1 National Clinical Research Center for Cardiovascular Diseases, State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, 100037 Beijing, China
2 Central China Sub-center of the National Center for Cardiovascular Diseases, 450000 Zhengzhou, Henan, China
3 National Clinical Research Center for Cardiovascular Diseases, Shenzhen, Coronary Artery Disease Center, Fuwai Hospital Chinese Academy of Medical Sciences, 518057 Shenzhen, Guangdong, China
†These authors contributed equally.
Abstract
Background: Little is known of the characteristics,
treatment, and outcomes of patients with ST-segment elevation myocardial
infarction (STEMI) but without standard modifiable cardiovascular risk factors
(SMuRFs, including smoking, hypercholesterolemia, diabetes, and hypertension) in
developing countries like China. Moreover, contributors to the excess mortality
of such SMuRF-less patients remain unclear. Methods:
This study was based on a nationally representative sample of
patients presenting with STEMI and admitted to 162 hospitals in 31 provinces
across mainland China between 2001 and 2015. We compared
clinical characteristics, treatments, and mortality during hospitalization
between patients with and without SMuRFs. We also investigated the possible
causes of differences in mortality and quantified the contributors to excess
mortality. Results: Among 16,541 patients (aged 65
Keywords
- ST-segment elevation myocardial infarction
- risk factors
- treatment
- mortality
Approximately 11–26% of patients hospitalized for ST-segment elevation myocardial infarction (STEMI) worldwide were found to have no standard modifiable cardiovascular risk factors (SMuRFs, including smoking, hypercholesterolemia, diabetes, and hypertension) at their first presentation [1, 2, 3, 4, 5, 6, 7]. Such patients are referred to as SMuRF-less, and their proportion among STEMI patients has been reported as 11.8% in China [2], 14.9% in Sweden [1], 19.2% in Australia [3], and 11.0–26.2% in the United States [4, 5, 6]. In some countries, this proportion has increased over time [3, 8]. Although they are commonly considered as low-risk populations and are often overlooked in research [1, 9], recent studies have reported that SMuRF-less patients experienced unexpectedly worse crude in-hospital mortality compared to those with SMuRFs [1, 2, 3, 5, 10, 11].
Comparisons regarding the management and outcomes between patients with and without SMuRFs are mainly from developed countries, while little is known in developing countries about the management of these patients in clinical practice. Furthermore, the reasons for the worse outcomes of SMuRF-less patients are still unclear, and observations were conflicting regarding the possible contributors. Some studies have suggested that the higher risk of mortality in SMuRF-less individuals can be fully accounted for by patient characteristics [10, 12], while others have indicated the underuse of treatments [1] and/or heterogeneity in patient characteristics [2]. Quantitative assessment of the major contributors should help determine the optimal measures for reducing the mortality of SMuRF-less patients.
Accordingly, we used the data from the China Patient-centered Evaluative Assessment of Cardiac Events Retrospective Study of acute myocardial infarction (AMI), namely China PEACE-Retrospective AMI Study [10]. This offers a nationally representative sample of patients who were hospitalized for STEMI in 162 hospitals across mainland China between 2001 and 2015. The aim of the present work was to compare the characteristics, therapies, and outcomes during hospitalization between STEMI patients with and without SMuRFs, and to explore the possible contributors to the differences in mortality.
The China PEACE-Retrospective AMI Study protocol has been published earlier [13, 14]. Briefly, a two-stage random sampling procedure was used to draw nationally representative cases hospitalized for acute myocardial infarction (AMI) in 2001, 2006, and 2011. In the first stage, a simple random sampling process was used to include representative hospitals from five economic-geographic strata: eastern-rural, central-rural, western-rural, eastern-urban, and central/western-urban regions. These strata were used because socioeconomic levels and healthcare resources vary across categories (Supplementary Fig. 1). In the second stage, AMI patients from the sampled hospitals were drawn using systematic random sampling methods. AMI hospitalizations were identified by International Classification of Diseases (ICD) codes, Ninth Revision (410.xx) and Tenth Revision (I21.xx), if available, or by the principal discharge diagnosis. This study also included patients admitted in 2015 using the same method.
Trained staff retrieved data from medical charts using clear abstraction approaches and standardized data definitions. Each medical record was copied by the participating hospital and transmitted to the central abstraction center. All abstractors received central training for two weeks. Those who could extract 10 sample medical records with more than 98% accuracy after training received certification. Rigorous monitoring was employed at each stage to ensure the accuracy of abstraction. Data quality was monitored by randomly auditing 5% of the abstracted records. The overall accuracy exceeded 98% [13, 14].
The central ethics committee of the Chinese National Center for Cardiovascular Diseases approved this study. Given the retrospective nature, written patient consent was not required. Ethics approval was also obtained from all participating hospitals.
