1 Molecular and Pharmaco-Epidemiology Unit, Department of Experimental Oncology, IEO, European Institute of Oncology IRCCS, 20139 Milan, Italy
2 Department of Health Sciences, San Paolo Hospital Medical School, University of Milan, 20100 Milan, Italy
3 PeaRL – Perinatal Research Laboratory, Department of Neurosciences, University of Florence, 50121 Florence, Italy
4 CiaoLapo Foundation for Perinatal Health, Stillbirth and Perinatal Loss Support, 59100 Prato, Italy
5 Department of Neurosciences, Psychology, Drug Research and Child Health, University of Florence, 50121 Florence, Italy
6 TOMA Advanced Biomedical Assays S.p.A., 21052 Busto Arsizio, Varese, Italy
7 Egeria Medical Center, 20122 Milan, Italy
†These authors contributed equally.
Academic Editor: Luca Roncati
Abstract
Background: Stillbirth is a worldwide devastating adverse pregnancy
outcome and specific maternal conditions have been associated with an increased
risk of fetal death. However, despite the worldwide increased efforts in
prevention of stillbirth, little improvements have been achieved in recent years.
Our aim was to explore the role of maternal conditions that can be ascertained at
the beginning of pregnancy (i.e., demographic and medical conditions/diseases)
and estimate their contribution to antepartum stillbirth. An early identification
of risk factors could offer to high-risk pregnancies a tailored antenatal
surveillance by trained staff leading to a potential reduction of stillbirth
rates. Methods: Retrospective case-control study in singleton
pregnancies. The difference between fetal survival rates in women with or without
risk factors was evaluated. Results: Antepartum stillbirth occurs more
frequently in infertile, older women, with systemic diseases. Maternal conditions
may affect fetal outcome in a time-dependent manner. Subdividing cases in early
stillbirths (before 28 weeks of gestation) and late stillbirth (
Keywords
- stillbirth
- gestational age
- diabetes
- hypertension
- autoimmunity
- thrombophilia
- obesity
The death of the fetus during the intrauterine life is a dramatic and devastating event of any affected pregnancy, irrespective of the duration of the gestation. More than 2.5 million stillbirths have been reported worldwide when applying the 28-weeks gestational age cut-off suggested by the World Health Organization for international comparison [1]; however, when applying the lower limit of 20 weeks, the number of fetal deaths would more than double [2]: half of stillbirths occur before 28 weeks of gestation [3], with an overall estimation of five to six million stillbirths annually [4].
Although stillbirth may occur during an otherwise apparently uneventful pregnancy, some maternal conditions/diseases have been identified as able to increase the risk of fetal death [5]. These worldwide diffuse maternal conditions include obesity [6], pre-pregnancy hypertension and diabetes, especially when associated with advanced maternal age [7, 8]. In accordance with the global trends, in Italy these maternal risk factors have been increasing in the last years [9] leading to a wider number of women potentially at “high-risk pregnancy”. Ideally, high quality antenatal care should identify and address the maternally related stillbirth risk factors at the beginning of any pregnancy [3, 8], to offer a personalized plan for high quality care during gestation [8], avoiding preventable stillbirths. Nevertheless, in the last few years the reduction of stillbirth rates has been lower than what we hoped for [7] and ending preventable stillbirths still remains an unreached goal [8]. Correctly targeting the pregnancy as low versus high risk is crucial for the prevention of adverse pregnancy outcomes [10]. Therefore, our purpose is to explore the role of maternal conditions that can be ascertained at the beginning of pregnancy (i.e., demographic and medical conditions/diseases) and estimate the respective contribution of these conditions to stillbirth. An early identification of risk factors could offer to high-risk pregnancies a specific antenatal surveillance by trained staff [11] leading to a potential reduction of stillbirth rates.
This was a retrospective case-control study of antepartum stillbirths in singleton pregnancies that occurred in a University Care Center in Northern Italy over 30 years before the COVID-19 pandemic (years 1987–2017). The Unit can provide antenatal, intrapartum and post-partum care to low risk and moderate-high risk pregnancies, with Obstetrics-Gynecology (Ob-Gyn), Anesthesiologist and Neonatologist (but not neonatal intensive care unit) physically present at all times and full complements of subspecialists readily available at all times for inpatients consultation; in-house availability of all of blood components; onsite availability of maternal intensive care unit. The average annual birth rate in the study period was 1824 deliveries/year (range 1561–2187).
Stillbirth was defined as spontaneous intrauterine fetal death which occurred before the onset of labor at 20 or more completed weeks of gestation. Deliveries resulting from legal terminations of pregnancy were excluded. 429 singleton stillbirths were eligible for the study.
Maternal characteristics and gestational age at delivery were retrospectively obtained from routinely collected, anonymized data from the obstetric clinical database of the San Paolo Hospital Medical School in Milan, Italy.
