1 Cardiology Department, Santa Maria della Misericordia Hospital, 06129 Perugia, Italy
2 Centre D'Investigation Clinique-Plurithématique Inserm CIC-P 1433, Inserm U1116, CHRU Nancy Hopitaux de Brabois, Institut Lorrain du Coeur et des Vaisseaux Louis Mathieu, F-CRIN INI-CRCT (Cardiovascular and Renal Clinical Trialists), Université de Lorraine, 54500 Vandoeuvre lès Nancy, France
Academic Editor: Tasneem Z. Naqvi
Abstract
Pulmonary congestion is a critical finding in patients with heart failure (HF) that can be quantified by lung ultrasound (LUS) through B-line quantification, the latter of which can be easily measured by all commercially-available probes/ultrasound equipment. As such, LUS represents a useful tool for the assessment of patients with both acute and chronic HF. Several imaging protocols have been described in the literature according to different clinical settings. While most studies have been performed with either the 8 or 28 chest zone protocol, the 28-zone protocol is more time-consuming while the 8-zone protocol offers the best trade-off with no sizeable loss of information. In the acute setting, LUS has excellent value in diagnosing acute HF, which is superior to physical examination and chest X-ray, particularly in instances of diagnostic uncertainty. In addition to its diagnostic value, accumulating evidence over the last decade (mainly derived from ambulatory settings or at discharge from an acute HF hospitalisation) suggests that LUS can also represent a useful prognostic tool for predicting adverse outcome in both HF with reduced (HFrEF) and preserved ejection fraction (HFpEF). It also allows real-time monitoring of pulmonary decongestion during treatment of acute HF. Additionally, LUS-guided therapy, when compared with usual care, has been shown to reduce the risk of HF hospitalisations at short- and mid-term follow-up. In addition, studies have shown good correlation between B-lines during exercise stress echocardiography and invasive, bio-humoral and echocardiographic indices of haemodynamic congestion; B-lines during exercise are also associated with worse prognosis in both HFrEF and HFpEF. Altogether, LUS represents a reliable and useful tool in the assessment of pulmonary congestion and risk stratification of HF patients throughout their entire journey (i.e., emergency department/acute settings, in-hospital management, discharge from acute HF hospitalisation, monitoring in the outpatient setting), with considerable diagnostic and prognostic implications.
Keywords
- lung ultrasound
- heart failure
- cardiovascular diseases
- cardiac oedema
Signs and symptoms of congestion are a common cause of heart failure (HF) hospitalisation [1], even to a greater extent than the presence of clinical signs of hypoperfusion [2]. Gradual accumulation (within days) or rapid redistribution (within hours) of intravascular and interstitial fluids [i.e., extravascular lung water (EVLW)] are the main causes of the two most common clinical presentations of acute HF (AHF), namely decompensated HF and pulmonary oedema (PO), respectively [2, 3]. Of note, signs and symptoms of pulmonary congestion are the most common findings in AHF, encountered in approximately 75% of AHF patients [2, 4].
Lung ultrasound (LUS) imaging has emerged as a simple semi-quantitative method to detect and assess pulmonary congestion in HF patients through the quantification of B-lines (also known as “comet-tail artifacts” or “lung comets” prior to the release of an International Consensus) [5]. These B-lines are reverberation artifacts, originating from water-thickened pulmonary interlobular septa [6, 7, 8, 9].
The diagnostic usefulness of B-lines has been initially identified in the intensive care unit (ICU) to differentiate PO from other causes of acute respiratory distress syndrome (ARDS) [10]. In this setting, B-lines were closely related to thickenings of the sub-pleural interlobular septa and ground-glass areas assessed by computed tomography [10]. Subsequently, LUS has demonstrated its diagnostic value in identifying a cardiogenic origin of dyspnoea in various settings [i.e., pre-hospital, emergency department (ED), ICU, cardiology/inpatient units] [10, 11, 12, 13, 14, 15, 16, 17]. Additionally, increasing evidence supports that LUS has a sizeable prognostic value in patients with AHF [18], both on admission [19, 20], and at discharge [21, 22]. Furthermore, dynamic changes in B-lines have been promoted as an efficient monitoring of pulmonary decongestion to assess diuretic response [23, 24].
Over the course of the last decade, accumulating evidence derived from ambulatory settings has suggested that LUS, in addition to its potent diagnostic value [25, 26, 27], also represents a key prognostic tool in both HF with reduced (HFrEF) and preserved ejection fraction (HFpEF) [25, 27, 28, 29]. Furthermore, LUS-guided therapy, as compared with standard care, has been shown to reduce the short- and mid-term risk of HF hospitalisations [30, 31]. Finally, B-line changes during exercise stress echocardiography (ESE) were shown to be correlated with different indices of haemodynamic congestion, and also associated with worse prognosis in both HFrEF and HFpEF [32, 33, 34, 35, 36].
The present review summarises current evidence on the use of LUS methodology, its applications as well findings in patients with HF in various clinical settings.
LUS examination can be performed using any commercially available 2-D echocardiographic equipment, and with any transducer probe (i.e., phased-array probes, high frequency linear-probes, curvilinear probes). Each transducer has specific advantages and disadvantages: namely, phased-array probes, as compared with curvilinear probes, have a multipurpose use by allowing both LUS and cardiac examinations; conversely, the footprint size of curvilinear probes (i.e., the length of the active transducer face in contact with the skin) render scanning between ribs more challenging comparatively to phased-array probes [37]. B-lines can be detected by all probes, although low frequency probes (i.e., phased-array or curvilinear probes in the 1 to 5 MHz range) are likely the most suitable for this purpose [38]. While B-line counts may slightly differ when using different transducers in a specific chest zone, the overall clinical picture is not affected by the use of a particular probe [38].
In normal conditions, the only displayable structure is the pleura, a hyperechoic horizontal line which moves synchronously with respiration; this movement is called lung sliding [38]. Additionally, there are some hyperechoic horizontal lines arising at regular intervals from the pleural line: the A-lines. These two findings represent the “A-profile”, a sign of normal content of air in the alveolar spaces. It can be encountered in patients with pneumothorax, asthma or pulmonary embolism [13].
Both physical examination and chest radiography are affected by low sensitivity (about 50–60%) in diagnosing pulmonary congestion in AHF [39]. LUS enables the detection of pulmonary congestion in patients presenting with acute dyspnoea with higher accuracy than chest auscultation or chest X-ray [17]. B-lines, the sonographic sign of alveolar-interstitial syndrome, increase together with a decrease in lung air content, resulting from an impedance mismatch between air and fluid-filled interlobular septa [10].
