- Academic Editor
†These authors contributed equally.
Background:
Exercise capacity serves as a direct
representation of cardiac function. The Duke Activity Status Index (DASI), a
self-administered 12-item questionnaire, covers aspects of daily living,
household tasks, sexual function, and physical activity. Although widely used to
evaluate exercise capacity, its validation in Chinese
cardiovascular disease
(CVD) patients has not
been thoroughly explored.
Considering
the significant cultural and lifestyle differences between China and Western
countries, which may influence Chinese patients’ comprehension and responses to
DASI, our objective is to culturally adapt DASI for Chinese patients with CVD to
ensure its precision in assessing exercise
capacity. Methods: The cultural
adaptation of the original DASI questionnaire into Chinese followed a rigorous
process to ensure its validity, reliability, and sensitivity to Chinese CVD
patients. The study included 107 outpatients diagnosed with CVD who completed the
DASI and cardiopulmonary exercise testing (CPET). Cronbach’s alpha, Spearman
correlation, and factor analysis were utilized to test reliability and validity.
Receiver operating characteristic (ROC) curve analysis was employed to assess the
prognostic utility of the DASI. Results: Participants had a mean DASI
score of 39.40
Cardiovascular disease (CVD) presents a persistent and significant global health challenge, contributing to substantial morbidity, mortality, and imposing a considerable economic burden on healthcare systems worldwide [1, 2]. In China, the prevalence of CVD continues to surge, with an estimated 330 million current cases, solidifying its position as a primary cause of death in the nation [3, 4]. Effective management of CVD is crucial for improving patient outcomes and reducing the risk of recurrent events. A critical aspect of CVD management is the assessment of cardiopulmonary function and exercise capacity, which are closely related to factors such as treatment outcomes, quality of life, disease progression, and prognosis [5, 6, 7].
Cardiopulmonary exercise testing (CPET) serves as a valuable tool for the
comprehensive evaluation of patients’ cardiopulmonary function and exercise
capacity [8, 9]. However, its high cost and technical demands limit its
applicability, particularly in primary medical institutions. As a result, the
development of low-cost, accessible, and easy-to-operate methods for diagnosing
and assessing CVD has become increasingly important. In CPET, a commonly used
threshold for peak oxygen uptake (Peak VO
The Duke Activity Status Index (DASI) questionnaire, originally developed in English, consists of 12 self-reported items and provides a practical and effective approach for estimating a patient’s functional capacity [12]. These items encompass various daily activities with differing physical exertion levels, including personal care, ambulation, household tasks, and recreational activities. Each item is assigned a specific point based on the energy expenditure required for the activity. Patients indicate whether they can perform each activity without difficulty (“Yes” or “No”), and the total DASI score is calculated by summing the points of all “Yes” items, ranging from 0 to 58.2. Higher score signify better functional capacity. DASI score have been found to correlate with quality of life in heart failure patients [13, 14] and to predict postoperative risk in patients undergoing inpatient noncardiac surgery [15, 16]. Moreover, the DASI questionnaire has demonstrated its prognostic value, as higher score have been associated with improved outcomes and reduced mortality rates in CVD patients [17, 18].
Although
the questionnaire has been used in Chinese patient populations [19, 20, 21], its
reliability and validity in this specific group have not been thoroughly
investigated. Furthermore, in our previous study [20] involving Chinese patients
with pulmonary hypertension, we discovered a weak correlation (r =
0.467) between the DASI score obtained from the original questionnaire and Peak
VO
The
primary objective of this investigation is to culturally adapt and validate the
DASI questionnaire for Chinese CVD patients. This includes an exploration of the
questionnaire’s reliability and validity. Additionally, we will explore whether
the adapted questionnaire can effectively identify patients with a better or
worse prognosis based on a Peak VO
This cross-sectional observational study was conducted at Guangdong Provincial People’s Hospital (GDPH), a tertiary-care teaching hospital situated in southern China. The observational protocol of the study obtained ethical approval from the Ethics Committee of Guangdong Provincial People’s Hospital (KY2023-053-02). All procedures were performed in adherence to the principles outlined in the Declaration of Helsinki.
