1 Department of Cardiology, Beijing Chaoyang Hospital, Capital Medical University, 100069 Beijing, China
2 Heart Center and Beijing Key Laboratory of Hypertension, Beijing Chaoyang Hospital, Capital Medical University, 100069 Beijing, China
3 Clinical School of Thoracic, Tianjin Medical University, 300203 Tianjin, China
4 Department of Cardiology, Tianjin Chest Hospital, 300222 Tianjin, China
5 Department of Emergency, Hebei Petrochina Central Hospital, 065000 Langfang, Hebei, China
†These authors contributed equally.
Abstract
Background: For individuals with persistent stable chest pain (SCP) and
a coronary artery calcium score (CACS) of 0, it might be challenging to establish
the best risk assessment method for determining the individuals who will not
benefit from further cardiovascular imaging testing (CIT). Thus, we investigated
the CACS-weighted clinical likelihood (CACS-CL) model in SCP patients with a CACS
of 0. Methods: Thus, to assess SCP, we originally enrolled 14,232
individuals for CACS and coronary computed tomography angiography (CCTA) scans
between January 2016 and January 2018. Finally, patients with a CACS of 0 were
included and followed up until January 2022. According to the established
CACS-CL cutoffs of 15% and 5%, the associations between coronary artery disease
(CAD) and major adverse cardiovascular events (MACEs) in risk groups were
evaluated, alongside the net reclassification improvement (NRI).
Results: Of the 6689 patients with a CACS of 0, the prevalence of CAD
increased significantly (p
Keywords
- risk assessment strategy
- stable chest pain
- coronary artery calcium score
- coronary computed tomography angiography
- coronary artery calcium score-weighted clinical likelihood model
Stable chest pain (SCP) in patients is suggestive of chronic coronary syndrome (CCS). Cardiac imaging testing (CIT) is widely employed to assess the presence of obstructive coronary artery disease (CAD) [1, 2]. Although coronary computed tomography angiography (CCTA) is increasingly recognized as the first-line CIT, per recently published guidelines [1, 2], an increasing body of clinical trials has demonstrated that most patients referred for CCTA as well as other cardiac imaging tests presented no adverse clinical events when the results were negative [3, 4, 5, 6]. As the desire to get the most out of limited resources increases, a lively discussion has appeared regarding how to enhance risk assessment to better choose patients for whom further CIT should be postponed [7, 8, 9, 10].
In this setting, there is a resurgence in interest in using the coronary artery calcium score (CACS) as part of the initial clinical decision-making process, to provide a more accurate evaluation for subsequent CIT [7, 11, 12, 13]. A recent meta-analysis of patients with SCP showed that a CACS of 0 had a negative predictive value of 97% for ruling out obstructive CAD [11]. However, substantial research has consistently established that a significant interaction exists between CACS and risk variables in predicting obstructive CAD and major adverse cardiovascular events (MACEs), while atherosclerosis could not be safely excluded in those with a high-risk factor burden but a CACS of 0 [14, 15, 16, 17]. Thus, considerable work is still needed to improve the CACS-based paradigm regarding risk assessment for SCP, particularly in patients with a CACS of 0.
Using a large cohort consisting of 41,177 symptomatic patients who underwent CCTA from 2008 to 2017, Winther et al. [18] developed a CACS-based tool to estimate the clinical likelihood (CL) of obstructive CAD, which included CACS over and above age, sex, symptoms, and other traditional cardiac risk factors. The diagnostic and prognostic values for this CACS-CL model have been validated in several external cohorts [8, 18, 19] and have been recommended by recent guidelines [1, 2]. However, to date, limited data exist on the performance of the CACS-CL model among patients with a CACS of 0. Consequently, the present study aimed to investigate the diagnostic and prognostic values for the CACS-CL model, as well as the effectiveness of current risk assessment strategies based on different cutoffs of CACS-CL, to optimize downstream referrals for CIT in a CCTA-based cohort comprising patients with SCP and a CACS of 0.
Briefly, the CCTA Improves Clinical Management of Stable Chest Pain (CICM-SCP) registry is an ongoing cohort of patients who were referred to CCTA as the first-line CIT to assess their SCP in relation to CCS (ClinicalTrials.gov Identifier: NCT04691037). As shown in Fig. 1, during a period of 24 months, between January 2016 and January 2018, 14,232 patients were finally enrolled in this registry, while details on the registry have been previously described [8, 17]. In the present analysis, patients with a CACS of 0 were included and followed up until January 2022. This study was approved by the Ethics Committees at local institutions and all participants provided informed consent.
