1 Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, 13620 Seongnam, Republic of Korea
2 Department of Obstetrics and Gynecology, Chungnam National University Hospital, 35015 Daejeon, Republic of Korea
3 Department of Pediatrics, Seoul National University Bundang Hospital, 13620 Seongnam, Republic of Korea
4 Department of Obstetrics and Gynecology, Seoul National University College of Medicine, 03080 Seoul, Republic of Korea
5 Department of Pediatrics, Seoul National University College of Medicine, 03080 Seoul, Republic of Korea
Abstract
Background: Late preterm birth is associated with increased risks of
adverse neonatal outcomes, including respiratory distress syndrome (RDS) and
hypoglycemia. The use of antenatal corticosteroids (ACS) has been shown to reduce
these risks in early preterm infants. However, the efficacy of rescue ACS in late
preterm infants remains uncertain. This study aimed to assess the effectiveness
of rescue ACS in reducing the incidence of RDS and hypoglycemia in late preterm
infants. Methods: A retrospective cohort study was conducted on women
who delivered singleton late preterm infants (34 + 0 to 36 + 6 weeks of
gestation) at a tertiary hospital. The inclusion criteria were completion of the
initial cycle of ACS in the early preterm period (before 34 + 0 weeks of
gestation). Data on maternal baseline characteristics, ACS administration, and
neonatal outcomes were collected from medical records. Statistical analyses,
including logistic regression and multivariate modeling, were performed to assess
the association between rescue ACS and neonatal outcomes. Results: A
total of 155 singleton late preterm infants were included in the study. Among
them, 27.8% (43/155) received rescue ACS after 34 weeks of gestation, while
72.2% (112/155) did not. Neonates who did not receive rescue ACS had a
significantly higher incidence of RDS compared to those who did (10.7%
vs. 0%, p = 0.038). However, the results were not
statistically significant in the multivariate analysis (odds ratio (OR), 0.07;
95% confidence interval (CI), 0.00–1.48; p = 0.087). Additionally,
there were no significant differences in the frequencies of hypoglycemia (glucose
level
Keywords
- late preterm delivery
- antenatal corticosteroid
- rescue corticosteroid
- betamethasone
- respiratory distress syndrome
- hypoglycemia
Late preterm birth is defined as delivery between 34 + 0/7 weeks and 36 + 6/7 weeks of gestational age [1]. The incidence of late preterm birth among live singleton births ranges from 3.0% to 5.0%. The rate of late preterm birth out of preterm birth is as high as 65%–75% and is on the rise, especially in high-income countries [2, 3]. Newborns born during the late preterm period face more neonatal complications than those born at term, including transient tachypnea of the newborn (TTN), respiratory distress syndrome (RDS), persistent pulmonary hypertension, and apnea [1, 2, 3, 4, 5].
Antenatal corticosteroid (ACS) administration prior to 34 + 0/7 weeks of gestation is known to reduce neonatal RDS, TTN, neonatal intensive care unit admission, and hospital stay [6, 7, 8]. Recently, studies on the efficacy of ACS administration have been actively conducted on late preterm infants, and the ALPS (Antenatal Betamethasone for Women at Risk for Late Preterm Delivery) trial has shown that late preterm ACS administration significantly reduces severe respiratory complications, such as TTN and the composite of RDS, bronchopulmonary dysplasia, and apnea [9]. Conversely, late preterm ACS administration has several adverse effects, including neonatal hypoglycemia, impaired growth, and long-term risk [7, 10, 11]. While the results are controversial, based on the ALPS trial, both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine recommend a single course of ACS for pregnant women between 34 + 0/7 and 36 + 6/7 weeks of gestation who are at an imminent risk of preterm delivery within the next 7 days or prior to reaching 37 + 0/7 weeks of gestational age [6, 12].
In a multicenter, randomized, placebo-controlled trial on rescue ACS, patients
who had singleton or twin pregnancies before 33 weeks of gestation and completed
a single course of ACS before 30 weeks of gestation were randomly chosen to
receive a rescue course of ACS or placebo at least 14 days apart from the initial
single course of ACS [13]. This trial reported that rescue ACS significantly
reduced neonatal morbidity at
The present study aimed to evaluate the efficacy of rescue ACS between 34 + 0/7 and 36 + 6/7 weeks of gestation in patients who completed an initial course of ACS before 34 + 0/7 weeks of gestation.
