1 Franklin College, University of Georgia, Athens, GA 30606, USA
2 MG Wellness LLC, Fortson, GA 30606, USA
3 Department of Research, College of Health Science, Faulkner University, Montgomery, AL 36109, USA
Academic Editors: Shigeki Matsubara and Michael H. Dahan
Abstract
Background: Vesicovaginal fistulas are complex medical/surgical issue that may arise after obstructed labor in areas without access to maternal health care providers. In some areas, fistulas have devastating social consequences on the patient. Easier visualization of the fistula during the surgery might contribute to better surgical success. For this purpose, we describe the use of inexpensive, humble methods available in resource-limited areas. The drug phenazopyridine makes urine orange, whereby easing visualization of fistula(s) during surgery. The objective of this study was to determine the effectiveness of phenazopyridine administration in the resource limited settings. Methods: Medical record review was conducted. Data has been prospectively followed from all patients with vesicovaginal fistulas. All cases were staffed by experienced gynecologic oncologists with multiple different medical trainees (American and Ivorian) assisting. For the first 3 mission trips, no phenazopyridine was given pre-operatively. For the fourth to ninth trip, phenazopyridine was given preoperatively along with enhanced recovery medications. All patients had transurethral catheters left in place for 2 weeks that were removed by a medical professional. Imaging was not available and so success of the repair was based on patient reported symptoms after removal. Patient outcomes (subjective success by patient report) were compared between the two groups (without versus with phenazopyridine). Two-tail Chi square statistics with a significance of 0.05 were performed. Results: 53 patients with vesicovaginal fistulas arising after obstructed labor were primarily treated during nine two-week mission trips. Another 5 patients had urethral vaginal fistulas and these were not included in the report. Of the 53 patients, 9 patients also had co-existing rectovaginal fistulas that were repaired at the same time. The first group of 17 vesicovaginal fistulas (no phenazopyridine given) had a success rate of 76.5% (13/17) while the second group (phenazopyridine given) had a success rate of 97.2% (35/36) (p = 0.016). At the same time the rate of multiple vesicovaginal fistulas in the same patient changed from 5.8% (1/17) in the first group to 22.2% (8/36) (p = 0.14). Conclusions: Using phenazopyridine pre-operatively aided the surgeons in diagnosing multiple vesicovaginal fistulas more commonly and may have benefitted patients by leading to a higher surgical success rate.
Keywords
- Phenazopyridine
- Vesicovaginal fistula
- Rectovaginal fistula
- Surgery
The formation of a vesicovaginal fistula (VVF) is a devastating condition that may arise after obstructed labor in developing world including Sub-Saharan Africa [1, 2, 3]. This condition and the often-associated rectovaginal fistula (RVF) both can have devastating social conditions on top of the known physical morbidity [4]. Women with these conditions often become social pariah. Surgically correcting these issues is important physically, socially, and culturally [5]. However, resources are lacking in many developing countries in Africa to adequately repair the fistulas that are present [6, 7]. Furthermore, the fistulas present after obstructed labor may be more complex and multiple in nature than initially seen. Complex fistulas may also arise after hysterectomy and caesarean deliveries.
The objective of this analysis is to review the data regarding VVF repair before and after the routine pre-operative use of phenazopyridine during short term medical missions (STMM). Specifically, the rates of multiple VVF, the rate of surgical success, and any correlations will be presented.
The STMM was part of a larger organization which provides other health sustainable health resources, education on an ongoing basis and access to clean water. Gynecologic oncologists, each with over a decade of experience repairing complex vesico-vaginal and recto-vaginal experience were involved in all the surgeries with a two-prong goal. First to help the women of Cote d’Ivoire. Second, to train Ivorian Obstetricians in the repair of these fistulas.
The information was collected from medical records for nine 2-week medical missions in the Zanzan Region of Cote d’Ivoire 2012–2019. Data was collected for all women with genito-urinary fistulas caused by obstructed labor with or without rectovaginal fistula. Only women undergoing primary surgical closure were included. No women with failed previous closures were included in this analysis. All fistulas included in this study were repaired via a transvaginal approach. Women with obliteration of the proximal urethra or absence of the urethra were not included in this analysis. No other patients were knowingly excluded.