In the context of AHF, B-lines are comet tail (vertical) hyperechoic artifacts which arise from the pleural line, moving synchronously with lung sliding. They are virtually constantly well-defined and laser-like, extending downward to the edge of the screen, often erasing A-lines [40]. Two other vertical artifacts, not fulfilling the aforementioned criteria, can be displayed by LUS: Z-lines (short, not erasing A-lines; no pathologic significance), and E-lines (arising above the pleural line in subcutaneous emphysema) [41].
The presence of
With regard to LUS findings, B-lines are dynamic in the setting of pulmonary
congestion associated with AHF, and can resolve rapidly with treatment [37].
B-line quantification has been generally reported as a count-based method (i.e.,
the sum of B-lines recorded at each scanning site) or as a scoring system (i.e.,
the number of “positive zones”, defined as a minimum number of B-lines in one
scanning site). According to current recommendations,
In the setting of acute dyspnoea, it may be challenging to differentiate PO from ARDS. As opposed to PO, inhomogeneous interstitial pattern (the “A/B profile”, i.e., predominant B-profile on one side and predominant A profile on the other), highly fragmented pleural line, reduced/abolished lung sliding, and presence of lung consolidation are commonly encountered in ARDS [13, 38, 40]. Similarly, LUS findings of COVID-19 pneumonia are similar to those observed in ARDS [44]. B-lines are frequently seen but may have a patchy distribution, the pleural line may appear irregular with areas of discontinuity; as disease severity progresses, small subpleural hypoechoic consolidations appear.
The transducer can be placed perpendicular to the ribs with the indicator facing cephalad (defined as longitudinal or sagittal scans) or, alternatively, positioned parallel to the intercostal space (defined as oblique or transverse scans) in order to display a larger section of the pleura [37, 38]. LUS can be performed with the patient in any position. However, patient positioning should be standardised when performing serial lung ultrasonographies due to its impact on B-line counts since patients with AHF may have a greater number of B-lines in the supine compared with the sitting position [45]. B-line variability can also occur according to the number of zones, echocardiographic equipment, clip-length, and type of transducer [46].
Several imaging protocols have been described in the literature according to different clinical settings, varying from simple 4-zone to 28-zone LUS. The 2012 International evidence-based recommendations on LUS recommended performing LUS with either 8 or 28 chest zones [5]. Recently, an Expert Consensus Document on LUS suggested that at least 6 zones should be examined in HF patients [42]. The enclosed Table 1 (Ref. [11, 12, 13, 16, 20, 21, 22, 23, 25, 26, 29, 30, 31, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61]) describes specific details regarding LUS scanning protocols. Fig. 1 shows chest zone locations with different lung ultrasound methodologies.
| Lung ultrasound technique – description | |||||
| Scanning protocol | Location of chest zones | - B-line quantification/positive LUS definition | Diagnostic value | Prognostic value | LUS-guided therapy |
| 28 chest zones [16] | 28 points: from the 2nd to 4th (5th on the right side) intercostal spaces at the parasternal, midclavicular, anterior axillary, and midaxillary lines | - B-line count [16, 21, 22, 26, 47, 48] | ++ | +++ | |
| - Picano’s congestion grading: mild (6–15 B-lines), moderate (16–30 B-lines), severe: |
- Decompensated status in CHF: B-line count |
-AHF (admission) | |||
| B-line score (positive if |
B-line count | ||||
| -AHF (discharge) | |||||
| B-line count | |||||
| 11 chest zones [49] | 3 anterior zones (from the sternum to the anterior axillary line, (upper, medium, and lower halves from clavicle to diaphragm) and 3 lateral zones (from the anterior to the posterior axillary line, same subdivision of the anterior area) on right the side; 2 anterior zones (lower zone not assessed due to cardiac interposition) and 3 lateral zones on the left side | - B-line score (sum of positive zone [49] | + | ||
| - Useful in monitoring decongestion; significant correlations with clinical/radiologic congestion score and natriuretic peptides | |||||
