- Academic Editors
-
-
-
Background: Atrial fibrillation (AF) is accompanied by inflammation and
fibrosis to variable extent. The biomarkers of fibrosis were measured in patients
with different forms of AF and cardiac status. Herein, we assessed the
associations of the baseline concentrations of different biomarkers with the
long-term success of pulmonary vein isolation (PVI) in patients with a
structurally normal heart. Furthermore, we compared biomarker levels before and 3
years after ablation to gain further insights into the AF mechanism.
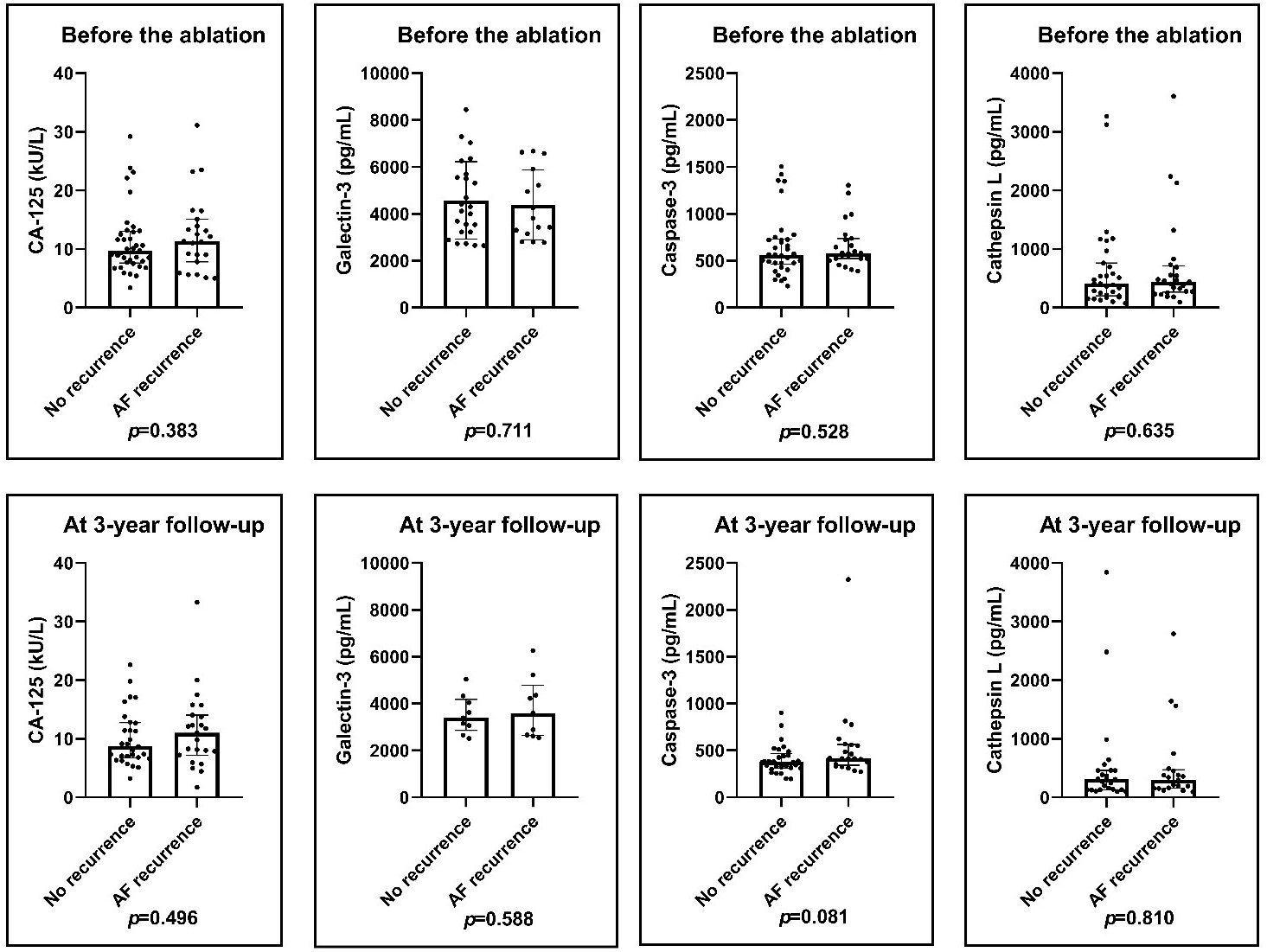
Methods: Patients, undergoing PVI for paroxysmal/persistent AF were
enrolled prospectively. Blood samples were obtained 24 hours before and 3 years
after ablation. Serum cancer antigen 125 (CA-125), plasma Caspase-3, Galectin-3
and Cathepsin L concentrations were measured. Follow-up visits every 6 months
included 12-lead electrocardiogram, 24-hour Holter, trans-telephonic monitoring
as well as transthoracic echocardiography after ablation. Biomarker levels, left
ventricular ejection fraction and left atrial (LA) diameters at baseline and at
the 3-year follow-up were compared in patients with versus without AF recurrence.
Results: A total of 63 patients were enrolled (23 women; age 61.4
(