During the first 2 STMMs, no phenazopyridine was used pre-operatively. During the subsequent STMMs, phenazopyridine was routinely given along with other enhanced recovery pre-operative medications (Table 1). Other than phenazopyridine, these medicines are standardly used to decrease discomfort and nausea after surgery.
| Medication | Dose | Route |
| Ibuprofen | 800 mg | po |
| Acetaminophen | 1000 mg | po |
| Dexamethasone* | 4 mg | po |
| Ondansetron** | 4 mg | po |
| Gabapentin | 300 mg | po |
| Phenazopyridine | 400 mg | po |
| * sometimes substituted with prednisone 10 mg. ** when available. | ||
Each surgeon wore surgical loupes and headlight for the procedure. Each patient’s vulva and vagina were prepped (2% chlorohexidine gluconate) and draped in the dorsal lithotomy position. A sterile urinary balloon catheter was placed transurethrally into the bladder. Scar tissue was dissected first. If the location of any fistula was close to ureteral orifices as identified by the ejection of phenazopyridine then pediatric feeding tubes were placed as stents into both ureters and sewn to the urinary catheter with 4-0 to allow easy removal with removal of the urinary catheter. No cystoscopic equipment was available in the mobile surgical unit in upcountry Cote d’Ivoire. The bladder and vagina were dissected to separate the layers. The fistula tract(s) were excised with micro-Castroviejo scissors to remove just the bladder mucosal edges. The bladder mucosa was closed with a running 3-0 polyglactin suture. Interrupted sutures of 3-0 polyglactin were then used to close bladder muscle over the mucosal suture line. For large defects, a bulbocavernosus flap was tunneled from either the patient’s right or left as determined by patient anatomy and surgeon preference. The flap was tunneled under mobilized vagina mucosa and anchored between bladder and vagina with 2-0 polyglactin suture. Vaginal mucosa was further mobilized to allow tension free closure in different direction than bladder closure. Vaginal tissue closure was performed with a running 3-0 polyglactin suture. When used, the site of bulbocavernosus dissection was closed with deep interrupted sutures of 2-0 polyglactin followed by mucosal closure in a running manner with 3-0 polyglactin or 3-0 poliglecaprone. All patients undergoing vesico-vaginal repair had their repair checked after completion by backfilling the urinary bladder with a dyed solution (either indigo carmine or methylene blue depending on availability).
Transurethral catheters were used for all patients and removed 14 days after the
procedural (by a nurse practitioner). In patients with stents, all were
successfully removed with removal of catheter. Success of surgery was determined
by patient’s subjective self-assessment after voiding after removal of the
transurethral catheter. Patients were again seen greater than 6 weeks after
surgery to evaluate condition. Data was compiled and analyzed by Chi-squared test
with SPSS (v27, IBM, Armonk, NY, USA) with an alpha = 0.05. Fisher’s exact test
was used to compare proportions when
Fifty-three women underwent treatment for previously untreated VVF caused by obstructed labor. The average operating time across all cases was 55 minutes with 95% CI (34.9, 75.1). The length of time with living with a fistula for the whole study population was 6.2 years 95% CI (5.6, 6.8). Group 1 women had been living with a fistula for an average of 5.7 years 95% CI (4.9, 6.3) while group 2 women had been living with a fistula for a mean of 6.4 years 95% CI (5.6, 7.2) (p = 0.59).