| 8 chest zones [50] | 2 anterior zones (from the sternum to the anterior axillary line, subdivided into upper and lower halves from clavicle to the second-third intercostal spaces and from the third space to diaphragm), and 2 lateral zones per side (from the anterior to the posterior axillary line, subdivided into upper and basal halves) | - B-line count [22, 25, 29, 30, 31, 51] | +++ | +++ | +++ |
| - B-line score [22, 52, 53, 54, 55, 56, 57] | AHF diagnosis: | CHF setting | LUS-guided therapy (intervention if B-line | ||
| - AHF: positive scan if |
Sensitivity 65–96% | Positive scanning was associated with adverse outcome (death or HHF) at 6–12 months (adjusted HRs from 1.8 to 4.1) | |||
| - CHF: positive scan if B-line count |
Specificity 69–96% | AHF (discharge) | |||
| NPV 88–94% | B-line count | ||||
| PPV 91–95% | |||||
| 6 chest zones [58] | 2 anterior zones (2nd and 4th intercostal spaces on the hemiclavicular line), and 1 lateral zone (5th intercostal space on the medium axillary line) per side. 2 additional basal zones on the posterior axillary line for pleural effusion assessment | - B-line score [17, 58] | ++ | ||
| AHF diagnosis: | |||||
| Sensitivity 91–94% | |||||
| Specificity 84–93% | |||||
| NPV 91–92% | |||||
| PPV 88–92% | |||||
| 5 chest zones [59] | The surface projections of the 5 major lung lobes | - B-line count (positive scan if B-lines |
+ | ||
| A positive scan independently predicted death of HHF at a median FU of 530 days (adjusted HR 2.9, p = 0.011) | |||||
| 4 chest zones (A) [60] | Four “wet spot” located on the third intercostal space along the midaxillary and anterior axillary lines on both hemithoraces, bilaterally) | - B-line count | + | ++ | |
| B-line grading congestion during stress echocardiography |
- Accuracy in detecting B-lines during ESE |
-Severe congestion during SE independently predicted death or nonfatal MI at a median FU of 15 months in a mixed cohort (adjusted HR 3.54, p = 0.006) | |||
| Sensitivity 94% | |||||
| Specificity 100% | |||||
| NPV 88% | |||||
| PPV 100% | |||||
| Scanning protocol | Location of chest zones | - B-line quantification/positive LUS definition | Diagnostic value | Prognostic value | LUS-guided therapy |
| 4 chest zones (B) [23] | Apical and mammillary regions on the midclavicular line bilaterally (as part of the CaTUS protocol, also including IVC, E/e’, and pleural effusion assessment) | - B-line score ( |
+ | + | |
| - AHF diagnosis (LUS alone): | -Resolution of pulmonary congestion at discharge in AHF (i.e., responder patients) independently predicted mortality at 6 months (HR 0.19, p = 0.010). | ||||
| Sensitivity 96% | |||||
| Specificity 81% | |||||
| NPV 88–94% | |||||
| PPV 91–95% | |||||
| - Responders at discharge had larger absolute decrease in E/e’, VAS score and IVCi during treatment and a lower E/e’, VAS score, BNP and IVCi on the day of discharge | |||||
| 4 chest zones (C) [20] | Upper anterior and basal lateral halves of the 8 chest zone protocol, bilaterally | - B-line count and B-line score [20] | + | ++ | |
| -Useful in monitoring decongestion in AHF patients | - Admission tertile II (B-lines 5–9) and III (B-lines | ||||
| - Discharge tertile III (B-lines | |||||
| BLUE Protocol [13] | 2 anterior symmetrical regions per lung, an upper BLUE point located at the anterior chest at the midclavicular line on the 2nd-3rd intercostal space, and a lower BLUE point located at the anterior axillary line, just above the nipple | - B-line score (positive if |
+++ | ||
| - AHF/PO diagnosis: | |||||
| Sensitivity 97% | |||||
| Specificity 95% | |||||
| NPV 99% | |||||
| PPV 87% | |||||
| CaTUS, cardiothoracic ultrasound; BLUE, Bedside Lung Ultrasound in Emergency;
HR, hazard ratio; ESE, exercise stress echocardiography; SE, stress
echocardiography; MI, myocardial infarction; IVCi, inferior vena cava index; VAS,
visual analogue scale, PO, pulmonary oedema; HHF, hospitalisation for heart
failure, AHF, acute heart failure; CHF, chronic heart failure; NPV, negative
predictive value; PPV, positive predictive value. B-line count: sum of B-lines in all zones. B-line score: sum of positive zones (defined as *LUS performed at the end of exercise and beginning of recovery within 1 to 2 min after termination of stress, or extemporaneously at the time of antidote administration in pharmacological stress testing. | |||||
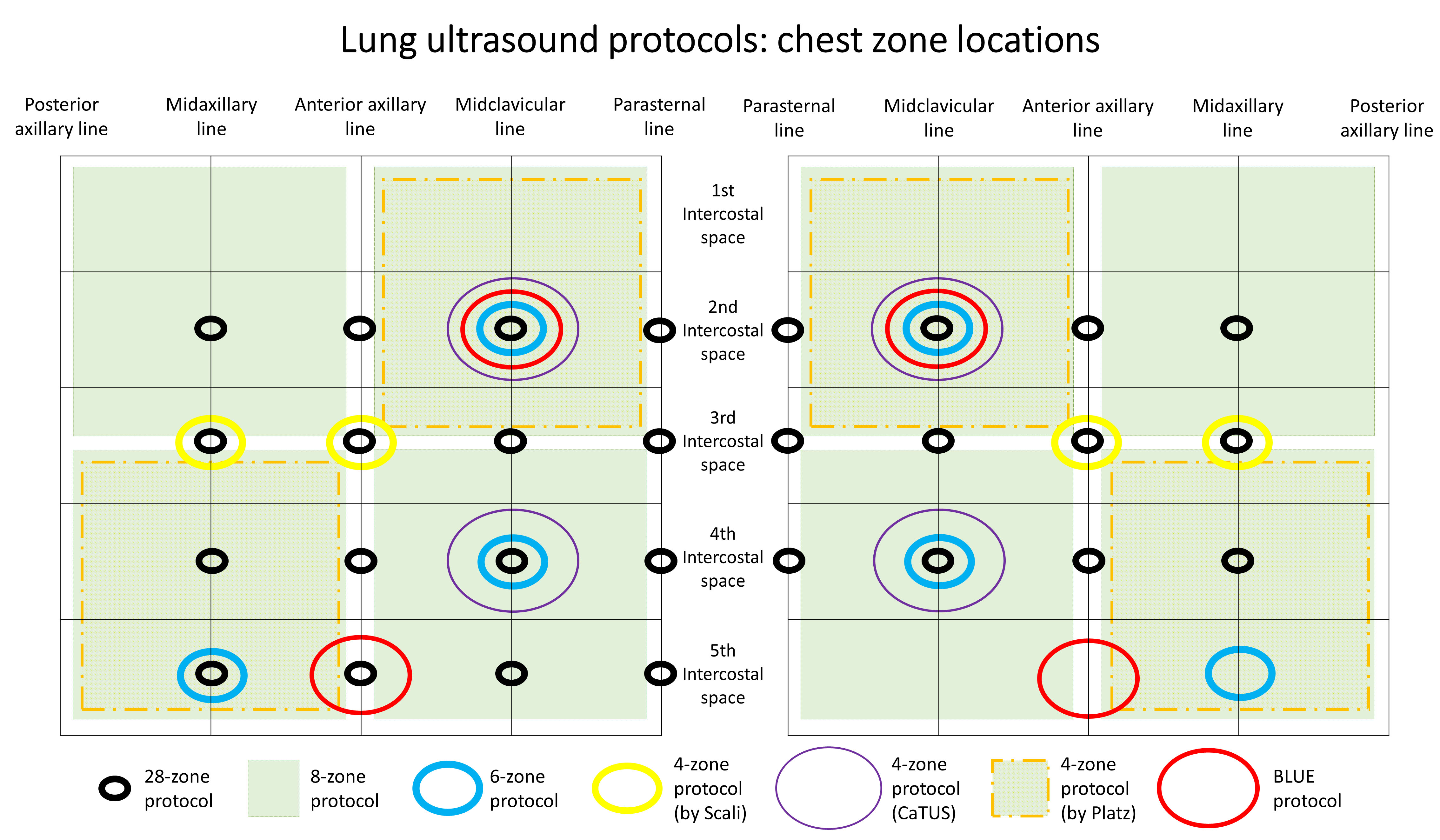 Fig. 1.
