1 Faculty of Medical Sciences in Katowice, Medical University of Silesia, 40-752 Katowice, Poland
2 Liverpool Centre for Cardiovascular Science at University of Liverpool, Liverpool John Moores University and Liverpool Heart & Chest Hospital, L14 3PE Liverpool, UK
3 Department of Clinical Medicine, Aalborg University, 9220 Aalborg, Denmark
Abstract
Dietary habits, including alcohol consumption, are among the significant risk factors for the occurrence of atrial fibrillation (AF). The pathophysiological relationship between alcohol consumption and AF is complex and multifactorial. However, there is conflicting information about the impact of alcohol consumption (in various doses and types) on the risk of AF and AF-related outcomes. Alcohol consumption is significantly associated with AF in a gender-independent manner. The widespread belief that moderate amounts of alcohol, especially red wine, have cardioprotective effects may mean that more people will use alcohol. Even small amounts of alcohol regularly consumed increase the risk of AF. In this narrative review, we will review the epidemiological associations between alcohol and AF, and the implications for incident AF and AF-related outcomes.
Keywords
- atrial fibrillation
- alcohol consumption
- cardiovascular risk
Atrial fibrillation (AF) is the most common cardiac arrhythmia in humans [1]. The 2019 global burden of AF is estimated at 59.7 million (95% confidence interval: 45.7 to 75.3 million), double the number of estimated cases in 1990 [2]. It is estimated that in 2050 the incidence of AF may increase by more than 60% [3]. Experts indicate that in 2050 the prevalence of AF in the USA and Europe will amount to 16 and 16–17 million cases, respectively [4]. The high prevalence of AF is a significant economic problem, associated primarily with frequent hospitalizations, absenteeism or complications of the disease, including stroke [5].
From a clinical point of view, an important issue is the effect of diet and lifestyle on the risk of AF [6]. Dietary habits, including alcohol consumption, are among the significant risk factors for the occurrence of AF. Manthey et al. [7] showed that the consumption of alcohol in the world is constantly increasing: 1990—5.9 L/capita; 2017—6.5 L/capita; 2030—7.6 L/person (in terms of pure ethanol). Alcohol use is a leading risk factor for global disease burden and causes substantial health loss [8]. According to World Health Organisation (WHO) worldwide, 3 million premature deaths every year result from harmful use of alcohol. This represents 5.3% of all deaths [9]. However, there is conflicting information about the impact of alcohol consumption (in various doses and types) on the risk of AF and AF-related outcomes.
In this narrative review, we will review the epidemiological associations between alcohol and AF, and the implications for incident AF and AF-related outcomes.
In scientific nomenclature, the basic way of determining the amount of alcohol consumed is the standard alcohol unit (SAU; drink), which is the amount of alcoholic beverage (of any kind) that contains 12.5 mL or 10 g of pure ethanol. For example: a small beer (330 mL; 4.5%) is 1.19 SAU; a large beer (500 mL; 4.5%) is 1.8 SAU; a glass of wine (175 mL; 12%) is 1.68 SAU; a shot of vodka (50 mL; 40%) is 1.6 SAU. There are other definitions of SAU. For example, in the UK it is the amount of an alcoholic drink that contains 10 mL or 8 g of pure ethanol. Another definition indicate that a unit of alcohol is 12 g of pure ethanol [10, 11].
In general, alcohol consumption has been defined as: light (
The association between excessive drinking and various forms of cardiovascular disease is well established [14]. The influence of the amount of alcohol consumed on the risk of most cardiovascular diseases takes the shape of a “J” curve [14]. Considering the constantly increasing prevalence of AF, it is clinically important how the relationship between the amount of alcohol consumed and the risk of this arrhythmia develops.
Alcohol may act proarrhythmogenic in many mechanisms. At the cellular level, alcohol can damage intercellular junctions and cells, trigger inflammation and oxidative stress, and disrupt the regulation of ion channels in the myocardium [14, 15]. Within the autonomic nervous system, alcohol increases the activity of the sympathetic component and reduces heart rate variability (HRV) [14, 15].
Moreover, alcohol promotes dilatation and fibrosis of the left atrium and increases its pressure [16, 17]. Long-term alcohol consumption promotes atrial cardiomyopathy (alcoholic cardiomyopathy) associated with structural, functional and electrical remodeling of the atria, thus stabilizing AF episodes and contributing to AF progression [16, 17]. In addition, alcohol consumption often leads to other risk factors for AF, such as being overweight, obstructive sleep apnea, and arterial hypertension [16]. Myocardial hypertrophy resulting from chronic alcohol consumption by increasing the reactivity of transient receptor potential cation channels (TRPC) leads to electrical instability of cardiomyocytes, which directly contributes to the occurrence of arrhythmias [18, 19].
Alcohol directly causes a number of disorders in the electrophysiology of the
heart. This effect is related to the dysregulation of ion channels. One
in silico study found that alcohol reduced I
Heavy alcohol consumption can result in the holiday heart syndrome, which was first described in 1978 and occurs when healthy subjects without heart disease known to cause arrhythmia experience AF after excessive alcohol consumption, which was observed mainly after weekends or holidays [21]. This can probably be attributed to such effects of alcohol as: inhibition of sodium channels in myocardial cells, stimulation of the sympathetic and parasympathetic nervous system, increase in the concentration of free fatty acids in the blood and stimulation of c-Jun N-terminal kinase 2 (JNK2) kinase [secondarily leads to the stimulation of calmodulin II kinase (CaMKII) and the release of calcium ions from the SR, which ultimately contributes to the development of AF], and above all - electrolyte changes, including hypokalemia and hypomagnesemia, after taking large doses of alcohol in a short time [21, 22, 23].
