- Academic Editor
†These authors contributed equally.
Background: Concerns are increasing over the mechanisms of drug
resistance pathogens among non-gonococcal urethritis (NGU) or cervicitis. The
study aims to explore the distribution of Ureaplasm urealyticum
(U. urealyticum) and Mycoplasma homins (M. homins)
isolates, characteristics of multidrug resistance, and the underlying mechanism
to allow clinicians to deliver rational therapy for NGU. Methods: Samples
from cervical secretions of 246 patients with NGU were collected. Mycoplasma
culture and drug susceptibility tests were performed, respectively. The
resistance genes were detected by multiplex Polymerase Chain Reaction (PCR), and
the PCR products were cloned and sequenced. Results: Out of 246 samples,
the overall prevalence of U. urealyticum and/or M. hominis
infection was 39.02% (96/246). In 96 culture positive samples, the overall
infection rate of U. urealyticum was higher than that of the single
M. hominis (46.87% vs. 28.13%) (p
Non-gonococcal urethritis (NGU) or cervicitisis is one of the most common sexually transmitted diseases [1]. The main pathogens are Ureaplasma urealyticum (U. urealyticum) and Mycoplasma hominis (M. hominis) in addition to Chlamydia trachomatis [2]. If the treatment is not timeous, NGU is apt to induce chronic prostatitis, or epididymitis, in men. In addition, both U. urealyticum and M. hominis were associated with endometritis, salpingitis, or pelvic inflammatory disease in women. Meanwhile, they have been suggested to be related to infertility [3]. Tetracycline, quinolones, and macrolides are the first-choice drugs used to treat Mycoplasma spp. and Ureaplasma spp. infection [4]. In recent years, Mycoplasma spp. and Ureaplasma species resistant to these drugs are increasing due to the abuse of antibiotics or irregular treatment, mixed infection, or repeated infection by pathogens and other factors, especially with regard to increasingly multidrug-resistant isolates, resulting in NGU infection recurrent or persist [5, 6]. Persistent or recurrent NGU due to multidrug-resistant Mycoplasma and Ureaplasma infection has become a difficult problem facing those in clinical practice [7, 8]. Therefore, the study aimed to explore the drug-resistance mechanism of U. urealyticum and M. hominis isolates in China; the selection of sensitive drugs is the key to effective control of Mycoplasma infection.
In this study, U. urealyticum and M. hominis isolates from 246 cases of recurrent NGU with resistance to 12 antimicrobial agents and the mechanism of drug resistance were analyzed. The results offer a reference for clinicians to make the right choice of antimicrobial agents as best possible.
We conducted a retrospective study of U. urealyticum and M. hominis-infected NGU patients at an affiliated hospital of Beihua University, China. 246 patients were enrolled in a gynecology outpatient clinic and sexually transmitted disease clinics during the period from June 2020 to June 2022. Clinical and microbiological data were recorded from the database. All of them had a history of sexual confusion or urethritis symptoms. Single U. urealyticum and M. hominis (or both) were positive after mycoplasma culture at the initial diagnosis. However, gonococcus, chlamydia, Candida, trichomonad, and other urogenital tract infections were excluded through clinical and laboratory tests. Empirical single antibiotic, or a combination of two antibiotics, for prophylaxis of NGU were administered with one month, and presence of coinfection with Chlamydia trachomatis was also excluded. Those with U. urealyticum and M. hominis combined with culture could still be positive with history of previous antibiotic prophylaxis for longer than two months could be included in the study. No repetitive isolates from a single patient were included. This study, entailing collection of clinical samples, was approved by the institutional ethics committees of the participating hospital and prior written informed consent was gained from all participants in the study.
Firstly, a cotton swab was used to wipe away the excessive mucus in the cervix after the patient exposed the cervix, discarded it, and then another sterile swab was inserted into the cervix to a depth of 1 to 2 cm. After remaining in place for 10 to 30 seconds, the swab was slowly rotated it through one complete turn. The sample thus collected was rapidly inoculated into liquid medium and sent to the laboratory as soon as possible.
A mycoplasma identification verification and antibiotic susceptibility testing
kit (RenFuBoSai, Co., Ltd, Zhengzhou, Henan, China) was used for the culture,
identification, and antibiotic susceptibility assay according to the instructions
supplied. The collected cotton swabs were washed in the culture medium, and 0.1
mL of culture medium was directly inoculated into 24 wells (50
Regarding drug susceptibility, a panel of 12 antimicrobial agents including doxycycline, minomycine, tetracycline, ciprofloxacin, levofloxacin, ofloxacin sparfloxacin, erythromycin, spiramycin, josamycine, roxithromycin, and azithromycin could be determined by two concentration wells of each agent. Interpretation of drug susceptibility: both wells were sensitive if yellow, low-concentration if one well was red, high-concentration if one well was yellow for the intermediary, and both wells were red, indicative of drug resistance.
