1 Department of Psychiatry, Beijing Children’s Hospital, Capital Medical University, National Center for Children Healthy, 100101 Beijing, China
2 Department of Medical Psychology, the First Medical Center, Chinese PLA General Hospital, 100853 Beijing, China
†The first two authors contribute equally.
Academic Editor: Rafael Franco
Abstract
Background: Exposure and response prevention (ERP) is a form of
cognitive behavioral therapy that can effectively relieve obsessive-compulsive
symptoms and tic symptoms in patients with obsessive-compulsive disorder (OCD)
and Tourette syndrome (TS). However, the effect size of ERP-based therapy is
still unclear. Methods: In this study, we performed a meta-analysis to
identify the efficacy of ERP-based therapy for individuals with OCD and TS. The
standard mean difference (SMD) with a 95% confidence interval (CI) was
calculated to assess the effect size of the efficacy for ERP-based therapy. We
used subgroup and meta-regression analyses to explore the heterogeneity of the
pooled SMD of ERP-based therapy for OCD. We also summarized the neuroimaging
studies for ERP-based therapy for OCD. This meta-analysis was registered within
the International Platform of Registered Systematic Review and Meta-analysis
Protocols (number: INPLASY2021120112). Results: A total of 18 studies
including a total of 1057 patients with OCD and 3 studies including 267 with
TS/chronic tic disorder were identified. We did not observe any indication of
publication bias using Egger’s funnel plot (p = 0.41). We observed a
small-to-medium effect size of ERP for both OCD (SMD = –0.27, 95% CI: –0.53 to
–0.01) and TS/chronic tic disorder (SMD = –0.35, 95% CI: –0.59 to –0.1). We
found no heterogeneity of ERP-based therapy for OCD between the ERP-based therapy
subgroup and medicine subgroup in the subgroup analysis (p = 0.72). We
found no heterogeneity of ERP-based therapy for OCD between the child subgroup
and adult subgroup in the subgroup analysis (p = 0.37). We used
meta-regression analysis to identify the heterogeneity of ERP-based therapy for
OCD and found that the sessions of therapy and publication year did not account
for any significant heterogeneity (p
Keywords
- exposure and response prevention
- cognitive behavioral therapy
- obsessive-compulsive disorder
- tourette syndrome
- tic disorders
- meta-analysis
Obsessive-compulsive disorder (OCD) is a chronic psychiatric disorder characterized by distressing and time-consuming obsessions and compulsions [1]. Obsessions are defined as intrusive and unwanted thoughts, urges, or images, and they are followed by compulsions, which aim to relieve these “uncomfortable feelings” [1, 2]. It has been reported that the lifetime prevalence of OCD is approximately 1%–3% [3, 4]. Patients are often affected by obsessions and compulsions that interfere with social, at home, educational attainment, and occupational aspects [1, 5].
Exposure and response prevention (ERP) is based on cognitive behavioral therapy (CBT) and is the primary psychological treatment for OCD in children, adolescents, and adults [6, 7, 8, 9, 10]. ERP involves exposure to feared obsessional stimuli while refraining from engaging in compulsive behaviors [11]. Research indicates that approximately 60%–85% of patients who complete ERP treatment achieve significant success in alleviating obsessive-compulsive symptoms [4, 12, 13]. Moreover, CBT (including ERP) is recommended as the first-line treatment for mild-to-moderate OCD in youth [14]. Although serotonin reuptake inhibitors (SRIs) are effective in reducing symptoms compared with placebo, only moderate effect sizes are found when compared to CBT (including ERP) [9, 15]. Recently, it was reported that the patient dropout rate for ERP was 10.24%, whereas the patient dropout rate for pharmacotherapy was 17.29% [16]. Interestingly, the same study found that patients who did not respond to SRI augmentation with risperidone or placebo showed significant reductions in OCD symptoms and depression when treated with ERP, as well as better quality of life and social functioning [17]. However, ERP-based CBT has no or only partial improvement for many young patients with OCD. For example, one study found that 60% of patients in an ERP-based CBT condition failed to demonstrate clinical remission in a large RCT for children and adolescents with OCD [18]. Although approximately 60% of patients who completed treatment improved, only 25% of patients were asymptomatic [19]. This suggests that most patients treated with ERP continue to experience OCD symptoms [20]. Based on these studies, the quantitative degree of efficacy of ERP is still unclear, and the factors influencing ERP need to be explored.
Previous research has focused on the neuroimaging findings of OCD. Some studies have indicated that brain function changes pre- and post-ERP-based therapy. A recent study found that OCD patients showed less inhibition-related activation in areas of the frontoparietal cortex, dorsal anterior cingulate cortex (ACC) and anterior insula than controls [21]. Stein et al. [22] found that OCD is associated with subtle alterations in cortico-striato-thalamo-cortical, fronto-parietal, and frontolimbic circuits. Few studies have focused on the neurological mechanism of ERP-based therapy for OCD patients [23]. Because of inconsistencies in the changes after interventions [24, 25], we surveyed neuroimaging studies of ERP-based interventions for OCD and summarized them in a systematic review.
