1 Laboratory of Toxicology & Pharmacology, Department of Biochemistry, Faculty of Science, University of Yaounde 1, BP 812 Yaounde, Cameroon
2 Division of Food Safety and Health, Agri-Food Safety and One Health Agency (AFS1HA), Yaounde, Cameroon
Abstract
Foods are frequently contaminated by natural toxins or toxic substances that have been illegally added, some of which are carcinogenic and pose potential cancer risks to consumers, particularly in low- and middle-income countries. This scoping review maps commonly reported food carcinogens and summarizes existing evidence on the role of these additives as risk factors for various cancers, such as breast, liver, lung, stomach, and colorectal (BLLSCr) cancers. Key findings highlight naturally occurring carcinogenic food contaminants (e.g., aflatoxins, heavy metals, bisphenol A, pesticide residues, polycyclic aromatic hydrocarbons (PAHs) from food processing) and economically motivated adulterants (e.g., Sudan dyes in palm oil, formaldehyde in meat) that frequently contaminate staple foods. There is evidence that these contaminants serve as a risk factor for certain cancers, especially BLLSCr cancers. Moreover, gender and socioeconomic disparities influence cancer prevalence, with men at higher risk for liver, lung, and gastric cancers, while breast cancer incidence rises among women in high-income settings. This review highlights two major contamination pathways: natural toxins and economically motivated adulterants. Meanwhile, strategies to prevent or control/reduce food contamination and associated dietary exposures to these carcinogens have been proposed. Exposure to nutritional carcinogens, as drivers of BLLSCr cancers, represents a food safety and public health challenge globally.
Keywords
- adulterants
- cancer risk factors
- food contaminants
- dietary exposure
- cancer incidence
Cancer is among the leading causes of death, and its burden continues to increase globally. According to the American Cancer Society (ACS), cancer caused an estimated 10 million deaths globally in 2020, making it the second leading cause of death [1]. Several factors, including genetics, lifestyle, and environmental factors, all contribute to the development of cancer. Of these factors, diet and exposure to dietary carcinogens have been identified as important contributors to cancer development. Dietary carcinogens are substances that are present in certain foods and can increase the risk of cancer when consumed in high amounts [2]. For example, cheese, dried fruits, and beer have been associated with the risk of lung cancer in China [3]. Furthermore, dietary polycyclic aromatic hydrocarbons (PAHs) have been linked to an increased risk of liver and lung cancer in China [4, 5].
Despite increasing recognition of dietary carcinogens, significant gaps persist in understanding their global prevalence, exposure pathways, and population-specific health impacts. Low- and middle-income countries (LMICs), such as Cameroon, Indian, Pakistani face heightened risks due to lax regulatory enforcement, limited food safety infrastructure, and socioeconomic disparities that amplify exposure, e.g., reliance on aflatoxin-contaminated staples [6, 7]. Additionally, the diversity of carcinogens from naturally occurring, e.g., mycotoxins such as aflatoxin B1, to the economically motivated adulterants (e.g., Sudan dyes) in food have been associated with different types of cancers [8] which might complicates risk assessment and mitigation. Existing studies often focus on isolated contaminants or regions, leaving a fragmented picture of their cumulative effects and interactions with other cancer drivers (e.g., hepatitis B and aflatoxin synergy in liver cancer) [9, 10].
This scoping review addresses these gaps by systematically mapping frequently reported dietary carcinogens and synthesizing evidence of their associations with breast, liver, lung, stomach and colorectal (BLLSCr) cancers. By categorizing contaminants into natural (e.g., PAHs, heavy metals) and intentional adulterants (e.g., formaldehyde, Sudan dyes), we provide an actionable framework for policymakers and public health practitioners [11]. The findings from this scoping review underscore the dual burden of food safety and cancer prevention in LMICs while proposing targeted strategies (that spans from regulatory reforms to consumer education) to reduce exposure. Furthermore, this work provides vital information to bridge critical knowledge gaps and advocates for integrated interventions to mitigate dietary cancer risks globally.