500
A series of primers for identification of resistance genes including erm
and tet were designed (Table 1). A 50-
| No. | Primers | Sequence (5’ to 3’) | Expected length | PCR condition | |
|---|---|---|---|---|---|
| T |
t | ||||
| 1 | ermA | F-AAGCGGTAAACCCCTCTGA | 190 | 56 | 60 |
| R-TTCGCAAATCCCTTCTCAAC | |||||
| 2 | ermC | F-AATCGTCAATTCCTGCATGT | 299 | 56 | 60 |
| R-TAATCGTGGAATACGGGTTTG | |||||
| 3 | tetA | F-GCTACACCTGCTTGCCT | 410 | 56 | 60 |
| R-CATAGATCGCCGTGAAGA | |||||
| 4 | tetB | F-TTGGTTAGGGGCAAGTTTG | 320 | 56 | 60 |
| R-GTAATGGGCCAATAACACCG | |||||
| 5 | tetM | F-AGTGGAGCGATTACAGAA | 260 | 56 | 60 |
| R-CATATGTCCTGGCGTGTCTA | |||||
| 6 | tetK | F-GTAGCGACAATAGGTAATAGT | 159 | 56 | 60 |
| R-GTAGTGACAATAAACCTCCTA | |||||
PCR steps were run at 94 °C for pre-denaturation for 5 min, followed by 30 cycles of denaturation for 30 s at 94 °C; the annealing temperature and conditions (Table 1) were applied for 30 s, followed by extension for 1 min at 72 °C and final extension at 72 °C for 5 min. PCR amplicons were done under electrophoresis on 2% (w/v) agarose gel in TBE buffer at 70 V for 60 min. Gels were stained and the band size was estimated using a DNA Marker with a molecular weight of 100 to 1200 bp as a reference.
The target fragments of the PCR products were excised using a sterile scalpel. A
gel kit for extraction of DNA (Promega, Madison, WI, USA) was utilized to purify
the PCR products extracted from the gel. Then the PCR products were ligated into
the pGEM-T® Easy vector (Takara, Shiga, Japan) and transformed
into E. coli DH
SSPS 10.0 statistical software (IBM Corp., Chicago, IL, USA) was used to compare
the differences in U. urealyticum and M. hominis infection and
drug resistance rates using the
All of patients had a course of disease of 3 to 26 months. They had an average
age of 28.14
This research compared the antimicrobial susceptibility patterns of the
individual U. urealyticum, M. hominis and both U.
urealyticum and M. hominis isolated from 96 culture positive samples.
Our findings showed that all U. urealyticum and M. hominis
strains exhibited resistance to at least three kinds of antimicrobial agents
(manifest as more than 70% resistance to erythromycin, tetracycline,
ciprofloxacin, and spiramycin, followed by ofloxacin, roxithromycin,
azithromycin, and josamycine (with more than 50% resistance thereto)). More than
80% of U. urealyticum and M. hominis strains were
susceptible to minomycine and doxycycline, whereas 81.16% and 77.44% of both U. urealyticum and M. hominis strains were susceptible
to minomycine and doxycycline. Surprisingly, the resistance rate under
mixed infection was higher that of erythromycin, tetracycline, and ciprofloxacin
compared to that under single infection (p
| Antimicrobial agents | U. urealyticum (n = 45) | U. urealyticum + M. hominis (n = 24) | M. homins (n = 27) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| S (%) | I (%) | R (%) | S (%) | I (%) | R (%) | S (%) | I (%) | R (%) | |
| Doxycycline | 87.01 | 0.75 | 12.24 | 81.16 | 5.13 | 13.71 | 83.55 | 8.56 | 8.09 |
| Minomycine | 84.72 | 2.80 | 12.48 | 77.44 | 7.45 | 14.39 | 85.84 | 8.82 | 5.34 |
| Tetracycline | 2.38 | 20.23 | 77.39 | 3.53 | 15.76 | 91.51 | 3.56 | 20.12 | 76.32 |
| Ciprofloxacin | 15.08 | 11.04 | 73.88 | 9.48 | 10.50 | 82.54 | 14.25 | 15.45 | 70.30 |
| Ofloxacin | 22.41 | 18.42 | 59.17 | 21.42 | 20.74 | 57.84 | 23.56 | 20.45 | 55.99 |
| Roxithromycin | 20.54 | 19.28 | 60.18 | 21.42 | 17.34 | 61.24 | 20.32 | 16.26 | 63.42 |
| Azithromycin | 21.87 | 16.78 | 61.35 | 14.24 | 23.52 | 62.24 | 22.27 | 17.52 | 60.21 |
| Erythromycin | 20.45 | 6.31 | 73.24 | 21.51 | 1.12 | 77.37 | 32.55 | 3.88 | 63.57 |
| Josamycine | 23.53 | 0.13 | 67.25 | 11.34 | 18.54 | 70.12 | 21.82 | 6.16 | 72.02 |
| Sparfloxacin | 25.37 | 26.54 | 48.18 | 28.44 | 22.29 | 49.27 | 23.56 | 28.71 | 47.73 |
| Spiramycin | 15.04 | 12.67 | 72.29 | 12.13 | 21.68 | 65.23 | 9.27 | 13.49 | 77.24 |
| Levofloxacin | 20.63 | 30.13 | 49.24 | 15.64 | 23.61 | 60.75 | 20.74 | 11.66 | 67.60 |
S, Sensitivity; I, Intermediate; R, Resistance.