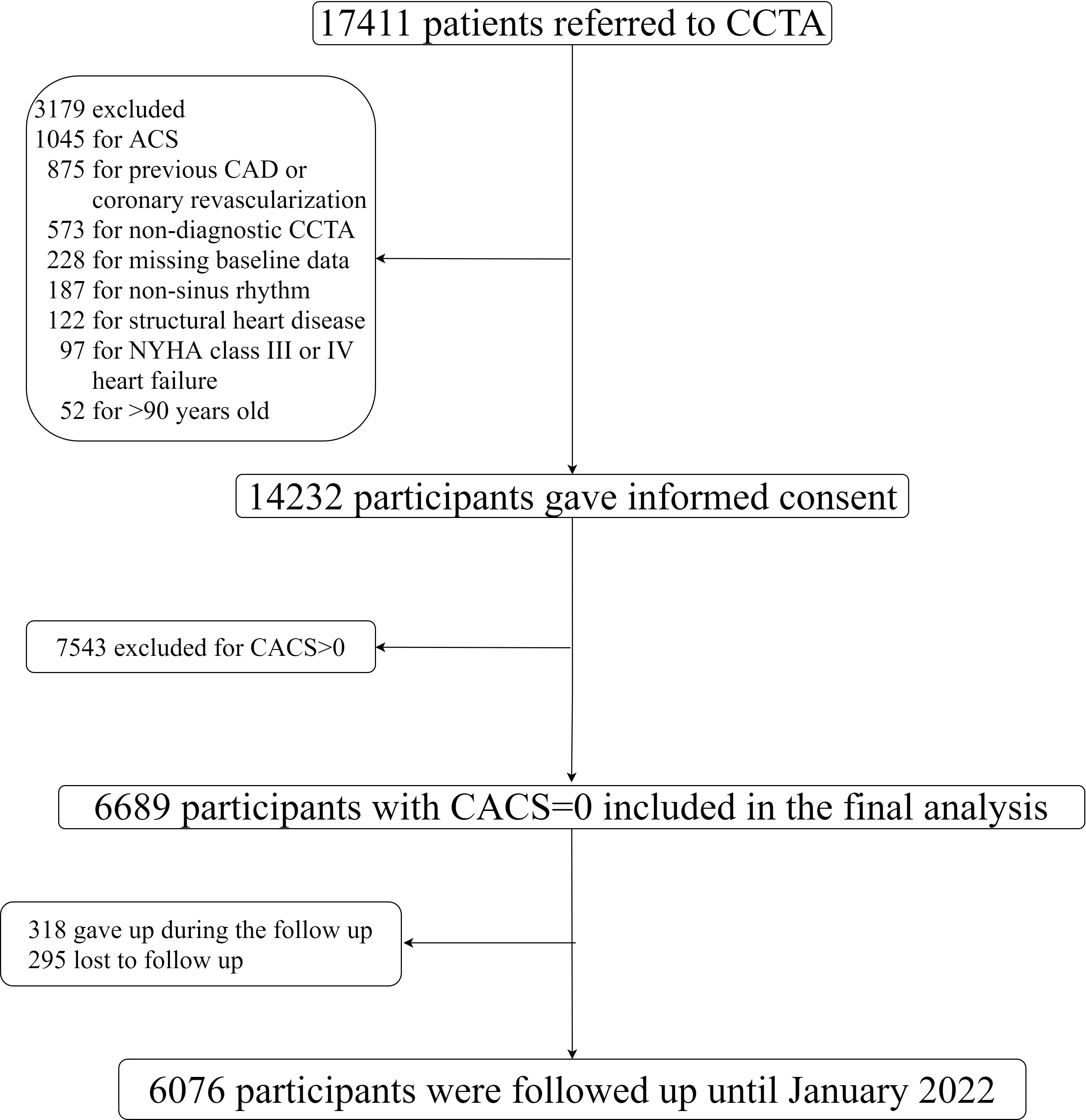 Fig. 1.
Fig. 1.Flow diagram. CCTA, coronary computed tomography angiography; ACS, acute coronary syndrome; CAD, coronary artery disease; CACS, coronary artery calcium score; NYHA, New York Heart Association.