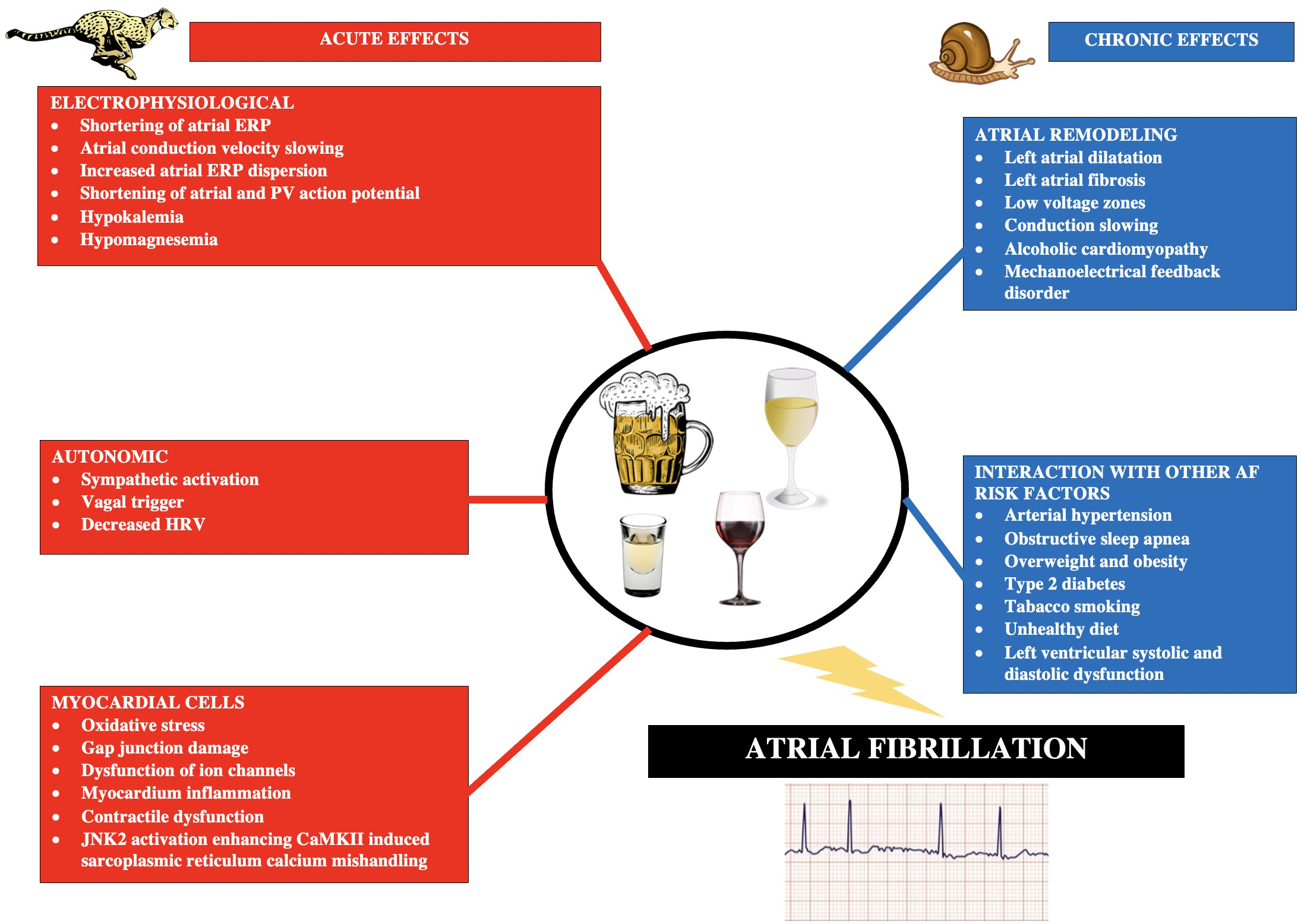
In a study by Voskoboinik et al. [24] including 75 patients undergoing AF ablation using high density electroanatomical mapping, moderate alcohol consumption (8–21 drinks/week) was found to be associated with lower bipolar voltage and slower atrial conduction velocity. In a randomized and placebo-controlled study by Marcus et al. [25], covering 100 subjects, acute exposure to alcohol reduces atrial effective refractory periods (AERP), particularly in the pulmonary veins, which is substrate for AF. In a study by Sha et al. [26], including 134 patients with AF, alcohol causes echocardiographic and electrophysiological changes such as impaired peak left atrial longitudinal strain, obvious inter-atrial conduction delay and increasing ERP dispersion. Intra-atrial conduction delay and ERP dispersion also increased with increasing levels of alcohol consumption [26]. The most important mechanisms of the influence of alcohol consumption on the pathogenesis of AF are summarized in Fig. 1 (Ref. [14, 15, 27, 28]).
