- Academic Editor
Background: Congenital heart disease (CHD) is a leading cause of
childhood morbidity, with an estimated prevalence of 0.8–1%. However, advances
in diagnosis and treatment now allow 90% of childhood CHD patients to survive to
adulthood, leading to increased interest in their quality of life (QoL). In this
study, we examine the impact of clinical and psychosocial variables, including
the number of surgical interventions (NSI), age at surgery, school achievement,
and social support, as mediating factors of QoL in CHD patients.
Methods: The study included 233 CHD patients (132 males) with an average
age of 15.2
This study is part of a broad research line dedicated to the study of congenital heart disease (CHD) in adolescents and young adults, which aims to understand the impact of the disease on quality of life (QoL), psychosocial adjustment, neurocognitive performance, as well as on associated psychiatric morbidity.
CHD is currently the leading cause of childhood morbidity. Estimates of its current prevalence are between 1 case in 100 births (1%) [1, 2, 3] and 5 to 8 cases in 1000 births (0.8%) [4]. In the 1950s, only 20% of children born with moderate or severe CHD (such as tetralogy of Fallot, transposition of the great arteries, and hypoplastic left heart syndrome) survived the first year of life [4]. Over the last decades, with progress in diagnosis and surgical conditions, 90% of patients with CHD survive to adulthood. That represents a new challenge, as blood flow and hypoxia during critical phases of fetal brain development may have irreversible consequences, leading to life-long cognitive impairment and generating interest in the study of their psychosocial adjustment, psychiatric morbidity, QoL, and their Neurocognitive performance [2, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15].
The diagnostic and therapeutic advances in CHD have contributed to decreased infant mortality and an increasing number of adolescents and adults with CHD. CHD is currently considered a chronic disease, so these patients face several difficulties in several domains. Survival does not always mean high QoL, with the need for hospitalization or interruption of pleasurable activities [3]. As a result, one of the key aspects for assessing healthcare impact outcomes in these patients is the study of variables associated with functional health, such as exercise capacity, or variables related to health indicators (such as a cardiopulmonary function) related to the patient’s QoL [16, 17, 18]. In addition, QoL is now widely used in exploratory studies on the efficacy of treatment methods from the patient’s point of view [19] to serve as the basis for guiding the decisions of professionals and patients at the level of the most appropriate healthcare. The definition of health by the World Health Organization (WHO) [20] implies that assessments of health status and their effects also include indicators of well-being, which can be achieved by evaluating health-related QoL.
The WHO defines QoL as the individual’s perception of their position in life in the context of their culture, the value system in which they live and their goals, expectations, standards, and concerns. QoL is a comprehensive concept that is affected by physical health, psychological state, personal beliefs, social relations, and its relationship with the salient characteristics of its environment [3, 20]. Studies have evaluated the relationship between health, illness, frequent hospitalizations, medical therapy, or health care with QoL in the patient’s physical, social, or psychological functioning [21]. The results in the physical domain of QoL turned out to be lower in adolescents with tetralogy of Fallot compared to healthy adolescents and in the domain of social relations when associated with executive dysfunctions associated with attention deficit hyperactivity disorder [22]. Some studies have found that children and adolescents with CHD show symptomatology of anxiety and/or depression related to the limitations imposed by the disease, frequent hospitalizations and, in some cases, the need for regular medication [3], as well as changes in body image in the postoperative period (which often leaves a large scar on the chest). As a result, these children become more introverted and isolated from others because they feel shame and guilt for their body image. One reason for poor QoL is the lack of social acceptance, especially in the school setting [3]. Wernovsky [23] have studied the school performance of these children and adolescents with CHD, which tends to be marked by various irregularities, such as learning difficulties, poor performance, behaviour problems, reduced socialization skills, low self-esteem and, in less frequent cases, delinquency, absenteeism, due to hospital admissions, surgeries and frequent treatments. One of the reasons for having a poor QoL is the lack of social acceptance, especially in the school environment [3]. Physical activity restrictions have an impact on the QoL of children with CHD, whether they are the same as those imposed by the disease condition, which reduces the opportunity to enjoy the benefits of physical activity for mental health [24], or by parents, who are often overprotective [3]. Patients often report problems such as shortness of breath, tiredness, chest pain, and dizziness during exercise [19].