The scanning, as well as interpretation of CACS and CCTA, were conducted as
described previously [8, 17]. Patients with a CACS of 0 were included in the
present study. Based on the Coronary Artery Disease–Reporting and Data System
[20], the maximal degree of coronary diameter stenosis was defined as no CAD
(0%), nonobstructive CAD (1–49%), and obstructive CAD (
Baseline clinical data, including age, sex, diabetes, hypertension,
hyperlipidemia, smoking, family history of CAD, and symptoms were collected and
defined as described previously [8, 17]. Hypertension was defined as blood
pressure
CACS-CL was estimated for each patient using the variables mentioned above (age,
sex, diabetes, hypertension, hyperlipidemia, smoking, family history of CAD, and
symptoms) as well as CACS based on plugins to the statistical software, packaged
from the original study by Winther et al. [18]. The
CADPTP models for implementation in R were available at
https://github.com/CardioLab/cadptp/tree/master/R. Based on the recommendations
of recent guidelines, CIT is not recommended in low-risk patients and should be
referred only to high-risk patients [1, 2]. Thus, we selected two different
cutoffs for CACS-CL (5% and 15%) to classify patients into either the low
(CACS-CL
The research endpoint and the collection of follow-up data were previously defined in detail [8, 17]. Briefly, all patients were followed at the 6th, 12th, 24th, 36th, 48th, 60th, and 72nd months after CCTA. MACEs were defined as a composite of all-cause death and nonfatal myocardial infarction (MI). All-cause death was used rather than cardiovascular death to eliminate the competing events of cardiovascular and noncardiovascular mortality, as well as the need for possibly difficult adjudication of causes of death, especially given the relatively low mortality. All MACEs were adjudicated via a review of the follow-up information and medical records by an independent clinical event committee who were blinded to other study data.
All data analyses were performed using MedCalc (version 15.2.2; MedCalc
Software, Mariakerke, Belgium) and R (version 3.2.4; R Foundation for Statistical
Computing, Vienna, Austria). A p value
Baseline characteristics according to CACS-CL (
| All | CACS-CL | p | ||||
| (n = 6689) | 5–15% (n = 1023) | |||||
| Age* | 57.26 |
56.38 |
59.43 |
67.59 |
||
| Male | 3813 (57) | 3035 (56) | 608 (59) | 170 (69) | ||
| Diabetes | 736 (11) | 542 (10) | 142 (14) | 52 (21) | ||
| Hypertension | 2408 (36) | 1842 (34) | 412 (40) | 154 (62) | ||
| Hyperlipidemia | 1940 (29) | 1517 (28) | 327 (32) | 96 (39) | ||
| Smoking | 1605 (24) | 1138 (21) | 339 (33) | 128 (52) | ||
| Family history of CAD | 1204 (18) | 921 (17) | 203 (20) | 79 (32) | ||
| Symptoms | ||||||
| Nonanginal anginal | 3478 (52) | 2980 (55) | 451 (44) | 47 (19) | ||
| Atypical anginal | 2542 (38) | 1897 (35) | 477 (47) | 168 (68) | ||
| Typical anginal | 669 (10) | 542 (10) | 95 (9) | 32 (13) | ||
Values are presented as n (%) unless stated otherwise.
CACS-CL, coronary artery calcium score-weighted clinical likelihood; CAD, coronary artery disease.