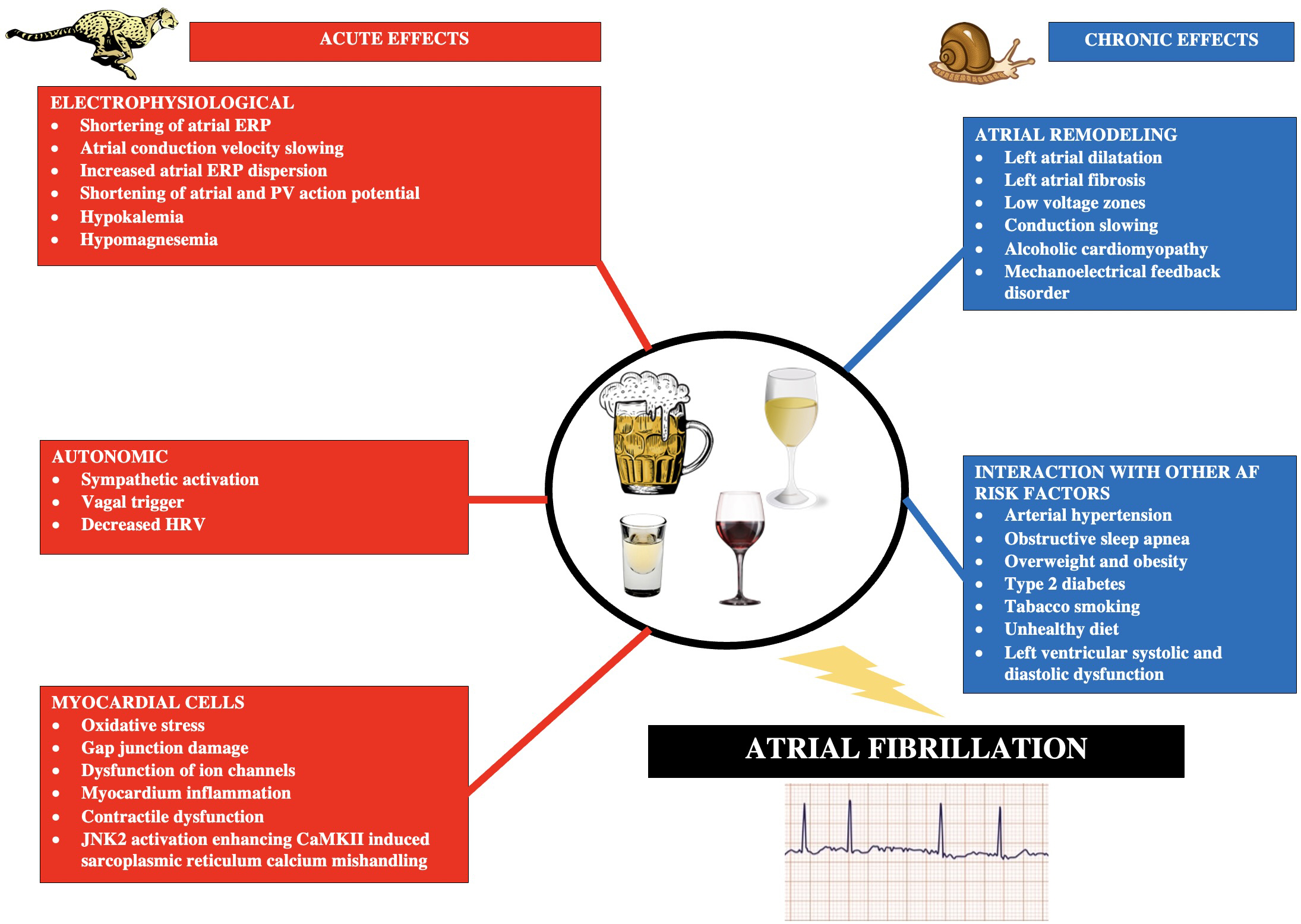 Fig. 1.
Fig. 1.Main acute and chronic pathophysiological mechanisms triggered by alcohol consumption and leading to the development of atrial fibrillation. Based on [14, 15, 27, 28]. Abbreviations: AF, atrial fibrillation; ERP, effective refractory period; PV, pulmonary vein; HRV, heart rate variability; JNK2, c-Jun N-terminal kinase 2; CaMKII, calmodulin II kinase.
The safer effect of drinking wine, observed in some studies [17], in contrast to other alcohols, may be due to the richness of polyphenols contained in this red and white beverage. Of particular interest is resveratrol, a polyphenol found in large amounts in red wine [29]. Resveratrol has been shown to reduce the inducibility of AF, potentially by reducing left atrial fibrosis and regulating ion channel function [30]. The overall effect of polyphenols on reducing the risk of AF is associated with, among others, anti-inflammatory, antioxidant and anti-fibrotic effects, as is the case with the consumption of polyphenol-rich coffee [31].
In summary, alcohol consumption triggers both acute and chronic mechanisms that lead to the onset of AF. Regular consumption of even ESC-acceptable alcohol doses (100 g/week) leads to electrical and structural remodeling of the atria and increases the risk of AF. The polyphenols contained in wine can to some extent mitigate the negative effects of alcohol itself.
The most important results relating alcohol consumption and AF are summarized in Table 1 (Ref. [17, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48]).
| Author, year, [Ref] | Meta-analysis/study characteristics | The amount of alcohol consumed and the risk of AF | Notes/Comment | What pattern of alcohol consumption increases the risk of AF? | |
|---|---|---|---|---|---|
| Compatibility with the ESC 2021 guidelines | |||||
| Samokhvalov A. et al., 2010, [32] | 6 studies/67,891 subjects | 12 g/day | F and M: RR = 1.08; 95% CI: 1.02–1.14 | Gender - did not affect the risk of AF Dose - The greater the alcohol consumption, the greater the risk of AF ESC 2021: no | |
| 24 g/day | F: RR = 1.07; 95% CI: 1.04–1.10 | ||||
| M: RR = 1.08; 95% CI: 1.04–1.11 | |||||
| 60 g/day | F: RR = 1.42; 95% CI: 1.23–1.64 | ||||
| M: RR = 1.44; 95% CI: 1.23–1.69 | |||||
| 120 g/day | F: RR = 2.02; 95% CI: 1.60–2.97 | ||||
| M: RR = 2.09; 95% CI: 1.52–2.86 | |||||
| Kodama S. et al., 2011, [33] | 14 studies/138,378 subjects | High versus low | RR = 1.51; 95% CI: 1.31–1.74 | Gender, comorbidities and reference group (low or no intake) did not influence the risk of AF ESC 2021: yes | |
| Gallagher C. et al., 2017, [34] | 9 studies/249,496 subjects | Low (1 drink/day) | HR = 0.95; 95% CI: 0.85–1.06 | Moderate alcohol consumption significantly increased the risk of AF only in men ESC 2021: yes | |
| Moderate | HR = 1.11; 95% CI: 1.05–1.18 | ||||
| High versus low/no consumption | HR = 1.34; 95% CI: 1.20–1.49 | ||||
| Larsson S. et al., 2014, [35] | 7 prospective studies/205,073 subjects | Increase alcohol intake by an additional drink (12 g pure alcohol)/day | RR = 1.08; 95% CI: 1.06–1.10 | The risk was not affected by: gender, geographical origin | |
| ESC 2021: no | |||||
| Yang L. et al., 2022, [36] | 13 studies/10,266,315 subjects | Small (about 1 drink/day) | HR = 1.05; 95% CI: 0.98–1.13 | Small F and M - no effect Moderate F - no effect M - (HR = 1.09; 95% CI: 1.07–1.11) Region: Europe Small - HR = 1.09; 95% CI: 1.02–1.17 Moderate - HR = 1.26; 95% CI: 1.09–1.44 Types of alcohol (spirits, beer, wine) Small - no impact Moderate - no impact ESC 2021: yes | |
| Moderate (about 2 drinks/day) | HR = 1.14; 95% CI: 1.07–1.21 | ||||
| Zhang H. et al., 2022, [37] | 13 prospective studies/668,905 subjects | Small ( |
F: HR = 0.97; 95% CI: 0.90–1.04 | Gender had some effect on the risk of AF associated with alcohol consumption ESC 2021: yes | |
| M: HR = 1.04; 95% CI: 0.97–1.11 | |||||
| Moderate (12–24 g/day) | F: HR = 1.02; 95% CI: 0.91–1.14 | ||||
| M: HR = 1.21; 95% CI: 1.10–1.33 | |||||
| High ( |
F: HR = 1.32; 95% CI: 1.10–1.60 | ||||
| M: HR = 1.54; 95% CI: 1.26–1.89 | |||||
| Giannopoulos G. et al., 2022, [38] | 16 studies/13,044,007 subjects | Moderate ( |
logOR = –0.20; 95% CI: –0.28 to –0.12 | The dependence taking the shape of the “J” curve was found ESC 2021: yes | |
| High ( |
logOR = 0.14; 95% CI: 0.01–0.2 | ||||