Furthermore, ERP is applied not only in patients with OCD but also in patients with Tourette syndrome (TS). TS is characterized by sudden motor movements and/or vocalizations (referred to as tics) for at least 12 months [26]. It has been reported that the worldwide prevalence of TS is nearly 1% [27]. TS and OCD often co-occur. They share common dysfunction in symptoms profiles [28] and pathophysiology [29]. The development of ERP for OCD might benefit the ERP for TS. Indeed, ERP has also been recommended as a first-line behavioral therapy in American, Canadian and European guidelines for tic disorders [30, 31, 32]. However, the efficacy of ERP for TS needs to be clarified. We can investigate the efficacy of ERP for both OCD and TS which might give us more indications for the development of ERP across different mental disorders.
Several studies on the meta-analysis of CBT for OCD have been conducted [6, 33, 34, 35]. However, the efficacy of ERP-based therapy for OCD & TS is still unclear. This meta-analysis aimed to find the effect sizes of ERP for OCD & TS. A meta-analysis method provides the opportunity to statistically combine the results of comparable trials [36]. Therefore, in the current meta-analysis, we attempted to identify the efficacy of ERP-based therapy (which included the ERP as the main procedure) for OCD & TS. We used meta-regression and subgroup analyses to determine potential heterogeneities in these approaches.
An extensive literature search was conducted in the following databases: PubMed, Web of Science, PsycINFO, and Google Scholar. We only considered studies published before November 1, 2021. The search terms were as follows: “obsessive-compulsive disorder” or “OCD” or obsessive/compulsive” or “Tourette’s syndrome” or “tics” or “tic disorders” and “cognitive behavior therapy” or “exposure and response” or “exposure and ritual prevention” or “ERP” or “EX/RP” or “psychotherapy” and “magnetic resonance imaging” or “MRI”. References of related articles were also searched for any other relevant studies.
Inclusion criteria were as follows:
(1) ERP or ERP-based therapy;
(2) The symptoms of OCD measured by a validated scale, such as the Yale-Brown Obsessive-Compulsive Symptom Scale (Y-BOCS) [37] or the Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) [38], and the Yale Global Tic Severity Scale (YGTSS) were used to assess the tic symptoms;
(3) Y-BOCS/CY-BOCS or YGTSS was used to assess the efficacy of ERP or ERP-based therapy;
(4) Both adult and child/adolescent OCD and tic disorder patients were included; and
(5) written in English.
Exclusion criteria were as follows:
(1) No Y-BOCS/CY-BOCS data or YGTSS data;
(2) Studies combining ERP with another type of behavioral therapy;
(3) Articles with duplicate records; and
(4) Articles such as case reports, editorials, comments, and review papers.
Notably, the Y-BOCS/CY-BOCS score range of severity for patients who have both
obsessions and compulsions was categorized as follows: mild OCD (
The quality of each study was assessed by the modified Jadad scale [39]. Each study was evaluated by using the following criteria: randomization, blinding strategy, withdrawals/dropouts, inclusion/exclusion criteria, adverse effects, and statistical analysis. Two authors independently scored each included trial and discussed with each other to reach a consensus on any differences.
We identified a total of 18 studies including 1057 patients diagnosed with OCD. Three studies including 267 patients diagnosed with TS/chronic tic disorder were included. Both children and adults patients were included. We extracted the following information from the included studies: authors, publication years, mean ages, numbers of males/females, sample sizes, diagnostic criteria, comparison group, online or face to face, in vivo/imaginal exposure, outcome measurements, the baseline Y-BOCS/CY-BOCS value and YGTSS value, and the number of therapy sessions.
A randomized effects model was used to examine the standard mean difference
(SMD) of ERP-based therapy. If the SMD was between 0.2 and 0.5, the efficacy of
ERP-based therapy was mild-to-moderate, whereas SMD values between 0.5 and 0.8
indicated that the efficacy of ERP-based therapy was moderate-to-large [40].
I
Based on the inclusion and exclusion criteria, a total of 18 studies were identified for OCD and 3 studies for TS. For the flowchart to identify the included studies, see Fig. 1. We list the extracted data in the Table 1 (Ref. [18, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61]). The quality assessment for the included studies was summarized in Table 2 (Ref. [18, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61]).