* years, mean
The receiver operating characteristic curve for the CACS-CL model is presented
in Fig. 2. The discrimination of the CACS-CL model was excellent, with an AUC of
0.805 (95% CI: 0.790–0.819, p
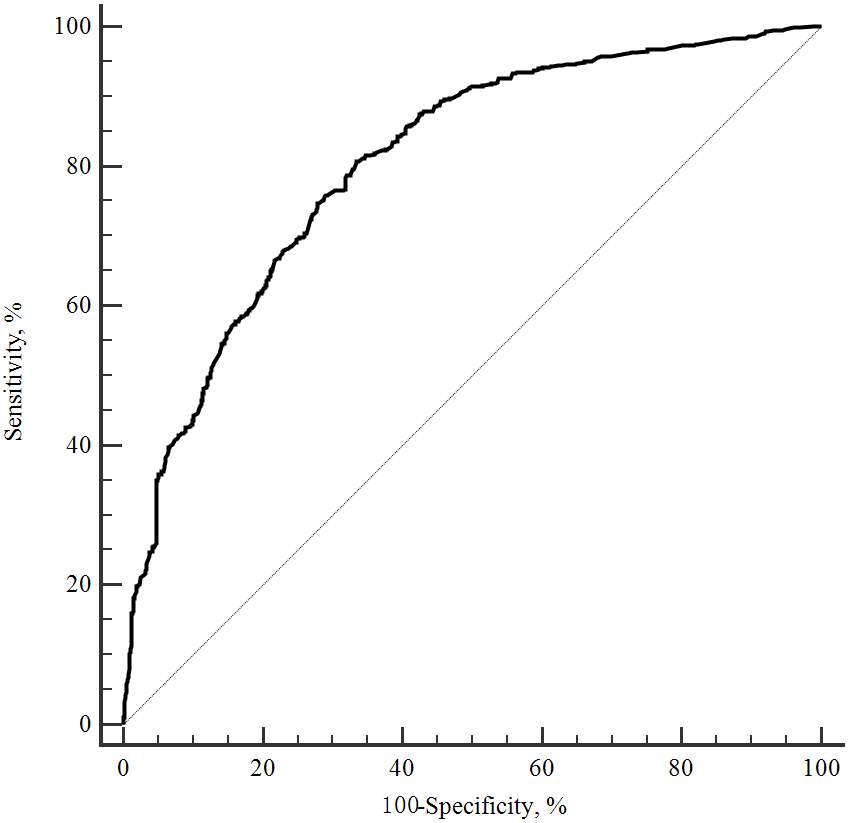 Fig. 2.
Fig. 2.ROC curve for the CACS-CL model to predict obstructive CAD. ROC, receiver operating characteristic; CACS-CL, coronary artery calcium score-weighted clinical likelihood; CAD, coronary artery disease.
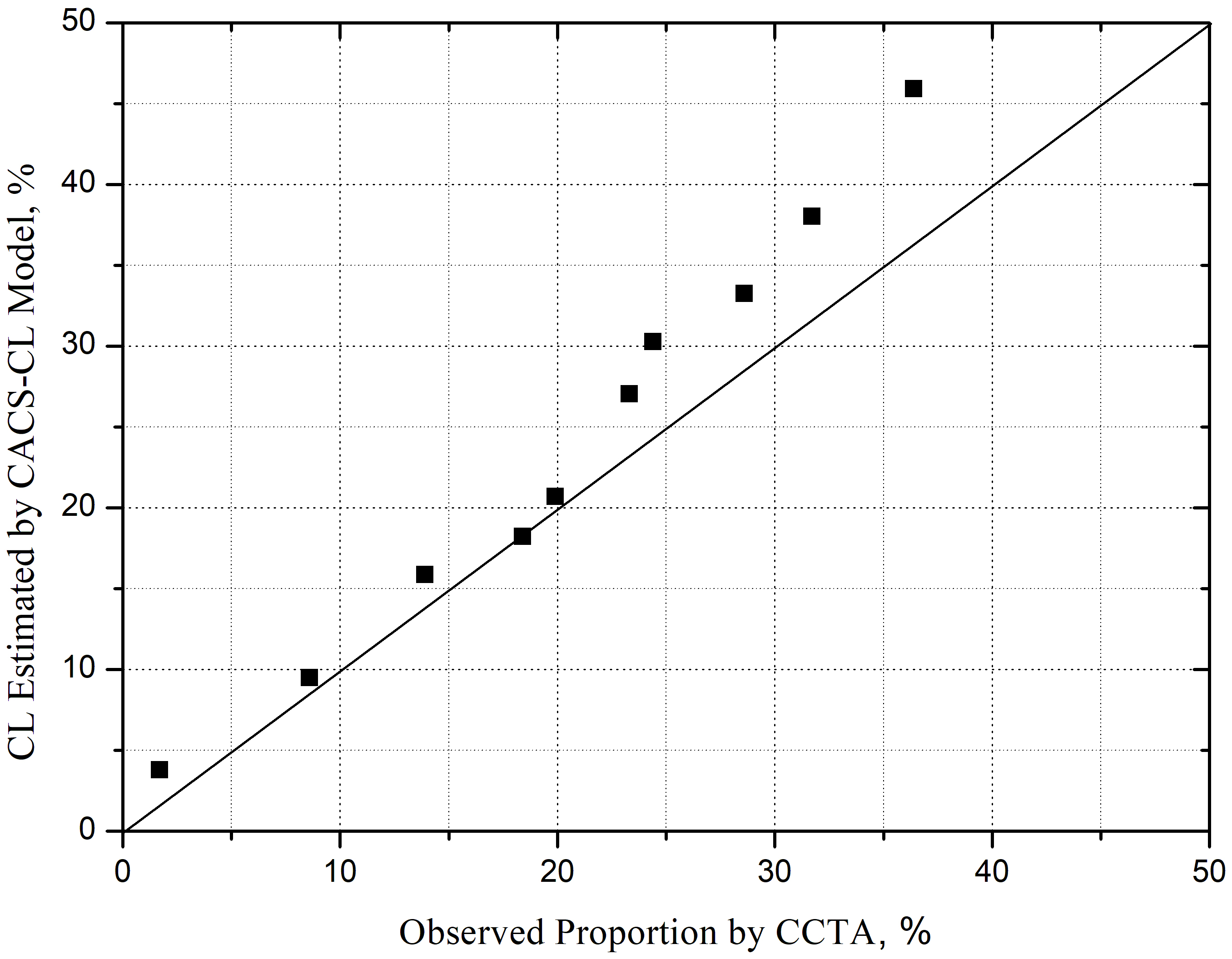 Fig. 3.