| Jiang H. et al., 2022, [39] | 13 prospective studies/10,151,366 subjects | Each increase in alcohol consumption by one drink | F: RR = 1.05; 95% CI: 0.96–1.14 | Women: J-curve association Men: linear association ESC 2021: no | |
| M: RR = 1.08; 95% CI: 1.05–1.11 | |||||
| Ariansen I. et al., 2012, [40] | 9193 patients with LVH and AH | HR = 1.60; 95% CI: 1.02–2.51 | Multivariate analysis ESC 2021: yes | ||
| Statistically insignificant risk | |||||
| Larsson S. et al., 2014, [35] | Prospective/79,019 subjects | 1–6 drinks/week | RR = 1.01; 95% CI: 0.94–1.09 | Comparison: |
|
| 7–14 drinks/week | RR = 1.07; 95% CI: 0.98–1.17 | ||||
| 15–21 drinks/week | RR = 1.14; 95% CI: 1.01–1.28 | ||||
| RR = 1.39; 95% CI: 1.22–1.58 | |||||
| Cha M. et al., 2020, [41] | Prospective/19,634 subjects | Drinking versus not drinking | HR = 2.21; 95% CI: 1.55–3.14 | Men more predisposed to alcohol-related AF ESC 2021: no | |
| Higher versus lower consumption | HR = 3.15; 95% CI: 1.98–4.99 | ||||
| Csengeri D. et al., 2021, [42] | Prospective/107,845 subjects | 1 g/day (0.08 drink) | HR = 1.01; 95% CI: 0.99–1.04 | No significant differences between vodka and beer. The risk of AF associated with wine consumption was the least expressed or insignificant ESC 2021: no | |
| 2 g/day (0.17 drink) | HR = 1.02; 95% CI: 1.0–1.04 | ||||
| 3 g/day (0.25 drink) | HR = 1.04; 95% CI: 1.02–1.05 | ||||
| 4 g/day (0.33 drink) | HR = 1.05; 95% CI: 1.03–1.07 | ||||
| 5 g/day (0.42 drink) | HR = 1.06; 95% CI: 1.04–1.08 | ||||
| 6 g/day (0.5 drink) | HR = 1.07; 95% CI: 1.05–1.1 | ||||
| 12 g/day (1 drink) | HR = 1.16; 95% CI: 1.11–1.22 | ||||
| 24 g/day (2 drinks) | HR = 1.36; 95% CI: 1.25–1.47 | ||||
| 36 g/day (3 drinks) | HR = 1.52; 95% CI: 1.35–1.7 | ||||
| 48 g/day (4 drinks) | HR = 1.59; 95% CI: 1.37–1.85 | ||||
| 60 g/day ( |
HR = 1.61; 95% CI: 1.35–1.92 | ||||
| Tu S. et al., 2021, [17] | Prospective/403,281 subjects | Increasing doses of alcohol | J-shaped relationship in total alcohol consumption, with the lowest risk of AF at less than 7 drinks/week | The strength of the study: comparable numbers of women and men. | |
| Beer and cider - any consumption is harmful | |||||
| Red and white wine and spirits: up to 10, 8 and 3 drinks/week, respectively, not associated with an increased risk of AF | |||||
| Gender - no significant differences were found | |||||
| ESC 2021: no | |||||
| Han M. et al., 2022, [43] | Prospective/1,537,836 subjects | 105–210 g/week | HR = 1.25; 95% CI: 1.12–1.40 | Multivariate analysis - no effect on AF risk ESC 2021: yes | |
| HR = 1.47; 95% CI: 1.18–1.83 | |||||
| Marcus G. et al., 2022, [44] | RCT, n-of-1 trial/446 patients | Acute exposure to alcohol | OR = 2.15; 95% CI: 1.17–3.61 | ESC 2021: no | Acute exposure to alcohol |
| Marcus G. et al., 2021, [45] | 100 subjects/Real-time detection of AF | 1 drink | After 4 hours: OR = 2.02; 95% CI: 1.38–3.17 | Individual AF episodes were associated with higher odds of recent alcohol consumption ESC 2021: no | |
| 2 drinks | After 4 hours: OR = 3.58; 95% CI: 1.63–7.89 | ||||
| Aung S. et al., 2022, [46] | 36,158 subjects | Occasional increase in alcohol consumption (weekend, holiday, etc.) | Statistically significant increase in ED visits for AF and for new-onset AF (1757 additional visits for new-onset, incident AF ED visits/100,000 person-years; 95% CI: 945–2.569 visits, p |
Population-based study | |
| ESC 2021: no | |||||
| Frederiksen T.C. et al., 2022, [47] | 43,758 subjects/Five-year changes in alcohol intake | Females: |
Multivariate analysis There were no differences in the effect of different types of alcohol on the risk of AF ESC 2021: yes | ||
| 7–13.9 drinks/week | |||||
| 14–20.9 drinks/week | |||||
| Biddinger K.J., 2022, [48] | 371,463 subjects from UK Biobank | Consumption versus non-consumption (Mendelian randomization) | OR = 1.24; 95% CI: 1.08–1.44 | Causality assessment Analysis with the exclusion of abstainers ESC 2021: no | |
| Non-consumption and 7, 14, 21 and 28 drinks/week | The relationship between alcohol and the risk of AF was dose-dependent. Already from the smallest dose of alcohol (1 drink/week) the risk of AF began to increase statistically significantly | ||||
Abbreviations: AF, atrial fibrillation; ESC, European Society of Cardiology; F, female; M, male; RR, relative risk; 95% CI, 95% confident interval; HR, hazard ratio; OR, odds ratio; LVH, left ventricular hypertrophy; AH, arterial hypertension; RCT, randomized controlled trial; ED, emergency department.