The study participants were recruited at the cardiovascular clinic of GDPH from
March to April 2023. Inclusion criteria were as follows: (1) age
The study flow diagram was shown in Fig. 1. All eligible patients were provided with the study introduction and had the opportunity to ask questions about the study before participation. Prior to commencing any study procedures, participants were secured with informed consent. The data collection procedure involved administering the culturally adapted DASI questionnaire first, with the participants’ DASI score being kept blinded to the CPET testing personnel. Subsequently, the participants underwent CPET testing on the same day. Before conducting CPET testing, physicians collected information about the participants’ exercise types, frequency, intensity, and duration to assess their physical activity levels. Additionally, demographic information (age, gender, body mass index [BMI], etc.), medical history, and relevant clinical data were obtained through interviews, medical record reviews, and physical examinations conducted by trained research personnel.
 Fig. 1.
Fig. 1.Study flow diagram. DASI, The Duke Activity Status Index; CPET, cardiopulmonary exercise testing; RER, respiratory exchange ratio.
The cultural adaptation of the original DASI questionnaire into Chinese followed a rigorous process to ensure its validity, reliability, and sensitivity to the Chinese cardiovascular disease patient population [23]. The process began with forward translation by two independent bilingual translators whose native language is Chinese, generating versions T1 and T2. Then, the two translators, a health professional, and a researcher in the field of CVD reviewed the translated questionnaire, resolved discrepancies, and established a consensus version (T-1.2). Subsequently, two different bilingual translators blinded to the original DASI translated the consensus version back into English, resulting in versions BT1 and BT2. Another second expert panel evaluated the conceptual and semantic equivalence between the back-translated English version and the original DASI questionnaire, and necessary modifications were made to the Chinese version. The culturally adapted Chinese DASI questionnaire was then pilot-tested on 15 patients with CVD to assess understandability, acceptability, and any potential issues related to the questionnaire’s content or format. Based on the feedback collected during pilot testing, further revisions were made as necessary. After incorporating the feedback, the final culturally adapted Chinese DASI questionnaire was developed and used in this study. Detailed information on the adaptation process is provided in Supplementary Table 1.
CPET was conducted using a cycle ergometer
(ERG 910 plus, SCHILLER, Baar, Switzerland) to evaluate aerobic
capacity and cardiopulmonary fitness in accordance with established guidelines
and practice principles
[24]. A
calibrated metabolic cart (CARDIOVIT CS-200 Office ErgoSpiro,
SCHILLER, Switzerland) was utilized to examine respiratory gas exchange on a
breath-by-breath basis, and continuous 12-lead electrocardiogram (ECG) monitoring
was performed throughout the test; blood pressure was automatically measured at
2-minute intervals.
The
CPET protocol utilized a ramp protocol, with participants instructed to maintain
a pedal cadence of 55–65 rpm. Physicians used
the formula provided by Wasserman et al. [25] to calculate the specific
incremental work rate based on each participant’s age, sex, height, and weight.
Taking into account
their physical activity levels, we made a decision on whether to select a power
output lower or higher than the computed value, with the aim of achieving a test
duration between 8 to 12 minutes. All patients underwent a standardized
procedure, which consisted of a 3-minute baseline period and a 3-minute warm-up
phase (warm-up, 0 W). Following this, they underwent the incremental exercise
test, after which a 5-minute cool-down period was
implemented.
The test was continued until they presented one of the following termination
criteria: (1) achievement of
According to the consensus-based standards for the selection of health
measurement instruments (COSMIN), a minimum sample size of 60 patients with CVD
was adequate for examining the internal consistency, test-retest reliability,
measurement error, and construct validity of the DASI questionnaire [27].