Fig. 3.Comparison of CACS-CL and proportion of obstructive CAD on CCTA by deciles of CACS-CL. CACS-CL, coronary artery calcium score-weighted clinical likelihood; CAD, coronary artery disease; CCTA, coronary computed tomography angiography; CL, clinical likelihood.
In total, 247 (4%), 1023 (15%), and 5419 (81%) patients had obstructive,
nonobstructive, and no CAD, respectively, based on CCTA. As illustrated in Fig. 4, compared to patients with CACS-CL
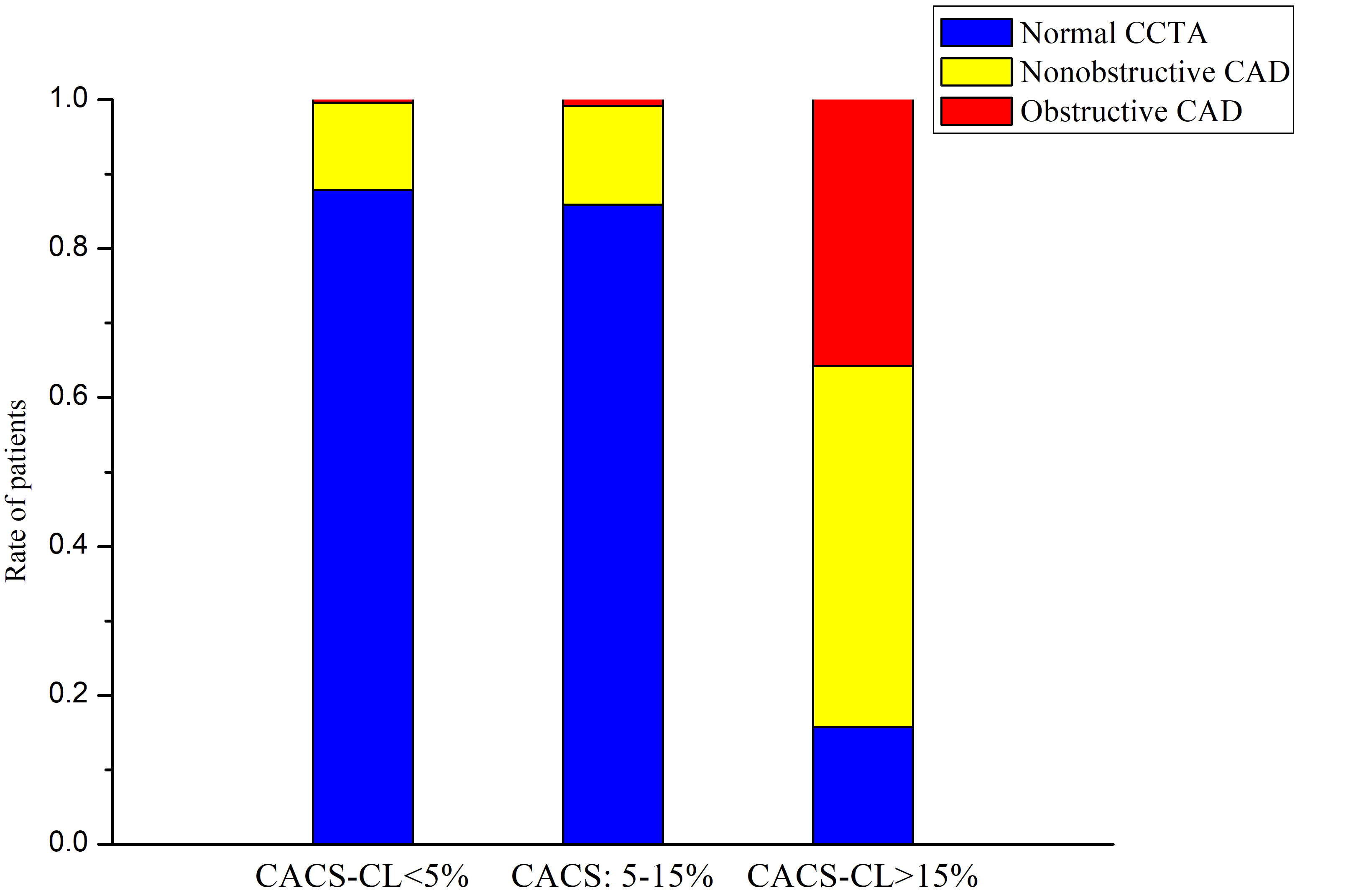 Fig. 4.