Fig. 1.Chest zone locations with different lung ultrasound methodologies.
The 8-zone protocol, introduced in 2006 by Volpicelli, represents the most versatile scanning method, largely adopted in both acute and chronic settings [25, 50]. Fig. 2 illustrates main findings with 8-zone protocol in different settings, and Fig. 3 shows an illustration in a patient with AHF. The 8-zone protocol consists of 2 anterior zones (from the sternum to the anterior axillary line, subdivided into upper and lower halves from the clavicle to the second-third intercostal spaces and from the third space to the diaphragm), and 2 lateral zones (from the anterior to the posterior axillary line, subdivided into upper and basal halves) per side. Volpicelli proposed another scanning protocol with 11 zones, 6 on the right side and 5 on the left side [49]. The 6 chest zone protocol was derived from the 8-zone protocol by locating six specific points of intersections on the hemiclavicular and midaxillary line [58].
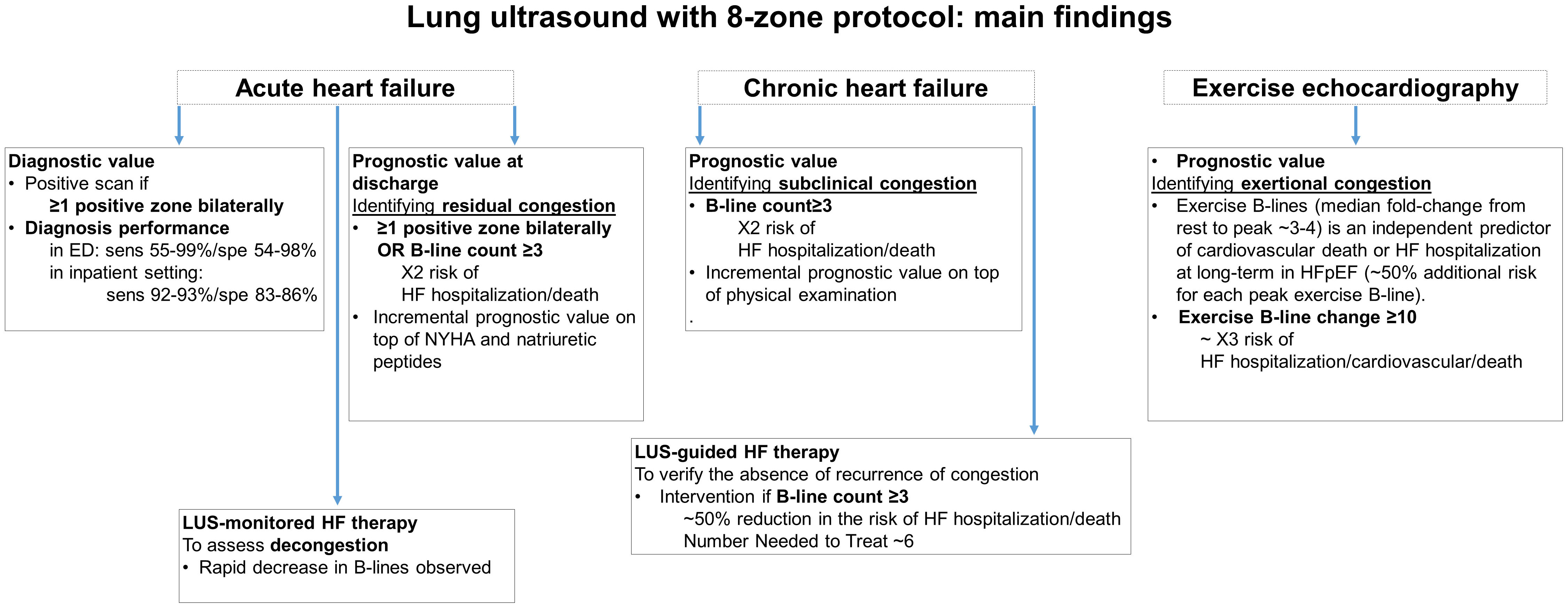 Fig. 2.
Fig. 2.Different applications and main findings of lung ultrasound methodology with 8-zone protocol.
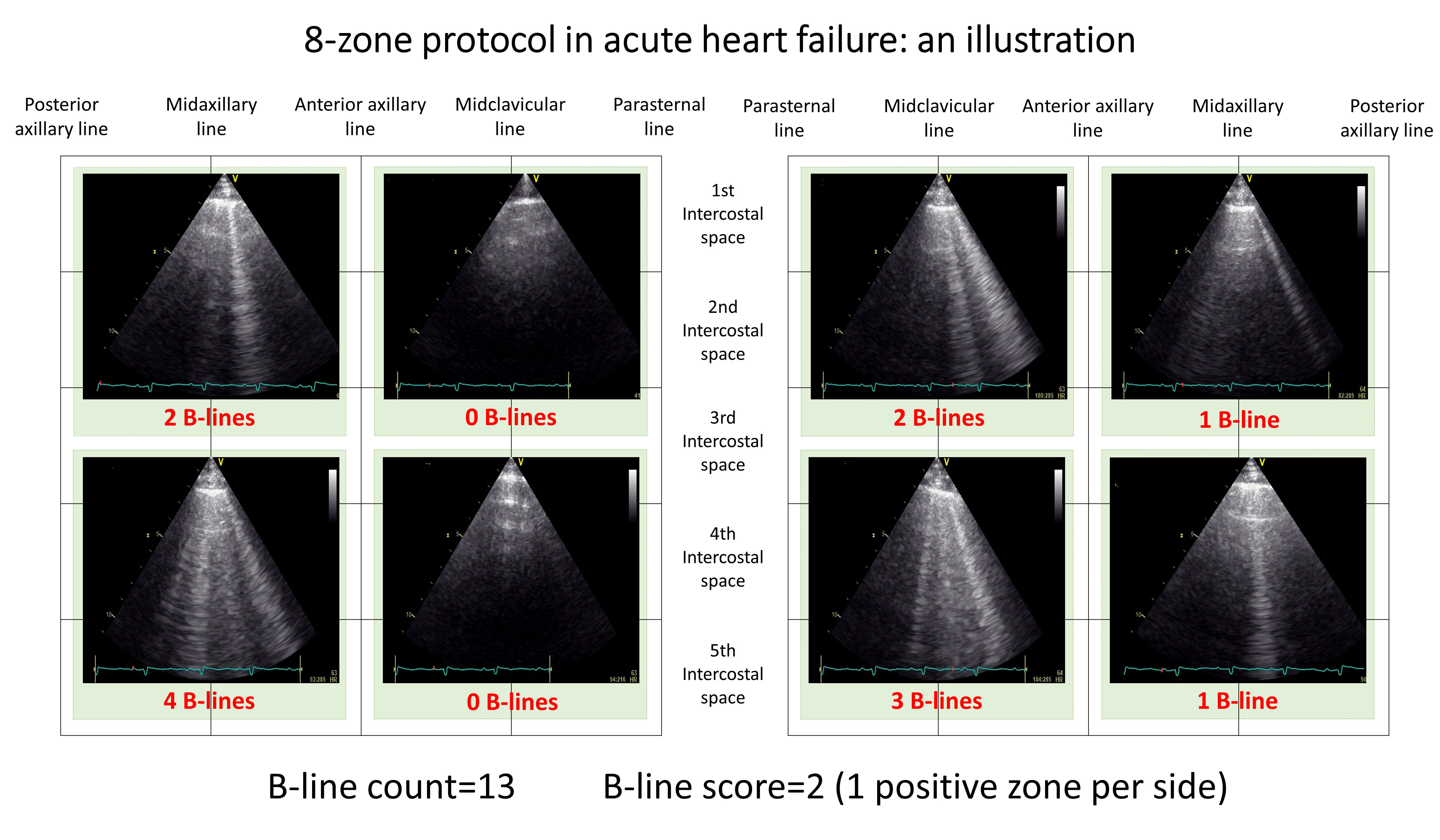 Fig. 3.