We hypothesized a
correlation with a coefficient of at least 0.35 between the DASI score and Peak
VO
The data analysis was performed using IBM SPSS
software version 20 (IBM Corp., Armonk, NY,
USA). Continuous variables are presented as mean
The internal consistency was evaluated using
Cronbach’s
Construct validity was examined using factor analysis [30]. A principal components analysis with varimax rotation and Kaiser normalization was conducted. The Kaiser-Meyer-Olkin (KMO) criteria confirmed the adequacy of the correlation matrix, which should be greater than 0.60, and Bartlett’s test with a significance level of 0.05. Factors with eigenvalues greater than or equal to one were considered significant factors. After the rotation matrix, items with a factor loading greater than or equal to 0.5 were included in the factor.
A Peak VO
Most of the DASI items were translated with minimal cultural adaptation. Three items, however, were adjusted to suit Chinese societal norms. Firstly, in item 9, we replaced “weeding” which is a less common activity in Chinese society, with “gardening or farm work, hoeing” which has a metablic equivalents (METs) value of 3.9 [33, 34, 35], classifying it in the moderate-intensity levels, similar to “weeding”. Secondly, in item 11, “golf, bowling, doubles tennis, or throwing a baseball or football” were replaced by “table tennis, fishing, or doubles badminton”. These replacements were made because these activities are more prevalent in China and are considered to represent moderate-intensity levels, corresponding to metabolic equivalents ranging from 3 to 6 [33, 34, 35]. Lastly, in item number 12, the activities “singles tennis, football, basketball or skiing” were replaced with “singles badminton, mountain climbing” both of which are considered high-intensity activities [35, 36]. During the pilot testing phase, patients encountered no issues in understanding all 12 items and found the activities mentioned to be relevant to their circumstances. As a