| Author | Published year | Age (years) | Male/Female | Diagnosis criteria | Sample size | Comparison group | Online or face to face | In vivo/imaginal exposure | Outcome measurements | Baseline Y-BOCS/CY-BOCS or YGTSS | Sessions |
| Hwang et al. [43] | 2021 | ERP: 24.7 |
11/16 | DSM-5 | 27 | OCfree CBT | Face to Face | N/A | Y-BOCS, BDI, BAI | ERP: 19.5 |
6 sessions/6weeks |
| Norman et al. [44] | 2021 | ERP: 24.23 |
30/57 | N/A | 87 | SMT | Face to Face | N/A | Y-BOCS, QIDS, CGI-S, HAM-A | ERP: 25.10 |
12 sessions/12 weeks |
| Kobayashi et al. [45] | 2020 | ERP: 29.44 |
9/8 | DSM-IV | 17 | TAU | Face to Face | N/A | Y-BOCS, PGI-S, CGI-S, BDI, K6, SDS, EQ5D, FAS-PV, FAS-SR | ERP: 26.67 |
16 sessions/16 weeks |
| Kyrios et al. [46] | 2018 | ERP: 32.59 |
61/117 | DSM-IV-TR | 178 | iPRT | Online | N/A | Y-BOCS, GAF, HAM-D, HAM-A | EPR: 22.58 |
12 sessions/12 weeks |
| Peris et al. [47] | 2017 | ERP: 13.66 |
35/27 | DSM-IV-TR | 62 | PFIT | Face to Face | N/A | CY-BOCS, CGI-I, COIS-RP, FAS, FES, PABS | ERP: 25.43 |
12 sessions/12 weeks |
| Marsden et al. [48] | 2017 | EPR: 33.31 |
21/34 | DSM-IV | 55 | EMDR | Face to Face | Both | Y-BOCS, OCI, PHQ-9, GAD-7, WSAS | ERP: 26.65 |
16 sessions/16 weeks |
| Foa et al. [49] | 2015 | EX/RP: 34.47 |
17/21 | DSM- IV | 38 | RIS | Face to Face | N/A | Y-BOCS, HDRS | ERP: 27.5 |
17 sessions/8 weeks |
| Foa et al. [50] | 2013 | EX/RP: 36.1 |
34/15 | DSM-IV | 49 | SSRI | Face to Face | N/A | Y-BOCS, HDRS, HARS, Q-LES-Q, SAS-SR | ERP: 25.1 |
16 sessions/8 weeks |
| Hoexter et al. [51] | 2013 | ERP: 33.3 |
11/18 | DSM-IV | 29 | Fluoxetine | Face to Face | N/A | Y-BOCS, DY-BOCS, BDI, BAI | ERP: 27.3 |
12 sessions/12 weeks |
| Belotto-Silva et al. [52] | 2012 | E/RP: 33.94 |
71/87 | DSM-IV | 158 | SSRI | Face to Face | N/A | Y-BOCS | ERP: 25.97 |
12 sessions/12 weeks |
| Connor et al. [53] | 2005 | 38.3 | 16/28 | DSM-IV | 44 | CAM | Face to Face | In vivo | Y-BOCS, Padual, CIQ, BAI, BDI | ERP: 19.2 |
20 sessions/20 weeks |
| Whittal et al. [54] | 2005 | ERP: 34.24 |
22/37 | DSM-IV | 59 | CBT | Face to Face | N/A | Y-BOCS, BDI | ERP: 21.66 |
12 sessions/12 weeks |
| Foa et al. [42] | 2005 | ERP: 33.8 |
19/46 | DSM-IV | 65 | CLOM | Face to Face | Both | Y-BOCS, CGI | ERP: 24.6 |
12 sessions/12 weeks |
| Nakatani et al. [55] | 2005 | E/RP: 32.5 |
6/14 | DSM-III-R | 20 | FLV | Face to Face | N/A | Y-BOCS, CGI-I, CGI-S, GAF, HAM-A/D | E/RP: 29.9 |
12 sessions/12 weeks |
| POTS [18] | 2004 | ERP: 11.4 |
31/25 | DSM-IV | 56 | Sertraline | Face to Face | N/A | CY-BOCS, CGI | ERP: 26.0 |
14 sessions/12 weeks |
| de Haan et al. [56] | 1998 | ERP: 13.25 |
11/11 | DSM-III-R | 22 | CLOM | Face to Face | N/A | CY-BOCS, LOI-CV | ERP: 21.5 |
12 sessions/12 weeks |
| van Balkom et al. [57] | 1998 | ERP: 13.25 |
17/19 | DSM-III-R | 38 | CT | Face to Face | In vivo | CY-BOCS, BDI, SCL-90 | ERP: 25.0 |
16 sessions/16 weeks |
| de Haan et al. [58] | 1997 | N/A | N/A | DSM-III-R | 47 | Cognitive | Face to Face | N/A | Y-BOCS, SCL-90, BDI | ERP: 24.7 |
16 sessions/16 weeks |