Fig. 4.Distribution of CAD according to CACS-CL (
During the 5-year follow-up (median: 61 months, interquartile range: 54 to 68
months), 1% (73/6689) of patients experienced MACEs: 19 patients died and 54
patients suffered from nonfatal MI. As shown in Table 2, the rates of the MACEs
were 0.6%, 1% (10/863), and 13% in patients with CACS-CL
| CACS-CL | ||||
| 5–15% (n = 1023) | ||||
| MACE | 31 (0.6) | 10 (1.0) | 32 (13) | |
| Death | 11 (0.2) | 3 (0.3) | 9 (3.6) | |
| Nonfatal myocardial infarction | 20 (0.4) | 7 (0.7) | 23 (9.4) | |
| Typical anginal | 542 (10) | 95 (9) | 32 (13) | |
| MACE in these patients | 23 (4.2) | 5 (5.3) | 19 (59) | |
| Atypical + nonanginal anginal | 4877 (90) | 928 (91) | 215 (87) | |
| MACE in these patients | 12 (0.3) | 5 (0.5) | 9 (4.2) | |
Values are presented as n (%) unless stated otherwise.
CACS-CL, coronary artery calcium score-weighted clinical likelihood; MACE, major adverse cardiovascular event.
Fig. 5 illustrates the Kaplan–Meier estimates for patients surviving free from
MACEs. The patients in the high-risk group according to the cutoff for CACS-CL =
5% and 15% had a significantly higher (log-rank p
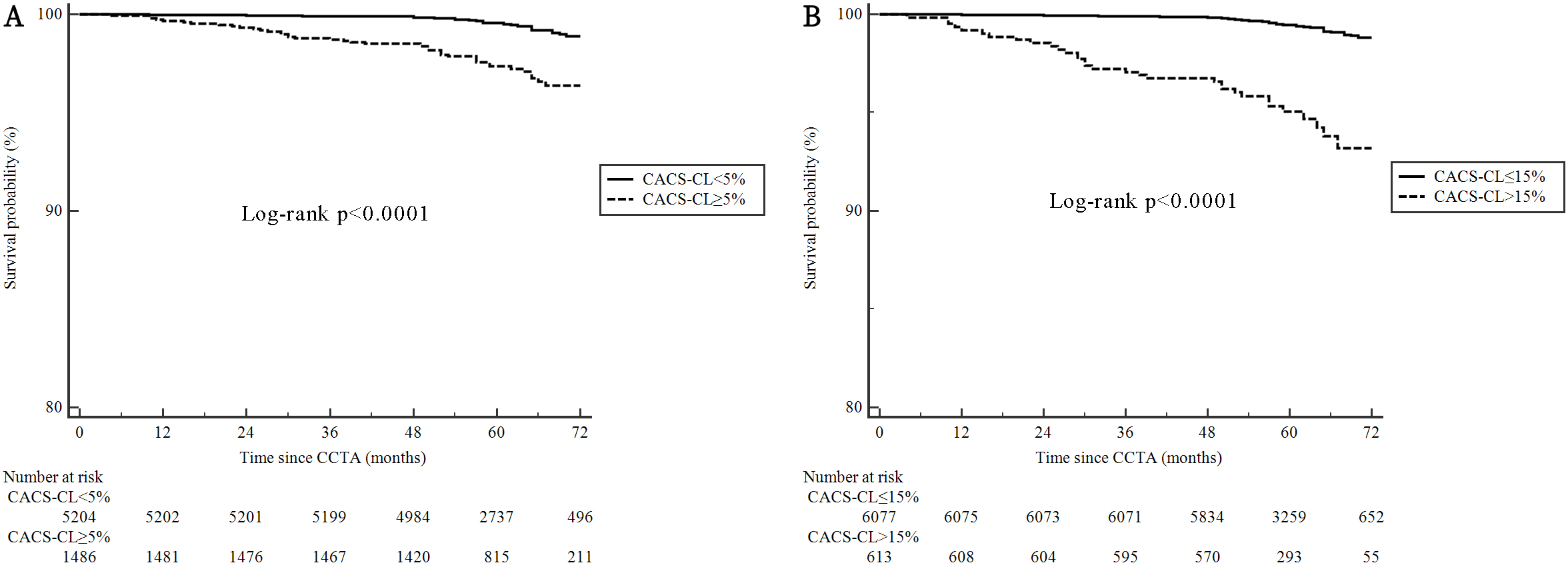 Fig. 5.