result, the Chinese version of DASI maintained the principal meanings of the original items, was easy to comprehend, and user-friendly. For the complete Chinese version of the DASI, please refer to Supplementary Table 2. Additionally, the English translated version of the Chinese DASI can be found in Supplementary Table 3. All participants found the questionnaire easy to respond to. They encountered no difficulties while completing it, demonstrating a clear understanding of all the listed activities.
Initially, 138 potential participants were screened for eligibility. Among them,
15 patients declined to participate, and 6 patients with severe comorbidities
were excluded. Additionally, 3 patients were unable to complete the CPET due to
physical constraints, while 7 others were excluded because of an RER
| Variable | Mean | |
| Age (years) | 48.01 | |
| Gender (female/male) | 47 (43.9%)/60 (56.1%) | |
| BMI (kg/m |
22.29 | |
| Diagnosis | ||
| Coronary artery disease | 52 (48.6%) | |
| Valvular disease | 20 (18.7%) | |
| Heart failure | 18 (16.8%) | |
| Pulmonary hypertension | 17 (15.9%) | |
| Educational level | ||
| Primary school | 23 (21.5%) | |
| Middle school | 28 (26.2%) | |
| High school | 42 (39.2%) | |
| College or above | 14 (13.1%) | |
| Smoking (yes/no) | 28 (22.6%)/79 (73.8%) | |
| Exercise habit (yes/no) | 30 (28.0%)/77 (72.0%) | |
| LVEF (%) | 53.16 | |
| DASI total score | 39.40 | |
| Peak VO |
19.53 | |
| Peak VO |
36 (33.6%) | |
BMI, body mass index; LVEF, left ventricular ejection fraction; DASI, Duke
Activity Status Index; Peak VO
For the culturally adapted Chinese version of the DASI, no floor or ceiling
effects were observed, as three (3%) patients scored the lowest possible points
and eleven (10%) scored the highest. The questionnaire exhibited acceptable
internal consistency, as evidenced by a Cronbach’s
In assessing criterion validity, a
moderate positive correlation was found between the DASI score and Peak VO
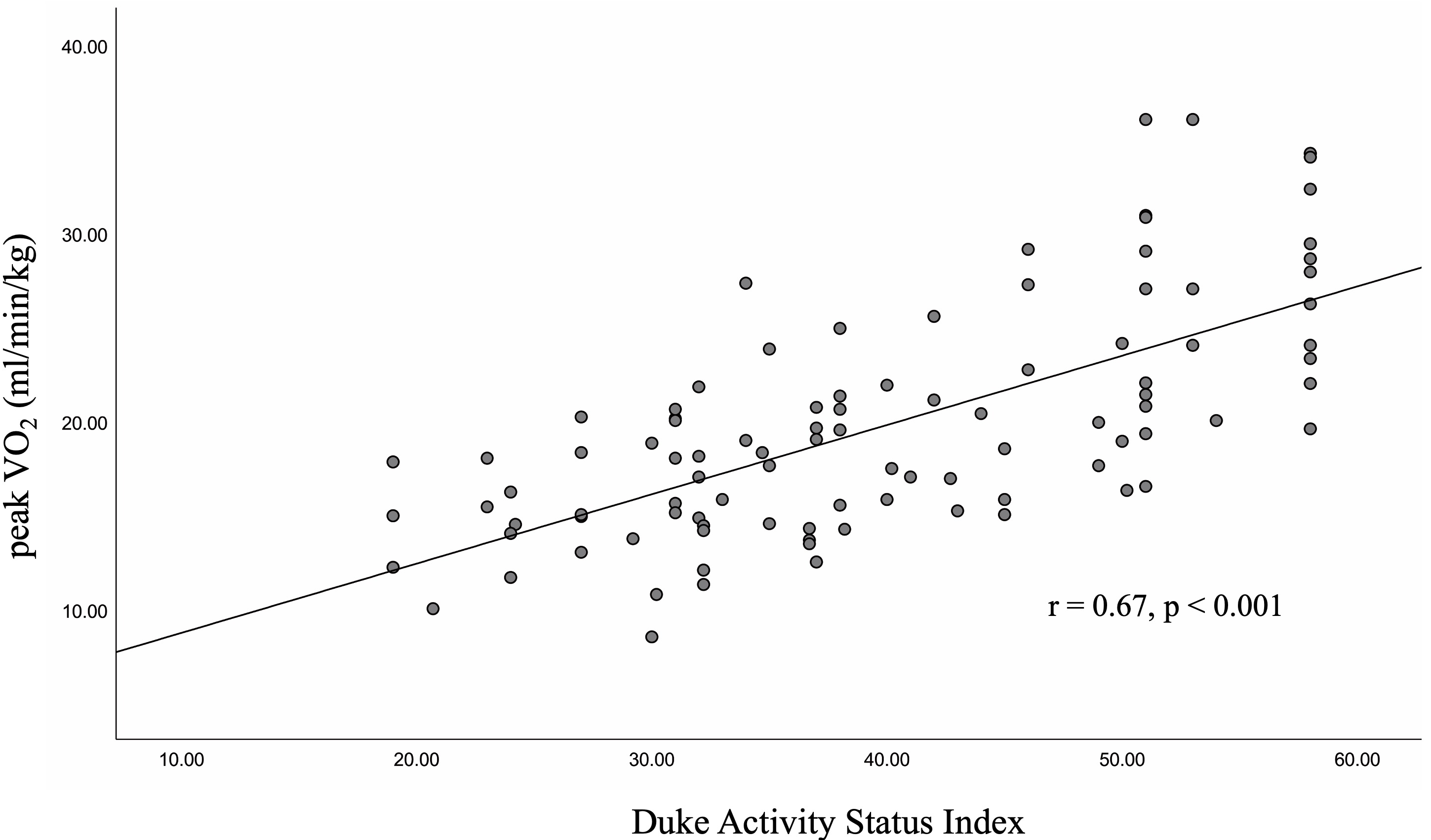 Fig. 2.