Maternal pre-pregnancy body mass index (BMI) was calculated according to the
standard formula (kg/m
Maternal autoimmune diseases include systemic conditions associated with the presence of autoantibodies i.e., systemic lupus erythematosus and antiphospholipid syndrome.
Inherited thrombophilia includes factor V Leiden mutation (FVL G1691A), prothrombin gene mutation (PGA G20210A), Methylenetetrahydrofolate reductase gene mutation (MTHFR C677T and/or A1298C) associated with hyperhomocysteinemia, protein C deficiency, protein S deficiency, and antithrombin deficiency.
Controls were randomly selected (by using the proc surveyselect of SAS software version 9.4 (SAS®, Milano, Italy), stratifying by 30-years study period) among women who delivered in the same period as cases with a 1:4 case:control rate. A two-sided log rank test with an overall sample size of 2145 subjects (of which 30% have at least one risk factor) achieves 100% power at a 0.05 significance level to detect a difference of 10% in the survival rates between the groups of exposed and unexposed subjects, assuming a survival proportion at the end of pregnancy of 80% in the exposed group (as indicated in the present case:control study). With the same assumptions, statistical power was 89% to detect a smaller difference of 5% between the two groups.
Baseline characteristics of the study population (i.e., maternal conditions that can be ascertained at the beginning of pregnancy) were expressed as median and interquartile range for continuous variables and as frequency and percentage for categorical variables.
Since Kolmogorov-Smirnov test suggested a non-normal distribution for the continuous variables included in the present study (BMI and maternal age), non-parametric tests were used. At univariate analysis, baseline maternal characteristics were compared between cases and controls with the Wilcoxon two-independent samples test for continuous variables and the Chi Square test for categorical variables.
Survival was measured from the 20th week of gestation to the date of delivery both for stillborn and liveborn fetuses. The difference between fetal survival rates for women with or without any of the considered risk factors was evaluated with the Log-Rank test, and the corresponding survival curves were plotted.
Since hazards in most curves were not proportional, we did not calculate hazard ratios for the whole period of gestation, but we defined early and late stillbirth as any stillbirth occurring up to 27.6 and from 28 weeks of gestation, respectively.