Fig. 5.Cumulative survival probability from MACEs according to
different cutoffs for CACS-CL. (A) CACS-CL
Table 3 is the reclassification table for obstructive CAD. Compared to the strategy, which used the cutoff for CACS-CL = 5%, among the 6442 patients without obstructive CAD, 901 patients were correctly reclassified from the high-risk group to the low-risk group. However, 35 patients were incorrectly reclassified from the low-risk group to the high-risk group by the strategy that used the cutoff for CACS-CL = 15%. Among the 247 positive patients, the strategy that used the cutoff for CACS-CL = 15% correctly reclassified one patient from the low-risk group to the high-risk group, although eight patients were incorrectly reclassified from the high-risk group to the low-risk group. Therefore, the NRI of the strategy that used the cutoff for CACS-CL = 15% compared with the strategy that used the cutoff for CACS-CL = 5% was 13.45% for negative patients, –2.84% for positive patients, and 10.61% for all patients. Similarly, when regarding any CAD in Table 4, the NRI was 13.84% for negative patients, –9.68% for positive patients, and 4.16% for all patients.
| Risk groups by CACS-CL = 15% | Total | Reclassification |
NRI |
p | ||||
| Low | High | Up | Down | |||||
| Risk groups by CACS-CL = 5% | ||||||||
| Negative patients | 0.54% | 13.99% | 10.61% | |||||
| Low | 5148 | 35 | 5183 | |||||
| High | 901 | 358 | 1259 | |||||
| Total | 6049 | 393 | 6442 | |||||
| Positive patients |
0.40% | 3.24% | ||||||
| Low | 20 | 1 | 21 | |||||
| High | 8 | 218 | 226 | |||||
| Total | 28 | 219 | 247 | |||||
CACS-CL, coronary artery calcium score-weighted clinical likelihood; CAD, coronary artery disease; NRI, net reclassification improvement.
| Risk groups by CACS-CL = 15% | Total | Reclassification |
NRI |
p | ||||
| Low | High | Up | Down | |||||
| Risk groups by CACS-CL = 5% | ||||||||
| Negative patients | 0.20% | 14.04% | 4.16% | |||||
| Low | 4562 | 11 | 4573 | |||||
| High | 761 | 85 | 846 | |||||
| Total | 5323 | 96 | 5419 | |||||
| Positive patients |
0.32% | 10.00% | ||||||
| Low | 627 | 4 | 631 | |||||
| High | 127 | 512 | 639 | |||||
| Total | 754 | 516 | 1270 | |||||
CACS-CL, coronary artery calcium score-weighted clinical likelihood; CAD, coronary artery disease; NRI, net reclassification improvement.
The study investigated the performance of the CACS-CL model in a real-world cohort and demonstrated its diagnostic and prognostic efficacies among patients with a CACS of 0, who had been referred to CCTA for SCP suspected of CCS. Compared to the risk assessment strategy with a CACS-CL cutoff of 5%, adopting a 15% cutoff appeared more promising for optimizing CIT referrals in negative CACS patients. Moreover, most MACEs occurred in typical anginal patients, meaning we further developed three distinct risk cohorts based on the distribution of MACEs according to CACS-CL and symptoms, thereby informing doctors of the need to take particular heed when managing these patients, especially if they have a high-risk clinical profile.