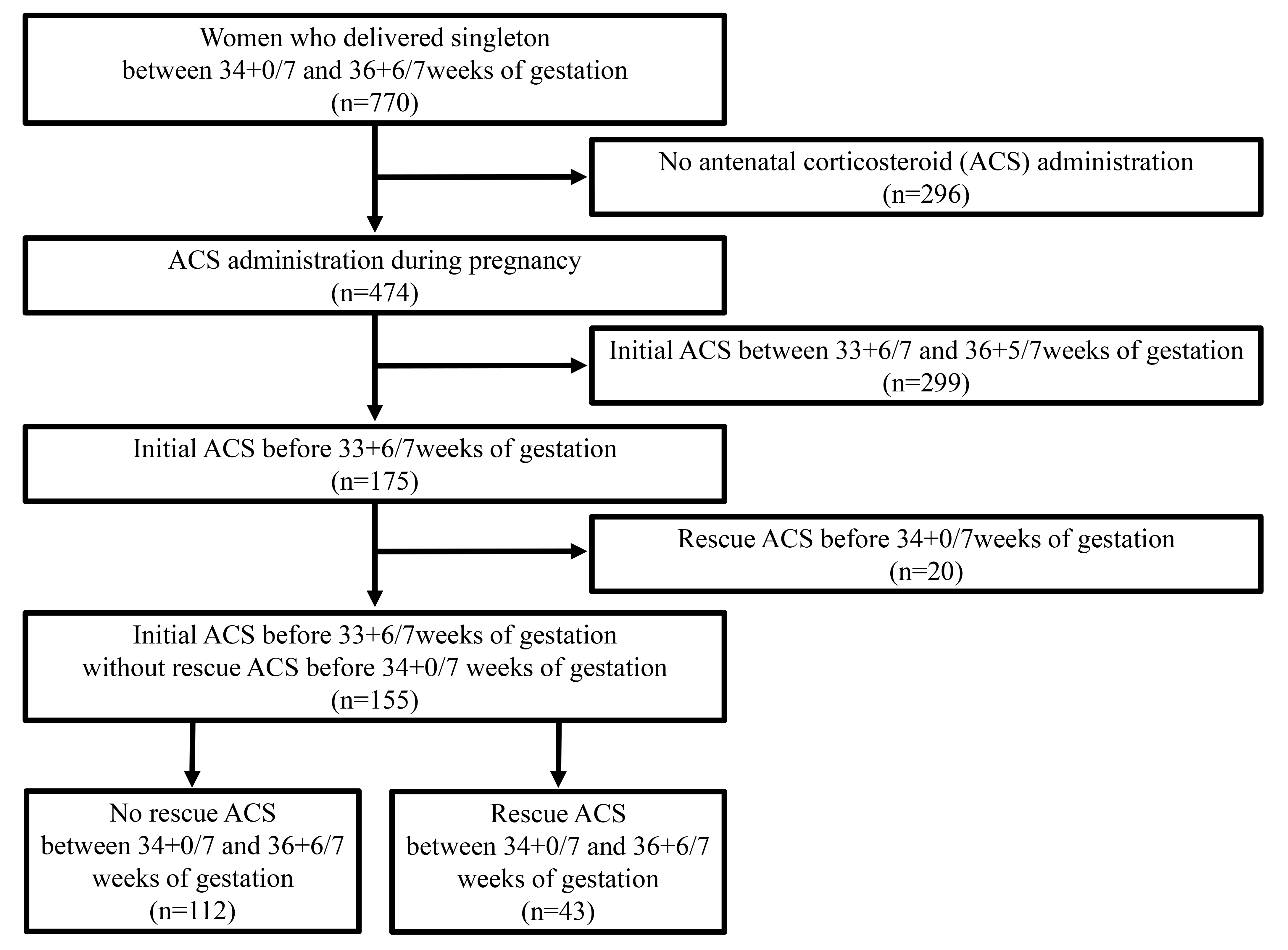
This was a retrospective cohort study conducted on women who delivered singleton late preterm infants (34 + 0 to 36 + 6 weeks of gestation) at Seoul National University Bundang Hospital from May 2016 to October 2021 (Fig. 1). The inclusion criteria were as follows: completion of the initial cycle of ACS in the early preterm period (before 34 + 0 weeks of gestation). The exclusion criteria were as follows: (1) patients who were not exposed to ACS during pregnancy; (2) patients who were provided with initial ACS during the late preterm period (33 + 6/7–36 + 5/7 weeks of gestation); (3) patients who received rescue ACS for more than one cycle; and (4) patients who received both initial and rescue ACS during the early preterm period (before 34 + 0/7 weeks of gestation).