We calculated the risk of any, early and late stillbirth predictable by maternal risk factors at baseline by using univariate and multivariate unconditional logistic regression in order to calculate Odds Ratio (OR) with 95% Confidence Intervals (CI). Multivariate logistic models included as covariates the characteristics that were associated with stillbirth at univariate analysis.
To investigate the cumulative risk according to the presence of one or more baseline maternal risk factors, we plotted survival curves for subjects with no, one, two and three or more risk factors at baseline and calculated the corresponding Log-Rank test. The OR and 95% CI according to the number of risk factors was calculated as well by using unconditional logistic regression.
p values
Table 1 summarizes the maternal characteristics, known at the beginning of
pregnancy, in cases and controls. As detailed in the table, maternal age was
higher in stillbirths than livebirths (median 33 years [interquartile range
29–36] in cases; median 32 years [interquartile 28–35] in controls; p
= 0.005), as well as maternal body mass index (median 23 kg/m
| Characteristic | Cases (N = 429) | Controls (N = 1716) | p-value |
|---|---|---|---|
| N (%) | N (%) | ||
| Maternal age (years) | 33 (29–36) | 32 (28–35) | 0.005 |
| Maternal pre-pregnancy BMI | 23 (21–26) | 22 (20–25) | 0.02 |
| Obesity (BMI |
26/183 (14%) | 122/1716 (7%) | 0.0007 |
| Autoimmune disease | 13/429 (3%) | 13/1716 (1%) | 0.0001 |
| Inherited Thrombophilia | 14/429 (3%) | 26/1716 (2%) | 0.02 |
| Pre-gestational diabetes (IDDM) | 6/429 (1%) | 5/1716 (0%) | 0.004 |
| Pre-gestational hypertension | 8/429 (2%) | 12/1716 (1%) | 0.02 |
| Overt Hypothyroidism | 11/429 (3%) | 48/1716 (3%) | 0.79 |
| Overt Hyperthyroidism | 5/429 (1%) | 9/1716 (1%) | 0.14 |
| Pre-gestational systemic infections | 8/429 (2%) | 24/1716 (1%) | 0.48 |
| Asthma | 3/429 (1%) | 20/1716 (1%) | 0.40 |
| Epilepsy | 4/429 (1%) | 28/1716 (2%) | 0.29 |
| Assisted reproductive technologies | 16/429 (4%) | 26/1716 (2%) | 0.003 |
| Note: significant p-values are in italic. p values were obtained by Wilcoxon two-independent samples test or Chi Square test, as appropriate. Data as exposed as number (percentage) or Median (Interquartile Range), as appropriate. Missing data for maternal age (only cases) = 20/429 (5%); missing data for maternal BMI (only cases) = 247/429 (58%). BMI, body mass index; IDDM, insulin dependent diabetes mellitus. | |||
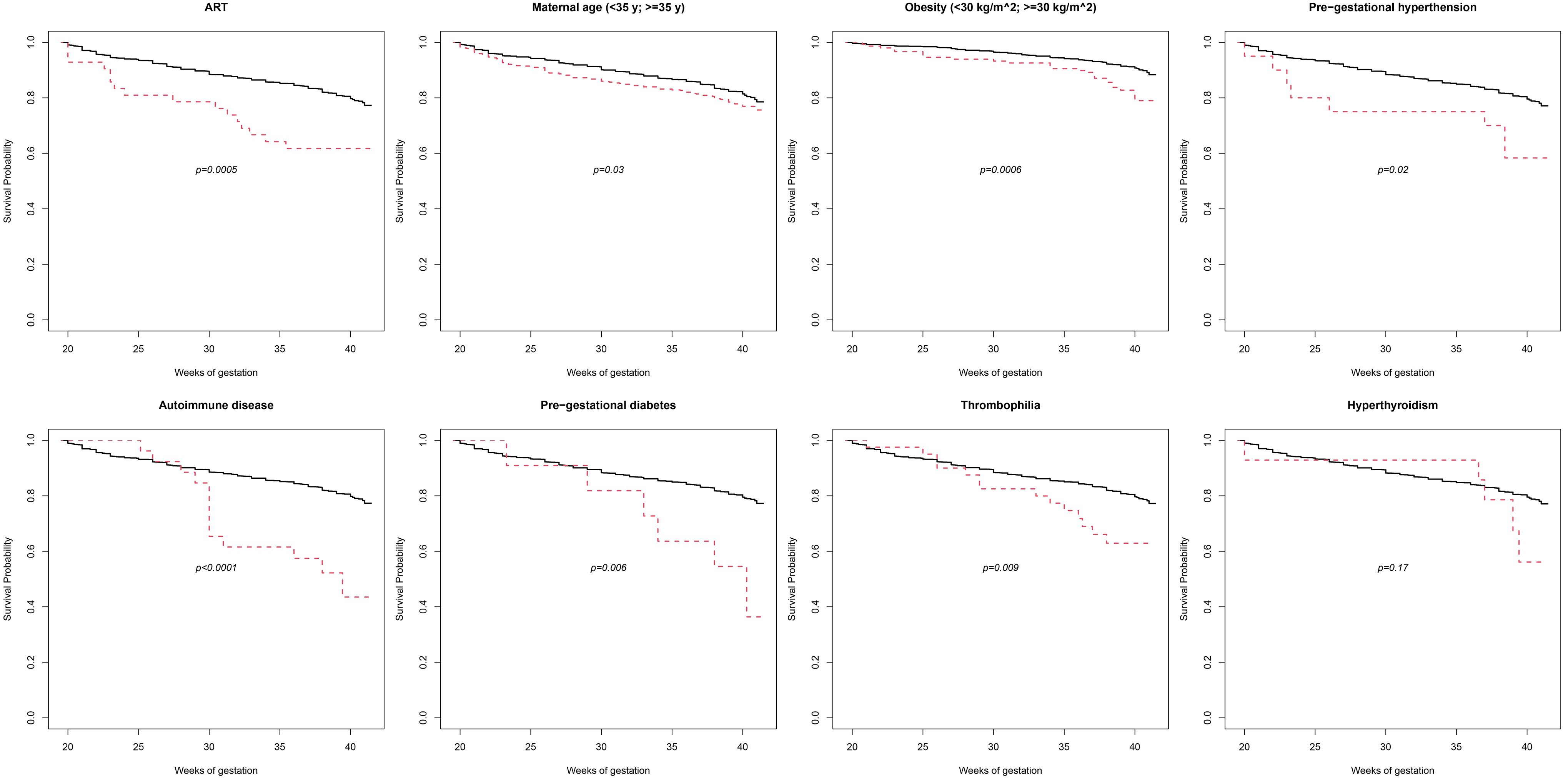
We assessed the effect of these significant factors by measuring the number of fetuses that survived. The survival probability at any weeks of gestation was calculated from twenty weeks of gestation and the total probability of survival are shown in Fig. 1.