In a meta-analysis of 6 studies the risk of AF was significantly increased from the consumption of 12 g or more of alcohol/day. A linear dose-response relationship has been demonstrated between alcohol consumption and the risk of AF [32]. A meta-analysis of 14 studies found that higher (versus lower) alcohol consumption was associated with a significant increase in the risk of AF (RR = 1.51; 95% CI: 1.31–1.74). A linear dose-response relationship has been demonstrated between alcohol consumption and the risk of AF [33]. A meta-analysis of 9 studies (249,496 subjects) found that heavy to moderate alcohol consumption was significantly associated with an increased risk of AF (by 34% and 11%, respectively). Low alcohol consumption was not associated with the risk of AF [34]. In a meta-analysis of 7 prospective studies (205,073 participants), it was found that each one drink/day increase in alcohol consumption was significantly associated with an 8% increase in the risk of AF (RR = 1.08; 95% CI: 1.06–1.10) [35]. One meta-analysis of 13 studies (10,266,315 subjects) found that regular moderate (about 2 units of alcohol/day) alcohol consumption increased the risk of AF (HR = 1.14; 95% CI: 1.07–1.21), while low alcohol consumption (about 1 unit of alcohol/day) had no effect on this risk [36]. Another meta-analysis of 13 studies (668,905 subjects) found that heavy alcohol consumption increased the risk of AF by 30% (HR = 1.30; 95% CI: 1.20–1.41), moderate by 12% (HR = 1.12; 95% CI: 1.06–1.18), while low did not affect the risk (HR = 1.00; 95% CI: 0.96–1.05) [37].
