†These authors contributed equally.
Academic Editor: Hsien-Yuan Lane
Background: This study investigated the impact of repetitive
transcranial magnetic stimulation (rTMS) on serum levels of Amyloid-
Alzheimer’s disease (AD) is the most common form of dementia, affecting over fifty million people worldwide and making up 50%–75% of all dementias with an incidence roughly doubling every five years after 65 years of age [1]. The disease deprives people of their independence, and is estimated to be a main leading cause of death globally [2, 3]. A number of risk factors, including older age, diabetes, hypertension and apolipoprotein E (ApoE) genotype are associated with an increased risk of developing AD [4, 5, 6]. Despite keen interest in the development of disease-modifying drugs for AD, treatments available are largely palliative in nature. The commonly used pharmacological treatments improve cognitive function in AD in only a limited fashion [7].
Noninvasive brain stimulation interventions have demonstrated satisfactory
outcomes in clinical trials of AD. Ahmed et al. [8] showed that
repetitive transcranial magnetic stimulation (rTMS) could improve cognitive
function in patients with AD. More recent research showed that rTMS (20 Hz) at
the left dorsolateral prefrontal cortex (DLPFC) could improve cognitive function
in patients with AD [9, 10]. These findings suggest rTMS as a potentially
beneficial intervention for cognitive rehabilitation in AD with a good safety
profile. However, the mechanism by which rTMS improves cognitive functions is at
present poorly understood. Animal experiment has indicated that rTMS can reverse
abnormal levels of A
This paper aims to characterize serum levels
of A
From June 1, 2020, to December 31, 2021, patients diagnosed with AD at the rehabilitation department or neurology department of the Chongqing Daping Hospital were recruited to participate in our study. AD was diagnosed by a senior neurologist following a previously described protocol [14]. All patients participating in the study underwent MRI examination. Dementia was diagnosed according to criteria modified from the Diagnostic Statistical Manual IV (DSM-IV), and AD was diagnosed according to the standard of the National Institute of Neurological and Communicative Diseases and Stroke/Alzheimer’s Disease and Related Disorders Association [15, 16, 17, 18]. Exclusion criteria included, those who refuse to participate in the study, serious physical illness (such as liver or kidney dysfunction, or severe cardiovascular illness), history of neurological diseases (such as epileptic disorders, seizures, brain tumors or trauma), mental illnesses (such as depression, schizophrenia or delirium), Mini-Mental State Examination (MMSE) value of 0–10, and patients who were not suitable for rTMS treatment (such as those with cardiac pacemakers or other metallic bodily implants). Patients were randomized using a random table number and received either rTMS or sham treatment.
The institutional reviewing committee of Chongqing Daping Hospital approved the research, and all patients and their caregivers provided written informed consent.
For clinical assessment, case histories were gathered from patient medical records, and data on current medication use was obtained via formal questionnaire. Collected patient information included age, gender, educational level, hypertension, hypercholesterolemia, coronary artery illness, history of stroke, diabetes mellitus, as well as osteoporosis. All comorbidities were diagnosed using the international classification of diseases, 10th revision (ICD-10-CM).
We used the mini-mental state examination (MMSE), Alzheimer’s disease assessment scale-cognitive subscale (ADAS-cog), and the Montreal cognitive assessment (MoCA) as assessments of cognitive function. Activity of daily living was assessed by modified Barthel index (MBI). These scales were administered according to our previous protocol [14]. Cognitive function and activity of daily living were estimated at baseline and at 2, 3, 4, and 6 weeks after rTMS therapy. All cognitive assessments were conducted by a trained neuropsychologist who had no knowledge of participants’ treatment assignment throughout the study course.