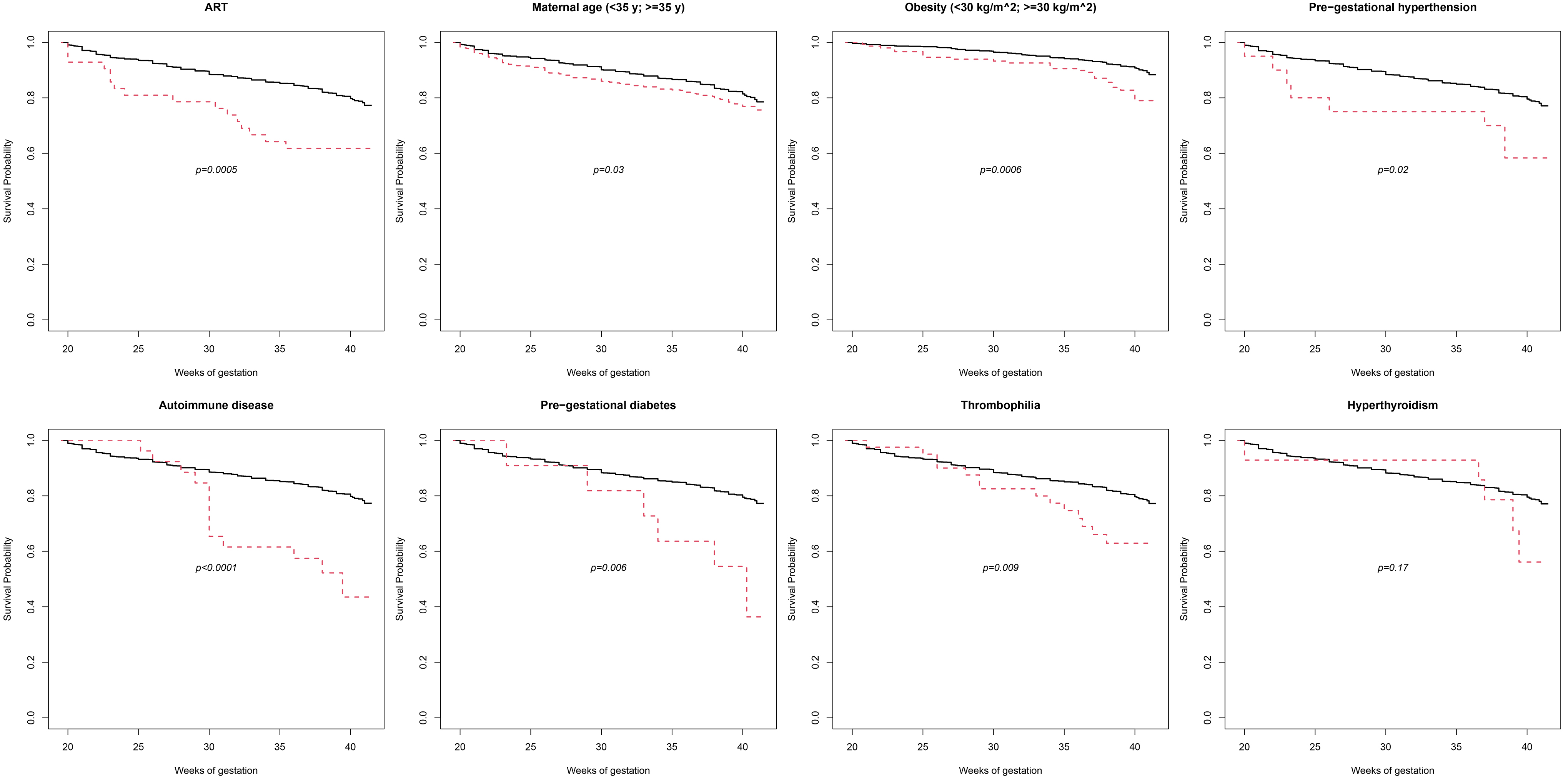 Fig. 1.
Fig. 1.Survival curves plotted according to the presence (dashed red line) or absence (solid black line) of maternal features. p-value was evaluated with the Log-Rank test and represents fetal survival rates for women with or without any of the considered risk factors. ART, assisted reproductive technologies; y, years.
Interestingly, some factors showed a significant increased risk for stillbirth at any gestational age (i.e., assisted reproductive technologies, maternal age above 35 years, obesity, pre-gestational hypertension), whereas other factors seemed to significantly increase stillbirth risk as advancing gestational age, starting from the third trimester of pregnancy: autoimmune disease, inherited thrombophilia and pre-gestational diabetes were associated with a rapid reduction of survival probability from 28 weeks of gestation. Survival curves for hyperthyroidism were apparently similar through all the gestation, but surprisingly they separate at the end of pregnancy.