| Hollis et al. [59] | 2021 | ERP: 12.2 |
177/47 | N/A | 224 | Psychoeducation | Online | N/A | YGTSS, TTSS, C&A-GTS-QOL | ERP: 28.4 |
N/A |
| Andrén et al. [60] | 2018 | HRT 12.79 |
15/8 | DSM-5 | 23 | HRT | Online | N/A | YGTSS, CGAS, PUTS, GTS-QOL, PTQ | ERP: 23.75 |
10 sessions/10 weeks |
| Verdellen et al. [61] | 2004 | HRT: 19.2 |
34/9 | DSM-IV | 43 | HRT | Face to Face | N/A | YGTSS, TF-institute, TF-home | ERP: 26.2 |
10 sessions |
| Abbreviations: ERP, exposure and response prevention; EX/RP, Exposure and Ritual Prevention; iPRT, internet-based progressive relaxation therapy; TAU, treatment as usual; Y-BOCS, Yale-Brown Obsessive Compulsive Scale; QIDS, Quick Inventory of Depressive Symptomatology; PGI, Patient Global Impression; K6, Kessler Psychological Distress Scale; SDS, Sheehan Disability Scale; EQ5D, EuroQol; FAS-SR, Family Accommodation Scale for OCD Self-Rated version; FAS-PV, Family Accommodation Scale for OCD Patient-Rated version; GAF, Global Assessment of Functioning; HAM-D, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale; PFIT, Positive Family Interaction Therapy; CY-BOCS, Children’s Yale-Brown Obsessive Compulsive Scale; CGI-I,Clinical Global Impression Scale – Improvement; COIS-RP, Child Obsessive-Compulsive Disorder (OCD) Impairment Scale – Parent-Report Revised; FAS, Family Accommodation Scale; FES, Family Environment Scale; PABS, Parental Attitudes and Behaviors Scale; EMDR, eye movement desensitization and reprocessing; OCI, obsessive compulsive inventory; PHQ-9, measure of depression symptoms; GAD-7, measure of anxiety symptoms; WSAS, work and social adjustment scale; RIS, Risperidone; HDRS, Hamilton Depression Rating Scale; SMT, Stress Management Training; HARS, Hamilton Anxiety Rating Scale; Q-LES-Q, Quality of Life Enjoyment and Satisfaction Scale; SAS-SR, Social Adjustment Scale-Self Report; DY-BOCS, Dimensional Yale–Brown Obsessive–Compulsive Scale; BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory; CGI, Clinical Global Impressions; E/RP, exposure with response prevention; SSRI, selective serotonin reuptake inhibitor; CAM, Cognitive Appraisal Model; IBA, Inference-based Approach; Padua, Padua Inventory; CIQ, Cognitive Intrusions Questionnaire; CLOM, Clomipramine; FLV, Fluvoxamine; CGI-S, Clinical Global Impressions-Severity of Illness Scale; LOI-CV, Leyton Obsessional Inventory-Child Version; SCL-90, Symptom Check-list; Cognitive, cognitive therapy; Psy, Psychoeducation; HRT: Habit reversal therapy; TTSS, Total Tic Severity Score; C&A-GTS-QOL, Child and Adolescent Gilles de la Tourette Syndrome–Quality of Life Scale; TF-institute, tic frequency observed at the institute; TF-home, tic frequency monitored at home. | |||||||||||
| First author | Published year | Was the research described as randomized? | Was the approach of randomization appropriate? | Was the research described as blinding? | Was the approach of blinding appropriate? | Was there a presentation of withdrawals and dropouts? | Was there a presentation of the inclusion/exclusion criteria? | Was the approach used to assess adverse effects described? | Was the approach of statistical analysis described? | Total |