Patients with a discharge diagnosis of STEMI were included, which was determined by combining the diagnosis at discharge with the results of electrocardiograms (ECGs). In cases where there was no definitive diagnosis from the local hospital, cardiologists from the coordinating center reviewed the medical logs and ECGs to determine the STEMI diagnosis. An independent cardiologist who did not take part in abstraction validated the AMI type by reviewing ECGs in randomly selected records. The concordance rate for the selected cases was 94.7%.
Patients were excluded if they had an established myocardial infarction, percutaneous coronary intervention (PCI), or coronary artery bypass graft before admission, or if their STEMI occurred during hospitalization. Also excluded were patients with missing baseline data on SMuRFs, patients transferred in or out because their hospitalization was truncated, and patients discharged alive within the first 24 hours, given that they were very likely to have left against medical advice and had very little time to receive treatment (Supplementary Fig. 2).
Similar to a previous study [1], we defined SMuRFs as having
at least one of the following modifiable risk factors: current smoking,
hypercholesterolemia, diabetes, or hypertension. The definition
of current smoking is having smoked regularly (at least one
cigarette per day) during the last six months.
Hypercholesterolemia was defined as having a low-density lipoprotein cholesterol
concentration
The use of in-hospital therapies recommended by the guidelines
for the management of STEMI was assessed, which included aspirin, P2Y
In-hospital mortality was defined as death or treatment withdrawal due to a terminal condition. The Chinese Government uses death or withdrawal of treatment as an indicator of hospital quality [16]. At the coordinating hospitals, cardiologists judged the clinical status of patients withdrawn from treatment based on their medical records. Composite complications included death, treatment withdrawal due to a terminal condition, congestive heart failure, re-infarction, ischemic stroke, or cardiogenic shock.
Continuous variables were analyzed using t-tests or
non-parametric equivalent tests and presented as medians with interquartile
ranges. Categorical variables were listed as percentages, and analysis was
performed using
To explore the link between SMuRF-less status and therapies received, mixed models with hospitals as a random intercept were used to account for age, sex, medical histories, clinical profiles at admission, and admission ward.
Survival curves and hazard functions for in-hospital mortality
were plotted. Mixed effect models were also used to assess
whether SMuRF-less was independently associated with mortality, accounting for
all explanatory variables stepwise. The models used in the
study were: an unadjusted model; model 1 (adjusted for age and sex);
model 2 (adjusted for model 1, medical
history [stroke, atrial fibrillation, chronic renal disease, heart failure,
peripheral arterial disease], and clinical characteristics at
admission [systolic blood pressure [SBP], heart rate, chest discomfort, cardiac
arrest, cardiogenic shock, stroke]); and model 3 (adjusted for model 2,
pharmacotherapies during hospitalization [aspirin, P2Y
To explore the possible contribution of each treatment to the disparities in mortality, the effect of each treatment was investigated using age- and sex-adjusted analyses, taking the SMuRF-less status into consideration. Formal mediation analyses were also performed to examine the extent to which specific variables (including all clinical profiles and treatments) might contribute to in-hospital mortality in SMuRF-less patients. A mediator was defined as a variable that lies along the causal chain connecting the predictor and mortality. Traditionally, mediators are often adjusted in the assessment of causal association. Meaningful associations between mortality and the predictor could thus be removed, leading to incorrect conclusions of no association. Therefore, formal mediation analyses would facilitate identifying potential factors to explain the higher mortality among SMuRF-less and SMuRF patients. We calculated the percent mediation by dividing the indirect effect with the total effect and presented the proportion of the total effect attributable to the mediator. These analyses were performed with the mma package, as detailed elsewhere [17].
The present study did not impute missing values for SBP and heart rate in the
models, since the missing data was minimal (
All statistical analyses were performed by SAS (version 9.4,
SAS Institute Inc., Cary, NC, USA) and software R (version 4.2.1, R Foundation
for Statistical Computing, Vienna, Austria). A two-sided p value
We included 16,541 patients (4970 women [30.0%], median age 66 years [56–74]), of whom 3288 (19.9%) had no documented SMuRFs and were henceforth referred to as SMuRF-less.