Fig. 2.The Association between the DASI score and Peak VO
To evaluate construct validity,
exploratory factor analysis was conducted after excluding item 1 from the
questionnaire, as all subjects in the sample reported their ability to perform
the proposed activities, resulting in no variance for this particular item. The
obtained KMO value (0.71) and Bartlett’s test (p
The ROC curve analysis demonstrated the discriminative ability of DASI in
identifying patients with a more favorable long-term prognosis (p
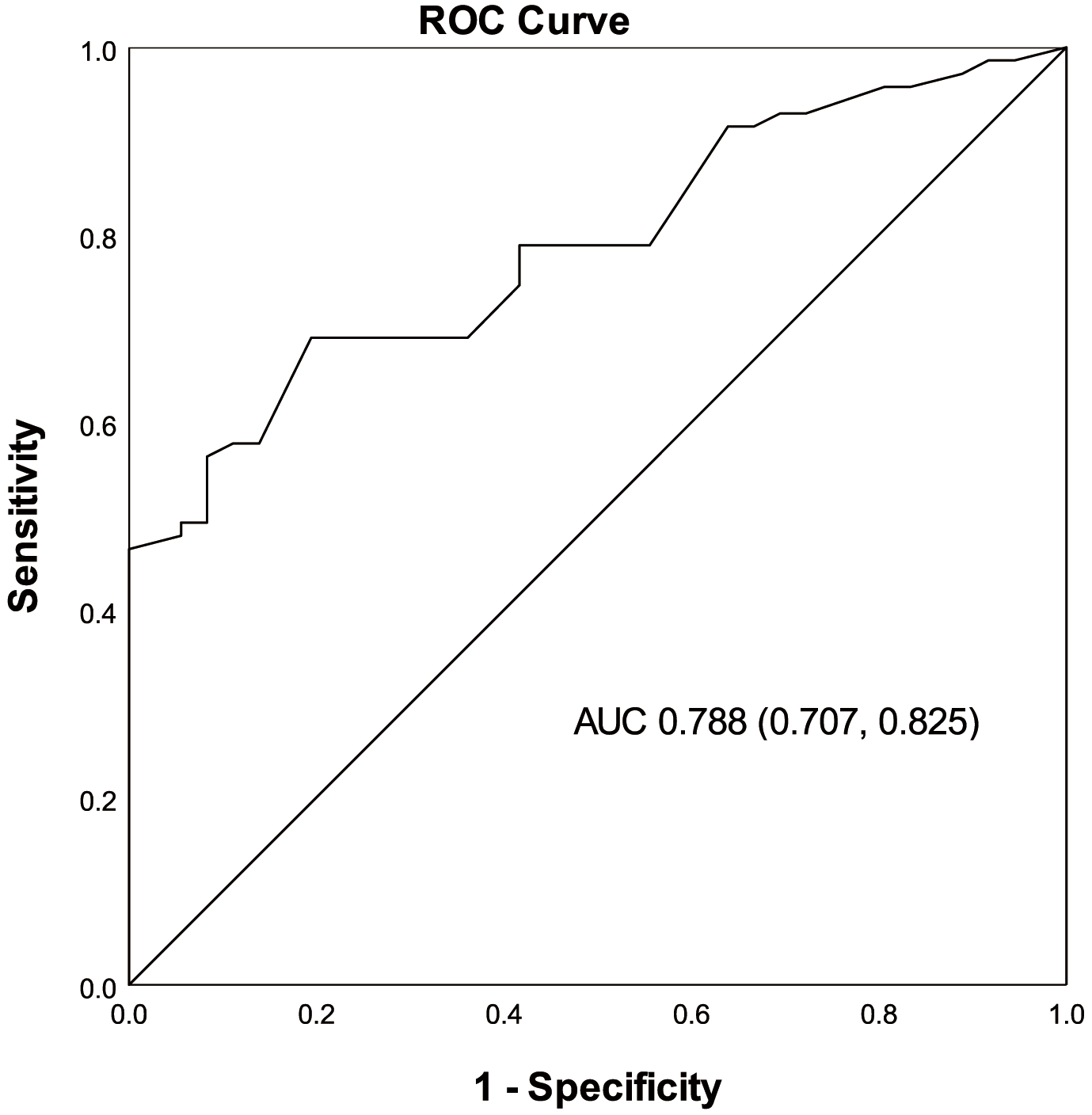 Fig. 3.