Fig. 3.8-zone protocol application: findings in a patient with acute heart failure.
The 28-zone protocol, more time-consuming in comparison with the 8-zone protocol, has had broad use particularly in the chronic ambulatory setting [26, 62] and at discharge from an HF hospitalisation [22]. It includes bilateral scanning from the 2nd to 4th (5th on the right side) intercostal spaces at the parasternal, midclavicular, anterior axillary and midaxillary lines [16, 22].
Three different 4-zone protocols have been reported in the literature. The first protocol (by Scali et al. [60]) was derived from the 28-zone protocol, in which four “wet spots” (i.e., the zones with highest B-line density, located on the third intercostal space along the midaxillary and anterior axillary lines on both sides) were identified. Correlation between B-line counts obtained with the 2 scanning protocols was excellent [60]. Another 4-zone protocol is part of the cardiothoracic ultrasound (CaTUS) protocol, including apical and mammillary regions on the midclavicular line bilaterally [23]. A third 4-zone protocol was proposed by Platz et al. [20], which includes upper anterior and basal lateral halves of the 8-zone protocol, bilaterally. In critical ICU patients, the bedside lung ultrasound in emergency (BLUE) protocol consists of six zones, 4 of which are investigated for the diagnosis of PO [13]. Finally, a 5-zone protocol was proposed by Gustafsson et al. [59].
There are several settings for LUS implementation in patients with dyspnoea and presumed AHF. ED physicians often face the challenge of differentiating between pulmonary and cardiac causes of acute respiratory failure; a timely diagnosis of AHF has major implications since early treatment can improve short-term outcomes [63].
In a prehospital setting, LUS feasibility was deemed excellent, with a very high negative predictive value (NPV) (approximately 95%) in ruling out AHF, and with a good positive predictive value (PPV) (77.3%) [15]. Additionally, LUS (NPV 100%, PPV 96%) was the best single method for diagnosing AHF in the prehospital setting (i.e., performed immediately after arrival of the patient at the ED but prior to any administered treatment) when compared with NT-proBNP and physical examination [64].
In the ED, the sensitivities and specificities of LUS for AHF range from 55 to 100% and from 54 to 98%, respectively [12, 17, 43, 50, 53, 54, 55, 57, 58, 65, 66, 67, 68, 69, 70, 71]. The diagnostic value of LUS (usually using the 8-zone method) has mostly been assessed alone or, in some studies [12, 57, 65, 67, 69, 70], integrated with various cardiac ultrasound protocols, including assessment of inferior vena cava diameter, left ventricular ejection fraction (LVEF), severity of mitral regurgitation, and estimated left ventricular filling pressures by E/e’.
In a large multicenter, prospective cohort study by Pivetta et al. [17]
(N = 1005), a 6-zone LUS approach had a significantly higher accuracy for AHF
(sensitivity 97%, specificity, 97.4%) compared to clinical workup alone, chest
X-ray or NT-proBNP, and showed an additive diagnostic value on top of a standard
approach [net reclassification improvement (NRI) 19.1%, 95% confidence interval
(CI) 14.6–23.6, p
Recently, Buessler et al. [43] compared the diagnostic accuracies of
various LUS scanning protocols [i.e., 4- (BLUE protocol), 6-, 8-, and 28-zone
protocols] in diagnosing AHF in a cohort of 117 ED patients admitted for acute
dyspnoea and diagnostic uncertainty. Among the studied scanning protocols, the
8-zone protocol (
In an inpatient setting (cardiology or internal medicine department), various
studies have also confirmed the diagnostic accuracy of LUS [16, 56, 72, 73, 74, 75], with sensitivities and specificities ranging from 81 to 97%, and from 79 to 86%,
respectively. Of particular interest, the diagnostic accuracy of LUS in detecting
high estimated left ventricular pressures (as assessed by E/e’
Overall diagnostic value can also be derived from various meta-analyses
published in the last decades, including different patient populations. Al Deeb
et al. [76] reported that the sensitivity and specificity of B-lines in
diagnosing acute cardiogenic pulmonary oedema was 94% and 92%, respectively, in
a mixed population (N = 1075) encompassing patients from ICU, internal medicine
wards, and prehospital-ED settings with different LUS methods, which also
included count-based methods. Martindale et al. [77] performed a
meta-analysis including 1918 patients (8 studies in an ED setting), assessed only
with score-based methods (primarily with the 8-zone protocol), with a reported
sensitivity and specificity of 85% and 93%, respectively. A more recent
meta-analysis by McGivery et al. [78] (1861 ED patients with
undifferentiated dyspnoea; 7 studies adopting the Volpicelli method), reported
comparable sensitivity (83%), albeit with lower specificity compared with the
study of Martindale et al. [77]. In a meta-analysis including a mixed
population of 1827 patients from ED or internal medicine settings, Maw et
al. [79] compared the accuracy of LUS with chest-X-ray in which LUS was found to be
more sensitive than chest-X ray in diagnosing AHF (88% vs. 73%, relative
sensitivity ratio = 1.2, p
In addition to B-lines, pleural effusion (i.e., an anechoic or hypoechoic space between the two pleural layers) also has diagnostic value for AHF [53, 58, 77]. Overall, unilateral (mostly on the right side) or bilateral pleural effusions are encountered in about 60% of patients with AHF [53] and are associated with a higher risk of death or HF hospitalisation when combined with B-lines in outpatients [59]. However, the identification of pleural effusion by LUS only has moderate accuracy for the diagnosis of AHF (sensitivity ~60%, specificity ~70%) [77]. As compared to pleural effusion alone, the coexistence of B-profile and pleural effusion increases LUS specificity, but may decrease sensitivity given that not all patients with acute cardiogenic dyspnoea show pleural effusion [58]. Finally, large pleural effusions may interfere with B-line quantification as they can induce B-lines that are not related to pulmonary congestion (but rather to passive changes in lung tissue compressed by pleural effusion).