The current desk-based scoping review paper has exploited existing literature on carcinogenic food contaminants and various diet-related cancers. It did not restrict the food carcinogen source whether as natural food contaminants or as illegally added, i.e., (adulteration or food fraud). Additionally, it concentrated on dietary carcinogens that may constitute risk factor/s for various types of cancer. The quality of each existing study of interest was not rigorously weighed. The review was conducted using data obtained from online publications on search engines and databases such as PubMed, Google Scholar, Web of Science, and Scopus. Keywords such as cancer, cancer risk factors, dietary carcinogens, food contaminants, and food adulterants were used to search. The reference lists of the relevant articles were searched manually and all other cited studies were reviewed and analyzed accordingly alongside the initially identified relevant studies. The inclusion criteria for the studies were: published in the English language, reported on dietary carcinogens and or diet-related cancer, and published between 2000 and 2024. When necessary, tables and figures were added to the narrative presentation of the results.
The current desktop-based study that has reviewed and summarized evidence from existing literature focused on food contaminant-related cancer prevalence in Cameroon, as well as natural and or intentionally added carcinogenic contaminants in foods that may serve as risk factors for cancer. According to this scoping review, there is a correlation between some dietary carcinogens and some cancers such as liver and breast cancers. This was as expected when considering the Expert Report of the World Cancer Research Fund and the American Institute for Cancer Research (World Cancer Research Fund (WCRF) International) which confirms diet as a risk factor for various types of cancers. Dietary carcinogens may come in contact with our foods in a variety of ways such as non-compliant food additives, natural food contaminants, food adulterants, and or formed from food components [12]. Some of the dietary carcinogens revealed in this study include aflatoxins, heterocyclic amines, PAHs, nitrosamines, heavy metals, pesticide residues, Sudan dye IV, formaldehyde, formalin, and lead. Although some mechanisms of food carcinogens as risk factors of cancer have been reviewed [8, 12, 13] there is a need for more information as evidence to support the linkage between food carcinogens and various cancer. Additionally, physical exercise, dietary changes, restrictions on food production and distribution, and early cancer detection and treatment may prevent and or reduce exposures [14].
Dietary risk factors for cancer, particularly food carcinogens, have been linked to cancers such as breast, liver, lung, stomach and colorectal cancers. Diet-related cancers are on the rise, contributing to the global cancer incidence. The International Agency for Research on Cancer (IARC) predicted that the number of new cancer cases globally will rise to 28.4 million in 2040, which is approximately 47% higher when compared to 2020. Certain food contaminants such as aflatoxins have been associated as risk factors for liver cancer. Additionally, the Global Burden of Disease (GDB) 2021 report revealed some types of cancer linked to dietary behaviors, with a higher cancer burden in men relative to women. These include stomach, breast, esophageal, colorectal, and lung cancers [15, 16].
Globally, liver cancer incidence has continued to rise significantly, with a 75% increase in cases between 1990 and 2015 [17]. Men are twice as likely as women to develop liver cancer. The incidence of liver cancer also rises with age, with individuals aged 65 and older having the highest incidences [18]. Liver cancer is more common in low- and middle-income nations, where chronic hepatitis B and C infections are more common. China, Mongolia, Vietnam, and parts of Sub-Saharan Africa have significant rates of liver cancer [19]. Likewise, global stomach cancer is more prominent in men than in women, and the risk increases with age. Stomach cancer is more common in low- and middle-income countries, especially in East Asia and parts of South America, Japan, Korea, Chile, and Colombia [20]. In contrast with liver and stomach cancers, the global incidence of breast cancer is more common in women than men, but the incidence also increases with age, with the majority of cases occurring in women over 50 years of age [21]. Socio-demographic factors such as income and education level have a bearing on breast cancer incidence, with higher rates occurring in women of higher socioeconomic status [22]. Breast cancer is more common in high-income countries such as the United States, Canada, and Western Europe, but the incidence is on the rise in low- and middle-income countries as well [23]. Colorectal cancer is known globally to affect both males and women equally, and the risk rises with age [24, 25]. Colorectal cancer incidence can also be affected by socioeconomic factors such as income and education level, with higher rates occurring in individuals with a higher socioeconomic standing. Although colorectal cancer is more prevalent in high-income countries like the United States, Canada, and Western Europe, it is fast becoming more common in low- and middle-income countries [26, 27]. Of all the above, the most prevalent. The IARC estimated that there will be approximately 2.2 million new cases of lung cancer and 1.8 million deaths from lung cancer globally in 2020 [15]. Altogether, lung cancer, like liver and stomach, is more prevalent in men than in women, with men being roughly three times more likely to acquire lung cancer than women [28]. However, the gender difference in lung cancer incidence is narrowing, most likely due to increased female tobacco use [29]. The above discussions suggest that breast, liver, lung, stomach, and colorectal cancers are amongst the most frequent food carcinogen-related cancers. These demographic patterns of cancer incidence correlate strongly with regional differences in exposure to dietary carcinogens [30], including aflatoxins in liver cancer-prevalent regions, processed meats in colorectal cancer hotspots, and PAHs in populations with high lung cancer rates. The following section examines these specific food-cancer linkages in detail.