Nonetheless, a meta-analysis of 16 studies (13,044,007 subjects) showed a
slightly different relationship between alcohol consumption and the risk of AF. A
relationship in the form of a “J” curve was found, as high alcohol consumption
(
In the losartan intervention for endpoint Reduction in Hypertension (LIFE) randomized clinical trial, including 9193 patients with electrocardiography (ECG) signs of
left ventricular hypertrophy and arterial hypertension, the consumption of
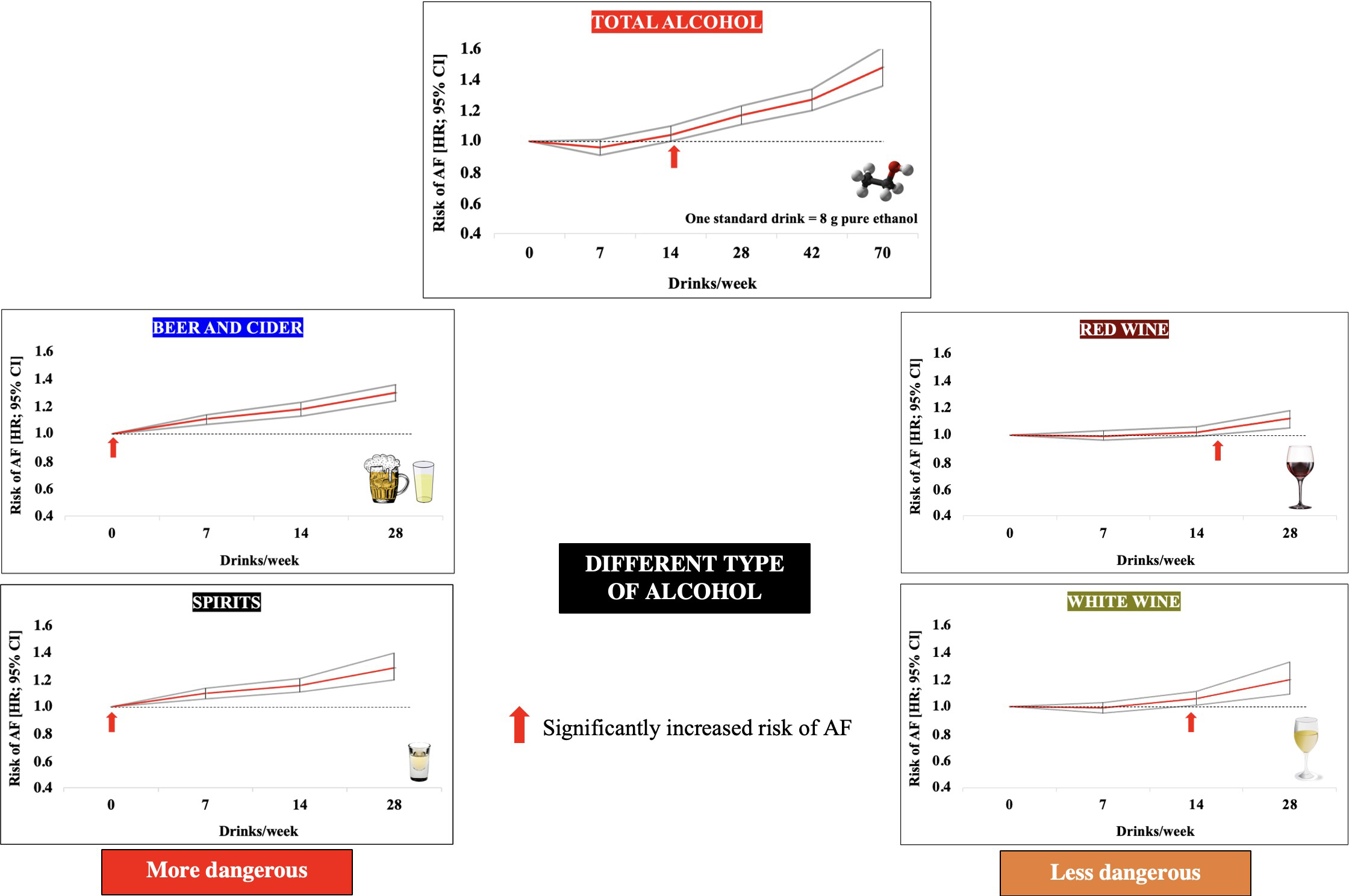
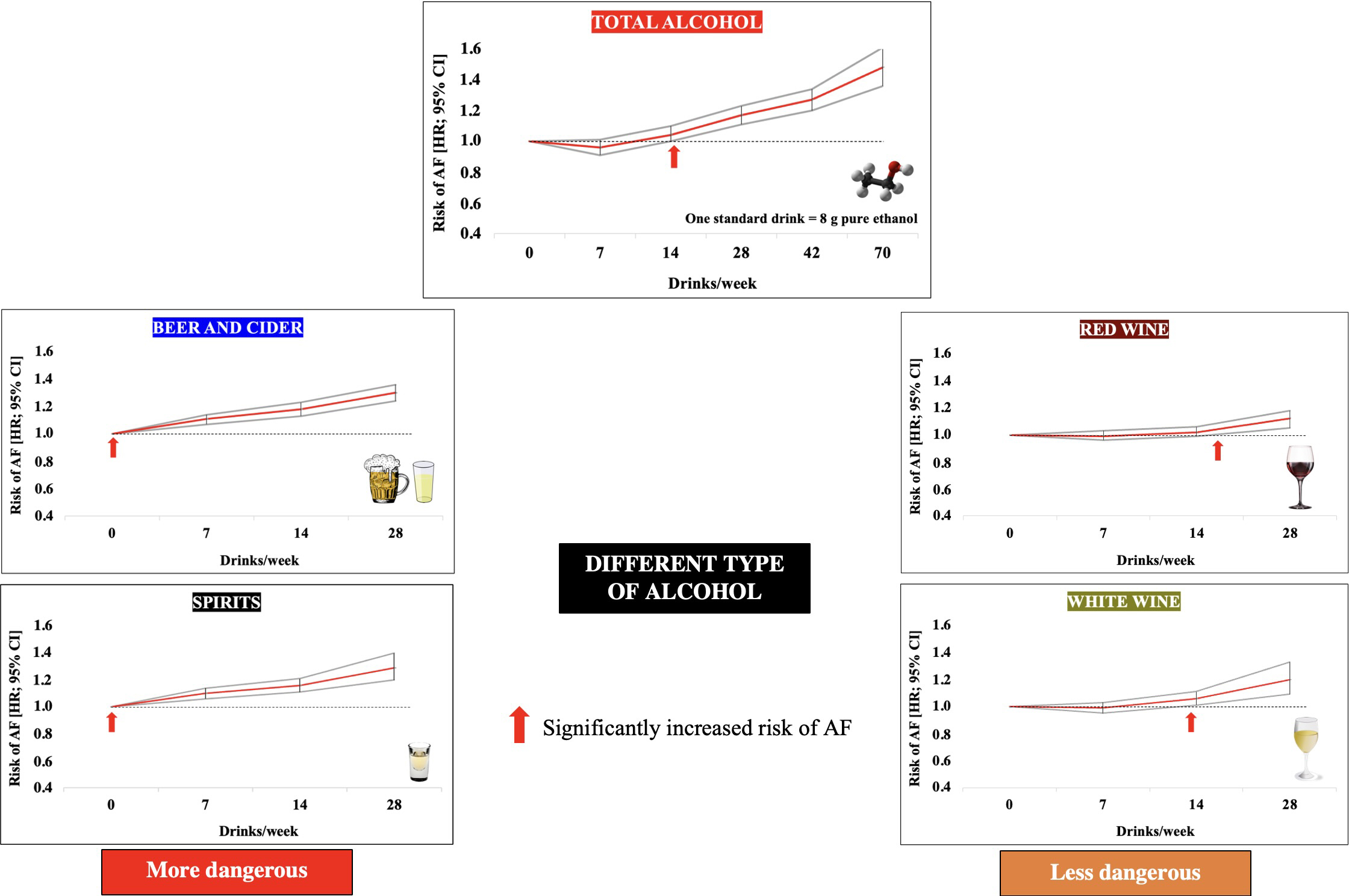 Fig. 2.
Fig. 2.Effect of alcohol consumption and different types of alcoholic beverages on the risk of developing atrial fibrillation. Data adapted from [17]. Abbreviations: AF, atrial fibrillation; HR, hazard ratio.
In an observational study by Frederiksen et al. [47] of 43,758
participants without AF at baseline, increasing alcohol consumption over a 5-year
follow-up was associated with a higher risk of AF [from
In the I-STOP-AFib randomized clinical trial of 466 patients, acute exposure to alcohol increased AF risk (OR = 2.15; 95% CI: 1.17–3.61), with no evidence that other exposures, including caffeine, triggered AF [44]. In another study by Marcus et al. [45], including 100 subjects, 56 of whom had at least 1 episode of AF, within 4 hours of consuming one drink, the risk of AF (real-time documentation of each alcoholic drink consumed was self-recorded using a button on the ECG recording device) was doubled (OR = 2.02; 95% CI: 1.38–3.17), with a greater than 3-fold higher odds of at least 2 drinks (OR = 3.58; 95% CI: 1.63–7.89).
