT, optical coherence tomography.
EC, WC and LC designed the research study. EC, WC, LZ, LF, ZC, YL, XZ, CL and YP performed the research. EC and WC analyzed the data and wrote the original draft. LZ and LF provided help and advice on data curation. LC reviewed and edited the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript
The study protocol was approved by the Ethics Committee of Fujian Medical University Union Hospital and the informed consent was also waived for the retrospective nature (2019KY051).
Not applicable.
This work was supported by Natural Science Foundation of Fujian Province, China (Grant No. 2018J01300 and 2020J01758), and Fujian provincial health technology project (Grant NO. 2020QNA035).
The authors declare no conflict of interest.