Several factors are known to contribute to the development of cancer such as genetics, lifestyle, environmental factors, and exposure to dietary carcinogens [6, 31], but of interest in this paper is dietary carcinogens as a risk factor of various types of cancer. Dietary carcinogens are substances present in food that have the potential to serve as risk factors for cancer or may induce cancers [4, 32, 33]. Although a variety of food contaminants exist [12], of interest in this study were the naturally occurring food contaminants (i) and those deliberately added as food adulterants (ii). Toxigenic microorganisms, e.g., fungi spp, and plants frequently contaminate foods and produce natural food contaminants during growth, harvest, storage, or processing, whereas food adulterants are either sometimes added to food to improve appearance, texture, or shelf-life [34, 35] or generally for economic purposes referred to as food fraud [36, 37]. Both kinds of dietary carcinogens are extensively distributed in the food chain and can endanger human health, thus requiring attention.
2.2.2.1 Natural Food Contaminant
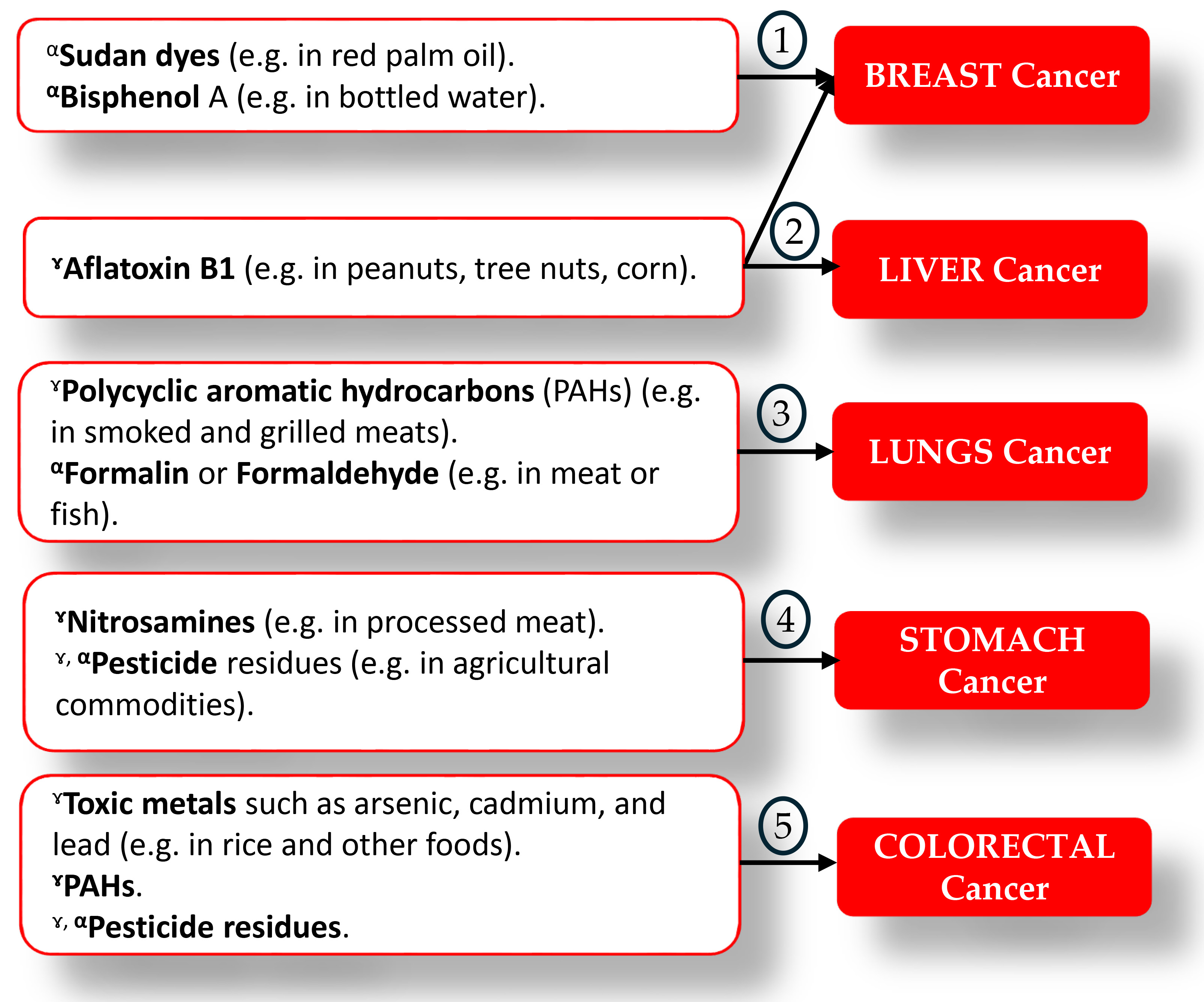
Agricultural commodities or foods that are damaged or poisoned because they either contain microorganisms, such as toxigenic fungi species, e.g., Aspergillus spp or toxic compounds such as secondary metabolites from toxigenic fungi species, also known as mycotoxins, that render food unsafe for consumption are often referred to as contaminated foods [38]. Where the food is rendered unsafe by the presence of microbial agents, such contamination is