Patients with CHD are regularly followed up at health services, where certain clinical variables (presence or absence of cyanosis, the severity of disease, surgical interventions, need for pharmacological therapy, presence of residual lesions) can help understand the situation and to ensure the best care. Among the variables above, the surgical interventions (their need, their quantity) may impact the perception of QoL, mainly in the physical domain [25]. Several studies have shown that newborns with CHD have a risk of neurodevelopmental changes before surgery, confirmed by neuroimaging [4, 26]. These changes are observed in the preoperative phase, suggesting the presence of cerebral anomalies in children with CHD [4]. Magnetic resonance imaging of the brain, performed before surgery, demonstrates a high incidence of preoperative brain injuries, such as corneal agenesis, holoprosencephaly, microcephaly, lissencephaly, Dandy-Walker malformation, and immature cortical mantle [5].
There has been much debate about the effect of cardiac surgery (with thoracic cavity opening) on neurocognitive performance in children and adolescents with CHD [13, 27, 28, 29].
In addition to the studies on the impact of surgical interventions on the health-related medical conditions of patients with CHD, some studies already focus on the QoL of these patients [30, 31]. The impact of the implantation of a prosthetic heart valve on the QoL has been studied since these patients are confronted with specific postoperative problems, such as the need for anticoagulants, the expected problems in future pregnancies (in the case of women), and the new operations provided by the prosthetic valve degeneration [30, 32].
As several of these consequences may arise from mild, moderate, or severe forms of CHD, it is crucial to plan adequate clinical resources and support to understand the underlying mechanisms that may explain different patterns of adaptation in patients, some fostering resilience and others increasing detrimental effects.
Therefore, in this study, we intended to test several mediation mechanisms between the severity of illness, the presence of cyanosis, and the QoL of patients. We hypothesized that some clinical (number of surgical interventions (NSI), age at first surgery) and psychosocial variables (school achievement, social support) might be mediators of the impact of illness in QoL in its different domains (physical, psychological, social relationships, environmental, and general).
Thus, this study examines the importance of selected clinical variables (NSI) in mediating the impact of CHD (namely severity and presence/absence of cyanosis) on the perception of QoL in patients.
To pursue this aim, we started by considering the following research hypotheses: (1) NSI has a mediating mechanism of impact, influencing the effect of type of congenital heart disease (TCHD) and decreasing the perception of QoL in patients with the cyanotic disease; and (2) NSI has a mediating mechanism of impact, influencing the effect of severity of congenital heart disease (SCHD) and decreasing the perception of QoL in patients with more severe diseases.
Then, we operationalized these main hypotheses in possible models of mediation. For each possible model, we defined and tested three paths (a, b, c) according to mediation meaning: (a) variations in the levels of the independent variable significantly give rise to variations in the presumed mediator; (b) variations in the mediator significantly give rise to variations in the dependent variable; and (c) when paths a and b are controlled, the previously significant relationship between the independent and dependent variables is no longer significant.
We are interested in better understanding how the severity and/or presence of cyanosis in CHD affects the QoL of patients. Therefore, we used mediation analysis to investigate the perception of QoL in patients with CHD.
Fig. 1 presents a diagram with the ten mediation models that we tested for the criterion variable “QoL”.
 Fig. 1.
Fig. 1.Diagram of mediation models. Blue: Models considering variable X1: Type of CHD (TCHD); Green: Models considering variable X2: Severity of CHD (SCHD). CHD, congenital heart disease; QoL, quality of life.
For each model, we tested three hypotheses:
Hypothesis 1: TCHD, the presence of cyanotic or acyanotic disease, or SCHD (severe, moderate, or mild), and NSI are positively related.
Hypothesis 2: NSI is negatively related to a specific domain or general QoL in patients with CHD.
Hypothesis 3: TCHD or SCHD is sequentially positively associated with NSI and is also associated with a decreased perception of a specific domain or general QoL. Estimating the indirect effect of the mediator (NSI) using the bias-corrected bootstrap method produces a confidence interval that does not include zero.
Model 1: Predictive mediator effect of NSI on patients’ perception of the psychological domain in QoL (PQoL) according to TCHD.
Model 2: Predictive mediator effect of NSI on the perception of social relationships domain in QoL (SRQoL) of patients according to TCHD.
Model 3: Predictive mediator effect of NSI on patients’ perception of the physical domain in QoL (PHQoL) according to TCHD.
Model 4: Predictive mediator effect of NSI on patients’ perception of the environmental domain in QoL (EQoL) according to TCHD.
Model 5: Predictive mediator effect of NSI on patients’ perception of the general domain in QoL (GQoL) according to TCHD.
Model 6: Predictive mediator effect of NSI on the perception of PQoL of patients according to SCHD.