The potential utility of LUS in monitoring pulmonary decongestion in response to
AHF treatment has been assessed in several studies [20, 23, 24, 47, 49, 80, 81].
In a mixed cohort of 340 patients admitted for dyspnoea, Frassi et al. [81]
showed that in the subgroup (N = 70) exhibiting a clinical response to treatment
(i.e., decrease in NYHA functional class
Of note, data on the concomitant decline of B-line counts and natriuretic peptides are conflicting [23, 49, 80]. Natriuretic peptide clearance in an acute setting appears to exhibit slower kinetics when compared with B-line variations to therapy, especially in the presence of renal failure [23]. Divergent results have also been reported for E/e’ [23, 80], although definitive conclusions cannot be drawn given the small size of these studies. The most probable underlying reasons for these discrepancies are the distinct kinetics of the various, congestion variables, as well as the fact that each congestion variable measures a different area of congestion, e.g., LUS specifically investigates pulmonary congestion whereas E/e’ investigates intracardiac pressure, which can induce pulmonary congestion differently depending on the physical properties of the alveolocapillary border and the level of lung inflammation.
Pulmonary congestion assessed by LUS has been shown to be associated with adverse outcome in patients hospitalised for AHF, regardless of the timing of quantification during the hospital stay [82]. Indeed, its prognostic value has been demonstrated at admission [19, 20, 21, 47, 82, 83] and at discharge [20, 22, 47, 48, 52, 82, 83, 84]. The enclosed Table 2 (Ref. [20, 21, 22, 25, 29, 47, 48, 51, 62, 82, 84, 85]) describes specific details regarding prognostic value of LUS in different settings.
| Author year | Population | Total | FU |
Chest zones; position | Age | LVEF% | B-lines quantification (stratification level) | Total events | Event details | HR/RR (CI) p value |
Covariates of adjustment |
| Outpatient setting | |||||||||||
| Curbelo et al., 2018 [51] | CHF | 99 | 12 m | 8; NA | 84.2 (6.5) | 57.5 (14.9) | Stratification |
36 | Death: 12 | Multi: 1.8 (0.8–4.0) p = NA | Gender, age, LVEF, NYHA class, GFR, Hb |
| HHF: 35 | Uni: 1.7 (0.8–3.5) | ||||||||||
| Dwyer et al., 2018 [29] | Ambulatory HF patients and hypertensive patients | 119 HF (total = 230) | 12 m | 8; supine | 66 (20–93) | 55 (46–62) | Stratified |
28 (patients with HF) | Death: 10 | Multi: 2.62 (1.15–5.96) p = 0.022 | Age, sex |
| HHF: 21 | Uni: 2.46 (1.15, 5.26) p = 0.020 | ||||||||||
| Pellicori et al., 2019 [62] | CHF | 342 | 7.8 (4.5–11.7) m | 28; near-supine position | 75 (68–82) | 45 (14) | Continuous and stratified 0–3; 4–13; |
60 | Death: 25 | Multi: 1.54 (0.68–3.48), p = 0.29 | Age, NYHA class (III vs. I/II), urea, Hb and log NTproBNP + JVD ratio |
| HHF: 35 | Uni: 4.33 (2.09–8.98), p | ||||||||||
| Platz et al., 2016 [25] | Patients with HF (NYHA II-IV) | 195 | 6 m | 8; NA | 66 (24–93) | 34 (23–51) | Stratified Tertiles | 50 | Death: 15 | Multi: 4.08 (1.95–8.54), p |
Age, gender, NYHA class III or IV, and congestion score |
| (0; 1–2; |
HHF: 48 | ||||||||||
| Urgent visit: 9 | Uni: 3.78 (1.88–7.63), p | ||||||||||
| Domingo et al., 2021 [85] |
At least 1 HHF and/or LVEF |
577 | 31 |
8; semi-supine | 68.8 (12.3) | 45.4 (12.6) | Continuous & quartiles | 157 | Death: 111 | Multi: 1.26 (0.89–1.77), p = 0.19 | Age, sex, BMI, ischemic aetiology, Log HF duration, NYHA, LVEF, diabetes, hypertension AF/AFlu, renal insufficiency, ACEI-ARB, BB, Loop diuretics, Hydralazine, nitrates |
| (Q1 = 1 B-lines, | |||||||||||
| Q2 = 3 B-lines, | |||||||||||
| Q3 = 7 B-lines, Q4 |
HHF: 74 | Uni: 1.66 (1.20–2.30), p = 0.002 | |||||||||
| AHF (admission) | |||||||||||
| Gargani et al., 2015 [47] | Dyspnoea and/or suspicion of AHF | 100 | 6 m | 28; supine or near supine | 70 (11) | 37 (14) | Stratified |
14 | Death: 4 | Multi: 4.87 (0.88–27.06), p = 0.07 | NYHA class, Hb, NT-proBNP at discharge, BL at admission and discharge |
| (5.3 |
HHF: 14 | Uni: 5.83 (1.82–18.62), p = 0.002 | |||||||||
| Coiro et al., 2016 [82] | ADHF | 50 (total 110) | 3 m | 28; supine or near supine | 73 (2) | 37 (2) | Stratified |
33 in whole cohort | Death: 16 | Multi: 9.20 (1.82–46.61), p = 0.007 | B-lines categorical, NYHA class, IVC diameter, echocardiographic (E/A |
| HHF: 26 | Uni: 5.85 (1.86–18.46), p = 0.003 | ||||||||||
| Gargani et al., 2021 [21] |
HFrEF | 296 HF (total = 1021) | 14.4 m | 28; supine | 70 (62–76) | 30 (23–35) | Stratified |
82 | Death: 40 | Multi: 1.90 (1.14–3.16) | Age, creatinine, NYHA class |
| HFpEF | 73 (66–80) | 55 (50–60) | HHF: 42 | ||||||||