 Fig. 1.
Fig. 1.Flow chart of the study.
Data on maternal baseline characteristics, such as age, parity, mode of delivery, gestational age at delivery, gestational age at initial ACS, and gestational age at rescue ACS, were obtained from medical records. Data regarding the presence or absence of pregnancy-related complications and risk factors, such as hypertensive disorder of pregnancy, gestational diabetes, and indication for initial ACS, were also collected. The study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-1905-540-005). The need for obtaining informed consent from the study participants was waived due to the retrospective nature of this study.
Based on the ALPS trial, we administered a course of ACS to patients in the late preterm period (34 + 0/7–36 + 6/7 weeks in gestation) who were at risk of delivery within 7 days or before 37 weeks of gestation in our institution since May 2016 [9]. In some cases, rescue ACS was also administered to late preterm infants based on the physician’s decision, although it is not recommended by guidelines [6, 8]. For this study, rescue ACS in the late preterm period was defined as the administration of at least one of two doses of 12 mg (3 mL) betamethasone, which is sodium phosphate 5.2 mg (betamethasone 4.0 mg) in 1 ample (1 mL), produced by Dawon Parm (Seoul, Korea), intramuscularly every 24 h between 34 + 0/7 and 36 + 6/7 weeks of gestation.
The primary outcomes assessed were RDS and neonatal hypoglycemia. RDS, typically
caused by surfactant deficiency, was diagnosed clinically if the neonate
exhibited respiratory distress requiring surfactant replacement at least once
[14, 15]. Neonatal hypoglycemia was defined as a glucose level
Continuous variables were compared using the Mann–Whitney U test, and
categorical variables were assessed using the Chi-square test. Fisher’s exact
test was used in cases where the frequency was less than 5 or when the sample
size of any variable was below 20% of the total sample size. Multivariate
logistic regression was used to determine the factors associated with neonatal
outcomes. Multivariate modeling with inclusion of the following factors was
applied: variables with p
During the study period, a total of 155 singleton late preterm neonates were exposed to ACS in the early preterm period (before 34 + 0 weeks of gestation) (Fig. 1). Clinical characteristics were compared based on rescue ACS administration after a gestational age of 34 weeks, and the results are summarized in Table 1.
| Rescue steroid administration | p-value | |||
| Absent (n = 112) | Present (n = 43) | |||
| Maternal age (years) | 34.0 (31.0–36.0) | 35.0 (31.0–37.0) | 0.468 | |
| Nulliparity | 56.3% (63) | 62.8% (27) | 0.460 | |
| Hypertensive disorder of pregnancy | 34.8% (39) | 44.2% (19) | 0.281 | |
| Gestational diabetes | 12.5% (14) | 23.3% (10) | 0.135 | |
| Gestational age at initial ACS administration (weeks) | 32.6 (31.3–33.3) | 31.4 (29.5–32.5) | ||
| Interval initial ACS administration to delivery (days) | 16 (8–26) | 25 (18–44) | ||
| Indication for initial ACS administration | ||||
| Spontaneous preterm birth | 48.2% (54) | 53.5% (23) | 0.557 | |
| Medically indicated preterm birth | 51.8% (58) | 46.5% (20) | ||
| Gestational age at delivery (weeks) | 34.4 (34.1–35.4) | 35.1 (34.5–35.3) | 0.011 | |
| Vaginal delivery | 33.9% (38) | 37.2% (16) | 0.701 | |
| Sex (male) | 59.8% (67) | 60.5% (26) | 0.942 | |
| Birthweight (grams) | 2260 (2023–2630) | 2280 (2035–2520) | 0.875 | |
| 1-min Apgar score |
22.3% (25) | 20.9% (9) | 0.851 | |
| 5-min Apgar score |
5.4% (6) | 2.3% (1) | 0.674 | |
| Respiratory distress syndrome | 10.7% (12) | 0% (0) | 0.038 | |
| Transient tachypnea of the newborn | 42.0% (42/100) | 25.6% (11/43) | 0.062 | |
| Hypoglycemia, glucose level |
10.7% (12) | 9.3% (4) | ||
| Hypoglycemia, glucose level |
62.5% (70) | 53.5% (23) | 0.305 | |
| Histologic chorioamnionitis | 25.0% (28) | 18.6% (8) | 0.399 | |
| Neonatal sepsis | 1.8% (2) | 0% (0) | ||
Data are presented as median (interquartile range) or as % (n). ACS, antenatal corticosteroid.