Model 7: Predictive mediator effect of NSI on the perception of SRQoL of patients according to SCHD.
Model 8: Predictive mediator effect of NSI on the perception of PHQoL of patients according to SCHD.
Model 9: Predictive mediator effect of NSI on the perception of EQoL of patients according to SCHD.
Model 10: Predictive mediator effect of NSI on the perception of GQoL of patients according to SCHD.
Participants were recruited consecutively at a tertiary university hospital’s outpatient pediatric cardiology clinic in northern Portugal. We included only patients with complete medical records, aged between 12 and 25 years, and the necessary basic educational level to understand and complete the written questionnaires. We excluded those patients with associated extracardiac malformations, mental or physical comorbidity, or chromosomal disorders that might have associated cognitive development problems. Of all patients invited, only nine refused to participate. Three-hundred-ninety-three patients participated in the study, but only 233 completed the protocol, considering neurocognitive variables and neonatal markers in fetal development. According to Table 1 we included only patients with complete medical records, aged between 12 and 25 years. Table 2 describes the distribution of participants according to the different clinical variables considered.
| Sociodemographic characteristics | Patients N = 233 | |
| Sex | Male | 132 |
| Female | 101 | |
| Age (in years) | Range | 12–21 |
| (M |
15.2 | |
| Years completed at school | 9.4 | |
| Years completed at school by father | 9.7 | |
| Years completed at school by mother | 10.3 | |
| Completed education | 2nd cycle | 27 |
| 3rd cycle | 116 | |
| Secondary level | 84 | |
| University degree | 5 | |
| Retentions at school | Number of patients | 69 |
| Years of retention (M |
0.5 | |
| Marital Status | Single | 233 |
| Married | 0 | |
| Divorced | 0 | |
| Living in marital union | 0 | |
N, No. of patients; M, mean; SD, standard deviation.
| Clinical variables | Number of patients (N = 233) | |
| Age when diagnosed | Neonatal period | 138 |
| Until 1 year | 49 | |
| 1–3 years | 13 | |
| 3–6 years | 12 | |
| 6–12 years | 15 | |
| 12–18 years | 6 | |
| Severity of CHD | Severe | 30 |
| Moderate | 119 | |
| Mild | 84 | |
| Type of CHD | Cyanotic | 80 |
| Acyanotic | 153 | |
| Residual lesions | Severe/moderate | 27 |
| Mild | 138 | |
| Without | 68 | |
| Intensive care | Yes | 163 |
| No | 70 | |
| Physical limitations | Physical limitations | 85 |
| Satisfactory physical competence | 148 | |
| Pharmacological therapy | Yes | 57 |
| No | 176 | |
| Surgical interventions | Yes | 163 |
| No | 70 | |
| Number of surgical interventions | 0 | 70 |
| 1 | 109 | |
| 2–4 | 50 | |
| 5–8 | 3 | |
| 10 or more | 1 | |
| Age at first surgery | Neonatal period | 68 |
| 7 months until 1 year | 28 | |
| 1–3 years | 23 | |
| 3–6 years | 18 | |
| 6–12 years | 20 | |
| 12–18 years | 6 | |
| Without surgery | 70 | |
CHD, congenital heart disease.
Relevant clinical data were collected retrospectively using each patient’s clinical record, including diagnosis, severity, category of CHD and surgical interventions, pharmacological therapy, and presence of residual lesions. Personal and demographic data were collected using a semi-structured interview focused on the relationship between the diagnosis of CHD and the various aspects of life. We used the Portuguese translation of the self-report questionnaire of the WHO (the WHOQOL-BREF) to assess subjective quality of life. This questionnaire is adapted to the general Portuguese population [33]. This questionnaire includes 26 questions, and the answers are filled in options of a Likert scale type, ranging from 1 to 5, where higher scores reveal a higher QoL, except for questions 3, 4, and 26, which are formulated inversely, and the scale is also inverted. The WHOQOL-Bref is organized into four domains of QoL: Physical (questions 3, 4, 10, 15, 16, 17, and 18), Psychological (questions 5, 6, 7, 11, 19 and 26), Social Relationships (questions 20, 21, and 22), and Environment (questions 8, 9, 12, 13, 14, 23, 24, and 25). Besides those, there is also an overall indicator, the General QoL, which includes the first two questions of the questionnaire. For each domain, the average of the scores needs to be calculated, and finally, the results are transformed into a scale from 0 to 100.