termed microbial food contamination (e.g., Aspergillus parasiticus, Bacillus cereus, and Escherichia coli), whilst the case of the presence of toxic chemicals in foods is known as chemical food contamination (e.g., mycotoxins and heavy metals). Generally, chemical food contamination is of interest to diet-related cancers (Fig. 1, Ref. [15, 16, 28, 39, 40, 41, 42, 43, 44, 45]).
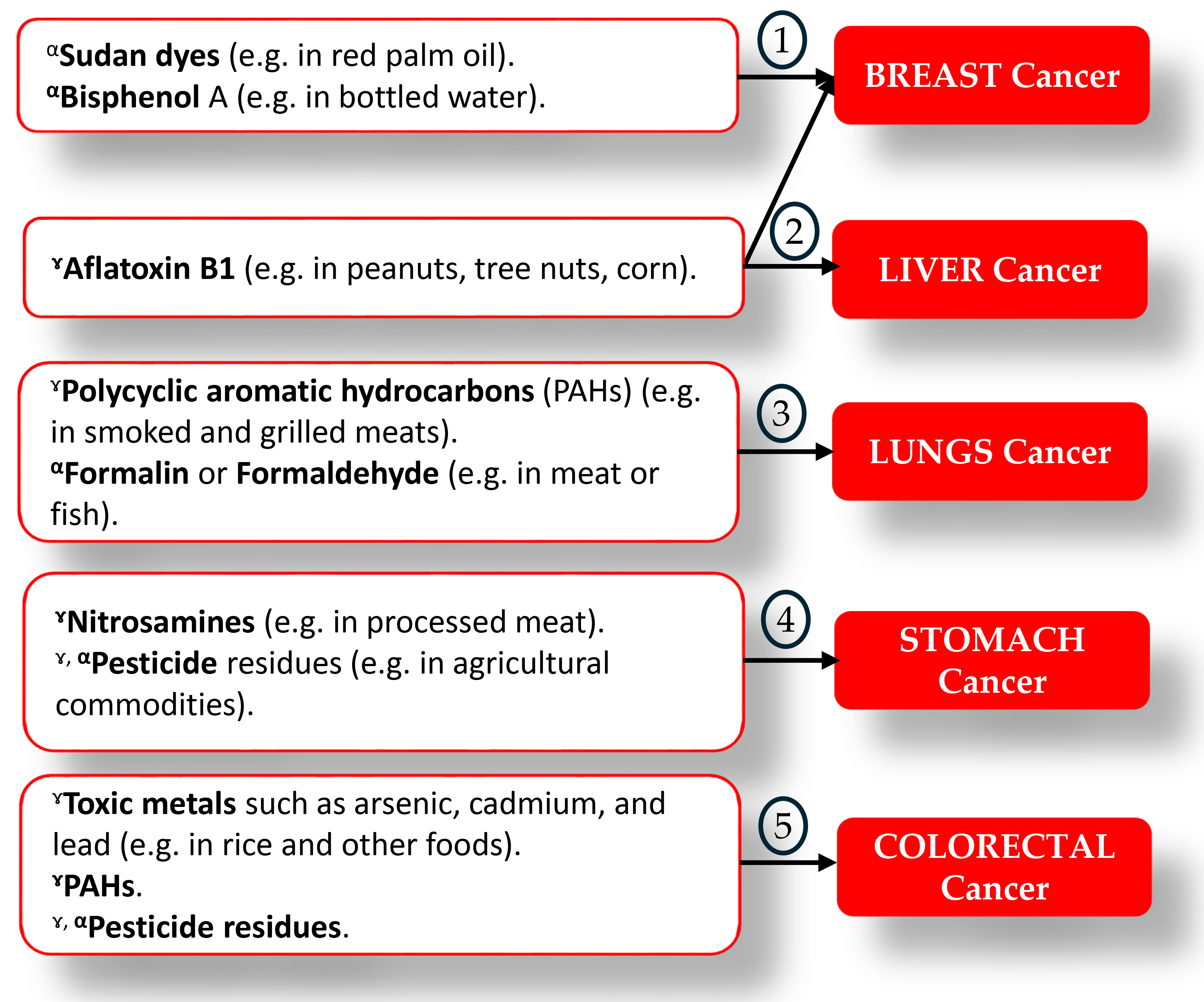 Fig. 1.
Fig. 1. Some dietary carcinogens and commonly contaminated foods, as well as speculated cancer-type adapted from 1 [40, 41], 2 [15, 16], 3 [28, 39, 42], 4 [43, 44], and 5 [45].⋎: Natural contaminant; α: Adulterant or Intentionally added contaminant; ⋎, α: Natural contaminant and adulterant.
Mycotoxins are secondary metabolites of toxigenic fungi species that frequently contaminate agricultural commodities worldwide. Over 500 different mycotoxins exist in the literature, but only five (aflatoxins, ochratoxins, fumonisins, trichothecenes [deoxynivalenol, nivalenol], and zearalenone) are currently recognized as economic and public health concerns [46, 47]. Some of these toxins are considered carcinogens, e.g., aflatoxins B1, ochratoxins A, and fumonisins B1. Aflatoxins are naturally occurring mycotoxins produced by the toxigenic fungi A. flavus and A. parasiticus [48, 49]. It commonly occurs in foods such as aflatoxin B1, aflatoxin B2, aflatoxin G1, and aflatoxin G2 with aflatoxin B1 being the most frequent, and toxic. Aflatoxins frequently contaminate agricultural commodities such as groundnuts, maize, and their food by-products, generally consumed as staple foods