In total, 155 singleton late preterm neonates were administered ACS in the early
preterm period due to expected birth but did not actually deliver (before 34 + 0
weeks of gestation). Among these, 27.8% (43/155) received rescue ACS after 34
weeks of gestation, while the remaining 72.2% (112/155) did not receive further
rescues ACS. Neonates who did not receive further late preterm rescue ACS had a
significantly higher frequently of RDS than those who did (0% with late preterm
ACS vs. 10.7% without late preterm ACS, p = 0.038). There were
no significant differences between the two groups in the frequencies of TTN
(25.6% vs. 42.0%, p = 0.089), hypoglycemia (glucose level
Patients were divided into two groups according to whether they experienced RDS: 143 patients did not experience RDS, whereas 12 did (Table 2). The gestational age at initial ACS administration and the gestational age at delivery was not different between the two groups (p = 0.118 for 32.4 weeks vs. 31.0 weeks and = 0.605 for 34.6 weeks vs. 35.2 weeks). The rate of rescue steroid administration was significantly lower in neonates with RDS than in those without RDS (0% [0/12] vs. 30.1% [43/143], p = 0.038). Other outcomes such as gestational age at delivery were not different between the two groups.
| Respiratory distress syndrome | p-value | |||
| Absent (n = 143) | Present (n = 12) | |||
| Maternal age (years) | 34.0 (31.0–36.0) | 35.0 (31.0–36.0) | 0.480 | |
| Nulliparity | 58.7% (84) | 50.0% (6) | 0.556 | |
| Hypertensive disorder of pregnancy | 39.2% (56) | 16.7% (2) | 0.213 | |
| Gestational diabetes | 15.4% (22) | 16.7% (2) | 1.000 | |
| Gestational age at initial ACS administration (weeks) | 32.4 (31.0–33.2) | 31.0 (30.3–32.9) | 0.118 | |
| Indication for initial ACS administration | ||||
| Spontaneous preterm birth | 50.3% (72) | 41.7% (5) | 0.563 | |
| Medically indicated preterm birth | 49.7% (71) | 58.3% (7) | ||
| Rescue steroid administration | 30.1% (43) | 0% (0) | 0.038 | |
| Gestational age at delivery (weeks) | 34.6 (34.1–35.4) | 35.2 (34.2–35.3) | 0.605 | |
| Vaginal delivery | 36.4% (52) | 16.7% (2) | 0.218 | |
| Sex (male) | 60.8% (87) | 50.0% (6) | 0.462 | |
| Birthweight (grams) | 2260 (2025–2600) | 2413 (2214–2820) | 0.099 | |
| 1-min Apgar score |
20.3% (29) | 41.7% (5) | 0.085 | |
| 5-min Apgar score |
3.5% (5) | 16.7% (2) | 0.093 | |
| Hypoglycemia, glucose level |
7.7% (11) | 16.7% (2) | 0.265 | |
| Hypoglycemia, glucose level |
49.0% (70) | 41.7% (5) | 0.628 | |
| Histologic chorioamnionitis | 24.5% (35) | 8.3% (1) | 0.297 | |
| Neonatal sepsis | 0.7% (1) | 8.3% (1) | 0.149 | |
Data are presented as median (interquartile range) or as % (n). ACS, antenatal corticosteroid.