Additional questionnaires and evaluations were used in this research and are detailed in another paper. A neuropsychological evaluation was carried out to evaluate the performance of different neurocognitive functions that the literature has shown may affect CHD patients [34, 35]. We used the NEO Five-Factor Inventory (NEO-FFI, reduced version), a self-report questionnaire that provides data to access personality traits in five domains (Neuroticism, Extroversion, Openness to Experience, Kindness, and Responsibility). We also used a standardized psychiatric interview (SADS-L) for the clinical diagnosis of psychopathological disorders, covering the patient’s lifetime up to the moment of the interview.
The study design is cross-sectional, with all the assessments being performed simultaneously. The patient’s medical history was collected retrospectively with the collaboration of the medical and administrative staff.
Statistical analyzes were performed using the IBM SPSS Statistics for Windows program, version 27 (IBM Corp., Armonk, NY, USA). For the characterization of the participants, we used descriptive statistics. Regarding the variable TCHD (cyanotic and acyanotic), to ensure that the groups would be equivalent in the main demographic variables, we compared parents’ schooling using Student’s t-test.
To test the mediation hypotheses, we used Hayes’s PROCESS version 3.5.3 (http://www.processmacro.org) [36] (model 4) for SPSS using 5000 bootstrap simulations to calculate the total direct and indirect effects of the variables. Unstandardized coefficients were used to test each model’s first and second hypotheses. The point estimate of the specific indirect effect through the mediator was performed as a test of the third hypothesis of each model.
A total of 233 patients were enrolled in the study, comprising 132 males and 101
females aged between 12 and 21 years (mean age = 15.2
| Main diagnosis | Number of patients (N = 233) |
| Ventricular septal defect | 48 |
| Atrial septal defect | 21 |
| Atrioventricular septal defect | 6 |
| Coarctation of the aorta | 23 |
| Pulmonary stenosis | 19 |
| Aortic stenosis | 7 |
| Dysplastic pulmonary valve | 2 |
| Bicuspid aortic valve | 10 |
| Mitral valve prolapse | 4 |
| Ductus arteriosus | 1 |
| Dilated coronary sinus | 1 |
| Dilated cardiomyopathy | 3 |
| Tetralogy of fallot | 36 |
| Transposition of the great arteries | 31 |
| Anomalous pulmonary venous drainage | 4 |
| Pulmonary atresia | 5 |
| Tricuspid atresia | 3 |
| Double outlet right ventricle | 3 |
| Truncus arteriosus | 2 |
| Univentricular heart | 2 |
| Hypoplastic left heart ventricle | 1 |
| Not specified | 1 |
CHD, congenital heart disease.
Demographic characteristics of parents’ education were compared between cyanotic and acyanotic CHD patients. The Levene test was performed to assess the assumption of variance between the two groups for both father’s and mother’s schooling, and the results validated the hypothesis that variance was equal in both groups for the Student’s t-tests. The t-test results demonstrated that the groups were equivalent in terms of demographic variables, and no statistically significant difference was found between the groups (father’s education: t = –1.114, p = 0.267; mother’s education: t = 1.458, p = 0.147).
We analyzed ten mediation models to determine the predictive mediator effect of
NSI on QoL in patients with CHD. The first hypothesis was supported for all ten
mediation models, with TCHD and SCHD showing a statistically significant
relationship with NSI. The second hypothesis, which states that NSI is negatively
related to QoL, was supported in four models: Model 1 (TCHD-
Model 1: Mediating effect of NSI between TCHD and the perception of PQoL of patients.
Model 2: Mediating effect of NSI between TCHD and the perception of SRQoL of patients
Table 4 and Appendix Fig. 2 show that independent variable X [TCHD (cyanotic or
acyanotic)] has a statistically significant relationship with the mediator
variable (M): NSI (B = –0.8520, size of effect (SE) = 0.1856, t = –4.5902, p
| Predictive mediator effect of the number of surgical interventions (NSI) on the perception of Psychological Domain in QoL (PQoL) of patients according to Type of Congenital Heart Disease (TCHD) | |||||||
| Coeff | SE | t | p | LLCI | ULCI | ||
| Path a | TCHD (X) | –0.8520 | 0.1856 | –4.5902 |
0.0000 | –1.2182 | –0.4858 |
| Path b | NSI (M) | –2.1444 | 0.8018 | –2.6746 |
0.0082 | –3.7264 | –0.5625 |
| Path c | Total effect of X on Y | 1.3570 | 2.0468 | 0.6630 | 0.5082 | –2.6814 | 5.3954 |
| Path c’ | Direct effect of M on Y | –0.4701 | 2.1260 | –0.2211 | 0.8252 | –4.6648 | 3.7246 |
| Indirect effect of X on Y ab 95% bootstrap confidence interval | Effect | BootSE | BootLLCI | ||||
| NSI | 1.8271 | 0.9954 | 0.3121 | 4.2045 | |||
SE, size of effect; LLCI, lower limit of confidence interval; ULCI, upper limit
of confidence interval; QoL, quality of life; Boot, resampling simulation. The number of sample
simulations for bias correction of confidence intervals: Level of confidence for
all confidence intervals: 95.