The total DNA of multidrug-resistant U. urealyticum and M. hominis as a template, the tetracycline and erythromycin resistance genes could be detected by multiplex PCR. PCR products were sequenced and BLAST analysis from GenBank showed that the DNA sequences from tetM and ermA gene were 100% identical to those described in GenBank (data not shown). Both tetM and ermA genes were successfully amplified in all tetracycline-resistant, and 50% of erythromycin-resistant U. urealyticum and M. hominis strains (Fig. 1).
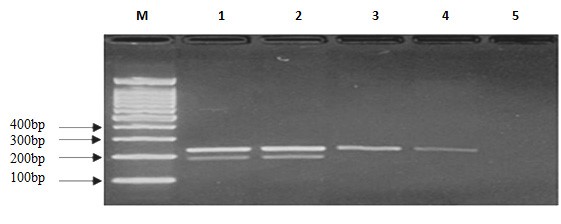 Fig. 1.
Fig. 1.Agarose gel electrophoresis of tetM and ermA genes detected by multiplex PCR among samples from recurrent non-gonococcal urethritis or cervicitis patients. Lane M, Marker; Lane 1, Positive control; Lane 2, Positive specimens carrying tetM and ermA; Lane 3–4, tetM gene; Lane 5, Negative control.
The aetiology of recurrent or persistent NGU shows a multi-factor nature.
Infectious agents including U. urealyticum and M.
hominis isolates accounted for less than 30% worldwide [9]. Ideally, treatment
with etiological diagnosis should be effective and incur only low-level
side-effects. Mycoplasmas are intrinsically resistant to
In the present study, the overall prevalence of U. urealyticum and/or
M. hominis infection was 39.02% (96/246) out of 246 samples and
multidrug-resistant U. urealyticum and M. hominis infection led
to NGU recurrence or persistence among NGU patients. This finding is consistent
with results reported by other studies [12, 13]. In fact, women are prone to
infection with U. urealyticum and M. hominis strains,
especially in sexually active periods. Mycoplasma spp. and
Urealyticum species were found in the female urogenital system as a part
of the normal flora. When the body was in a normal condition, there are no
clinical symptoms. When the patient’s immunity was low and the patient’s
genitourinary environment changed, the number of mycoplasmas would increase
correspondingly and achieve the effect of pathogenicity, and more reports
indicate that mycoplasma infection in the genital tract will not only cause
pelvic inflammatory disease, endometritis, etc., but more serious cases
will induce some pathological changes leading to female infertility [14, 15].
Zheng et al. [16] analyzed 4082 Chinese patients infected with
U. urealyticum and M. hominis, and their findings showed that
the rate of Mycoplasma infection was 48.2% in women. Similar to M.