for many in sub-Saharan African regions such as Cameroon [50] and aflatoxins B1 is classified as Group 1 carcinogens by the International Agency for Research on Cancer [39]. Ochratoxin A is another naturally occurring mycotoxin that contaminates nuts in general, but also contaminates cereals, coffee, wine, and spices, and has been linked to kidney/lung cancer in humans [51]. It is generally classified as a group 2B carcinogen, i.e., possible human carcinogen [52] with LD50 estimated at 20–25 mg per kg. Likewise, the South African discovered mycotoxins known as fumonisin (particularly fumonisin B1) which is well known to contaminate cereals and has been classified as a group 2B carcinogen [53, 54].
Polycyclic Aromatic Hydrocarbons (PAHs) are a class of organic compounds produced during the incomplete combustion of organic materials such as wood, coal, and petroleum [55]. PAHs can be found in foods that have been grilled, smoked, or charred, such as meat, seafood, and vegetables. Some PAHs, such as benzo[a]pyrene, have been classified as Group 1 toxins [56]. Dietary PAHs exposure [57] may occur via the consumption of grilled or charred meats or foods, and or eating foods on which PAHs have settled. Food contamination by PAHs can originate from environmental pollution as well as during food preparation and processing. Out of 16 PAHs detected in foods, according to the European Commission, four types are commonly detected in foods and drinks, namely, benzo[a]pyrene (BaP) (group 1), chrysene (Chr) (group 1B), benz[a]anthracene (BaA) (group 2B), benzo[b]fluoranthene (BbF) (group 2B) [58].