Fig. 3.Discriminative properties of the DASI in identifying the
patients with Peak VO
Using
the established DASI cut-off value of 36.85, we categorized the participants,
assigning 71 patients to the high DASI group and 36 patients to the low DASI
group. Analyzing the LVEF between these groups, we found that patients with a
high DASI score demonstrated significantly higher LVEF compared to those with a
DASI score
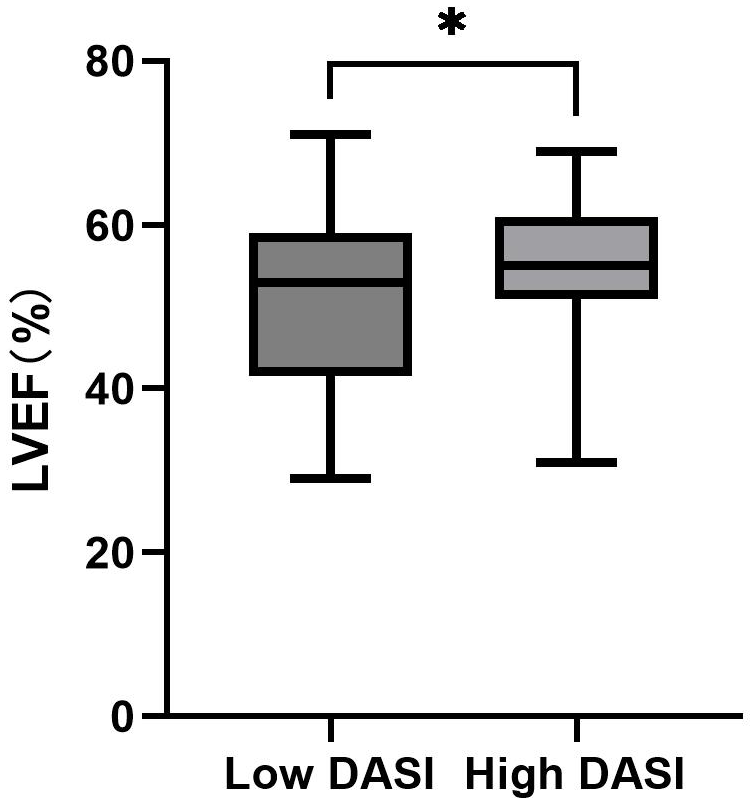 Fig. 4.
Fig. 4.Comparison of LVEF between High DASI Group and Low DASI Group. LVEF, left ventricular ejection fraction; DASI, Duke Activity Status Index; *, p
Our findings demonstrate that the culturally adapted DASI questionnaire possesses acceptable reliability, validity, and the ability to predict long-term prognosis in Chinese CVD patients. These results support that the culturally adapted DASI for the Chinese population can provide a reasonably accurate reflection of the exercise capacity of Chinese CVD patients, endorsing the use of DASI as a valuable assessment tool for this patient population.