hominis, Mycoplasma genitalium (M. genitalium) is also part of
the normal flora, however, it is difficult to culture the organism. Besides,
evidence for any treatment of persistent or recurrent NGU should cover
Mycoplasma, Chlamydia trachomatis, and even flora associated
with bacterial vaginosis. Sarier et al. [17] reported that the
quantification of the Mycoplasma load may provide a useful information
for differentiating NGU infection or compensation. Generally, higher organism
load (
Tetracycline was the first-choice for treatment with U. urealyticum and M. hominis infection as well as erythromycin [18, 19]. In recent years, reports of resistance to tetracyclines and erythromycin have increased year-on-year. The average U. urealyticum resistance rate to tetracycline increased from 46.4% in 2000 to 68.3% in 2020 [18, 20]. The resistance rate of doxycycline is generally maintained at 35%, and it can, at time of writing, be used as a tetracycline-replacement drug. The resistance to tetracycline is mainly mediated by the membrane-associated tet protein, which acts mainly by exchanging protons with the cation complex of tetracycline [21, 22]. All tet proteins belong to the MF protein family, and at least 18 tetracycline active efflux system proteins have been recorded in bacteria [23]. The four efflux system protein genes including tetA, tetB, tetK, and tetM were detected in the study. The tetracycline-resistant strains were all positive for tetM, which was consistent with the drug-resistant phenotype. It was caused by the expression of ribosome-protected tetM protein. tetM is the most popular active efflux system in U. urealyticum isolates, as reported elsewhere [24, 25]. Additionally, the erythromycin-inactivating enzyme ermA gene, which is highly tolerant to erythromycin, was detected in erythromycin-resistant U. urealyticum and M. hominis isolates. The ermA gene expresses erythromycin ribosome methylation whose enzyme methylates erythromycin ribosomal target sites. The literature reports that bacteria resistance to erythromycin was related to the chemical structure of macrolides [26]. Interestingly, 50% of erythromycin-resistant U. urealyticum and M. hominis isolates carried the ermA gene.
In the present study, all U. urealyticum and M. hominis isolates were recognized as exhibiting multidrug-resistance. They exhibited resistance to at least three kinds of antimicrobial agents (manifest as more than 70% resistance to erythromycin, tetracycline, ciprofloxacin, and spiramycin, followed by ofloxacin, roxithromycin, azithromycin, and josamycine (with resistance thereto of more than 50%). More than 80% of U. urealyticum and M. hominis strains were susceptible to minomycine and doxycycline, whereas 81.16% and 77.44% of both U. urealyticum and M. hominis strains were susceptible to minomycine and doxycycline. Surprisingly, the resistance rate of the mixed infection was higher that of erythromycin, tetracycline, and ciprofloxacin when compared to commensurate rate under single infection. Besides, U. urealyticum and M. hominis isolates were highly resistant to ciprofloxacin. Fluoroquinolone antibacterial agents are among the most rapidly developed, chemically synthesized antibacterial agents in the past 20 years, and they are widely used in animal husbandry and medical applications [27, 28]. Studies have found that mutations in the DNA gyrase gene located on the Mycoplasma chromosome cause the DNA gyrase gene concerning antimicrobial agents to change, thereby reducing drug accumulation and drug resistance, which is the cause of quinolone resistance [29, 30].
Our findings reported the multidrug U. urealyticum and M. hominis isolates among female NGU patients in Eastern and Northern China and reflected certain regional profiles therein. On the one hand, female mucopurulent non-gonococcal cervicitis and urethritis are equivalent, on the other hand, the incidence of female infertility in China is increasing year-on-year. Infertility is a serious threat to women’s health. The spectrum of drug-resistance in Mycoplasma is constantly changing. U. urealyticum and M. hominis culture, plus drug susceptibility testing, can offer good guiding significance for clinical treatment [31, 32]. However, there were some limitations to the present research: first, the sample size was small, with some selection bias therein; second, we could not conduct laboratory screening to detect M. genitalium and Chlamydia trachomatis. Besides that, we could not quantitatively evaluate Mycoplasmas in the genital tract. Next, more data from multiple centers should be included and in-depth exploration of treatment could be conducted in future research.
Among outpatients with recurring NGU, the U. urealyticum infection dominated among Mycoplasma infections, followed by M. hominis, and mixed U. urealyticum and M. hominis infection. Minomycine and doxycycline are recommended for empirical clinical treatment. In the determination of U. urealyticum and M. hominis infection, antibiotic susceptibility testing is crucial for effective therapy.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
LM conceived, designed the experiments and wrote a draft manuscript. BL and ML analyzed, interpreted the results of the experiments and revised the manuscript. WC performed the experiments. PL and XF collected the clinical data. All authors read and approved the final manuscript.
Ethical approval for collecting clinical samples was received by the institutional ethics committees of the participating hospital (Ethical approval number: Protocol Number 2020-02-05). Informed consent forms were reviewed and signed by all participants before samples collection.
We thank three anonymous reviewers for excellent criticism of the article.
The present project was a part of Jilin Science and Technology Development Program (20190304101YY and 20190301014NY); the Health and Family Planning Commission of Jilin Province (2018J098) and “14th Five-Year Plan” Science and Technology Project of Jilin Provincial Department of Education (JJKH20220076KJJ) also supported the project.
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