When the patients were classified according to whether they experienced
hypoglycemia (glucose level
| Hypoglycemia (glucose level |
p-value | |||
| Absent (n = 142) | Present (n = 13) | |||
| Maternal age (years) | 34.0 (31.0–36.0) | 33.0 (30.0–36.5) | 0.648 | |
| Nulliparity | 58.5% (83) | 53.8% (7) | 0.747 | |
| Hypertensive disorder of pregnancy | 38.7% (55) | 23.1% (3) | 0.373 | |
| Gestational diabetes | 16.2% (23) | 7.7% (1) | 0.693 | |
| Gestational age at initial ACS administration (weeks) | 32.4 (31.0–33.2) | 32.5 (29.5–33.2) | 0.730 | |
| Indication for initial ACS administration | ||||
| Spontaneous preterm birth | 49.3% (70) | 53.8% (7) | 0.753 | |
| Medically indicated preterm birth | 50.7% (72) | 46.2% (6) | ||
| Rescue steroid administration | 27.5% (39) | 30.8% (4) | 0.755 | |
| Gestational age at delivery (weeks) | 34.8 (34.1–35.4) | 35.0 (34.1–35.3) | 0.671 | |
| Vaginal delivery | 37.3% (53) | 7.7% (1) | 0.035 | |
| Sex (male) | 60.6% (86) | 53.8% (7) | 0.636 | |
| Birthweight (grams) | 2273 (2034–2635) | 2260 (2070–2383) | 0.633 | |
| 1-min Apgar score |
22.5% (32) | 15.4% (2) | 0.735 | |
| 5-min Apgar score |
4.2% (6) | 7.7% (1) | 0.465 | |
| Respiratory distress syndrome | 7.0% (10) | 15.4% (2) | 0.265 | |
| Transient tachypnea of the newborn | 36.4% (48/132) | 45.5% (5/11) | 0.549 | |
| Histologic chorioamnionitis | 25.4% (36) | 0% (0) | 0.040 | |
| Neonatal sepsis | 0.7% (1) | 7.7% (1) | 0.161 | |
Data are presented as median (interquartile range) or as % (n). ACS, antenatal corticosteroid.
As shown in Table 4, we conducted a logistic regression analysis of risk factors
for RDS and performed multivariate modeling. Variables with p
| Univariate | Multivariate | |||
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Maternal age (years) | 0.99 (0.85–1.16) | 0.898 | ||
| Nulliparity | 0.78 (0.36–4.59) | 0.698 | ||
| Hypertensive disorder of pregnancy | 0.35 (0.07–1.68) | 0.189 | 0.99 (0.21–4.66) | 0.978 |
| Gestational diabetes | 0.53 (0.06–4.31) | 0.550 | ||
| Gestational age at initial ACS administration (weeks) | 0.88 (0.69–1.12) | 0.303 | ||
| Indication for initial ACS administration | 0.83 (0.24–2.85) | 0.772 | ||
| Rescue steroid administration | 0.10 (0.01–1.76) | 0.116 | 0.07 (0.00–1.48) | 0.087 |
| Gestational age at delivery (weeks) | 1.06 (0.50–2.26) | 0.874 | ||
| Vaginal delivery | 0.39 (0.08–1.89) | 0.244 | ||
| Sex (male) | 0.53 (0.15–1.82) | 0.313 | ||
| Birthweight (grams) | 1.00 (1.00–1.00) | 0.077 | 1.00 (1.00–1.00) | 0.063 |
| 1-min Apgar score |
3.30 (0.94–11.59) | 0.062 | 3.21 (0.73–14.12) | 0.123 |
| 5-min Apgar score |
6.18 (1.05–36.38) | 0.044 | 2.36 (0.26–21.58) | 0.448 |
| Hypoglycemia, glucose level |
0.86 (0.10–7.19) | 0.889 | ||
| Hypoglycemia, glucose level |
0.35 (0.10–1.26) | 0.109 | 0.35 (0.10–1.31) | 0.119 |
| Interval initial ACS administration to delivery (days) | 1.01 (0.98–1.05) | 0.382 | ||
OR, odds ratio; 95% CI, 95% confidence interval; Multivariate modeling with inclusion of the following factors was applied:
variables with p
In this study, neonates who received late preterm rescue ACS had a lower
occurrence of RDS. Other neonatal outcomes, including TTN of the newborn and
hypoglycemia (glucose level
ACS administration may cause temporary maternal hyperglycemia, leading to fetal hyperinsulinemia and subsequent hypoglycemia [20].
In the ALPS trial, hypoglycemia (glucose level
Gyamfi-Bannerman et al. [22] re-analyzed the data of infants enrolled in the ALPS trial and reported no significant difference in the incidence of neonatal hypoglycemia between the betamethasone and placebo groups (29.3% vs. 17.3%; relative risk (RR), 1.69; 95% CI, 1.46–1.96). In addition, most cases of neonatal hypoglycemia resolved spontaneously within 24 h in both groups, and the time to resolution was shorter in the betamethasone group than that for the placebo group (2.80 h [interquartile range: 2.03–7.03] vs. 3.74 h [interquartile range: 2.15–15.08]; p = 0.002) [13].
In our study, late preterm rescue ACS was not associated with hypoglycemia
(glucose level
ACS administration accelerates alveolization by promoting normal thinning of the double capillary loops, forming thin gas-exchanging walls of alveoli, and inducing lung maturation by promoting pneumocyte II maturation and pulmonary surfactant generation [23, 24].