Baseline characteristics
are presented in Table 1. SMuRF-less individuals were older (69 years [59–76]
vs. 65 years [55–74], p
| Variable | SMuRF-less (N = 3288) | p value | |||
| Age (years), median (interquartile range) | 69 (59, 76) | 65 (55, 74) | |||
| Age (years), N (%) | |||||
| 79 (2.4) | 372 (2.8) | ||||
| 40–59 | 789 (24.0) | 4345 (32.8) | |||
| 60–79 | 1873 (57.0) | 7158 (54.0) | |||
| 547 (16.6) | 1378 (10.4) | ||||
| Female, N (%) | 1104 (33.6) | 3866 (29.2) | |||
| Medical history, N (%) | |||||
| Stroke | 251 (7.6) | 1705 (12.9) | |||
| Peripheral arterial disease | 1 (0.0) | 16 (0.1) | 0.224 | ||
| Atrial fibrillation | 29 (0.9) | 105 (0.8) | 0.607 | ||
| Chronic renal disease | 37 (1.1) | 300 (2.3) | |||
| Heart failure | 28 (0.9) | 79 (0.6) | 0.102 | ||
| Time from symptom onset to admission (hours), median (interquartile range) | 15 (4, 72) | 16 (4, 72) | 0.970 | ||
| Clinical profile at admission | |||||
| Chest discomfort, N (%) | 2940 (89.4) | 12,265 (92.5) | |||
| Cardiogenic shock, N (%) | 310 (9.4) | 803 (6.1) | |||
| Acute stroke, N (%) | 56 (1.7) | 245 (1.8) | 0.576 | ||
| Cardiac arrest, N (%) | 52 (1.6) | 168 (1.3) | 0.160 | ||
| SBP (mmHg), median (interquartile range) | 120 (100, 130) | 130 (111, 150) | |||
| SBP (mmHg), N (%) | |||||
| 317 (9.7) | 581 (4.4) | ||||
| 90–139 | 2365 (72.1) | 7652 (57.8) | |||
| 598 (18.2) | 4997 (37.8) | ||||
| Heart rate (beats/min), median (interquartile range) | 76 (64, 90) | 78 (66, 90) | 0.139 | ||
| Left ventricular ejection fraction (%) |
55 (46, 61) | 56 (48, 62) | 0.003 | ||
| CRP (mg/L) |
9.4 (4.1, 35.9) | 7.0 (3.0, 28.1) | 0.106 | ||
| Total cholesterol (mmol/L) |
4.0 (3.5, 4.5) | 4.7 (3.9, 5.4) | |||
| LDL-C (mmol/L) |
2.3 (1.9, 2.8) | 2.8 (2.2, 3.5) | |||
| HDL-C (mmol/L) |
1.1 (0.9, 1.3) | 1.1 (0.9, 1.3) | 0.859 | ||
| Triglycerides (mmol/L) |
1.1 (0.8, 1.5) | 1.3 (1.0, 2.0) | |||
| Glucose (mmol/L) |
6.4 (5.4, 8.2) | 7.0 (5.7, 9.5) | |||
| Hemoglobin (g/L) |
130 (117, 143) | 135 (122, 148) | |||
| Hematocrit (%) |
39 (35, 42) | 40 (36, 44) | |||
| EGFR (mL/min per 1.73 m²) |
80.5 (59.9, 102.0) | 84.2 (64.4, 105.8) | |||
| Duration from admission to cardiac enzyme measurement (minutes) |
107 (12, 630) | 93 (7, 340) | |||
| Concentration of troponin (multiple of upper limit of normal) |
37.7 (5.2, 146.0) | 37.5 (6.1, 168.7) | 0.142 | ||
| Admission ward, N (%) | |||||
| Cardiac ward | 1375 (41.8) | 7263 (54.8) | |||
| Non-Cardiac ward | 1913 (58.2) | 5990 (45.2) | |||
| Hospital characteristics, N (%) | |||||
| Teaching hospital | 2267 (68.9) | 10,633 (80.2) | |||
| PCI-capable hospital | 1820 (55.4) | 9595 (72.4) | |||
| Hospital with CCU | 1031 (31.4) | 2676 (20.2) | |||
| Economic-geographic region, N (%) | |||||
| Central | 942 (28.6) | 2992 (22.6) | |||
| Eastern | 1620 (49.3) | 7578 (57.2) | |||
| Western | 726 (22.1) | 2683 (20.2) | |||
| Urban/rural, N (%) | |||||
| Urban | 1672 (50.9) | 8421 (63.5) | |||
| Rural | 1616 (49.1) | 4832 (36.5) | |||
Abbreviations: SBP, systolic blood pressure; CRP, C-reactive protein; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; EGFR, estimated glomerular filtration rate; PCI, percutaneous coronary intervention; CCU, cardiac care unit; SMuRF, standard modifiable cardiovascular risk factor; N, number.