The OR for stillbirth through all gestation were evaluated (Table 2):
significant stillbirth risk factors were assisted reproductive technologies (OR
2.52; 95% CI 1.34–4.74), obesity (OR 2.16; 95% CI 1.37–3.41), autoimmune
disease (OR 4.09; 95% CI 1.88–8.90), inherited thrombophilia (OR 2.19; 95% CI
1.14–4.24), pre-gestational diabetes (OR 4.85; 95% CI 1.47–15.98) and
pre-gestational hypertension (OR 2.70; 95% CI 1.10–6.64). Interestingly,
subdividing cases in early stillbirths (before 28 weeks of gestation) and late
stillbirth (
| Characteristics | Univariate | Multivariate |
| OR (95% CI) | OR (95% CI) | |
| ALL | ||
| Maternal age |
1.24 (0.99–1.56) | - |
| Obesity (BMI |
2.16 (1.37–3.41) | - |
| Maternal age (years) | 1.03 (1.01–1.05) | 1.02 (1.00–1.04) |
| BMI | 1.05 (1.01–1.08) | - |
| Autoimmune disease | 4.09 (1.88–8.90) | 4.24 (1.94–9.23) 3.56 (1.58–8.06) |
| Inherited Thrombophilia | 2.19 (1.14–4.24) | 2.29 (1.18–4.43) 2.28 (1.18–4.43) |
| Pre-gestational diabetes (IDDM) | 4.85 (1.47–15.98) | 4.28 (1.25–14.63) 4.26 (1.24–14.58) |
| Pre-gestational hypertension | 2.70 (1.10–6.64) | 2.15 (0.83–5.60) 2.25 (0.86–5.83) |
| Overt Hypothyroidism | 0.91 (0.47–1.78) | - |
| Overt Hyperthyroidism | 2.24 (0.75–6.71) | - |
| Pre-gestational infections | 1.34 (0.60–3.00) | - |
| Asthma | 0.60 (0.18–2.02) | - |
| Epilepsy | 0.57 (0.20–1.63) | - |
| Assisted reproductive technologies | 2.52 (1.34–4.74) | 2.63 (1.39–4.95) 2.50 (1.32–4.76) |
| EARLY STILLBIRTHS ( | ||
| Maternal age |
1.59 (1.17–2.17) | 1.53 (1.12–2.09) |
| Obesity (BMI |
2.61 (1.25–5.47) | - |
| Maternal age (years) | 1.04 (1.01–1.07) | 1.03 (1.01–1.06) |
| BMI | 1.06 (1.01–1.12) | - |
| Autoimmune disease | 1.34 (0.30–5.97) | - |
| Inherited Thrombophilia | 1.34 (0.46–3.88) | - |
| Pre-gestational diabetes (IDDM) | 1.74 (0.20–14.94) | - |
| Pre-gestational hypertension | 3.68 (1.28–10.56) | 3.99 (1.38–11.51) 3.88 (1.35–11.18) |