The first seventeen of these women were not given phenazopyridine, while during the subsequent STMMs, 36 women were given phenazopyridine one half hour to hour before surgery. The overall success rate was 91% (Fig. 1). The success rate repairing the fistula was 76.5% (13/17) for the first group, and 97.2% (35/36) (p = 0.016) for the second group (Fig. 1).
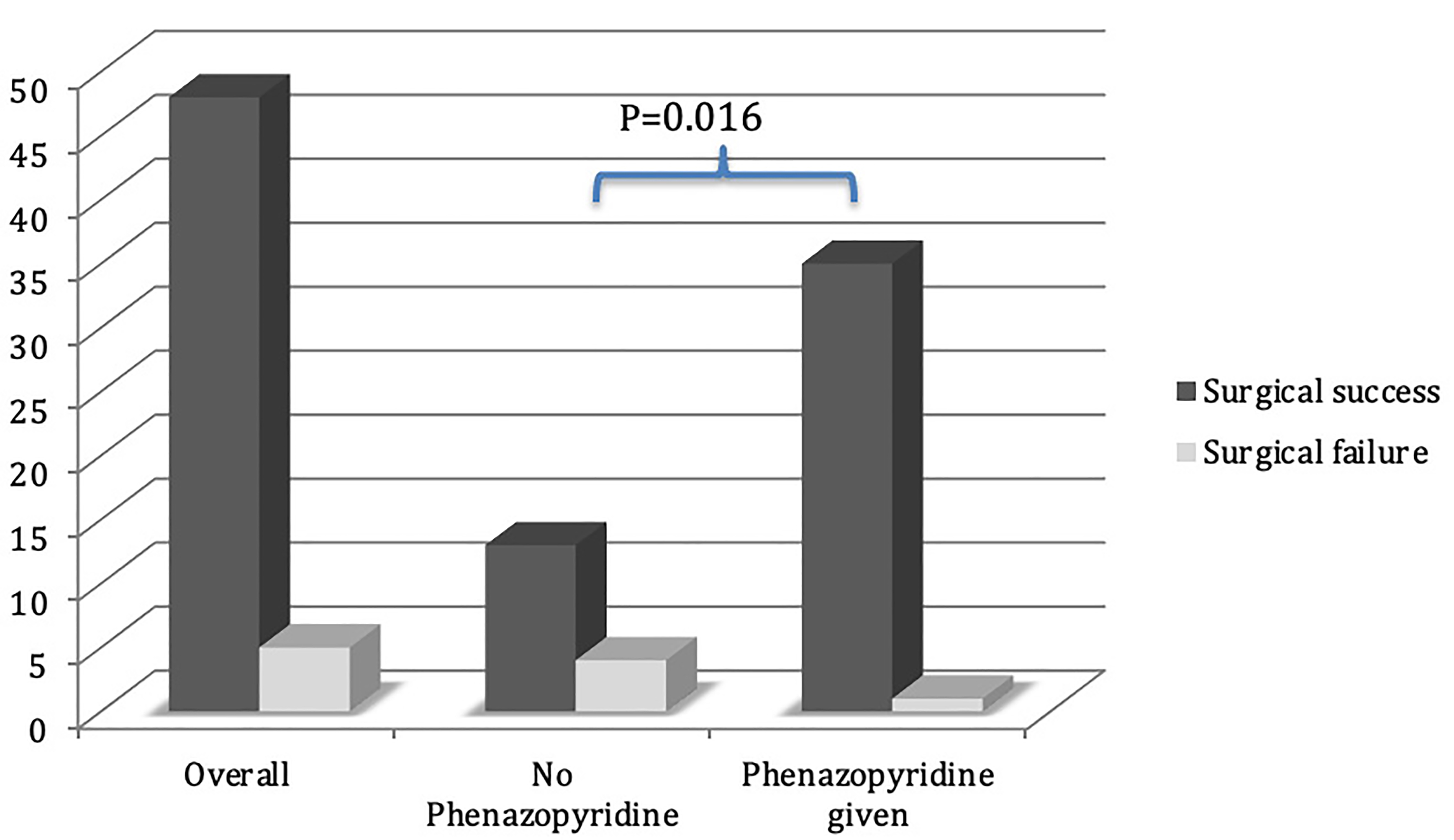 Fig. 1.
Fig. 1.Comparison of surgical success with or without phenazopyridine.
The number of multiple fistula patients in the first group is unknown. Seven of 36 (19.4%) in the phenazopyridine treated group had multiple fistulas in the lower genital tract. When multiple fistulas were detected at surgery, all detected fistula were repaired in that surgery.
Phenazopyridine is an oral pharmacologic agent used to relieve lower urinary tract symptoms including: irritation, pain, burning, urgency and frequency. It is not an antibiotic and only relieves symptoms. It has the side effect of causing urine to discolor orange because of the delocalization of electrons found in the 2 aromatic rings (Fig. 2). This side effect is advantageous because it allows defects in the lower urinary tract to be readily seen on vaginal examination.
 Fig. 2.
Fig. 2.Phenazopyridine 2D structure.
Since this is just an observational study and not a randomized controlled trial, the increased surgical success from the introduction of pre-operative phenazopyridine to see multiple fistulas cannot be definitively accredited to the phenazopyridine. Other causes could include increased awareness of multiple fistulas. Increased surgical skill is also a possibility; however, the gynecologic oncologists involved in this study already had greater than a decade of surgery performing greater than 200 complex genito-urinary repairs (obstetric or gynecologic vesicovaginal) and enterovaginal repairs (over 100 each). Other confounders cannot be ruled out or discredited; however, identification of multiple fistulas is still an important fact since they appear to be common (19.4%). With the ability to identify patients who need multiple repairs, and not just one repair, more patients can be helped to have these physical defects corrected and hopefully return to desired social roles. Although these findings of this study may have no role in resource rich area, these techniques may be helpful to the gynecologist repairing fistula(s) in resource poor areas.
With the goal of short-term medical missions being to provide sustainable care for those being treated, using a safe simple method to easily identify multiple fistulas when present is an important treatment adjuvant. Not all medical providers in remote areas of underdeveloped countries have access to technology available in developed countries. Therefore, it is important to have simple safe options available.
MG wrote the manuscript and helped gather the data. KM hypothesized the experiment and helped write the paper. JG analyzed the data and helped write the paper. All authors read and approved the final manuscript.
The study was conducted in accordance with the Declaration of Helsinki, and the protocol for the retrospective review was approved by the Ethics Committee of Faulkner University (approval number: 21-08011). As this was a retrospective study, no informed consent was necessary.
We would like to express my gratitude to all those who helped me during the writing of this manuscript. Thanks to all the peer reviewers for their opinions and suggestions.
This research received no external funding.
The authors declare no conflict of interest. JG is serving as one of the Editorial Board members of this journal. We declare that JG had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to MHD and SM.