The proportion of eligible patients for aspirin, P2Y
Among eligible patients, those in the SMuRF-less group were
less likely to be treated with medications, including aspirin (89.0% vs. 94.7%,
p
| SMuRF-less | Adjusted OR (SMuRF-less versus |
p value | |||
| Medical therapies, N (%) | |||||
| Aspirin within 24 h | 2452 (83.7) | 11,239 (88.9) | 0.77 (0.68, 0.88) | ||
| P2Y |
1606 (55.0) | 9051 (71.8) | 0.72 (0.64, 0.81) | ||
| DAPT within 24 h | 1561 (53.5) | 8757 (69.6) | 0.76 (0.67, 0.85) | ||
| 821 (37.4) | 4566 (44.7) | 0.92 (0.82, 1.02) | 0.117 | ||
| ACE inhibitor/ARB within 24 h | 1384 (50.2) | 8231 (67.3) | 0.57 (0.52, 0.62) | ||
| Statin within 24 h | 1901 (64.5) | 9922 (78.1) | 0.76 (0.67, 0.85) | ||
| Aspirin | 2606 (89.0) | 11,963 (94.7) | 0.64 (0.54, 0.76) | ||
| P2Y |
1784 (61.1) | 9908 (78.6) | 0.67 (0.58, 0.76) | ||
| DAPT | 1734 (59.4) | 9687 (77.0) | 0.67 (0.59, 0.76) | ||
| 1721 (78.3) | 8745 (85.7) | 0.66 (0.58, 0.75) | |||
| ACE inhibitor or ARB | 1376 (49.9) | 8333 (68.1) | 0.56 (0.51, 0.61) | ||
| Statin | 2059 (69.9) | 10,814 (85.1) | 0.61 (0.53, 0.70) | ||
| Procedures, N (%) | |||||
| Cardiac catheterization | 715 (43.9) | 4841 (52.4) | 0.88 (0.77, 1.01) | 0.070 | |
| Coronary artery lesion, |
|||||
| Intermediate | 5 (1.4) | 55 (2.2) | / | 0.547 | |
| Left anterior descending artery | 295 (80.4) | 2104 (84.8) | / | 0.032 | |
| Left circumflex artery | 162 (44.1) | 1426 (57.5) | / | ||
| Right coronary artery | 246 (67.1) | 1697 (68.4) | / | 0.791 | |
| Left main coronary artery | 25 (6.8) | 137 (5.5) | / | 0.399 | |
| Multivessel disease, |
236 (64.3) | 1800 (72.6) | / | 0.001 | |
| Non-obstructive coronary disease, N (%) |
14 (3.8) | 51 (2.1) | / | 0.035 | |
| PCI (non-primary) | 322 (19.8) | 2152 (23.3) | 0.86 (0.75, 0.99) | 0.038 | |