In a study covering 36,158 individuals, occasional (holiday, etc.) increases in
alcohol consumption were associated with a statistically significant increase in
ED visits for AF and for new-onset AF, with 1757 additional visits for new-onset,
incident AF ED visits/100,000 person-years (95% CI: 945–2569 visits,
p
In summary, most studies provide evidence of a strong association between alcohol consumption and the risk of AF. It cannot be arbitrarily concluded that light or moderate alcohol consumption (up to 100 g/week) does not affect the risk of AF, as even small amounts of alcohol regularly consumed increase the risk of AF.
A prospective study by Larsson et al. [35] found that for liquor, the
risk of AF was increased when drinking 7–14 and
In summary, the risk of AF depends on the type of alcohol consumed (highest: beer, cider and spirits; lowest: white and red wine).
Women consume significantly less alcohol compared to men. In a meta-analysis by Kodama et al. [33], heavy alcohol consumption increased the risk of AF in both women and men (37% and 32%, respectively). A similar finding was made in the meta-analysis by Samokhvalov et al. [32] showing an increased risk of AF in both women and men with 12 g of alcohol/day and more). In a prospective study by Tu et al. [17] involving an equal number of women and men (52.4% versus 47.6%), no significant sex differences in the risk of AF associated with alcohol consumption were found.
A meta-analysis by Gallagher et al. [34] found that moderate alcohol consumption significantly increased the risk of AF in men (HR = 1.26; 95% CI: 1.04–1.54) but not in women (HR = 1.03; 95% CI: 0.85–1.24). In a study by Cha et al. [41], men were also more predisposed to a higher risk of AF related to alcohol consumption compared to women. A greater susceptibility of men to develop AF in relation to alcohol was also found in the meta-analysis by Yang et al. [36] who found that although low alcohol consumption did not affect the risk of AF, moderate alcohol consumption increased it among men (HR = 1.09; 95% CI: 1.07–1.11) but not among women. A meta-analysis by Zhang et al. [37] found that moderate and heavy alcohol consumption was significantly associated with the risk of AF among men (HR = 1.21; 95% CI: 1.10–1.33 and HR = 1, respectively, 54; 95% CI: 1.26–1.89), while among women this was only evident with high alcohol consumption (HR = 1.32; 95% CI: 1.10–1.60). In a meta-analysis by Jiang et al. [39], the relationship between alcohol consumption and the risk of AF is linear among men, while among women it takes the shape of a “J” curve. In an observational study by Frederiksen et al. [47] of 43,758 participants without AF at baseline was found that increasing alcohol consumption in a 5-year follow-up significantly increased the risk of AF only among women.
Some [29, 31, 32, 34, 36], but not all [15, 27, 28, 47], studies have found a higher risk of AF in men who consume alcohol. Several studies have failed to show an increase in the risk of AF at all levels of alcohol consumption in women. Most of these earlier studies included only a few women who consumed large amounts of alcohol.
In summary, sex does not seem to have a significant effect on the risk of AF associated with alcohol consumption.
An important issue is whether certain gene polymorphisms of enzymes involved in alcohol metabolism (alcohol dehydrogenase—ADH; aldehyde dehydrogenase—ALDH) [50] may affect the risk of AF associated with alcohol consumption.
In a study by Tolstrup et al. [51], covering 88,782 subjects,
ADH1B/ADH1C genetic variants were not found to affect the risk of AF associated
with alcohol consumption. In a Mendelian randomized study (approximating the
possibility of causal inference) by Yang et al. [52] including 8964
subjects, the rs671 polymorphism of the ALDH2 gene (decreased activity
resulting in greater accumulation of the highly toxic acetaldehyde) showed a
significant association with the risk of AF in men (OR = 1.65; 95% CI:
1.06–2.67). In Mendelian randomization, genetically predicted daily alcohol
consumption was positively associated with the risk of AF in both sexes (OR =
3.17; 95% CI: 1.18–9.24) [52]. In a study by Yamashita et al. [53],
including 656 subjects, the ALDH2
In a study by Biddinger et al. [48] of 371,463 participants from UK Biobank, which used Mendelian randomization (promoting the possibility of causal inference), alcohol consumption was significantly associated with the risk of AF (OR = 1.24; 95% CI: 1.08–1.44).
In summary, genetic polymorphisms of the genes of enzymes involved in ethanol metabolism may modulate the risk of AF associated with alcohol consumption.
In the Atherosclerosis Risk in Communities (ARIC) Study 15,222 subjects followed for 19.7 years, current and former drinkers were found to be at higher risk of AF than those who never drank alcohol, and every decade abstinent from alcohol was associated with an approximate 20% (95% CI: 11–28%) lower rate of incident AF [54]. Conversely, every additional decade of past alcohol drinking was associated with a 13% (95% CI: 3–25%) higher rate of AF and every additional drink/day during former drinking was associated with a 4% (95% CI: 0–8%) higher rate of AF [54]. The results of this study indicate that the lowest risk of AF was among subjects who had never consumed alcohol. In a study by Choi et al. [55], covering 1,112,682 patients with type 2 diabetes who were followed for 4 years, alcohol abstinence was associated with a low risk of AF development (HR = 0.81; 95% CI: 0.68–0.97).
In summary, reducing alcohol consumption is associated with a significant decrease risk of incident AF.
In a meta-analysis of 9 studies (5436 patients) conducted by Grindal et al. [56], including patients after catheter ablation due to AF, the impact of alcohol consumption on the risk of recurrence of arrhythmia showed that compared with patients who consumed little or no alcohol, those who consumed moderate or high amounts of alcohol had a higher probability of recurring AF (OR = 1.45; 95% CI: 1.06–1.99).
In a randomized clinical trial including 140 patients with AF, the effect of
reducing the amount of alcohol consumed (from 16.8
In summary, reducing alcohol consumption significantly reduces the risk of AF recurrence in patients after catheter ablation.
