Noncommunicable chronic diseases, such as obesity, cardiovascular disease (CVD),
and type 2 diabetes (T2D), pose significant health challenges globally. Important
advances have been made in the understanding of the pathophysiologal mechanisms
and treatment of noncommunicable diseases in recent years. Lack of physical
activity is a primary contributor to many noncommunicable diseases including
metabolic syndrome, T2D, CVD, and obesity. Certain diabetes medications and
non-pharmaceutical interventions, such as physical activity and exercise, are
shown to be effective in decreasing the CVD risks associated with heart disease,
stroke, obesity, prediabetes, and T2D. The ability to measure and analyze
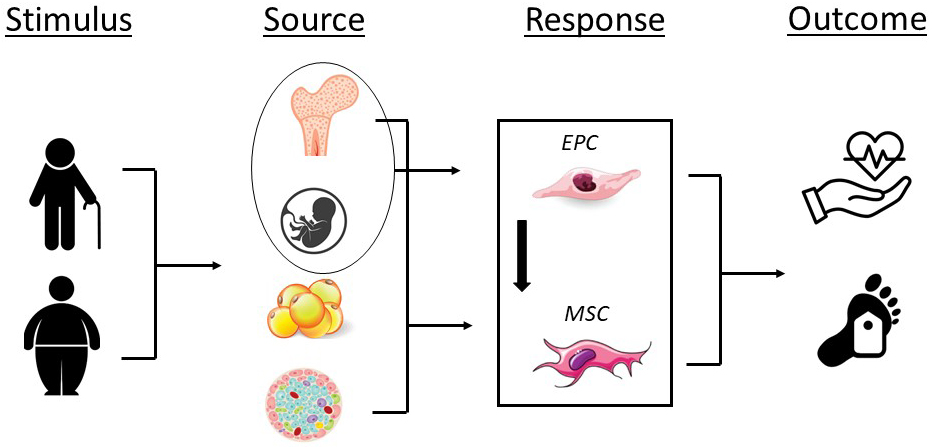
circulating adult stem cells (ASCs) has gained particular interest due to their
potential to identify at-risk individuals and implications in various
therapeutics. Therefore, the purpose of this narrative review is to (1) provide
an overview of ASCs; specifically endothelial progenitor cells (EPCs) and
mesenchymal stromal cells (MSCs), (2) describe the responses of these cells to
acute and chronic exercise, and (3) highlight the potential effect of exercise on
EPCs and MSCs in aging and disease. EPCs are circulating cells, abundantly
available in peripheral blood, bone marrow, and umbilical cord, and are defined
by cell surface markers such as CD34. EPCs are expected to play an
important role in angiogenesis and neovascularization and have been implicated in
the treatment of CVD. MSCs are essential for maintaining tissue and organ
homeostasis. MSCs are defined as multipotent heterogeneous cells that can
proliferate in vitro as plastic-adherent cells, have fibroblast-like
morphology, form colonies in vitro, and can differentiate into
ostyeoblasts, adipocytes, chondroblasts, and myoblasts. In the presence of aging
and disease, EPCs and MSCs decrease in quantity and functional capacity.
Importantly, exercise facilitates EPC differentiation and production from bone
marrow and also helps to promote migration and homing to the hypoxic and damaged
tissue which in turn improve angiogenesis and vasculogenesis. Similarly, exercise
stimulates increases in proliferation and migratory activity of MSCs. Despite the
reported benefits of exercise on EPC and MSC number and function, little is known
regarding the optimal exercise prescription for aging and clinical populations.
Moreover, the interactions between medications and exercise on EPCs and MSCs is
currently unclear. Use of ASCs as a biomarker have the potential to revolutionize
the management of patients with a variety of metabolic and obesity related
disorders and also pro-inflammatory diseases. Further investigation of clinical
entities are urgently needed to understand the implications of interventions such
as exercise, diet, and various medications on EPC and MSC quantity and function
in aging and clinical populations.