| CABG | 6 (0.2) | 48 (0.4) | 0.83 (0.35, 2.00) | 0.684 | |
| Reperfusion therapies, N (%) | |||||
| Primary PCI | 262 (17.3) | 1992 (28.8) | 0.80 (0.66, 0.98) | 0.028 | |
| Fibrinolytic therapy | 532 (35.0) | 2275 (32.9) | 0.88 (0.76, 1.01) | 0.065 | |
Abbreviations: DAPT, dual antiplatelet therapy; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; SMuRF, standard modifiable cardiovascular risk factor; OR, odds ratio; N, number.
Individuals without
SMuRFs experienced significantly higher crude in-hospital
mortality (18.5% vs. 10.5%, p
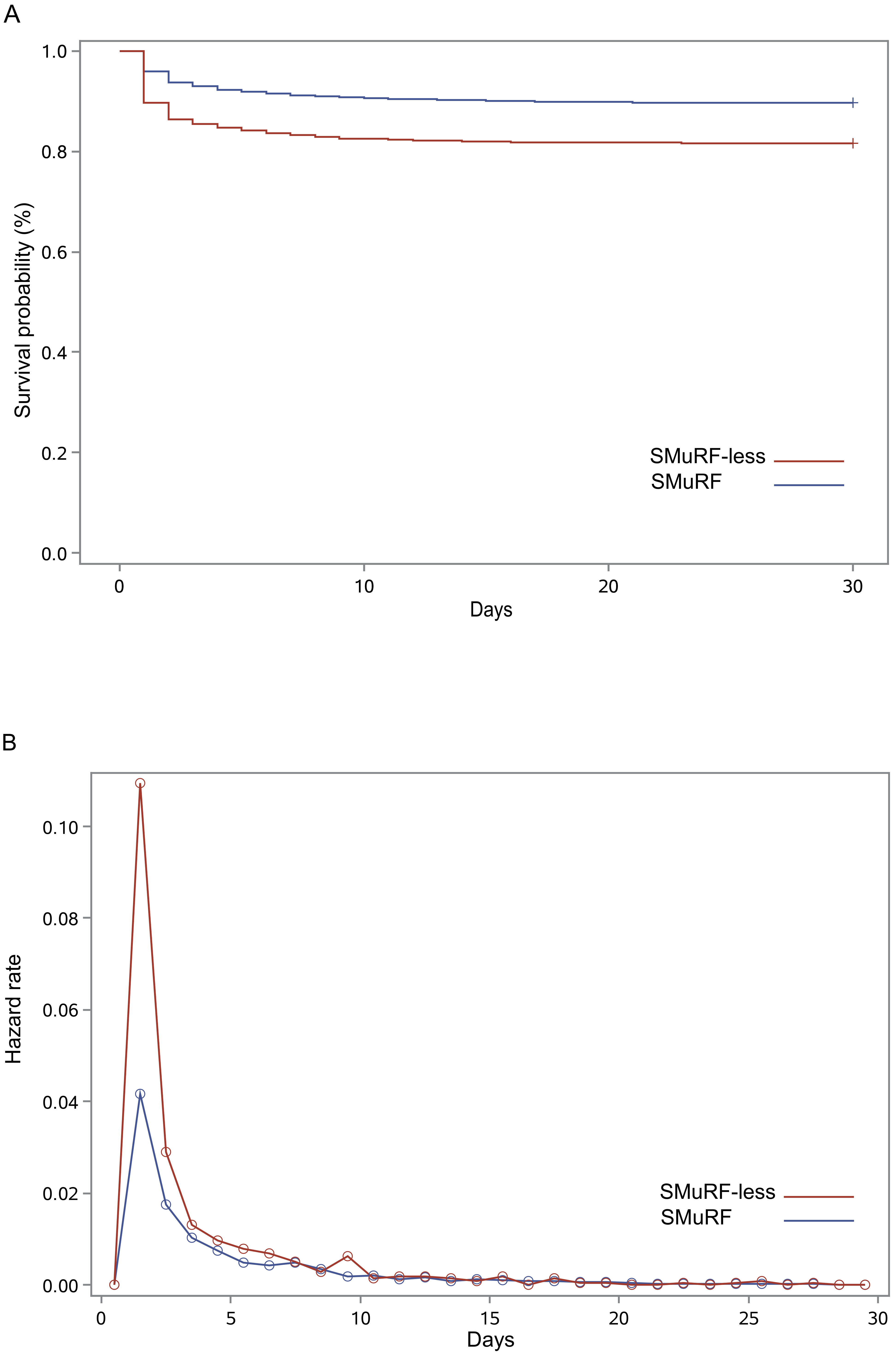 Fig. 1.
Fig. 1.Survival curves and hazard function curves based on SMuRF status. (A) Kaplan-Meier survival curves for in-hospital mortality until discharge. (B) Hazard function for mortality during hospitalization. SMuRF, standard modifiable cardiovascular risk factor.
After adjustment for age and sex, the SMuRF-less group had a 68% greater risk of in-hospital death (OR 1.68; 95% CI 1.50–1.88) (Fig. 2). This difference was reduced after adjusting for clinical profiles (OR 1.41; 95% CI 1.25–1.59). After further adjustment for in-hospital treatment, the difference was no longer significant (OR 1.05; 95% CI 0.92–1.20). Among all of the individual treatments, the use of ACE inhibitors/ARBs (OR 1.29; 95% CI 1.15–1.45) or statins (OR 1.36; 95% CI 1.21–1.54) resulted in the largest reduction in the OR of mortality for SMuRF-less patients (Supplementary Fig. 3). The results of these analyses agreed with those for sex stratification (Supplementary Figs. 4,5) and for the use of a 7-day timeframe (Supplementary Figs. 6,7). However, after excluding individuals who died within 24 hours of admission and after adjusting for age and sex, the disparity in in-hospital mortality was only marginally significant (OR 1.16; 95% CI 1.00–1.35) (Supplementary Fig. 8).