Heavy metals such as cadmium, lead, and arsenic can contaminate food from both natural and artificial sources of food [55, 59]. They can accumulate in the food chain and represent a significant health risk, particularly when exposed for an extended period. Cadmium and cadmium compounds, for example, are designated as a Group 1 carcinogen to cause cancer in the lungs, but have been linked to kidney and prostate cancers [56] and are further complicated by their extremely long half-life of 10–30 years of cadmium dispersion to organs [60]. Lead is classified as a group 2A carcinogen, i.e., with a probable carcinogenic effect on humans [54] and has been associated with the brain [61] and breast [62, 63] cancers. Both cadmium and lead are heavy metals of carcinogenic potential, when the exposure is in excess amounts, correlate with the risk of multiple cancers (including breast, lung, gastrointestinal, kidney, and gynecological cancers) [63, 64, 65]. Likewise, exposures to cadmium and lead in fast foods and soft drinks sold in Yaounde, Cameroon have been speculated to be associated with the observed cancer prevalences [66].
Bisphenol A (BPA), a ubiquitous synthetic monomer, is a chemical that is used in the manufacture of plastic goods like food containers, water bottles, and baby bottles. The estrogenic properties of BPA can leach into the food and water supply. The US Environmental Protection Agency (EPA) and the U.S. Food and Drug Administration (FDA) had fixed a safe reference dose (RfD) of BPA for humans at 50 µg/kg/day, based on a 1000-fold reduction of the dose used in the NTP study [67]. BPA exposure has been linked to an increased chance of breast and prostate cancer in studies [67, 68]. Notwithstanding, this is still a prelude as to whether BPA is carcinogenic in men or not [69].
Pesticides are widely used in agriculture to keep pests and diseases at bay. Pesticide residues on food, on the other hand, have been linked to an increased risk of several kinds of cancer, including lymphoma, leukemia, and prostate cancer [70]. According to the WHO’s IARC’s 2015 monograph (Volume 112): evaluation of five organophosphate insecticides and herbicides, the IARC classifies glyphosate (a herbicide), and malathion and diazinon (both being insecticides) as probably carcinogenic to humans (Group 2A), whilst, tetrachlorvinphos and parathion (also insecticides) were classified as possibly carcinogenic to humans (Group 2B) [56].
2.2.2.2 Food Adulterants
Carcinogenic food adulterants are deliberately added to food for financial gain or to enhance appearance or texture [34, 35, 37]. Food adulteration is a global problem that can cause severe damage to Public Health and Safety [71, 72]. Adulteration of foods is a kind of food fraud. Simply, food fraud may be defined as “Any actions taken by businesses or individuals that deceive other businesses and/or individuals in terms of misrepresenting food, food ingredients, or food packaging that brings about financial gain” [36]. In short, any form of intentional manipulation of food for economic gain may be regarded as food fraud [73]. Some types of food fraud include deliberate substitution, dilution, counterfeiting, or misrepresentation of food, ingredients, or packaging; or even false or misleading statements made about a product. Each and or all of these types of fraud may affect food quality and safety, may damage consumer confidence, and harm food businesses or brands [37, 74, 75, 76, 77]. Some common types of adulterants include Sudan dye I–V, formaldehyde/formalin, and lead chromate, amongst others.
Sudan dye I–V, a well-known fat-soluble azo dye, which is generally used to stain fuel and industrial grease, is carcinogenic. The IARC classifies Sudan dyes as Group 3 carcinogens and is banned as food additives worldwide. As such, it is unsuitable for human consumption [78, 79]. Sudan dye IV is occasionally added to the most useful vegetable available, palm oil, and has been confirmed in some African countries including Ghana [80, 81] and recently speculated in Cameroon [82, 83]. In addition to red palm oil, Sudan dye IV has been detected in chili powder, and paprika and has been associated with human liver and bladder cancer [84].
Formaldehyde, a preservative and disinfectant, is sometimes used to enhance the appearance and texture of meat and fish [35, 85]. It is designated as a Group 1 carcinogen and has been linked to nasopharyngeal cancer in humans [39]. WHO recommends an indoor limit of the colorless, pungent-smelling, and highly reactive chemical with toxic properties, formaldehyde of 0.1 mg/m3 (i.e., 0.08 ppm) [86]. Formaldehyde is known to exist endogenously, and the concentration of endogenous formaldehyde in the blood of humans is approximately 2–3 mg/L (i.e., 0.1 mM) [87]. Also, formaldehyde can be found naturally in food up to the levels of 300 to 400 mg/kg, including fruits and vegetables (e.g., pear, apple, green onion), meats, fish, crustaceans, and dried mushrooms [88].