The reliability of the culturally adapted Chinese version of the DASI questionnaire was found to be consistent with those reported in other populations [12, 37, 38], suggesting that the cultural adaptation process successfully maintained the questionnaire’s psychometric properties. Concerning construct validity, our exploratory factor analysis identified three factors that collectively accounted for more than half of the total variance, differing from the two factors typically found in most validation studies [14, 38]. These factors represent different dimensions of functional capacity, reflecting the original design intention of the DASI questionnaire. In our study, the factor loadings of item 9 showed a relatively equal contribution to both factor 2 (0.522) and factor 3 (0.534). This indicates that item 9 is incapable of distinguishing between various levels of metabolic cost in physical activities, a situation also noted in the Brazilian version of the DASI [38]. In that study, item 9 was assigned a value of 4 METs during development, but the analysis results showed its correlation with higher METs activities. This could stem from the notable prevalence of urban residents among our study participants. The gardening or farm work activities described in item 9 are activities that are not commonly practiced by urban residents in China. Nevertheless, we have chosen to retain this item due to China’s identity as an agrarian nation, where a substantial proportion of the population resides in rural areas.
In
the present study, we observed a moderate positive correlation between DASI score
and Peak VO
Notably, this study’s most prominent advantage is the utilization of CPET for
assessing Peak VO
When
categorizing patients into groups with better or worse long-term prognosis based
on the Peak VO
It is important to acknowledge the inherent limitations of the DASI questionnaire, such as the reliance on patients’ self-reporting, which may introduce biases or inaccuracies in the assessment due to factors like memory lapses or social desirability. However, the results of the educational level (Table 1) in this study indicated that patients of varying educational backgrounds can effectively understand and complete the questionnaire, showcasing its suitability across education levels. Furthermore, it offers advantages such as ease of administration, low cost, minimal burden on patients, and a demonstrated correlation with exercise capacity. Therefore, the findings may hold implications for healthcare teams, particularly in primary healthcare settings within the context of China. The adapted DASI questionnaire, to be specific, could play a role in cardiac rehabilitation, assisting healthcare professionals in tailoring individualized exercise programs, monitoring patients’ progress, and evaluating the effectiveness of interventions to improve functional capacity and overall cardiovascular health.
This study has several limitations that warrant consideration. Firstly, the single-center design may limit the generalizability of our findings - conducting multicenter studies could provide more robust evidence. Secondly, as shown in the data scatter plot in Fig. 2, the DASI score is not a perfect measure of exercise capacity. Therefore, when a precise assessment of exercise capacity is necessary, DASI cannot replace exercise testing [12]. Thirdly, being a cross-sectional study, it does not assess the relationship between DASI score and clinical endpoints. Prospective cohort studies could help investigate this relationship. Fourthly, the participant selection may have introduced bias, as some patients were unable to complete the CPET or were excluded for other reasons, and future studies should consider refining screening criteria. Moreover, this study did not assess test-retest reliability or the sensitivity of DASI to functional capacity changes over time, which should be explored in future research.
This study validates the culturally adapted DASI questionnaire as a straightforward and efficient tool for reasonably evaluating exercise capacity in Chinese CVD patients. This adapted questionnaire demonstrated satisfactory reliability and validity in this patient group, as well as the ability to discern patients with a better long-term prognosis, thus assisting in the identification of high-risk CVD patients.
CVD, cardiovascular disease; CPET, cardiopulmonary exercise testing; Peak
VO
The data presented in this study are available on request from the corresponding author.
YXL and HFZ designed the research study, wrote the manuscript, and designed the table and figure. HFZ analyzed the data. MFL, GLZ and TW collected data. MYX and JWD provided help with data collection. LG, HM and QSG revised the manuscript, and were involved in the acquisition, analysis, and interpretation of data for the work, and obtained final approval. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Informed consent was obtained from all subjects involved in the study. The study was conducted in accordance with the Declaration of Helsinki, and approved by the ethical review committee of Guangdong Provincial People’s Hospital (KY2023-053-02).
We would like to thank all the participants in the study.
This research was supported by the grants from Start-up Funding of National Natural Science Foundation of China (No.8207050582, 8217142362) and High-level Hospital Construction Project of Guangdong Provincial People’s Hospital (DFJH201922).
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