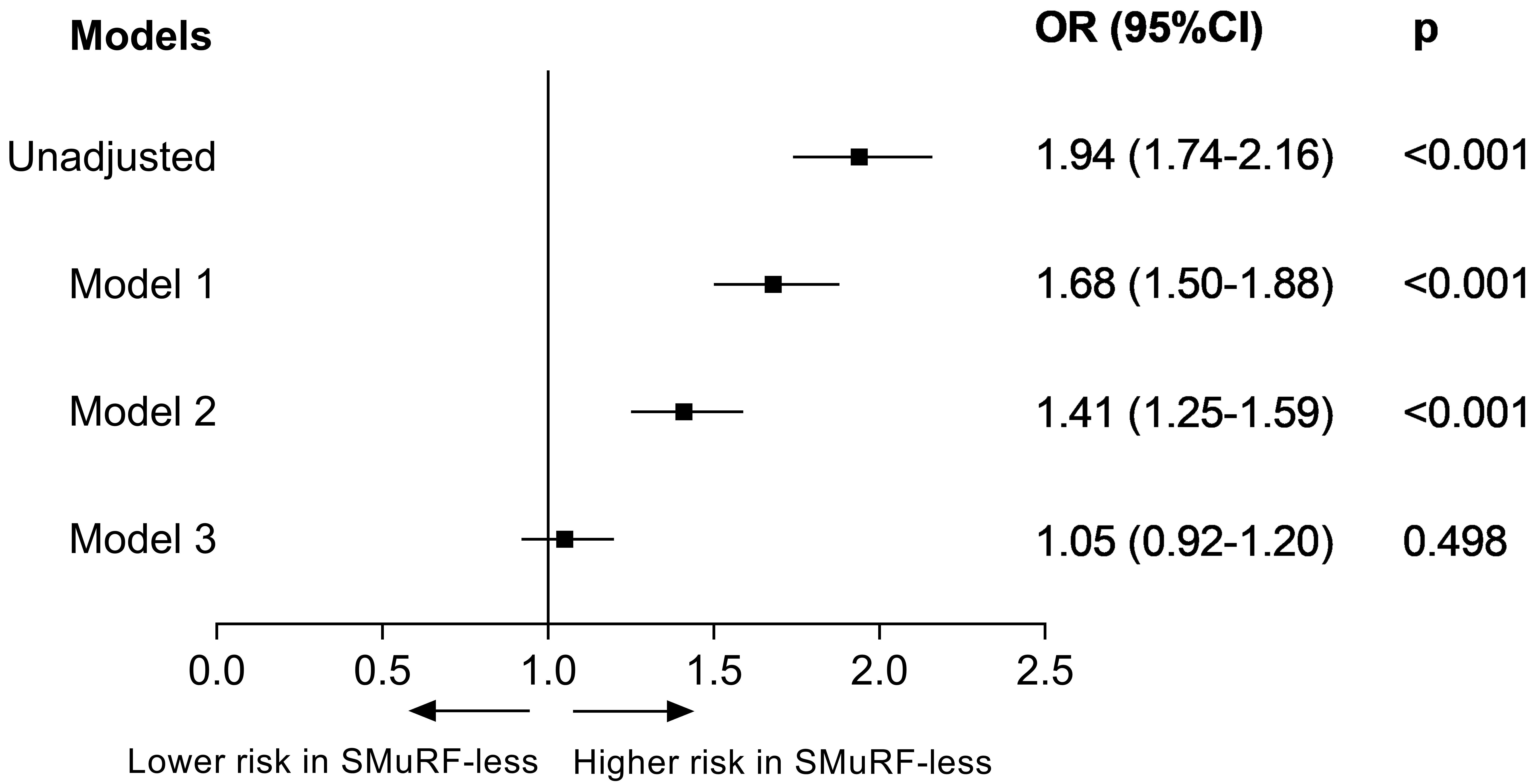 Fig. 2.
Fig. 2.Adjusted odds ratio for mortality during hospitalization between patients with and without
SMuRFs. Model 1: adjusted for age and sex; Model 2:
adjusted for the variables in model 1 and for the clinical profiles (including
previous stroke, previous atrial fibrillation, previous chronic renal disease,
previous heart failure, previous peripheral arterial disease, chest discomfort,
cardiac arrest at admission, cardiogenic shock at admission, stroke at admission,
heart rate, and systolic blood pressure); Model 3: adjusted for the variables in
model 2 and for in-hospital pharmacotherapies (including aspirin, P2Y
Table 3 lists the mediating factors and their percent mediation in the overall population. Mediating factors were estimated to account for 92.5% of the excess in-hospital mortality observed in SMuRF-less patients compared to those who had SMuRFs. Although 23.0% of the excess mortality in SMuRF-less patients was mediated by worse clinical profiles, the majority (69.1%) was mediated by suboptimal in-hospital treatment. The contributions from in-hospital statin and ACE inhibitor/ARB treatments were 32.5% and 22.4%, respectively, accounting for the largest proportion of difference in mortality. The mediation analyses were repeated in the eligible patients, with similar results obtained. Among the eligible patients for ACE inhibitors/ARBs, 23.4% of the excess in-hospital mortality was due to the underuse of this treatment, while among the eligible ones for statins, 30.6% of excess mortality was due to treatment underuse.
| Mediated effect | |||
| Total indirect effect |
92.5% | ||
| Indirect effect through: | |||
| Clinical profile | 23.0% | ||
| Systolic blood pressure | 9.6% | ||
| Cardiogenic shock at admission | 3.7% | ||
| Acute stroke at admission | 1.9% | ||
| In-hospital treatment | 69.1% | ||
| In-hospital statin | 32.5% | ||
| In-hospital ACE inhibitor/ARB | 22.4% | ||
| In-hospital |
7.7% | ||
| Primary PCI | 7.4% | ||
| In-hospital aspirin | 3.4% | ||
| In-hospital P2Y |
2.4% | ||
| In-hospital DAPT | 1.6% | ||
Abbreviations: ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; PCI, percutaneous coronary intervention; DAPT, dual antiplatelet therapy; SMuRF, standard modifiable cardiovascular risk factor.