| OCD | ||||||||||
| Hwang et al. [43] | 2021 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Norman et al. [44] | 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Kobayashi et al. [45] | 2020 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Kyrios et al. [46] | 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Peris et al. [47] | 2017 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Marsden et al. [48] | 2017 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 4 |
| Foa et al. [49] | 2015 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Foa et al. [50] | 2013 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Hoexter et al. [51] | 2013 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Belotto-Silva et al. [52] | 2012 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 6 |
| Connor et al. [53] | 2005 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 4 |
| Whittal et al. [54] | 2005 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 6 |
| Foa et al. [42] | 2005 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Nakatani et al. [55] | 2005 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| POTS [18] | 2004 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| de Haan et al. [56] | 1998 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| van Balkom et al. [57] | 1998 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| de Haan et al. [58] | 1997 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| TS | ||||||||||
| Hollis et al. [59] | 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Andrén et al. [60] | 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Verdellen et al. [61] | 2004 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
 Fig. 1.
Fig. 1.Flow chart of the included studies. ERP, exposure and response prevention; OCD, obsessive-compulsive disorder; Y-BOCS, the Yale-Brown Obsessive-Compulsive Scale; CY-BOCS, the Children’s Yale-Brown Obsessive-Compulsive Scale; YGTSS, the Yale Global Tic Severity Scale.
The pooled SMD of ERP-based therapy for OCD was –0.27 (95% CI: –0.53 to
–0.01), with a heterogeneity (I
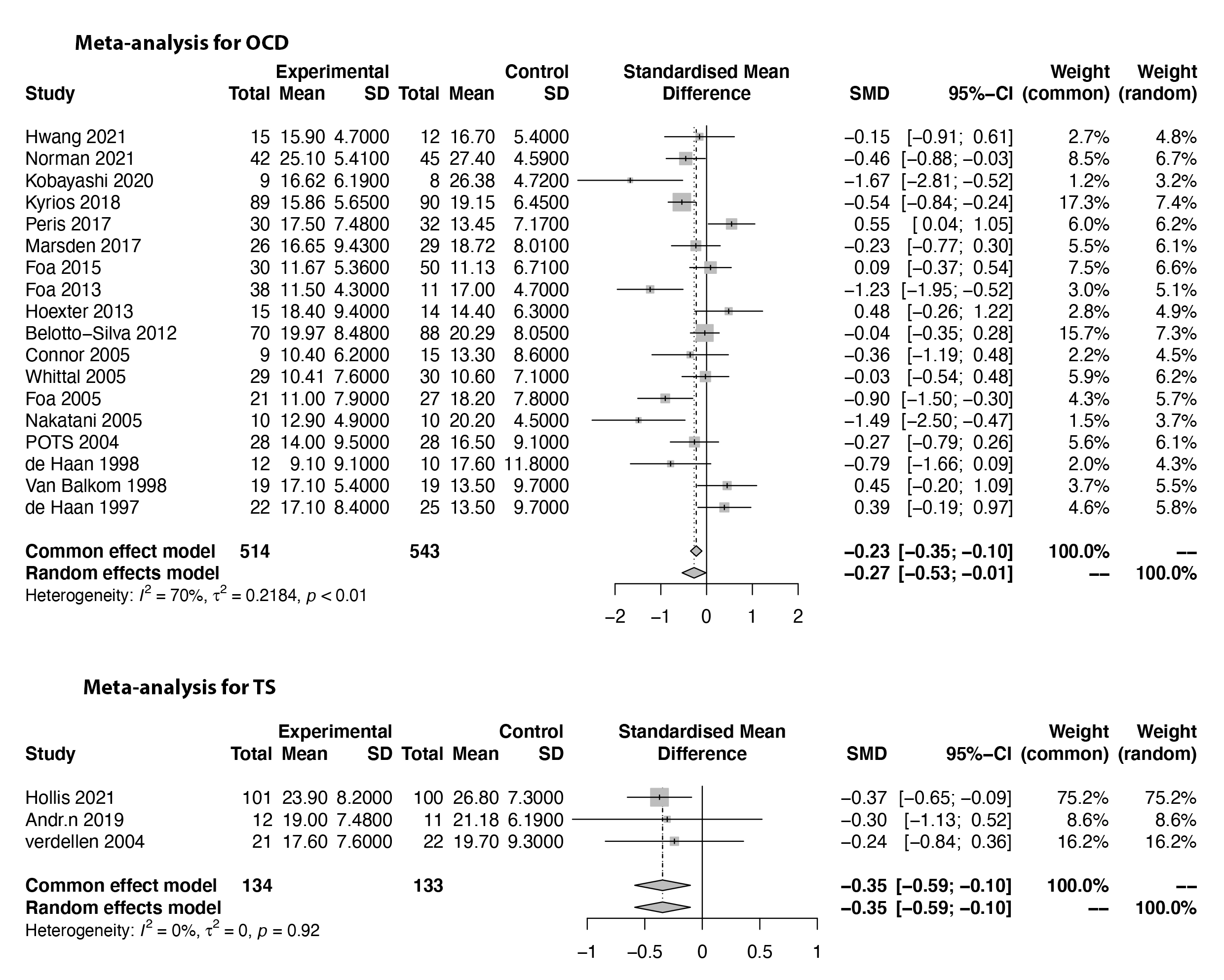 Fig. 2.
Fig. 2.Forest plots of the meta-analysis of efficacy for ERP-based therapy for OCD and TS.
We used sensitivity analysis to explore the heterogeneity of the pooled SMD of
ERP-based therapy for OCD. This method omits one study at a time and tracks the
change in I
A subgroup analysis of the pooled SMD of ERP-based therapy for OCD was conducted
to identify the potential source of heterogeneity by different comparison groups
and different age groups. Furthermore, we found no heterogeneity of ERP for OCD
between different comparison groups (p = 0.72) (Fig. 3). For the
subgroup analysis of the different age groups, heterogeneity was found in both
adults (I
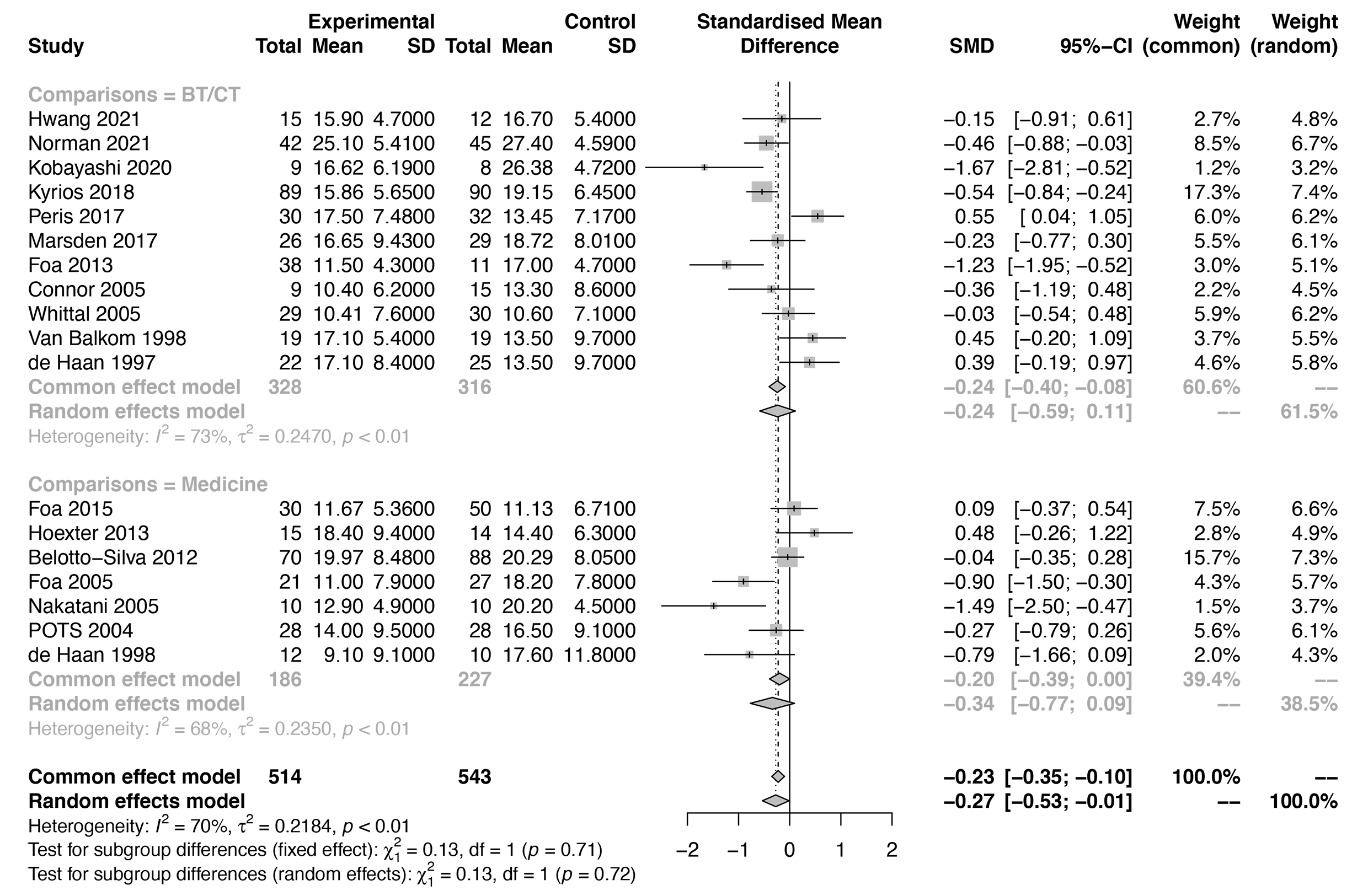 Fig. 3.