| Overt Hypothyroidism | 1.46 (0.68–3.14) | - |
| Overt Hyperthyroidism | 0.96 (0.12–7.64) | - |
| Pre-gestational infections | 1.83 (0.69–4.84) | - |
| Asthma | 0.43 (0.06–3.22) | - |
| Epilepsy | 0.62 (0.15–2.60) | - |
| Assisted reproductive technologies | 3.10 (1.43–6.71) | 2.83 (1.30–6.20) 2.80 (1.28–6.14) |
| LATE STILLBIRTHS ( | ||
| Maternal age |
0.98 (0.72–1.34) | - |
| Obesity (BMI |
1.98 (1.15–3.41) | - |
| Maternal age (years) | 1.02 (0.99–1.04) | - |
| BMI | 1.04 (1.00–1.08) | - |
| Autoimmune disease | 6.55 (2.90–14.8) | 6.43 (2.81–14.70) |
| Inherited Thrombophilia | 2.94 (1.40–6.18) | 3.16 (1.50–6.65) |
| Pre-gestational diabetes (IDDM) | 7.57 (2.17–26.35) | 8.22 (2.36–28.64) |
| Pre-gestational hypertension | 1.87 (0.52–6.67) | - |
| Overt Hypothyroidism | 0.46 (0.14–1.48) | - |
| Overt Hyperthyroidism | 3.34 (1.02–10.94) | 2.62 (0.74–9.28) |
| Pre-gestational infections | 0.93 (0.28–3.11) | - |
| Asthma | 0.74 (0.17–3.19) | - |
| Epilepsy | 0.53 (0.12–2.22) | - |
| Assisted reproductive technologies | 2.03 (0.87–4.73) | - |
| Note: significant ORs and p-values are in Italic. BMI, body mass index; IDDM, insulin dependent diabetes mellitus. | ||
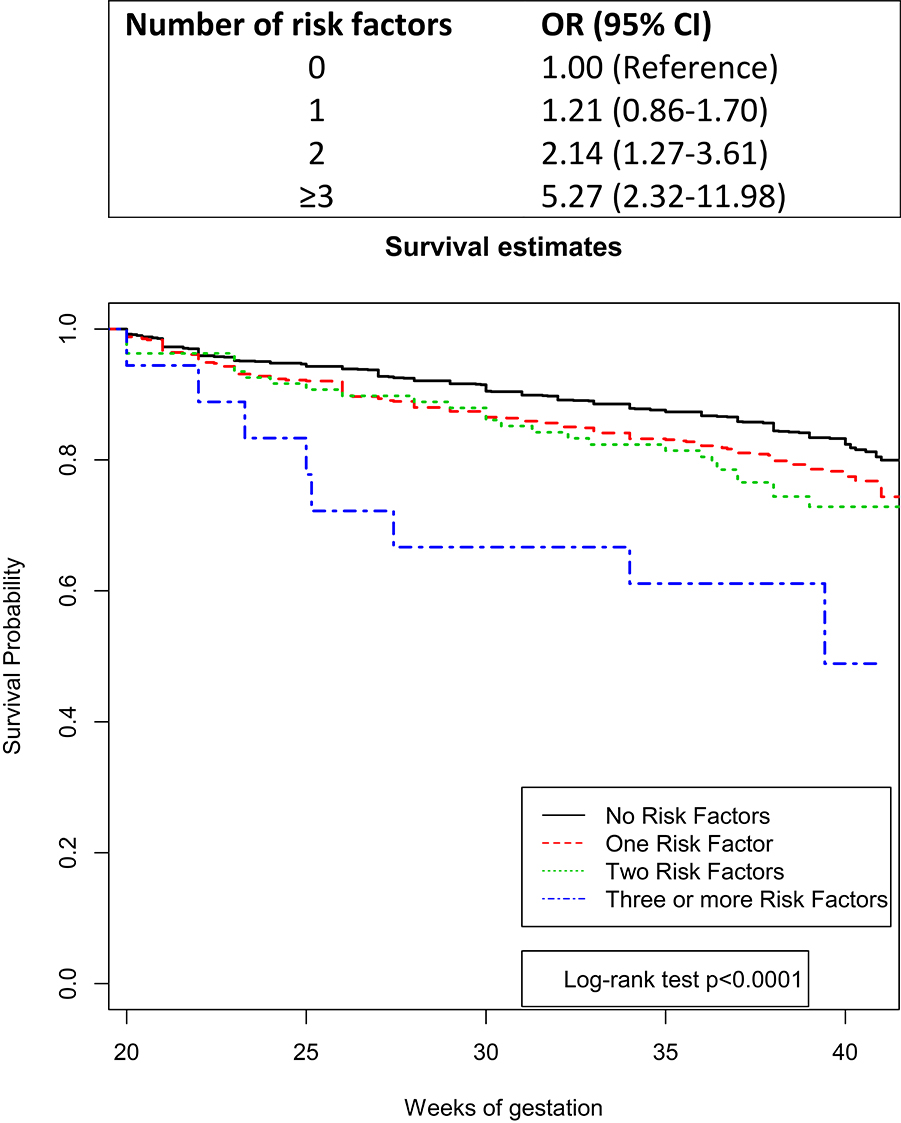
Finally, we evaluated the cumulative burden of stillbirth risk factors according to the number of conditions affecting pregnant women. Fig. 2 shows the OR and the 95% CI for stillbirth in women with and without risk factors. Notably, the risk of stillbirth increases with the increasing of the number of factors affecting the mother. Analyzing the survival proportion of cases during pregnancy according to the number of risk factors, we observed that pregnancies were affected more severely and earlier as the number of abnormal maternal conditions increased (Fig. 2).
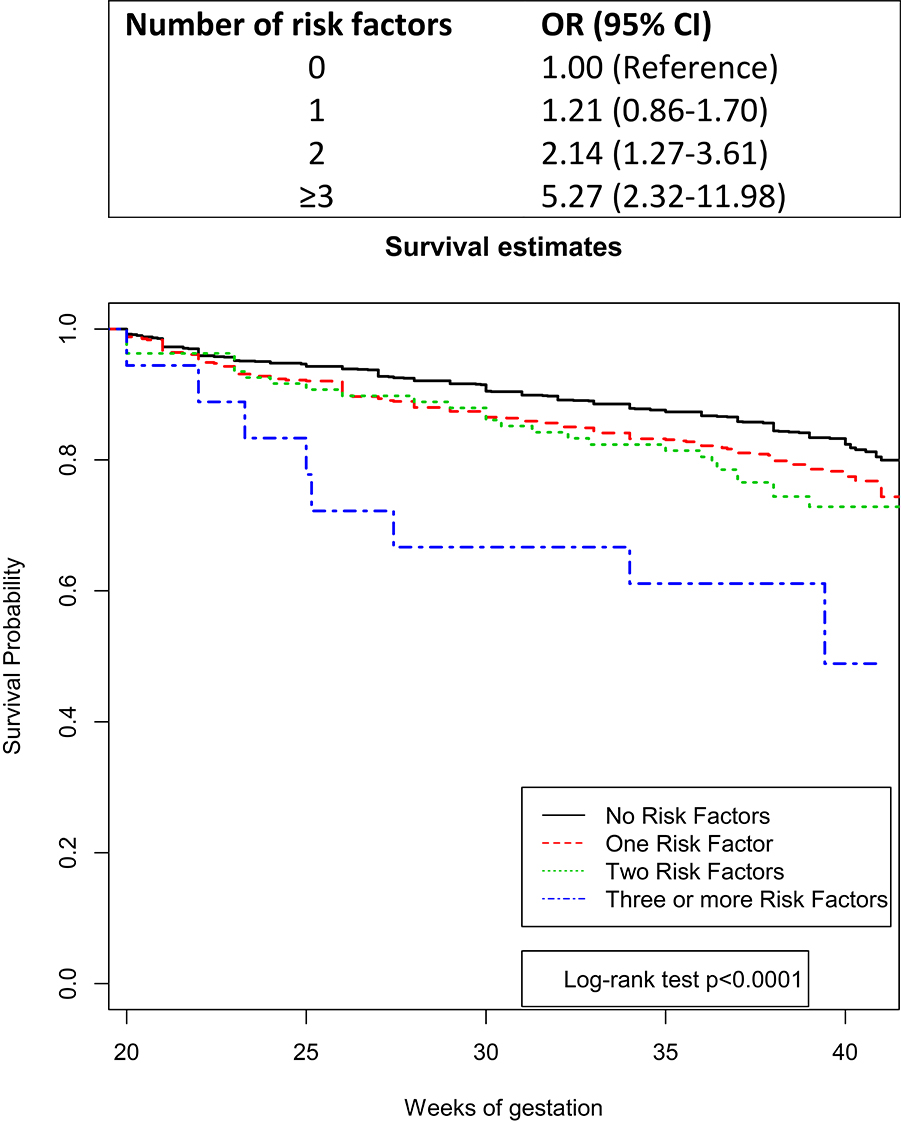 Fig. 2.