After excluding patients who died within 24 hours of hospitalization, mediation analyses produced similar results to those of the overall population, i.e., 30.3% of the difference in mortality between SMuRF-less and SMuRF patients could be explained by the underuse of ACE inhibitors, and 13.8% by the underuse of statins.
Given that the most prominent in-hospital mortality difference was within the
first 24 hours of hospitalization, we performed a sensitivity analysis using
mediation analysis to examine the potential contributors to
excess mortality in SMuRF-less patients within this period (Supplementary
Table 4). The clinical profiles and treatments within 24 hours jointly accounted
for 57.9% of the relationship between the SMuRF-less status and
mortality within 24 hours. The underuse of P2Y
Almost one in five patients hospitalized for STEMI in China has no SMuRFs. Compared to patients with SMuRFs, SMuRF-less individuals presented with a more serious condition and received fewer evidence-based therapies, even among the eligible patients. The higher risk of in-hospital mortality in SMuRF-less patients was largely explained by the differences in the severity of illness and in-hospital treatments. In particular, the underuse of statins and ACE inhibitors/ARBs contributed to most of the excess risk of death in SMuRF-less patients.
In this
nationally representative sample of Chinese patients
hospitalized for STEMI, the proportion of SMuRF-less patients was similar to that
reported in developed countries [1, 3, 12]. However, it was almost 2-fold higher
than reported in the CAMI (China Acute Myocardial Infarction) registry study [2],
possibly due to the differences in study design. The CAMI registry study
prospectively enrolled patients from a
non-random sample, therefore potentially
missing some patients who died during the very early phase of hospitalization
[2]. Of note, we observed that
In line with previous studies, SMuRF-less patients were sicker and older [1, 2, 10, 18, 19]. The older age may increase the absolute baseline risk of AMI, independent of SMuRFs [11, 20]. In addition, SMuRF-less patients presented more often with cardiogenic shock at admission, and had higher mortality within the first 24 hours. Reduced or absent myocardial ischemic preconditioning, or differences in plaque composition, may partially explain the more severe presentation of SMuRF-less patients [7, 21]. Recent studies also reported a larger infarct size, worse flow (grade 0/1), and less calcification in SMuRF-less patients [7, 22].
As reported earlier, SMuRF-less patients received fewer evidence-based therapies [2, 3, 10, 11, 23]. Potential explanations for this undertreatment include: (1) less eligibility for therapy due to a more severe condition, (2) limited treatment opportunities due to early death, (3) delayed diagnosis due to atypical symptoms, and (4) treatment bias because of lower risk factors. Here, we extended previous studies by only focusing on patients who had no contraindications and survived the first 24 hours upon admission. Nevertheless, we found this group remained undertreated. Importantly, we observed that fewer SMuRF-less patients had chest discomfort and were admitted to the cardiac ward, possibly reflecting early diagnostic uncertainty [24]. The delayed diagnosis may lead to a delay in the initial management and, subsequently, to undertreatment. Reperfusion therapy, in particular, is required to be performed within a recommended time window [25]. The lack of hypertension and hypercholesterolemia in individuals without SMuRFs may also partially explain their undertreatment [12, 22, 26]. These findings suggest that there might be an unreasonable risk factor-driven treatment bias, i.e., only patients with risk factors would be treated with ACE inhibitors/ARBs or statins in clinical practice.
A higher rate of in-hospital mortality was observed in SMuRF-less patients. Particularly, the most prominent excess mortality occurred within the first 24 hours. This finding extended previous studies [1, 3, 5, 11, 12], and first restricted the difference in outcome to the very early stage. The worse baseline profiles and suboptimal treatment of SMuRF-less patients contribute to the excess in-hospital mortality. Mediation analyses allowed us to better identify the contributors, of which the underuse of clinical care was observed as the most important contributor. In particular, the suboptimal use of statins and ACE inhibitors/ARBs contributed the largest proportion to the excess risk of in-hospital mortality. And the immediate underuse of antiplatelet therapy was the largest contributor to the excess risk of death within 24 hours. Our results concur with prior research showing that immediate initiation of statins [27, 28], ACE inhibitors [29, 30], and antiplatelet therapy reduce in-hospital mortality after STEMI [31]. Despite the benefits of early reperfusion therapy, its impact on mortality between the two groups was modest in this study. As mentioned above, the underuse of statins and ACE inhibitors/ARBs might be due to risk-driven bias, while the underuse of antiplatelet therapy could be due to the delay in diagnosis.