| AHF (discharge) | |||||||||||
| Coiro et al., 2015, 2016 [22, 82] | ADHF | 60 | 3 m | 8 and 28; supine or near supine | 72.1 (10.2) | 47.5 (27.2–52) | Continuous and stratified ( |
18 | Death: 10 | Multi: 4.1 (0.95–14.63), p = 0.055 | Clinical (lung rales, ankle oedema, NYHA class |
| (MDRD) creatinine clearance | |||||||||||
| HHF: 15 | Uni: 5.8 (2.1–16.3), p = 0.001 | (E/A | |||||||||
| Gargani et al., 2015 [47] | Dyspnea and/or suspicion of AHF | 100 | 6 m | 28; supine or near supine | 70 (11) | 37 (14) | Stratified |
14 | Death: 4 | Multi: 11.74 (1.3–106.16), p = 0.028 | NYHA class, Hb, NT-proBNP at discharge, BL admission & discharge |
| HHF: 14 | Uni: 24.12 (3.15–184.55), p = 0.002 | ||||||||||
| Rivas-Lasarte et al., 2020 [84] | ADHF without sub-clinical congestion (n = 59) | 100 (total 123) | 6 m | 8; semi-recumbent | 65 (14) | 38 (13) | Stratified B-lines ( |
28 | Death: 3 | Multi: 2.63 (1.08–6.41), p = 0.033 | Age, renal insufficiency, AF, anaemia, NYHA class, NT-proBNP levels, systemic clinical congestion, group intervention (LUS-guided strategy) |
| ADHF with sub-clinical congestion (n = 41) | 70 (10) | 39 (14) | HHF: 19 | Uni: NA | |||||||
| Urgent visit: 12 | |||||||||||
| Platz et al., 2019 [20] | Acute HF | 132 (349) | 3 m | 4; semi-recumbent | 72 (60–83) | 41 (17) | Stratified B-lines (3 tertiles: 0–3; 4–6; |
42 | Death: 13 | Multi: 1.45 (0.6–3.46), p = 0.41 | Age, log creatinine, SBP (stratified by sex) |
| 76 (64–86) | 39 (14) | HHF: 32 | Uni: 1.42 (0.61–3.32), p = 0.42 | ||||||||
| Rueda-Camino et al., 2021 [48] | ADHF with preserved LVEF | 103 | 3 m (2.4 |
28 | 82.2 (9.1) | 61.1 (7.0) | Stratified |
28 | Death: 1 | Multi: 2.46 (1.11–5.46), p = 0.03 | Sex, functional class, Charlson’s comorbidity index, Barthel’s index, respiratory comorbidity (COPD, asthma, and sleep apnoea-hypopnea syndrome) |
| HHF: 27 | Uni: 2.39 (1.12−5.12), p = 0.024 | ||||||||||
| AA, aldosterone antagonist; ACEI, angiotensin converting enzyme inhibitor; AF,
atrial fibrillation; AFlu, atrial flutter; ARBs, angiotensin receptor blockers;
ARNI, angiotensin receptor neprilysin inhibitor; ADHF, acute decompensated heart
failure; AHF, acute heart failure; CAD, coronary artery disease; CCB, calcium
channel blocker; CHF, congestive heart failure; COPD, chronic obstructive
pulmonary disease; CRT, cardiac resynchronisation therapy; CV, cardiovascular;
FU: follow-up; Hb, haemoglobin; HHF, hospitalization for HF; HR, hazard ratio;
GFR, glomerular filtration rate; ICD, implantable cardioverter defibrillator;
ILD, interstitial lung disease; IVCd: inferior vena cava diameter; LVEF, left
ventricular ejection fraction; LUS, lung ultrasound; MRA, mineralocorticoid
antagonist; multi, multivariable; NA: not available; NYHA, New York Heart
Association; RR, risk ratio; SBP, systolic blood pressure; Uni, univariable; VAD,
ventricular assist device. *B-lines ^FU mean or median duration reported in parenthesis. a adjusted hazard ratio presented for selected cut-offs. $ HRs provided by the authors. Hazard ratios are presented for combined end-points. | |||||||||||
In a study by Platz et al. [20] using the 4-zone protocol, a B-line
count
Residual pulmonary congestion as assessed by B-line count at time of discharge has been shown to identify a subset of patients with AHF at high risk of readmission or death [20, 22, 47, 48, 52, 82, 83, 84], while its prognostic value appeared to be far superior to admission B-lines when assessed in the same study [47, 83].
In 2015, two different research groups first demonstrated the prognostic value
of discharge B-lines as assessed with the 28-zone protocol [22, 47]. Gargani
et al. [47] showed that a B-line count
The presence of subclinical pulmonary congestion assessed with the 8-zone
protocol at discharge (i.e., “dry lung” on auscultation with a B-line count
Finally, the overall prognostic value of both admission and discharge B-lines
has been assessed in several meta-analyses [88, 89, 90]. A fixed-effect meta-analysis
by Rastogi et al. [90] which included studies published from 2010 and
2021, yielded the following cut-off points for pooling risk estimates: (i)
admission: B-lines
Various studies have highlighted the usefulness of LUS in identifying a
decompensated HF status in an outpatient setting. In a cohort of 97 HFrEF
outpatients, Miglioranza et al. [26] found that LUS (assessed with the
28-zone protocol) yielded a C-statistic of 0.89 in identifying a decompensated
status (NT-proBNP
Pulmonary congestion assessed by LUS is associated with worse prognosis in
ambulatory patients [25, 27, 28, 29, 51, 62, 85, 91] (see Table 2 for more details).