Fig. 2.Cumulative risk of stillbirth according to the presence of one or more baseline maternal risk factors. Fetal survival curves were plotted for pregnancy from mothers with none, one, two and three or more risk factors at baseline. Log-Rank test was used to calculated p-value.
The association between maternal risk factors and stillbirth is well established in the medical literature [1, 3, 5, 12]. Our data confirm that stillbirth occurs more frequently in infertile older mothers, in women with high body mass index and in women with high prevalence of diseases, such as diabetes and hypertension. Other retrospective investigations performed utilizing data that have been collected over 30 years like ours, highlighted the importance of understanding the maternal characteristics associated with stillbirth nowadays, as modern predictors of stillbirth risk [13]. Although many risk factors for stillbirths become apparent late in pregnancy, many maternal conditions can be ascertained and addressed early in pregnancy [14, 15], recognizing and potentially preventing their contribution to the adverse fetal outcome. Our results about the increasing of the risk of stillbirth associated with advanced maternal age and maternal diseases are in agreement with previous studies performed in the United States and United Kingdom aimed at identifying maternal risk factors known at the beginning of pregnancy [14, 16]. Accordingly, Yerlikaya et al. [16] provided an algorithm for prediction of stillbirth, developed on a model based on maternal characteristics and medical history recorded in early pregnancy. They stated that this model based on an early recognizing of risk factors can potentially predict one-third of subsequent stillbirths [16]. However, different geographic area may show different stillbirths risk factors. To our knowledge, this is the first Italian study that evaluates the role of maternal baseline characteristics as risk factors of stillbirth addressable at pregnancy confirmation. Moreover, the specific timeframe when these early ascertainable factors represent a significantly higher danger to the fetus needs more research worldwide. The present study stratifies the risk of stillbirth according to the baseline maternal conditions and the gestational age (before and after the 28th weeks of gestation).
The strength of our study is that we have focused our attention on baseline maternal conditions known at the beginning of pregnancy. This is a useful moment to plan effective antenatal care in any women-centered facility. The early awareness of risk factors may contribute to accelerated progress towards the prevention of stillbirths, for example by planning a specific and personalized antenatal surveillance by trained staff.
However, our study has some limitations: firstly, we utilized data that has been
collected over 30 years, where there have been several changes in obstetric
protocols and guidelines; this may have influenced the outcomes studied. However,
the comparison between stillbirths and a large controls group of livebirths
delivered in the same years limits the potential bias. In fact, the same
antenatal care was offered to both groups. Moreover, our previous study,
performed in the same study period, subdivided the population into different
study sub-periods, in order to evaluate the prevalence in time and the
association with stillbirth of the identified risk factors [9]. In that study we
observed an increasing of the prevalence of women aged
Secondly, the study is retrospective which can lead to information being largely missed or not collected (such as ethnicity/racial origin, patterns of migration, smoking etc.). Thirdly, the study took place in a single maternity hospital which might reduce the generalizability of our results. However, many similarities between maternal risk factors observed in our cases were found in published literature from around the world [3, 5, 12], supporting the reliability of our data. Moreover, a mono-center study allows the homogeneity of pregnancy care between cases and controls.
Interestingly, our results highlight that maternal conditions can affect fetal outcome in a time-dependent manner.
Some conditions (i.e., pre-gestational hypertension and assisted reproductive technologies) represent a risk factor early in pregnancy while others (i.e., autoimmune disease, inherited thrombophilia, insulin dependent diabetes mellitus) manifest their effect mainly late in pregnancy.