As the first nationally representative study to describe the characteristics of STEMI patients without SMuRFs in developing countries, our study has several clinical implications. First, physicians should be aware of the disparities in presentation between SMuRF-less and SMuRF patients to minimize the delays in recognition and triage. Second, our mediation analyses first found that the underuse of ACEI/ARB and statins explained most of the excess in-hospital mortality of SMuRF-less patients,emphasizing the importance of equitable treatments for this population. It is also worth highlighting that suboptimal treatments exist not only in SMuRF-less patients but also in SMuRF patients, suggesting that there is room to improve overall care for all AMI patients. Prior studies also showed suboptimal prescriptions for secondary prevention and poor risk factor control in patients with risk factors [32, 33]. Quality improvement programs and the establishment of national systemic measures of performance may provide additional impetus to improve the care with AMI [34]. Additionally, during primary care and specialist follow-ups, the importance of medication adherence should be emphasized at each consultation, and referral for additional support should be recommended if necessary. Third, the large number of SMuRF-less patients indicates the need to explore new markers for early atherosclerosis and improve the available risk tools in order to prevent AMI events, as traditional risk assessment methods are inadequate. Large-scale genome-wide association studies have found 55 genetic loci linked to coronary artery disease, with 66% of these loci being unrelated to conventional cardiovascular risk factors [35]. Imaging and biochemistry studies have also detected subclinical atherogenesis, even in healthy SMuRF-less individuals [36, 37]. It is therefore important to develop better risk prediction tools, including genetic, metabolomic, inflammatory, and imaging markers. Fourth, the primary prevention strategy in SMuRF-less individuals should be reconsidered. The US Preventive Services Task Force recently advised that clinicians offer or refer to behavioral counseling interventions to encourage physical activity and healthy eating to prevent cardiovascular disease in people without traditional risk factors [38]. Fifth, about 40% of the excess mortality of SMuRF-less patients occurring within 24 hours of admission has no obvious explanation. This indicates there are knowledge gaps in the underlying biological mechanisms responsible for early death after the onset of STEMI. Our findings could enable a better understanding of this often overlooked population in developing countries, where data is still quite limited.
Our study has several limitations. First, the data were
retrospectively collected based on medical records. The lack of quantified
variables, such as socioeconomic factors, lifestyle, and lipoprotein (a), might
cause some residual confounding. It has been demonstrated that low lipoprotein (a)
concentration (
Almost one-fifth of patients hospitalized for STEMI in China had no SMuRFs. These patients were more ill than those with SMuRFs, with half of them dying within 24 hours of hospitalization. Moreover, they received fewer recommended therapies and had higher hospital mortality rates, mainly due to suboptimal treatment. The underuse of ACE inhibitors/ARBs and statins explained a large percentage of the excess mortality of both overall and eligible SMuRF-less patients, which highlights the need to optimize evidence-based health care to address the disparity in outcome.
STEMI, ST-segment elevation myocardial infarction; SMuRFs, standard modifiable cardiovascular risk factors; China PEACE-Retrospective AMI, China Patient-centered Evaluative Assessment of Cardiac Events Retrospective Study of Acute Myocardial Infarction; AMI, acute myocardial infarction; ECGs, electrocardiograms; PCI, percutaneous coronary intervention; DAPT, dual antiplatelet therapy; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; SBP, systolic blood pressure; OR, odds ratio; CI, confidence interval; CAMI, China Acute Myocardial Infarction.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
WG and XZ designed the research study. WG, XZ, and XL performed the research. YW and WG analyzed the data. WG and YW drafted and revised the manuscript. JY and AT contributed substantially in the design of the study and interpretation of data. JLiu, HZ, SH, and JLi were major contributors in the acquisition and interpretation of data and contributed to the critical revision of the manuscript. All authors read and approved the final manuscript. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The central ethics committee at the China National Center for Cardiovascular Diseases approved the study (approval number: 2012-377), with a waiver of patients’ written consent given the retrospective nature. All collaborating hospitals accepted the central ethics approval or obtained local approval from an internal ethics committee.
We appreciate the multiple contributions made by study teams at the National Clinical Research Center for Cardiovascular Diseases and the Yale New Haven Hospital Center for Outcomes Research and Evaluation in the realms of study design and operation. We thank the support provided by the Chinese government.
This research was funded by CAMS Innovation Fund for Medical Sciences (CIFMS), 2021-I2M-1-011.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.rcm2409249.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.