Platz et al. [25] first demonstrated the prognostic value of B-lines
(assessed with the 28-zone protocol) in a cohort of 195 NYHA class II–IV HF
outpatients. Patients in the third tertile (B-line count
The usefulness and prognostic impact of LUS in addition to standard care in the
management of HF outpatients has recently been assessed in several studies (Table 3, Ref. [30, 31, 92]). Rivas Lasarte et al. [30] randomised 123 outpatients
discharged from AHF to either standard follow-up (N = 62) or a LUS-guided
follow-up (N = 61). In both groups, patients were treated according to current
guidelines, and followed the same schedule of visits after hospital discharge. In
the LUS-group (assessed with the 8-zone protocol), treating physicians were
encouraged to modulate diuretic therapy in accordance with the recorded B-lines
during follow-up; a B-line count
| Author year | Study design | Population description | Chest zones; position | B-lines quantification | FU | Total N | Number in each group | Age | LVEF% | Total events | Deaths | HHF | Urgent visits | HR/RR (CI) p value | Covariates of adjustment | Main exclusion criteria |
| Rivas-Lasarte et al., 2019 [30] | Single-blind randomized clinical trial | HF patients (HF defined by shortness of breath, pulmonary congestion on X-ray and high NT-proBNP values in the first 24 h of admission | 8; semi-recumbent | Counts | 6 m | 123 | control group (n = 62) | 69 (11) | 39 (15) | 25 | 2 | 13 | 13 | 0.52 (0.27–0.99), p = 0.049 | NA | Inability to attend FU visits; life expectancy of |
| LUS group (n = 61) | 69 (13) | 39 (14) | 14 | 3 | 14 | 3 | ||||||||||
| Araiza-Garaygordobil et al., 2020 [31] | Single-blinded, randomized controlled trial | ADHF patients | 8; semi-recumbent | Counts | 6 m | 126 | control group (n = 63) | 63 (51–73) | 34.9 (14) | 30 | 6 | 8 | 25 | 0.55 (0.30–0.99), p = 0.044 | Adjusted for sex, age, and NT-proBNP |
Severe lung disease preventing LUS interpretation, lack of will to participate, life expectancy shorter than 6 months, chronic kidney injury with Egfr |
| LUS group (n = 63) | 62 (52–71) | 30 (15.2) | 20 | 9 | 4 | 9 | ||||||||||
| Marini et al., 2020 [92] | Randomised multi-centre non-blinded study | Chronic HF and optimised medical therapy with LVEF |
8; NA | NA | 3 m | 244 | control group (n = 117) | 69.79 (11.34) | 30.73 (8.43) | 25 | 4 | 25 | NA | 0.44 (0.23–0.84), p = 0.01 (RR for HHF) | NA | NA |
| LUS group (n = 127) | 73.22 (10.94) | 32.16 |
12 | 5 | 12 | NA | ||||||||||
| ACEI, angiotensin converting enzyme inhibitor; ARBs, angiotensin receptor blockers; ARNI, angiotensin receptor neprilysin inhibitor; HF, heart failure; CRT, cardiac resynchronization therapy; FU, follow-up; GFR, glomerular filtration rate; HR, hazard ratio; ICD, implantable cardioverter defibrillator; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid antagonist; NA, not available/not applicable. | ||||||||||||||||
Lung ultrasonography is a reliable and reproducible tool to assess EVLW during stress echocardiography in HF patients (both in HFrEF and in HFpEF,) in conjunction with ESE or pharmacological stressors, both at submaximal and maximal workloads [32, 33, 60, 61, 94]. In a large mixed cohort of 2145 patients referred for stress echocardiography (exercise ~45%, dypiridamole ~50%) with known/suspected coronary artery disease or HF, approximately 15% developed moderate or severe pulmonary congestion as assessed with the 4-zone protocol by Scali et al. [61] (see Table 1 for LUS timing and congestion grading during stress echocardiography), while severe stress B-lines (HR 3.54, 95% CI 1.47–8.69, p = 0.006) independently predicted long-term death or nonfatal myocardial infarction. The authors concluded that stress echocardiography can be easily complemented with LUS to assess dynamic changes in pulmonary congestion through B-line quantification and better stratify the prognosis of HF patients. These findings confirmed earlier preliminary results from the same group [95].
With particular reference to HF patients, LUS has been shown to enable real-time
monitoring of pulmonary congestion elicited by exercise, showing a swift increase
in B-line count [96]. Agricola et al. [36] first described B-line
development during exercise with LUS (28-zone protocol) performed in the recovery
phase (
With respect to HFpEF, we demonstrated that submaximal ESE coupled with LUS (28-zone protocol) allowed the detection of
pulmonary congestion development (median B-line count from 3 to 9) in a cohort of
31 HFpEF patients, occurring concomitantly with changes in E/e’, PASP and
natriuretic peptides (i.e., BNP); these variations were significantly greater in
magnitude when compared with changes observed in the control group (N=19
hypertensive patients) [32]. In a subsequent study, we found that these B-line
changes were mostly predicted by worsening echocardiographic indices of diastolic
function (i.e., E/e’ and strain rate-derived A wave) in an extended cohort of 81
patients [94]. In another study comprised of a cohort of 61 invasively-proven
HFpEF patients undergoing submaximal haemodynamic exercise testing, the onset or
increase in B-lines (assessed in 2 positions in the left third intercostal space
along the mid-axillary and mid-clavicular lines) was associated with an increase
in both PCWP and right atrial pressure, and
to an impairment in right ventricular (RV)-to-pulmonary circulation coupling,
both at rest and during exercise, as assessed by ratios of tricuspid annular
plane systolic excursion (TAPSE) and RV s’ or invasive mean pulmonary arterial
pressure [34]. Additionally, in another cohort of 188 HFpEF patients undergoing
combined cardiopulmonary-echocardiography exercise stress testing, epicardial
adipose tissue accumulation (i.e.,
In the same cohort of HFpEF patients [94], we demonstrated that both peak B-line
counts (HR 1.50, 95% CI, 1.21–1.85, p
LUS represents a reliable and useful tool for the assessment of pulmonary congestion and risk stratification of HF patients throughout the entire patient journey (i.e., ED/acute settings, in-hospital management, discharge from an acute HF hospitalisation, and monitoring in the outpatient setting), with considerable diagnostic and prognostic implications. The 8-zone protocol appears to offer the best trade-off with no sizeable loss of information.
SC—Writing - original draft, Validation, Visualization. TR—Writing - review & editing. NG—Writing - original draft, Validation, Visualization, Supervision.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.