Fig. 3.Forest plots of the subgroup analysis by different comparisons for the efficacy of ERP-based therapy (medicine and BT/CT).
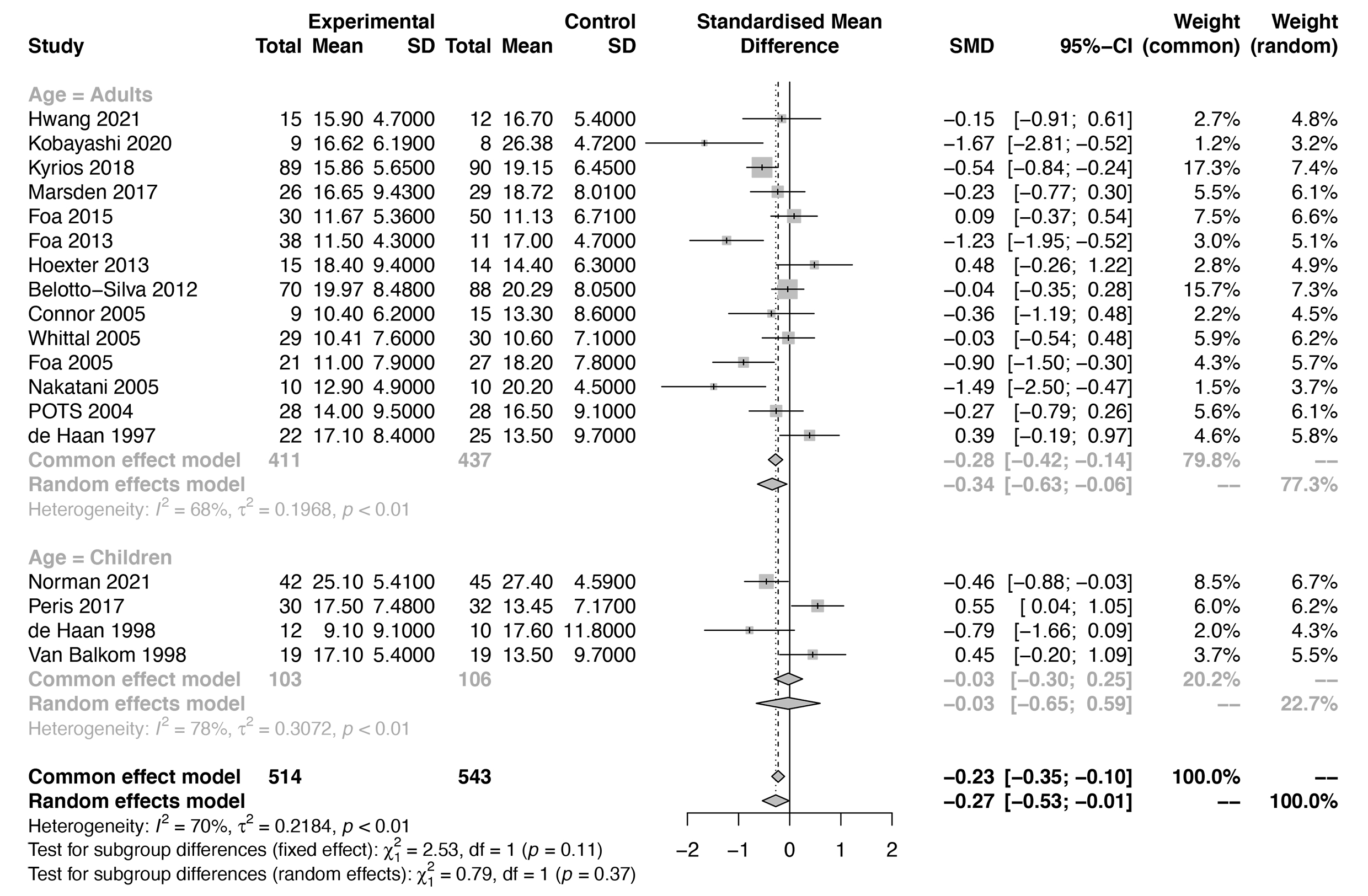 Fig. 4.
Fig. 4.Forest plots of the subgroup analysis by age group for the efficacy of ERP-based therapy (adults and children).