Autoimmune diseases are known conditions that can affect fetal outcomes, including an increased risk of fetal death [17, 18, 19, 20]. To improve the pregnancy outcome, it is important to individualize the correct risk profile for each woman [21]. Medical literature suggests that an accurate management of the mother (ideally starting at the preconception or at least at the beginning of pregnancy), will influence and optimize the fetal outcomes [21]. Close monitoring during pregnancy is an essential strategy to improve the placental functions [21] and, in turn, ending potentially preventable stillbirth. Our data suggest that the highest increase of the risk of fetal death starts from the 28th weeks of gestation. Therefore, from this gestational age is crucial to maintain a strict follow-up of the pregnancy affected by maternal autoimmune diseases.
Inherited thrombophilia is a disorder associated with an increased predisposition to developing thromboembolism including in the placenta vessels. Nevertheless, there is conflicting evidence with respect to the presence and the strength of associations between inherited thrombophilia and adverse pregnancy outcomes [22, 23, 24]. Previous studies observed an association between protein S deficiency, heterozygous for factor V Leiden or prothrombin gene and stillbirth [25]. However other studies have failed to demonstrate such association [23]. Moreover, conflicting results are available about the therapy, concluding that antithrombotic treatment appears unable to modify pregnancy outcome [23]. Our data show an increased prevalence of inherited thrombophilia in stillbirths than in livebirths, with a significant reduction in the fetal survival rate from the third trimester. We are aware that the thrombophilic defect found in mother of stillborn babies may not be viewed as the cause of the adverse pregnancy outcome but just as an association. Nevertheless, the significance of our results suggests that a close monitoring of thrombofilic women during the third trimester of pregnancy may be indicated.
Pre-gestational diabetes mellitus is a known risk factors for stillbirth [26, 27]. Fetal outcomes have been related with suboptimal maternal glucose control [28]. Substantial variations between clinics have been highlighted in medical literature, regarding glycemic control and, therefore, pregnancy outcomes [28]. In Minnesota (USA) reduction of the rate of diabetes-related stillbirth was obtained thanks to distribution of education materials to caregivers and patients, to optimize maternal conditions before conception and during all pregnancy [29]. Our observations support this contest of improving awareness about diabetes suggesting that fetal outcomes may benefit from a more strictly pregnancy monitoring, especially from the 28 weeks of gestation.
Interestingly, stillbirths at term show a prompt decrease of fetal survival after 38 weeks of gestation in cases with overt hyperthyroidism, although it is not statistically significant (possibly due to the low number of cases). Pregnancy loss in women suffering from hyperthyroidism has been previously described in case series [30, 31, 32, 33, 34] and previous population-based study speculated that high thyroid hormone levels in the late pregnancy could have direct effect on the fetus, leading to stillbirth [35]. It is well known that thyroid dysfunction may affect fetal health, particularly if hyperthyroidism is associated with thyroid autoimmunity [36]: thyroid-stimulating hormone receptor antibodies are able to cross the placenta leading to life-threatening fetal hyperthyroidism [37]. Our data are in agreement with the previously observed high risk of late stillbirth in hyperthyroidism, suggesting the helpfulness of a strict monitoring of fetal wellbeing at term of pregnancy, up to considering an appropriate timing of delivery.
Finally, our data highlights that the risk of stillbirth increases with the increasing of the number of conditions affecting the mother. It is difficult to suggest general indications for the management of pregnancy in women with multiple risk factors because each disease/condition has its own features. Moreover, epidemiological results are not sufficient to provided evidence-based recommendations. Nevertheless, in agreement with previous suggestion provided by other Authors [16], our study suggests the need for achievable early awareness of maternal risk factors and personalized management of the pregnancy which would contribute to avoid preventable stillbirths. However, the extent to which this early recognizing of maternal risk factors could prevent stillbirth remains to be determined.
Our results highlight that the risk of stillbirth increases as the increasing of the number of abnormal maternal clinical conditions, in a time-dependent manner. Early awareness of the maternal conditions addressable at the beginning of pregnancy is the first step to plan evidence-based accurate and effective antenatal care; timing and type of management depend on the different diseases and comorbidities, keeping in mind that maternal risk factors may have cumulative impact on the pregnancy concurring to increase the risk of fetal death.
Conception and design of the article by LA. LA performed the literature search, drafted the manuscript, collected, and analyzed data. SR expanded the literature research, performed statistical analysis, and drafted the manuscript. GB and AMM revised database and discussed results. VM, AV and CR actively discussed results. All authors read, edited, and approved the final manuscript.
The study was exempt from code number because, according to our National Code of Clinical Research, retrospective archive studies (performed using anonymized database) do not need ethics approval. Following Italian Data Protection Act 9/2013, material previously collected for diagnostic purposes can be used for research as long as the privacy is ensured.
The authors are grateful to parents and volunteers of CiaoLapo Charity for support and inspiration. The authors are thankful to Ms Dawn Savery for helpful commenting. SR would like to thank her stillborn daughter, Elisa, to give her motivation to collaborate in the present study.
This research received no external funding.
The authors declare no conflict of interest. Anna Maria Marconi and Laura Avagliano are serving as one of the Editorial Board members and Guest editors of this journal. We declare that Anna Maria Marconi and Laura Avagliano had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to Luca Roncati.