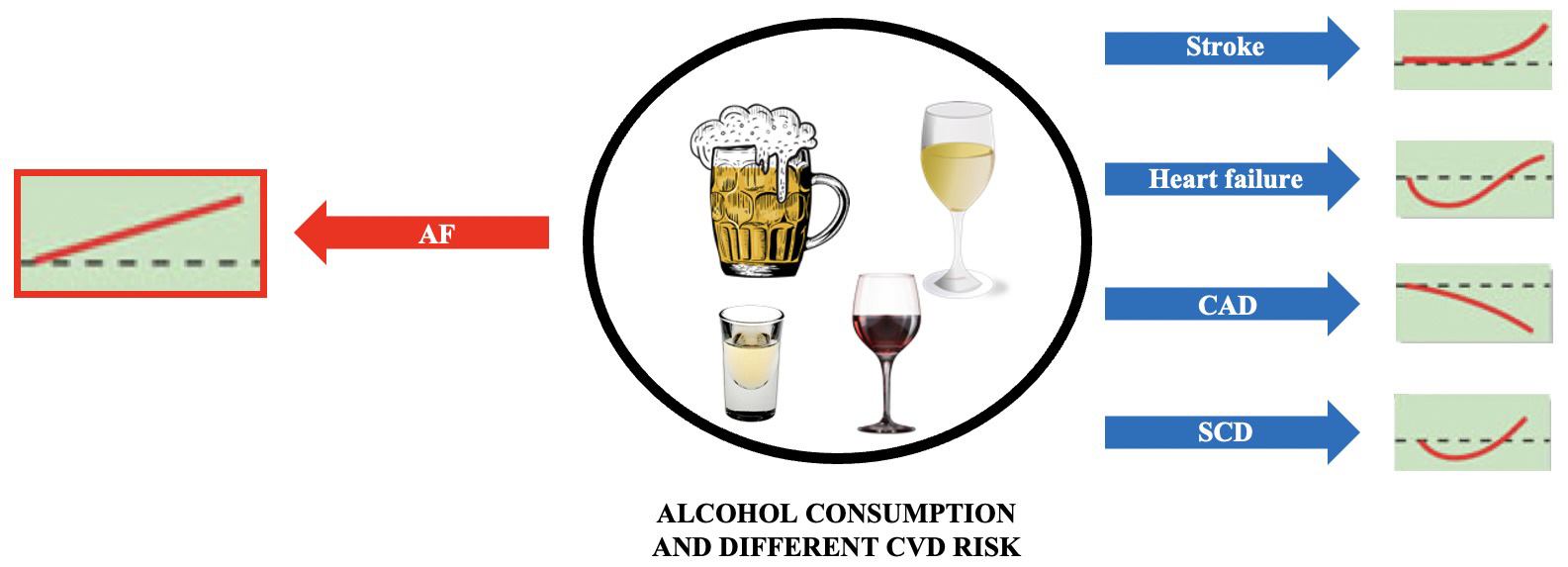
The effect of alcohol consumption on the risk of AF is different from other
cardiovascular diseases (Fig. 3, Ref. [60]). Based on current knowledge, it is
not possible to establish a completely safe amount of alcohol that would not
increase the risk of AF. In patients with new onset AF, limiting alcohol
consumption should be recommended, or be advised to change their consumption
pattern (
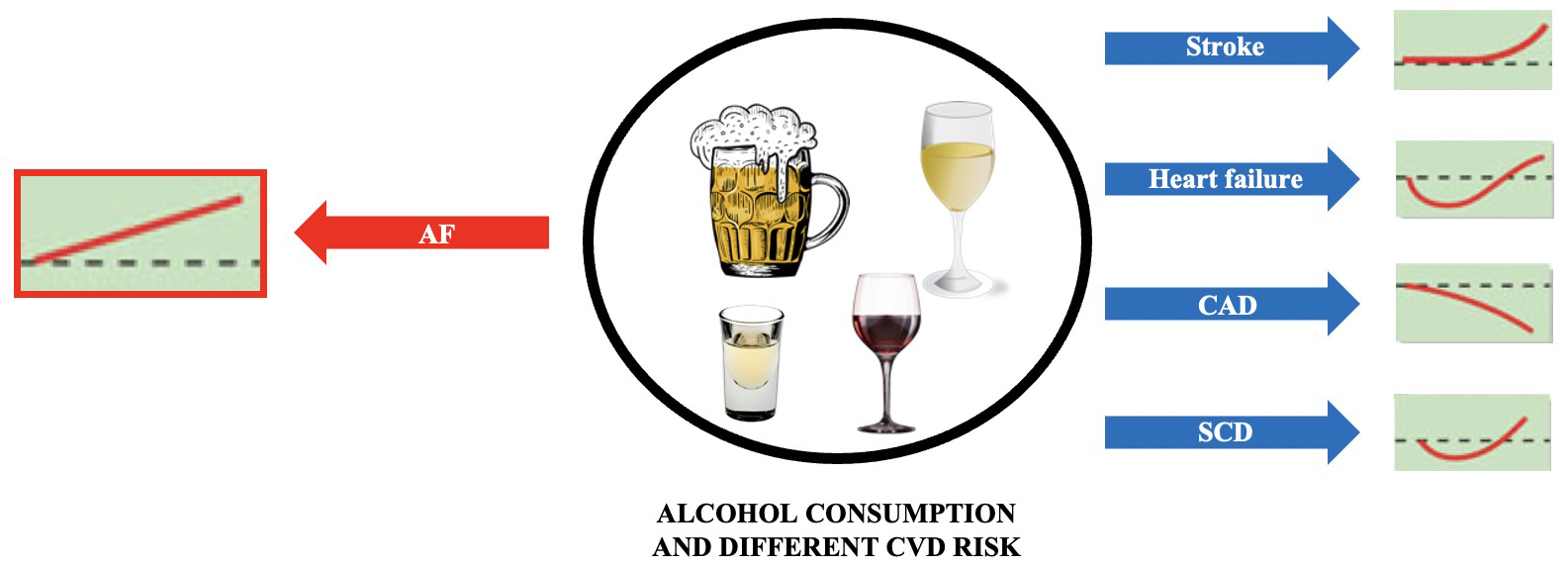 Fig. 3.
Fig. 3.Alcohol consumption and the risk of different cardiovascular diseases. Based on [60]. Abbreviations: AF, atrial fibrillation; CAD, coronary artery disease; SCD, sudden cardiac death.
Writing, review, and revision of the manuscript—SS, GYHL. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.