Patients in the rTMS group received rTMS to the left DLPFC for an uninterrupted session of 20 minutes. The figure-of-eight coil was placed over the F3 point according to the International 10/20 EEG system to target the left DLPFC. Each patient underwent sessions of rTMS (20 Hz and pulses at 100% resting motor threshold intensity) five times a week for six weeks, using the rTMS system (Yiruide Medical Equipment New Technology Co., Ltd, Wuhan, China). Within each session, 2 s of stimulation was followed by a 25 s gap, with a total of 1760 pulses per session. In the sham group, an identical coil was placed on the patient, but no magnetic stimulation was administered, and the patients heard the same voice recordings as those used for patients receiving rTMS. All patients received donepezil treatment (5–10 mg/day depending on the severity of the disease).
Levels of serum A
Student’s T-test or one-way analysis of variance (ANOVA) followed by
Tukey’s post hoc test was used to analyze the normally distributed baseline
continuous data. Non-normally distributed data were represented as the median
Initially, 50 patients were screened for eligibility. One refused to participate, and a further three were excluded due to severe physical disease, cardiac pacemaker or other metal implant. Of the 46 eligible AD patients, 23 were randomly assigned to the rTMS treatment group and the other 23 were randomly assigned to the sham (non-rTMS) group. Hereafter, no patients dropped out from the study for its 6-week duration. Thus, 46 patients were included in the final statistical analysis. A summary schematic of patients’ participation is shown in Fig. 1.
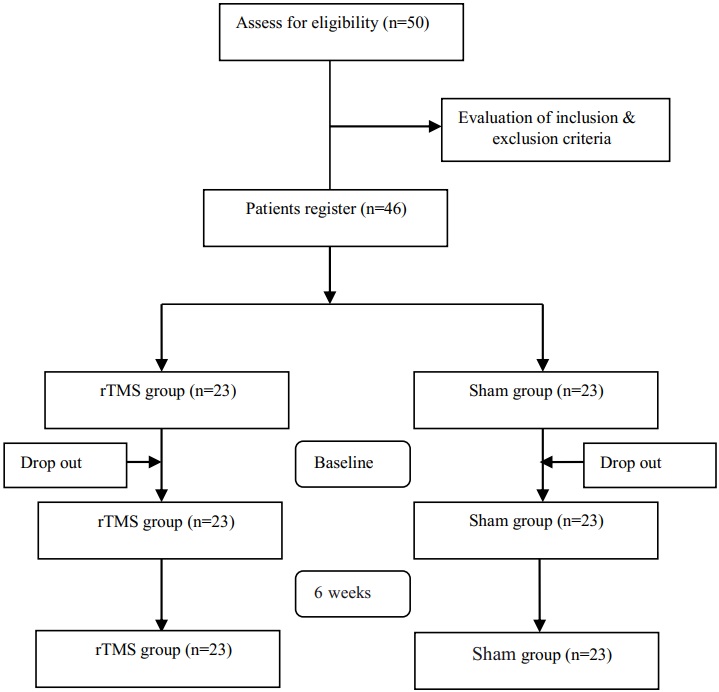 Fig. 1.
Fig. 1.A summary of the patients’ participation in the study. rTMS, repetitive transcranial magnetic stimulation.