We conducted a meta-regression analysis to explore the heterogeneity of pooled
SMD of ERP-based therapy for OCD. The sessions of therapy and publication year
did not account for any significant heterogeneity (p
| Predictors | tau |
I |
H |
R |
The test of moderators (p) |
| Publication year | 0.237 | 75.37% | 4.12 | 0.00% | 0.608 |
| Session | 0.240 | 76.35% | 4.23 | 0.00% | 0.998 |
| Note: tau | |||||
Differences in the involved brain areas after ERP interventions between OCD patients and control subjects were detected. Within the ERP group, after-treatment response was significantly associated with greater pretreatment activation within the medial prefrontal and amygdala regions, as well as connectivity increases between the cerebellum and caudate/putamen and between the cerebellum and prefrontal cortices after interventions. Studies about the involved brain areas of ERP for TS were not found. For more details see Table 4 (Ref. [44, 51, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72]).
| Studies | Year | M/F ratio OCD | M/F ratio controls | Mean age of OCD patients | Mean age of controls | Involved brain areas |
| Cyr et al. [63] | 2021 | 12/13 | 11/12 | 12.76 (2.92) | 11 (3.27) | lateral amygdala/ventromedial prefrontal cortex |
| Norman et al. [44] | 2021 | 14/28 | 16/29 | 24.23 (9.13) | 24.51 (9.32) | the right temporal lobe/rostral anterior cingulate cortex/ventromedial prefrontal/orbitofrontal/lateral prefrontal/amygdala |
| Cao et al. [64] | 2021 | 22/12 | 27/23 | 18–50 | 28.48 (6.19) | the left lingual gyrus/left middle temporal gyrus/left precuneus/left fusiform gyrus |
| Pagliaccio et al. [65] | 2020 | 14/14 | 14/13 | 12.14 (3.34) | 11.26 (3.23) | middle and superior frontal/angular/lingual/precentral/ superior temporal/supramarginal gyri |
| Thorsen et al. [66] | 2020 | 12/19 | 8/18 | 30.19 (9.21) | 31 (10.73) | the right inferior frontal gyrus/the right amygdala/the right inferior frontal gyrus/the pre-supplementary motor area/supplementary motor area |
| Cyr et al. [67] | 2020 | 12/13 | 11/12 | 12.8 (2.9) | 11.0 (3.3) | left angular gyrus and left frontal pole/frontoparietal/ventral attention/cingulo-opercular/right putamen/posterior insula and posterior insula (auditory network) |
| Moody et al. [68] | 2017 | 22/21 | 14/10 | 33 (10.7) | 31 (12.0) | the cerebellum/caudate/putamen/dorsolateral/ventrolateral prefrontal |
| Göttlich et al. [69] | 2015 | 5/12 | 4/15 | 32.6 (11.6) | 30.4 (9.6) | amygdala/superficial amygdala |
| Olatunji et al. [70] | 2014 | 6/6 | - | 32.25 (9.9) | - | anterior temporal pole/amygdala/dorsolateral prefrontal |
| Huyser et al. [71] | 2013 | 5/12 | 6/14 | 13.8 (2.8) | 14.6 (2.6) | orbitofrontal |
| Hoexter et al. [51] | 2013 | 5/10 | 6/8 | 33.3 (10.0) | 33.1 (11.6) | right medial prefrontal |
| Freyer et al. [72] | 2011 | 7/3 | 6/4 | 36.1 (9.36) | 39.6 (10.48) | orbitofrontal cortex/right putamen/the caudate nucleus/pallidum |
| Note: OCD, Obsessive-Compulsive Disorder; M/F, males/females. | ||||||
In addition to the relief of clinical core symptoms after ERP, functional recovery is also something we need to discuss. For OCD patients, ERP can help improve family functioning, which including levels of family accommodation and psychological distress. Therefore, we summary the related studies which also report the functional recovery of ERP in Supplementary Table 1. These results indicated that the ERP might also improve the patients’ social function.
In this study, we conducted a meta-analysis to identify the efficacy of ERP-based therapy for OCD and TS/chronic tic disorder. A small-to-moderate effect size of ERP-based therapy was found in the experimental groups compared to the control groups. The effect sizes were comparable with the medicine (i.e., risperidone, fluoxetine, clomipramine, and sertraline) and other behavior therapies. The results indicate that ERP-based therapy can be effective in alleviating obsessive-compulsive symptoms and tic symptoms.
In the present study, we found that ERP-based therapy for OCD can be applied in
both adults and children. For example, in a randomized controlled trial,
ERP-based therapy alone does not differ from sertraline alone (p = 0.24)
after 12 weeks of treatment in OCD patients aged 7 through 17 years [18]. For
adult patients with OCD, ERP is comparable to first-line pharmacological
treatments (e.g., SRIs) [11]. However, to determine whether ERP-based therapy for
OCD shows differences between children and adults, more studies including
different age groups are needed in the future. Moreover, it should be noted that
the I
Currently, modifications of CBT formats, such as CBT augmented with d-cycloserine [73], internet-delivered treatments [74], video teleconferencing methods [75], and Bergen 4-day treatment (B4DT) [76], are also used in OCD patients. The modifications of ERP programs based on different individual needs may require further investigation in the future. Many patients with OCD have no access to ERP [77], and possible barriers include clinician-related factors, aspects of the phenomenology of OCD, willingness to experience unpleasant sensations during ERP, financial barriers, and geographical factors [78, 79]. Several options for accessing online CBT have been developed to make it easier to access this treatment [80, 81], but further research is needed to extend the reach of ERP online. Furthermore, more research is needed regarding the long-term efficacy of ERP, as longer treatment durations may yield reduced OCD symptoms. The potential benefits of the combination of behavioral therapy and pharmacotherapy are also required to help patients not responsive to monotherapy or with severe OCD.