 Fig. 2.
Fig. 2.Model 1: unstandardized path coefficients for mediation.
The direct effect between variables X: TCHD and Y: PQoL shows a positive
association (B = –0.4701, SE = 2.1260, t = –0.2211, p
Model 2: Mediating effect of NSI between TCHD and the perception of SRQoL of patients.
Table 5 and Appendix Fig. 3 show that hypothesis 1 is corroborated (the presence
of cyanosis is positively associated with statistical significance to the
increase in NSI). NSI is negatively correlated in a statistically significant way
with SRQoL (B = –2.0814, SE = 0.8179, t = –2.5448, p
| Predictive mediator effect of the number of surgical interventions (NSI) on the perception of Social Relationships Domain in QoL (SRQoL) of patients according to Type of Congenital Heart Disease (TCHD) | |||||||
| Coeff | SE | T | p | LLCI | ULCI | ||
| Path a | TCHD (X) | –0.8520 | 0.1856 | –4.5902 |
0.0000 | –1.2182 | –0.4858 |
| Path b | NSI (M) | –2.0814 | 0.8179 | –2.5448 |
0.0118 | –3.6952 | –0.4676 |
| Path c | Total effect of X on Y | –1.5928 | 2.0842 | 0.7642 | 0.4457 | –2.5194 | 5.7050 |
| Path c’ | Direct effect of M on Y | –0.1806 | 2.1687 | –0.0833 | 0.9337 | –4.4597 | 4.0985 |
| Indirect effect of X on Y ab 95% bootstrap confidence interval | Effect | BootSE | BootLLCI | ||||
| NSI | 1.7734 | 0.9804 | 0.0139 | 0.2983 | |||
SE, size of effect; LLCI, lower limit of confidence interval; ULCI, upper limit
of confidence interval; QoL, quality of life; Boot, resampling simulation. The number of sample
simulations for bias correction of confidence intervals: Level of confidence for
