Background: The impact of
polycystic ovary syndrome (PCOS) on endometrial receptivity
and embryo quality is a subject of debate. Different PCOS patient types may
exhibit different effects on these factors. This study aimed
to identify causes for low live birth rate by comparing endometrial receptivity
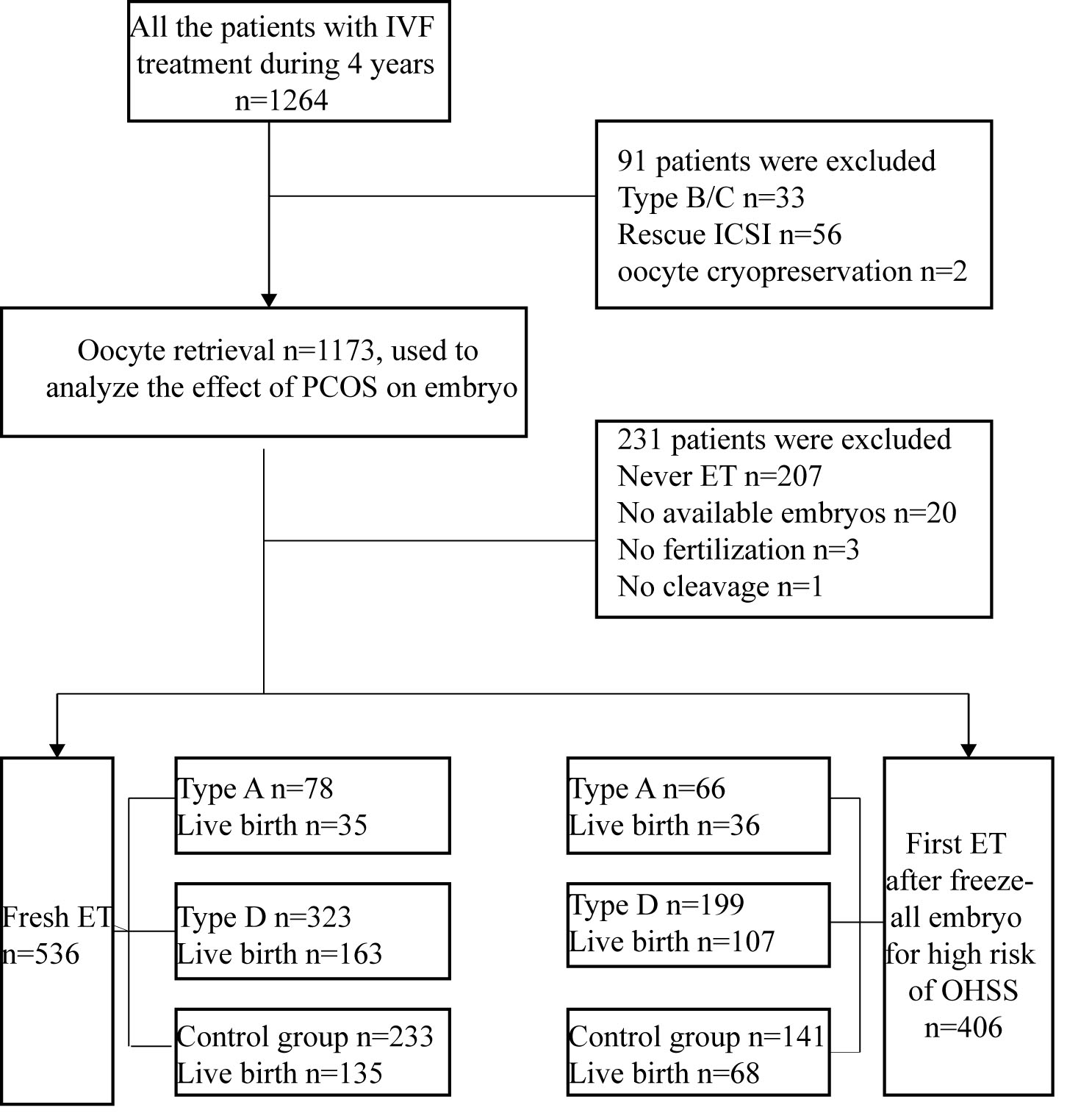
and embryo quality among different PCOS types. Methods: Overall, a total of 767 PCOS patients with first in vitro fertilization (IVF)/intracytoplasmic sperm
injection (ICSI) treatment classified into phenotype A (n =
167 patients) and phenotype D (n = 600
patients) were eligible for analysis. Patients with single
polycystic ovary (n = 406 patients) served as a control group
to exclude the advantages of clinical outcome from higher number of oocytes
retrieved in women with PCOS. Results: In phenotype A
and D, Anti-Müllerian hormone (AMH), antral follicle count
(AFC) and basic estradiol were significantly higher compared to
single polycystic ovary. However,
estradiol, progestin and endometrial thickness on the human chorionic
gonadotropin (hCG) day were significantly decreased. In fresh
cycles, phenotype A had a significant statistical decrease in the live birth rate
compared with single polycystic ovary (35/78 [44.87%]
vs. 135/233 [57.94%], p 0.05), although there was no
significant difference in the number of embryo transplants and clinical pregnancy
rate among the three groups. It might be associated with the significant
reduction of total gonadotropin (Gn) dose, Gn duration, and follicular output
rate (FORT) in all the typed PCOS groups. In the first frozen embryo transfer
(ET) cycles, no significant difference was observed for estrogen, progestin, or
endometrial thickness on the day of ovulation and live birth rate. Women with
live birth had a higher estradiol on the hCG day in the phenotype A (3763 [3121,
4752] vs. 2954 [2112, 4036] ng/mL) while a lower
estradiol in the single polycystic ovary (3312 [2341, 4465] vs. 3417
[2350, 4638] ng/mL). In multivariate logistic regression analysis, estradiol on
the hCG day was a significant independent factor predicting live birth for women
with phenotype A (odds ratio (OR) 1.000, 95% confidence interval (95% CI):
1.000–1.001), p = 0.034) and single polycystic ovary (OR 1.000, 95%
CI: 0.999–1.000, p = 0.013) in fresh ET. Conclusions:
The various subtypes of PCOS have no significant adverse
effect on embryonic outcome. It was not directly caused by PCOS; however, low
levels of estradiol may be the reason for the low live birth rate
owing to significant reduction of total Gn dose, Gn duration
and FORT as a result to low incidence of ovarian hyperstimulation syndrome (OHSS)
in phenotype A.