A landmark meta-analysis of 79,903 patients with SCP showed that the prevalence of no, nonobstructive, and obstructive CAD among those with a CACS = 0 was 84%, 13%, and 3%, respectively [11], which were consistent with data in the present study. Additionally, a CACS of 0 predicted a low incidence of MACEs [2], which was also determined by this study. These findings all supported the importance of a CACS = 0 in a value-based healthcare delivery model as a “gatekeeper” for further CIT among individuals with persistent SCP. However, several studies found that the diagnostic and prognostic values of a CACS of 0 were also dependent on clinical variables [14, 15, 16, 17]. In line with this, the disease burden of CAD and MACEs was widely distributed across different CACS-CL.
Hence, the investigation of the CACS-CL model, including CACS over and above traditional risk factors, to improve risk assessment in SCP patients with a CACS of 0 was valuable. To the best of our knowledge, this is the first research study to thoroughly verify and compare the CACS-CL model and different CACS-CL cutoffs in SCP patients with a CACS of 0. In this study, despite the possibility of a sub-optimal calibration due to ethnic variance, our findings indicated that the CACS-CL model accurately predicted obstructive CAD and MACEs in SCP patients with a CACS of 0, which was similar to the general SCP patients [8, 18, 19]. Thus, a CACS-CL model-based risk assessment strategy to defer unnecessary CIT may be effective and safe for general SCP patients, even patients with SCP and a CACS of 0 [8, 18, 19].
More fundamentally, among SCP patients with a CACS of 0, which was considered a
low-risk population, a better strategy for selecting patients who would benefit
from further CIT is required in the contemporary environment of rising healthcare
costs [7]. To address this gap, we compared two different CACS-CL cutoffs of 15%
and 5% using several measures. The results from the analyses of NRI and
Kaplan–Meier estimates all favored a CACS-CL cutoff of 15%, for positive NRI
and stronger associations of risk groups with MACEs. Thus, the risk assessment
strategy, which used a CACS-CL cutoff of 15% seemed to be more effective and
safer at deferring further CIT in SCP patients with a CACS of 0. The superiority
in the CACS-CL cutoff of 15% over the 5% cutoff might be attributed to the
similar distribution of CAD between patients with CACS-CL
There were numerous limitations in this study that should be mentioned. Firstly, this study was an observational subset of a large cohort, meaning there were potential selection biases resulting from the clinical decisions of local physicians. Unfortunately, due to the lack of more detailed information from this observational registration, we cannot specifically identify the causes of deaths nor validly differentiate between the Type I and II MIs. Moreover, the change in CACS during the follow-up, which has great clinical significance, could not be collected. Secondly, the analysis focused on whether there was at least 50% coronary diameter stenosis, thereby limiting the identification of individuals benefiting most from revascularization, such as those with left main disease or 3-vessel disease with a maximum degree of coronary diameter stenosis 70% [22]. Thirdly, this study solely targeted negative CACS patients with SCP, meaning these findings should not be generalized to other patient groups. Lastly, larger population sizes and long-term outcome data are essential for validating and confirming the study’s findings.
Among patients with SCP who are suspected of CCS and possess a CACS of 0, the CACS-CL model accurately predicted CAD and MACEs. Compared to the risk assessment strategy using a cutoff for CACS-CL = 5%, the strategy that used a cutoff for CACS-CL = 15% seemed to be more effective and safer to defer further CIT in SCP patients with a CACS of 0.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
JZhou and JZhao designed the research study. YT, CL, TC, YL, CW collected the patient data. YT performed the research. YT, CL, TC analyzed the data. YT, CL, TC wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This observational study was approved by the Tianjin Chest Hospital Ethics Committee, and informed consent has been obtained from the patients. The ethics approval number: 2017-KY-004.
Not applicable.
This work was supported by the National Natural Science Foundation of China (62206197 and 62106160), Applied and Basic Research by Multi-input Foundation of Tianjin (21JCYBJC00820), Tianjin Health Research Project (TJWJ2022QN067), Tianjin Scientific and Technological Project (23KPXMRC00110), Tianjin Key Research Program of Traditional Chinese Medicine (2023006) and Tianjin Health Industry High-level Talent Selection and Training Project (TJSQNYXXR-D2-134).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.