all confidence intervals: 95.
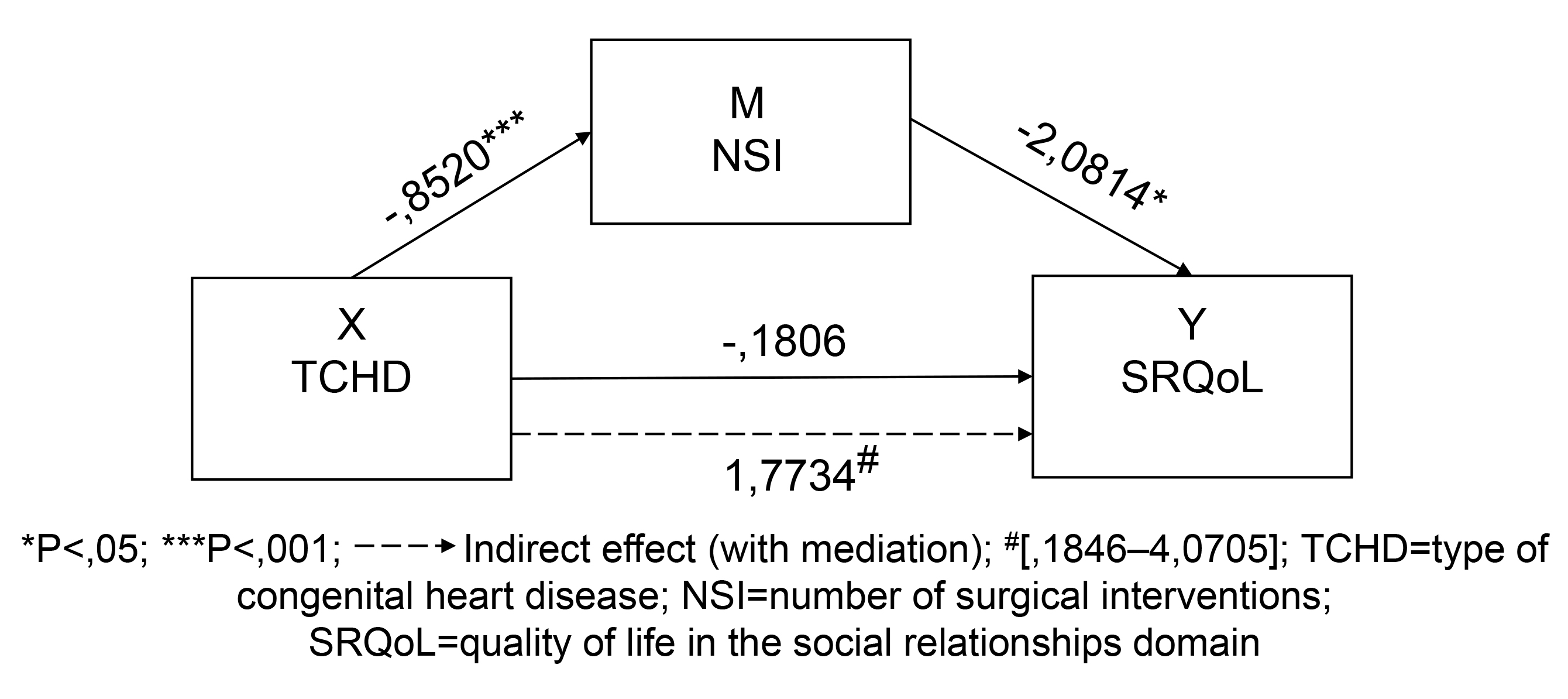 Fig. 3.
Fig. 3.Model 2: unstandardized path coefficients for mediation.
The direct effect between the variables X: TCHD and Y: SRQoL shows a positive
association (B = –0.1806, SE = 2.1687, t = –0.0833, p
Model 6: Mediating effect of NSI between SCHD and the perception of PQoL of patients.
Table 6 and Appendix Fig. 4 show that variable X: SCHD (severe, moderate, or
mild disease) has a statistically significant relationship with the variable M:
NSI (B = –0.6774, SE = 0.1321, t = –5.1271, p
| Predictive mediator effect of the number of surgical interventions (NSI) on the perception of Psychological Domain in QoL (PQoL) of patients according to Severity of Congenital Heart Disease (SCHD) | |||||||
| Coeff | Se | T | p | LLCI | ULCI | ||
| Path a | SCHD (X) | –0.6774 | 0.1321 | –5.1271 |
0.0000 | –0.9381 | –0.4167 |
| Path b | NSI (M) | –2.1608 | 0.8247 | –1.9947 |
0.0095 |
–3.7881 | –0.5335 |
| Path c | Total effect of X on Y | 0.9565 | 1.4855 | 0.6439 | 0.5205 | –1.9747 | 3.8877 |
| Path c’ | Direct effect of M on Y | –0.5073 | 1.5650 | –0.3241 | 0.7462 | –3.5955 | 2.5809 |
| Indirect effect of X on Y ab 95% bootstrap confidence interval | Effect | BootSE | BootLLCI | ||||
| NSI | 1.4638 | 0.8178 | 0.2649 | 3.4237 | |||
SE, size of effect; LLCI, lower limit of confidence interval; ULCI, upper limit
of confidence interval; QoL, quality of life; Boot, resampling simulation. The number of sample
simulations for bias correction of confidence intervals: Level of confidence for
all confidence intervals: 95.
