Background: Concerns are increasing over the mechanisms of drug
resistance pathogens among non-gonococcal urethritis (NGU) or cervicitis. The
study aims to explore the distribution of Ureaplasm urealyticum
(U. urealyticum) and Mycoplasma homins (M. homins)
isolates, characteristics of multidrug resistance, and the underlying mechanism
to allow clinicians to deliver rational therapy for NGU. Methods: Samples
from cervical secretions of 246 patients with NGU were collected. Mycoplasma
culture and drug susceptibility tests were performed, respectively. The
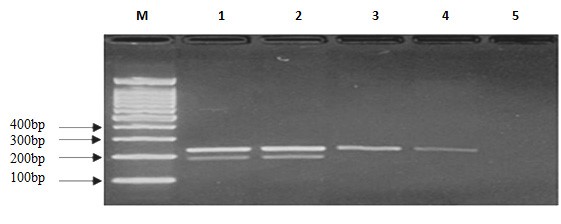
resistance genes were detected by multiplex Polymerase Chain Reaction (PCR), and
the PCR products were cloned and sequenced. Results: Out of 246 samples,
the overall prevalence of U. urealyticum and/or M. hominis
infection was 39.02% (96/246). In 96 culture positive samples, the overall
infection rate of U. urealyticum was higher than that of the single
M. hominis (46.87% vs. 28.13%) (p 0.05), and the
coinfection rate was 25.00% (24/96). Each U. urealyticum and M.
hominis isolate exhibited resistance to at least three types of antimicrobial
agents (manifest by more than 70% resistance to erythromycin, tetracycline,
ciprofloxacin, and spiramycin, followed by ofloxacin, roxithromycin, azithromycin
and josamycine (with resistance thereto of more than 50%)). More than
80% of U. urealyticum and M. hominis isolates were
susceptible to minomycine and doxycycline, whereas 81.16% and 77.44% of both U. urealyticum and M. hominis isolates were also
susceptible to minomycine and doxycycline. Surprisingly, the resistance
rate of the mixed infection was higher that of erythromycin, tetracycline and
ciprofloxacin comparison to the single infection (p 0.05). All
tetracycline-resistant isolates carried the tetM gene and 50% of
erythromycin-resistant isolates carried the ermA gene.
Conclusions: Among outpatients with recurrent NGU, the U.
urealyticum infection dominated, followed by M. hominis, mixed
U. urealyticum and M. hominis infection. Minomycine and
doxycycline are recommended for empirical clinical treatment. The determination
of U. urealyticum and M. hominis infection, antibiotic
susceptibility testing is crucial for effective therapy.