The efficacy of ACS in late preterm infants remains controversial, and there are
few studies on rescue ACS in late preterm infants. According to the ALPS trial,
ACS in late preterm infants reduces the risk of composite RDS, TT of the newborn,
or apnea (13.9% vs. 17.8%; RR, 0.78; 95% CI, 0.66–0.93; p =
0.004) [9]. Mansouri et al. [25] reported that the incidence of neonatal
RDS was significantly lower in the group administered betamethasone (12 mg/kg/BW
twice every 24 h) at 35–36 weeks compared to in the untreated group in a
double-blind randomized controlled trial (8% vs. 20%, p
Shanks et al. [26] conducted a randomized controlled study that
compared the surfactant-to-albumin ratio (TDx-FLM-II), a laboratory marker that
is useful for determining fetal lung maturity, depending on ACS administration in
pregnant women at 34 + 0/7–36 + 6/7 weeks. They showed that the
surfactant-to-albumin ratio (TDx-FLM-II) significantly increased in the group
exposed to ACS after 34 weeks (28.37 mg/g vs. 9.76 mg/g, p
In our study, we found that late preterm ACS might be associated with a reduced risk of RDS; however, the results were not statistically significant in the multivariate analysis (OR, 0.07; 95% CI, 0.00–1.48; p = 0.087). It is presumed that the small sample size was insufficient to obtain statistical significance. Through this study, we were not able to definitively prove whether mothers who have already received steroids once during the early preterm period, when labor is predicted, can definitely have reduced RDS or TTN by receiving rescue steroids when labor is predicted in the late preterm period. Additionally, we could not establish a correlation of late preterm ACS with increased neonatal hypoglycemia. Therefore, we believe that future large-scale studies are needed to investigate the efficacy or potential adverse effects of administering rescue steroids in women with singleton pregnancies.
Although studies on the efficacy of late preterm ACS have been actively conducted before and after the ALPS trial, there have been few studies on the efficacy of rescue ACS in late preterm infants. The major strength of our study is being the first to evaluate the benefits and side effects of rescue ACS in late preterm infants. Our findings may shed some light on rescue ACS use in late preterm infants.
However, this study had a few limitations. First, as this was a retrospective hospital-based cohort study, the number of patients who were exposed to rescue ACS in late preterm was insufficient to reach statistical significance. Further studies with a larger number of pregnant women are needed to verify the efficacy of late preterm rescue for ACS. A second potential limitation is that we only collected data from neonates within 24 h of birth. Potential long-term outcomes, such as neurodevelopmental outcomes, need to be evaluated in future studies. Third, residual disturbances due to other factors or interventions, such as fetal anomalies and antibiotic treatment, and maternal factors of gestational diabetes or pregestational diabetes were not addressed but cannot be excluded.
Administering rescue ACS in the late preterm stage may not reduce the risk of RDS among women at risk of late preterm birth who initially received ACS before 34 weeks of gestation. Additionally, it does not appear to increase the risk of neonatal hypoglycemia within the first 24 hours after birth. There has been no prior research on the use of rescue steroids in the late preterm period following the ALPS trial. Although this is a limited study, further research is needed on mothers who receive rescue ACS, specifically those who initially received ACS in the early preterm period, and more than a week has elapsed since. Further studies with larger sample sizes are needed to confirm these results and assess potential long-term implications.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
DEJ: Conceptualization, Data curation, Manuscript writing; JYL: Data curation; EJO: Data curation; KNL: Conceptualization, Data curation, Investigation, Project development, Manuscript writing, Review & editing; HK: Conceptualization, Data curation, Investigation; HJK: Conceptualization, Formal analysis, Manuscript writing; JYP, YHJ: Methodology, Formal analysis, Validation, Review & editing; KJO: Methodology, Project development, Review & editing; CWC: Validation, Review & editing. All authors contributed to editorial changes in the manuscript. All authors approved the final manuscript.
The study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-1905-540-005). The requirement for the acquisition of informed consent from the study participants was waived owing to the retrospective nature of this study.
We would like to express our deepest gratitude to everyone who assisted us during the composition of this manuscript. We particularly want to recognize the invaluable contribution of the Medical Research Collaborating Center at Seoul National University Bundang Hospital. Special thanks to Park Young Mi for her rigorous statistical analysis, which was instrumental in our research.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.