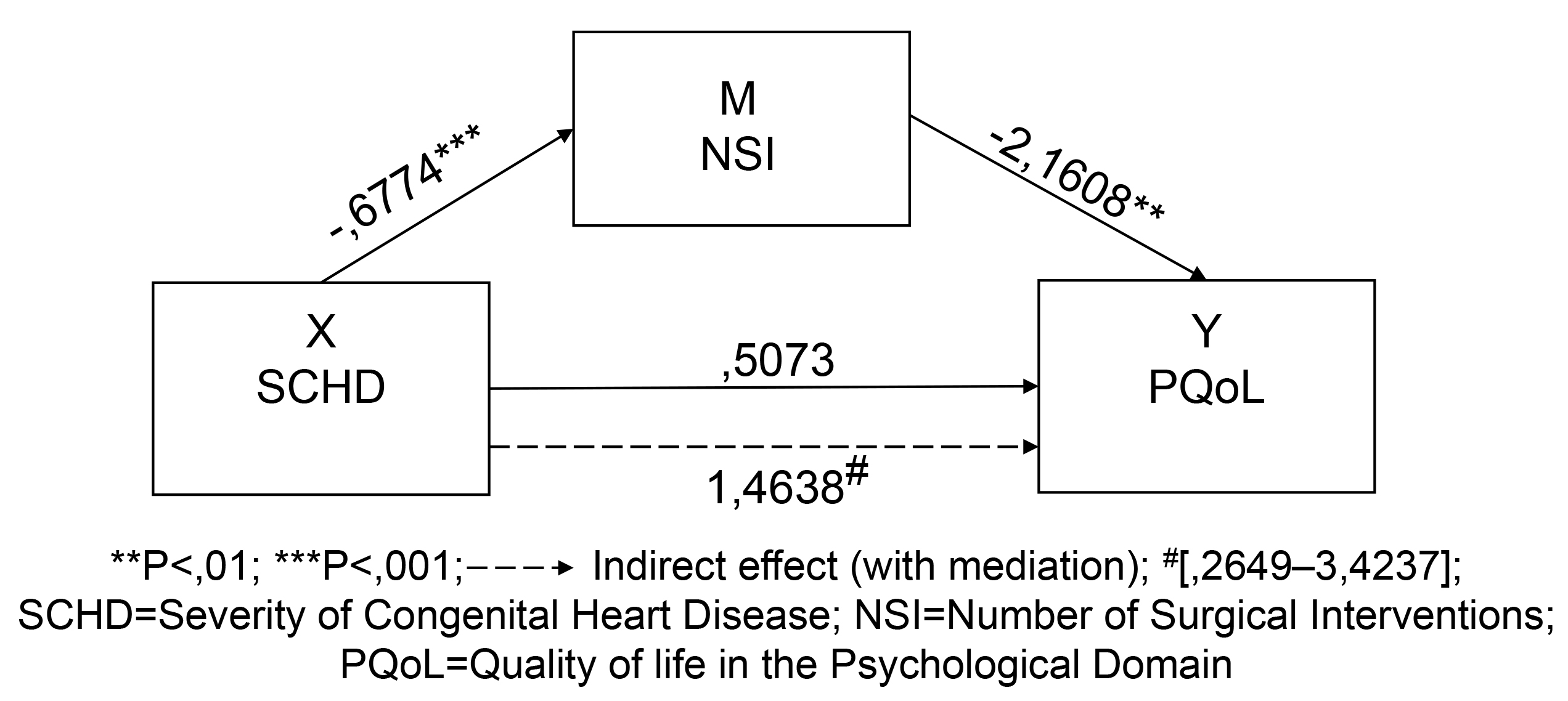 Fig. 4.
Fig. 4.Model 6: Unstandardized path coefficients for mediation.
The direct effect between the variables X: SCHD and Y: PQoL shows a positive
association (B = –0.5073, SE = 1.5650, t = –0.3241, p
This study aimed to investigate the impact of selected clinical variables (namely, the number of surgeries) as mediators of the relationship between CHD (including severity and presence/absence of cyanosis) and patients’ perception of QoL. The available body of research on the perception of QoL in CHD patients is already extensive. Previous studies have highlighted that the increased survival of the CHD population due to advances in pediatric cardiac care has led to a rise in lifelong medical, psychosocial, and behavioural challenges, raising concerns about these patients’ well-being and perceived QoL.
However, new evidence is still needed, particularly regarding the mediation effects of contextual variables. More comprehensive and realistic explanatory models could benefit researchers, clinicians, and CHD patients. The prevalence of CHD is estimated at 0.3% in the global population of approximately 4.4 billion adults, which translates to approximately 13 million adult CHD survivors worldwide [37, 38]. Based on these figures, we can expect approximately 25,000 adults with CHD in Portugal. To the best of our knowledge, this is the first study to examine the importance of certain clinical variables as mediators of the impact of illness on QoL in CHD patients.
We tested 10 models to assess the predictive mediating effect of NSI on QoL in multiple domains (physical, psychological, social relationships, environmental, and general) in CHD patients while also considering the TCHD and SCHD criteria separately. Before proposing these models, we thoroughly reviewed the existing research on QoL and the impact of surgical interventions on these patients [4, 25, 39, 40, 41, 42]. Following a strategic plan, we also performed several statistical tests beforehand to identify potential models for further investigation. We then used the methodology of multiple bootstrap simulations proposed by Hayes [36] to more thoroughly examine these models.