In this study, we found evidence to support the efficacy of ERP-based therapy for reducing obsession-compulsion symptoms. Behavioral therapy and SRIs were found to be comparable in improving the symptoms in adults with OCD [6, 7], and ERP also exhibited efficacy for reducing tic symptoms. It appears that the mechanisms that underlie the treatment of OCD and tic disorders are similar to some extent. Indeed, OCD and TS overlap in many aspects, such as their clinical phenomenology and tendency to co-occur in affected individuals. A tic-related OCD subtype in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) may occur in 10%–40% of patients diagnosed with childhood OCD [1, 82], and approximately 25%–50% of patients with TS meet the criteria for OCD [83, 84]. Similarly, approximately 30% of patients with OCD have a history of combined TS [85, 86]. Both animal studies and neuroimaging studies suggest that abnormal function of cortical basal ganglia circuitry results in tics and compulsive behaviors [87, 88, 89]. Abnormalities of the dopaminergic system may be the common pathophysiologic mechanism of TS and OCD [90], and based on these similarities, it is perhaps not surprising that ERP was not only effective for mild-to-moderate OCD and TS/chronic tic disorder but may also be a promising behavior therapy for the tic-related OCD subtype.
Patients with tic disorder are trained to endure premonitory urges (PUs), or “uncomfortable bodily feelings”, a longing to make things “just right” [91, 92] to suppress tic symptoms in ERP. The long period exposed to the unpleasant sensation and to resist the tic symptoms, the patients will learn to endure the sensation [30]. Habit reversal therapy (HRT) is another form of CBT that is effective for the treatment of tic disorder and includes awareness training, relaxation training, and competing-response training as its core procedures. ERP and HRT are both recommended as first-line behavioral treatments for tic disorder [30, 31, 93], and the combination of the two may be a new direction for behavior therapy in the future. In addition, ERP has also been applied to anorexia nervosa, body dysmorphic disorder, anxiety disorder, hypochondriasis, and repetitive behaviors in autism [8, 94, 95, 96, 97, 98]. ERP (unlike medication) has essentially no untoward effects and that benefits of ERP are typically retained after termination of treatment. And more follow-up studies are needed in the future.
The neurological mechanism of the effectiveness of EPR is unclear, but it may lie in changes in the prefrontal cortex and anterior cingulate cortex (ACC). A prior study found that the volume of gray matter within the medial prefrontal cortex was correlated with the response to ERP-based CBT in OCD patients [51]. A study found that with intensive ERP-based CBT, the degree of improvement in OCD symptoms significantly increases in right dorsal ACC activity and decreases in bilateral thalamic activity [99]. OCD patients who respond to exposure therapy have thinner rostral ACC than those who do not [100]. Greater conflict-related activity in the anterior insula and anterior and posterior cingulate predicted a greater ERP response in OCD patients [65]. Some associations between brain activation and treatment response were specific to ERP-based CBT [44]. More studies are needed to research the neurological mechanism of ERP for OCD and other psychiatric diseases.
Additionally, study found that the family-based ERP might also help to improve family functioning and quality of life, social functioning [45]. Likewise, TS patients had better quality of life in the ERP group than psychoeducation group at 3 months [59]. We might need more evidence for this dimension of ERP in future studies.
Several limitations are needed to be noted. First, the included studies and sample size were limited, which might reduce the credibility of the results. Second, the validated scales for OCD were restricted to widely used scales of Y-BOCS and CY-BOCS, and the studies that applied the other scales were not included. Third, the studies included not only ERP but also ERP-based therapy, which might increase the heterogeneity of the data. Despite these limitations, this study provided evidence of the treatment effect of ERP on OCD & TS.
In summary, we identified a small-to-medium effect size of ERP-based therapy to relieve obsessive-compulsive symptoms and tic symptoms. We suggest that combining ERP with other therapies and online services might be an ideal direction for ERP in the future. The prefrontal cortex and ACC might have associations with the neurological mechanism of the ERP.
ERP, Exposure and response prevention; CBT, Cognitive behavioral therapy; OCD, Obsessive-compulsive disorder; TS, Tourette syndrome; SMD, standard mean difference; CI, Confidence interval; SRIs, Serotonin reuptake inhibitors; Y-BOCS, Yale-Brown Obsessive-Compulsive Symptom Scale; CY-BOCS, Children’s Yale-Brown Obsessive-Compulsive Scale; BT/CT, Behavior therapy/cognitive therapy; HRT, Habit reversal therapy; PUs, premonitory urges; MRI, Magnetic Resonance Imaging.
For this manuscript, YC and YL took the initiative. MW finished the data collection. YL performed the data analysis and JY and LC finished the draft.
Not applicable.
Thanks very much for the support of the Pediatric Medical Coordinated Development Center of Beijing Hospitals Authority.
This work was supported by the National Natural Science Foundation of China (NSFC) under Grant No. 82171538 and the Beijing Natural Science Foundation under Grant No. 7212035.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.jin2103097.