The baseline clinic data of all patients are
shown in Table 1. At baseline, there were no significant differences between the
rTMS group and the sham group in terms of age, sex, body mass index, education
level, comorbidities, drug treatment, and cognition assessment scores (p
| Characteristics | rTMS group (n = 23) | Sham group (n = 23) | p | |
| Demographics | ||||
| Age, years |
67.8 |
68.9 |
0.473 | |
| Female, n (%) | 12 (52.2) | 13 (56.5) | 0.767 | |
| BMI, kg/m |
23.9 |
24.0 |
0.922 | |
| Educational level, years |
4.7 |
4.6 |
0.905 | |
| Comorbidities | ||||
| Hypertension, n (%) | 8 (34.8) | 7 (30.4) | 0.753 | |
| Hyperlipidemia, n (%) | 5 (21.7) | 3 (13.0) | 0.436 | |
| Diabetes, n (%) | 6 (26.1) | 2 (8.7) | 0.119 | |
| Coronary artery disease, n (%) | 3 (13.0) | 2 (8.7) | 0.520 | |
| History of stroke, n (%) | 3 (13.0) | 7 (30.4) | 0.108 | |
| Osteoporosis, n (%) | 6 (26.1) | 8 (34.8) | 0.521 | |
| Drug treatment | ||||
| Donepezil, mg |
8.3 |
8.2 |
0.899 | |
| Cognition assessment | ||||
| MoCA score |
16.0 |
15.9 |
0.878 | |
| MMSE score |
13.8 |
14.0 |
0.715 | |
| ADAS-cog score |
28.0 |
27.4 |
0.547 | |
| MBI score |
80.0 |
78.9 |
0.467 | |
| Abbreviations: BMI, body mass index; SD, standard deviation; MoCA, Montreal cognitive assessment; MMSE, mini-mental state examination; ADAS-cog, Alzheimer’s disease assessment scale–cognitive subscale; MBI, modified Barthel index; rTMS, repetitive transcranial magnetic stimulation. | ||||
Differences in serum A
| Parameter | Group (n) | Baseline visit | 2 weeks | 3 weeks | 4 weeks | 6 weeks |
| ApoE (mg/L), |
rTMS (23) | 35.41 |
35.34 |
34.28 |
34.22 |
33.49 |
| Sham (23) | 35.48 |
35.51 |
35.43 |
35.49 |
35.58 | |
| A |
rTMS (23) | 94.41 |
93.99 |
70.55 |
69.74 |
68.13 |
| Sham (23) | 92.38 |
92.11 |
92.37 |
91.23 |
90.19 | |
| A |
rTMS (23) | 62.76 |
60.85 |
42.71 |
41.68 |
40.16 |
| Sham (23) | 60.88 |
60.01 |
60.81 |
59.94 |
60.32 | |
| Total A |
rTMS (23) | 157.17 |
154.84 |
113.26 |
111.42 |
108.29 |
| Sham (23) | 153.26 |
152.12 |
153.18 |
151.17 |
150.51 | |
| p75ECD (pg/mL), |
rTMS (23) | 50.12 |
51.24 |
68.18 |
70.26 |
73.88 |
| Sham (23) | 52.33 |
53.01 |
53.28 |
53.68 |
53.36 | |
Differences in cognitive function scores at each measurement time point from
baseline are shown in Fig. 2. At week 6, the rTMS group showed a statistically
significant improvement in MoCA, MMSE and MBI scores relative to sham group
(p
 Fig. 2.
Fig. 2.Cognitive function and
activity of daily living scores at baseline and study time points for the two
groups. Cognitive function of patients with AD was assessed using MoCA, MMSE,
ADAS-cog and MBI scores. (A) Changes in MoCA score. (B) Changes in MMSE score.
(C) Changes in ADAS-cog score. (D) Changes in MBI score. *p
Serum A
| A |
A |
Total A |
p75ECD | |||||
| r-value | p-value | r-value | p-value | r-value | p-value | r-value | p-value | |
| MoCA | –0.78 | –0.76 | –0.74 | 0.84 | ||||
| MMSE | –0.83 | –0.76 | –0.81 | 0.9 | ||||
| ADAS-cog | 0.77 | 0.69 | 0.73 | –0.86 | ||||
| MBI | –0.68 | –0.61 | –0.66 | 0.72 | ||||
| Abbreviations: MoCA, Montreal cognitive assessment; MMSE, mini-mental state examination; ADAS-cog, Alzheimer’s disease assessment scale–cognitive subscale; MBI, modified Barthel index. | ||||||||
In studying the impact of rTMS on cognitive function in patients with AD, we
measured serum levels of A
There remains a lack of effective pharmacological or psychosocial interventions for AD and related dementias. Thus, there is an urgent need to investigate novel therapeutic approaches, one of which is neuromodulation. Current evidence suggests that rTMS is a non-invasive, safe and effective strategy for AD treatment [19, 20]. Recent research has demonstrated the impact of inhibitory rTMS of the prefrontal cortex on memory in patients with AD. Turriziani et al. [21] found that inhibition of the right DLPFC by rTMS improved recognition as well as memory function in patients with AD. In a study of 131 AD patients between 60 and 90 years of age, Sabbagh et al. [22] showed that patients treated with rTMS showed improvements relative to those undergoing sham procedures. In a meta-analysis of randomized controlled trials of rTMS in AD, Wang et al. [23] found a treatment benefit for patients with mild-to-moderate AD. More recently, Li et al. [9] showed significant recovery of cortical plasticity in patients with AD receiving rTMS compared to a cohort receiving pseudo-stimulation, which not only supports the clinical use of rTMS for the treatment of AD, but also provides potential clinical biomarkers for the assessment of cognitive function changes. These studies suggest that rTMS holds important therapeutic benefits for patients with AD.