As a primary finding from this analysis, we were able to confirm that the presence of cyanosis and the severity of CHD relate to the number of surgical interventions performed in patients. Secondly, we also confirmed that NSI negatively relates to patients’ quality of life in psychological and social relationship’s dimensions. Both facts could be expected and have been described previously in the literature. But the most relevant finding of this study is that the detrimental effect of cyanosis and severity of illness in QoL, in psychological and social relationship’s dimension, is fully explained by the mediating effect of the number of surgical interventions performed in the patients, in a pure mediation effect.
Our results from the tests of the mediation models suggest that patients, particularly those with more severe and cyanotic CHD, who undergo a greater number of surgical interventions, have an increased risk of perceiving negative QoL in the Psychological and Social Relationships domains. Interestingly, we did not find evidence of a mediation effect in other domains of QoL, such as Physical, Environmental, and Global. It appears that patients are more aware of the psychological and social consequences of the disease when evaluating their QoL, perhaps because they associate these consequences with a loss of freedom or control, which can indicate resilience, mental health, or some form of stress or exhaustion.
These findings provide a comprehensive foundation for planning and organizing effective interventions by healthcare professionals, including psychologists, for CHD patients. One of the strengths of this study is the substantial sample size of CHD patients, which is comparatively large compared to other studies in this area. Another positive aspect is the diverse range of variables analyzed and the extensive evaluation of sociodemographic factors, including age and the diversity of CHD diagnoses. Additionally, this study is advantageous because it allows for analyses of the relationship between patients’ perceptions of QoL and clinical and procedural variables.
A poorer perception of QoL has been reported by patients submitted to a greater number of surgeries in the Psychological and Social Relationships Domains [25, 39, 40]. The results of this study suggest that NSI can be considered a mediator variable, which explains the mechanism by which the two independent predictors under focus (and SCHD) influence the dependent variables (perceptions of QoL in various domains). Mediators explain how external physical events assume inner psychological significance [43]. In this study, NSI serves as a mediating variable, explaining how TCHD and SCHD impact certain domains of QoL, specifically the Psychological and Social Relationships domains.
NSI may explain how CHD impacts the Psychological domain of QoL through the feeling of threat to life and fragility associated with surgeries and the restrictions of freedom and autonomy [25, 39, 40]. NSI can also explain how CHD impacts social relationships since the recurrent hospitalizations and the associated circumstances can lead to restrictions on access to the family environment to full social support [25, 39, 41], factors that are strong predictors of QoL.
Our study has some limitations. On the one hand, the diversity of the analyzed variables may pose challenges in grouping all the results together. However, other variables could be introduced, such as the effect of the number of surgeries on body aesthetics, the ease or difficulty in physical exercise (sport), the social parameters regarding the difficulties that the severity of the disease may pose in obtaining a driving license, requirements for obtaining bank credits or health insurance, or difficulty in obtaining or maintaining employment due to potential absence from work as a result of new surgeries or treatments. Another variable that would be interesting to consider in the future is the age of patients at the last surgery, as it is reasonable to expect that the most recent memory of surgical interventions could influence the personal perception of QoL.
Given these findings and the need to plan and organize effective interventions by healthcare professionals, including psychologists, for CHD patients, it would be helpful to consider and include variables that may have a “dampening” effect on the impact of CHD on patients’ perception of QoL. This could include providing patients better access to family support, psychosocial support, integration, and academic performance. Raising awareness among healthcare professionals, education professionals, families, and the community could help ensure the inclusion of these variables and a greater capacity to involve family members and key members of the social network of patients in healthcare services.
Childhood CHD is a complex and multifaceted condition that poses a significant challenge for patients, their families, and healthcare professionals. Here, we explored the impact of CHD on patients’ QoL and investigated the mediating variables that may influence this relationship. We found that patients with more severe and cyanotic diseases typically have more surgical interventions, which increases the risk of negative outcomes and harms patients’ perception of QoL. These findings will help health professionals and psychologists treating childhood CHD patients.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
MEGA and JCA designed the research study. MEGA supervised the collection of data and data analysis, contributed to the writing and revised all the manuscript. FM, FN, PB, AB, SES, SS performed the study, collecting data, and contributed in data analysis. FM contributed to the writing of the manuscript in general, and FN, PB, AB, SES, SS contributed for the writing of the Methods section. MP collected the medical data and JOM supervised the collection of medical data. VV and BP provided help and counseling in data analysis. All authors read and approved the final manuscript, and contributed to edition changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This study was approved by the Ethics Committee of Centro Hospitalar e Universitário de S. João (also known as Hospital S. João) in Porto, Portugal, with the Project identification number 08.09. All subjects gave their informed consent for inclusion before they participated in the study.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