Lead chromate (aka chrome yellow) has been classified as group 1B [39]. The adulteration of turmeric with lead chromate poses a significant health risk, including an elevated risk of various cancers [89, 90]. Lead chromate, a toxic substance, generally added to turmeric during processing to enhance the yellow color, contributes to the risk of developing cancers and other diseases such as kidney cancer, lung cancer, nasal ulcer, nasal irritation, anemia, abortion, and brain damage [90].
Table 1 (Ref. [40, 41, 42, 43, 44, 45, 91, 92, 93, 94]) provides a summary of some potential preventive ways to manage various types of carcinogenic food contaminants. This information can be used as a reference for those interested in learning more about the impact of dietary carcinogens on cancer incidence, as well as, ways to reduce exposure and prevent cancer.
| Food contaminant or adulterant | Strategies to prevent contamination of foods | Reference |
|---|---|---|
| Aflatoxins | -Crop testing and tracking regularly. | [40, 41, 92, 93] |
| -Application of fungicides and insecticides. | ||
| -Proper crop storage and management. | ||
| -Establishing regulation guidelines for aflatoxin levels in food. | ||
| Sudan dye | -Regular testing and monitoring of food crops to reduce fungal contamination. | [40, 41] |
| Bisphenol A | -Proper storage and handling of food crops. | |
| Aflatoxins | -Setting regulatory limits for aflatoxin levels in food. | |
| Benzene | -Limiting the use of benzene in industrial operations; monitoring benzene levels in food and beverages. | [42, 94] |
| Polycyclic aromatic hydrocarbons (PAHs) | -Use of marinades with herbs and spices. | |
| Formalin or formaldehyde | -Cooking methods that produce less smoke and fewer PAHs. | |
| -Use of leaner meats. | ||
| Nitrosamines | -Limiting or eliminating intake of processed meat products. | [43, 44] |
| Pesticide residues | -Putting rules in place to limit the use of nitrite and nitrate additives in processed meats. | |
| Toxic metals (e.g., lead, arsenic, and cadmium) | -Utilization of alternative cereal grains such as quinoa, buckwheat, and amaranth. | [45, 91] |
| PAHs | -Adequate watering and fertilization techniques. | |
| Pesticide residues | -Setting maximum levels for PAHs in food. |
2.2.3.1 Control of Food Carcinogen Exposures
While complete elimination of all food carcinogens might not be feasible, there are multi-pronged approaches to significantly reduce exposure throughout the food supply chain. These strategies can be broadly categorized into two main areas which are prevention and reduction approaches.
There is need for the implementation of preventive measures such as Good Agricultural Practices (GAP) and Good Manufacturing Practices (GMP) that have established guidelines for safe food production and handling to minimize the introduction or formation of contaminants (some of which are carcinogens) in food at the source [95]. The GAP focuses on agricultural practices that minimize contamination from environmental toxins, such as mycotoxins and heavy metals [46], while GMP ensures proper sanitation, processing methods, and storage procedures to prevent the formation of carcinogens during food production and manufacturing [96]. Additionally, Food Safety Management Systems (FSMS) frameworks integrate GAP and GMP principles into a comprehensive plan for managing food safety hazards, including carcinogens [97]. The FSMS involves risk assessments, preventive controls, monitoring procedures, corrective actions, and verification steps throughout the food supply chain. More to that, educating consumers about food choices, safe handling practices, and proper cooking techniques can further empower individuals to reduce their exposure to carcinogens in their diet. Finally, advancement in technology will lead to continuous research and development of innovative technologies for food processing, storage, and packaging can lead to even more effective methods for minimizing carcinogen formation and contamination.