While rTMS has been applied in the treatment of AD, its mechanism remains
unclear. A
Whether and how the serum levels of p75ECD change in patients with AD after rTMS
treatment is not well documented. Neurotrophin receptor p75 is an A
Whether rTMS regulates the core pathogenetic biomarkers in patients with AD, and what the potential mechanisms of that are, is still unclear. The extracellular signal-regulated kinase (ERK) 1/2 signaling pathway has been shown to be affected by rTMS. In a study of depression, it was found that rTMS promoted the proliferation of hippocampal neural stem cells by increasing the level of p-ERK1/2 [30]. In addition, magnetic stimulation promoted the proliferation of human amniotic membrane cells by activating the ERK1/2 pathway [31]. Tumor necrosis factor-convertase (TACE) is the key enzyme for p75ECD release, and its activation is achieved through phosphorylation modification. Moreover, ERK1/2 is considered a key upstream signal that regulates TACE phosphorylation [32]. Hence, we speculate that the ERK1/2 signal pathway is an important way by which rTMS regulates p75ECD release in AD.
In patients with AD, the ApoE polymorphism is the primary genetic factor related to a more aggressive clinical course. rTMS plays a potentially protective role in the prevention and treatment of AD by decreasing ApoE expression as well as promoting autophagic flux [33]. In clinical study of induced controlled brain disruption with rTMS as a model of brain injury and adaptation, ApoE polymorphism status was found to determine the effect of rTMS on distributed brain network performance [34]. In the present study, we found no distinctions in serum ApoE levels between the two study groups, however.
Our study had a number of
limitations. First, the main limitation of the study is the lack of correction of
multiple testing correction. Given this limitation, our results are probabilistic
and these data require verification in further studies. Second, it has previously
been reported that low versus high frequencies of rTMS differently impact
cognitive function as well as cortical excitability in patients with AD [8]. This
was not investigated in our study. Third, a recent study suggested that rTMS is
related to clinical cognitive improvements in individuals with mild cognitive
impairment (MCI) [35]. We did not evaluate the influence of rTMS on patients with
MCI. In addition, we did not study the relationship between rTMS and different
degrees of AD dementia. Fourth, it has been shown that rTMS mediates the
secretion and expression of brain-derived neurotrophic factor (BDNF) as well as
other proteins involved in the regulation of synaptic plasticity [36]. In
addition, previous studies found that after rTMS APOE
Our results suggest that rTMS may decrease the serum levels of A
YT and BL—study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript; YZ, XF—study concept and design, acquisition of data; LL, DC—acquisition of data, analysis and interpretation of data; CG—study concept and design, study supervision, critical revision of manuscript for intellectual content.
This study was approved by the Institutional Review Board of Chongqing Daping Hospital, and all of the participants and their caregivers provided written informed consent. Ethical approval number of our study (Medical research ethics review (2018) No. 127).
We would like to express our gratitude to all those who helped us during the writing of this manuscript. Thanks to all the peer reviewers for their opinions and suggestions.
This study was supported by project of Army Medical University: Military Medical pre Research Fund (2017XYY05).
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