Reduction Strategies to lessen the number of carcinogens present in food reaching consumers. FSMS plays a crucial role in reducing exposure by identifying critical control points (CCPs) where contamination with carcinogens is most likely to occur. Implementing specific control measures at these CCPs, such as temperature control during processing or proper drying techniques for grains to prevent mycotoxin growth, significantly reduces the final number of carcinogens in food [98]. Additionally, regular inspections of fields or farms, processing facilities, and storage warehouses by regulatory agencies can help identify potential sources of contamination and ensure compliance with various food safety legislations. This proactive approach may help prevent carcinogens from entering the food supply chain.
2.2.3.2 Management of Consumers to Reduce Dietary Carcinogen Exposures
While the food industry implements preventative measures to minimize carcinogens, individual consumers also play a significant role in managing their exposure. By making informed choices about the food they purchase and how they handle it at home, consumers can significantly reduce their dietary intake of carcinogens [91, 92]. This empowers them to take charge of their health and contributes to lower overall cancer risk. Table 2 (Ref. [40, 41, 42, 43, 44, 45, 92, 99]) explores key strategies consumers can utilize to prevent and or control exposure to carcinogens. These strategies encompass preventive, control, and treatment strategies for selected diet-related cancers such as breast, liver, lung, stomach and colorectal (BLLSCr) cancers.
| Type of cancer | Prevention/Control strategies | Reference |
|---|---|---|
| Breast cancer | -Maintain a healthy weight | [40, 41] |
| -Engage in regular physical body activity | ||
| -Limit your booze consumption | ||
| Liver cancer | -Get vaccinated for hepatitis B | [40, 92] |
| -Avoid sharing needles or other injection equipment | ||
| -Limit alcohol intake | ||
| -Engage in regular physical activity | ||
| Lung cancer | -Avoid tobacco use and exposure to secondhand smoke | [42, 99] |
| -Protect against exposure to environmental pollutants | ||
| -Engage in regular physical activity | ||
| -Consume a healthy diet | ||
| Stomach cancer | -Consume a healthy diet rich in fruits and vegetables | [43, 44] |
| -Avoid exposure to environmental pollutants | ||
| -Treat and manage H. pylori infection | ||
| Colorectal cancer | -Consume a fiber-rich diet | [45] |
| -Engage in regular physical activity | ||
| -Avoid smoking and exposure to secondhand smoke | ||
| -Limit alcohol intake |
This paper has reviewed and highlighted some food carcinogens that are potential risk factors for various cancers, thus constituting a major global health challenge. The food carcinogens highlight in this review are naturally occurring contaminants (e.g., aflatoxins, heavy metals, bisphenol A, pesticide residues, polycyclic aromatic hydrocarbons) and economically motivated adulterants (e.g., Sudan dyes, formaldehyde) that are known to frequently contaminate staple foods, and serve as risk factors for some cancers. Breast, liver, lung, stomach, and colorectal cancers are among the predominant food carcinogen-related cancers in the literature. The trends and growing literature on food carcinogens as risk factors for these cancers underscore the need for food safety and public health interventions to reduce dietary exposure to these carcinogens. Potential strategies to control food carcinogens to reduce dietary exposures have been proposed. These strategies span across the crop growing phase (e.g., regular testing), storage, processing, product compliance with regulations, and product commercialization phases. Also, strategies to prevent and or control some diet-related cancers have been presented. For example, consumers may engage in physical exercise (for breast cancer), and reduce alcohol (for liver and colorectal cancers) and tobacco (for lung cancer) consumption. It may hereof be recommended that a comprehensive food safety and public health interventions be implemented to minimize dietary exposure to food carcinogens. These efforts should promote healthier agricultural, food preparation and manufacturing standards, and dietary practices, with the goal of reducing the global incidence of various diet-related cancers. Future research should explore the development and implementation of integrated public health strategies aimed at reducing dietary exposure to food carcinogens, given their significant role in global cancer incidence. Studies are needed to evaluate the effectiveness of control measures across the food supply chain, including agricultural practices, storage conditions, food processing, and regulatory compliance, in minimizing carcinogenic contamination. Additionally, further research should investigate the impact of lifestyle and dietary interventions on the prevention of food carcinogen-related cancers, particularly breast, liver, lung, stomach, and colorectal cancers, to inform evidence-based public health recommendations.
WAA designed the research study. WAA and BPT prepared the manuscript. KEF and EAA contributed in sourcing relevant articles. ANT and PFM provided advice on the study. WAA and BPT analyzed the data. WAA and BPT wrote the manuscript. All authors have contributed to the editorial changes made to the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.