Academic Editors: Manuel Martínez-Sellés and Alpo Vuorio
Background: The
coronavirus disease 2019 (COVID-19) pandemic has severely affected healthcare
systems around the world. This study aimed to investigate the perceptions of
cardiologists regarding how the COVID-19 pandemic has affected the clinical
practice patterns for acute coronary syndrome (ACS). Methods: A
multicenter clinician survey was sent to 300 cardiologists working in 22
provinces in China. The survey collected demographic information and inquired
about their perceptions of how the COVID-19 pandemic has affected ACS clinical
practice patterns. Results: The survey was completed by 211 (70.3%)
cardiologists, 82.5% of whom were employed in tertiary hospitals, and 52.1%
reported more than 10 years of clinical cardiology practice. Most respondents
observed a reduction in ACS inpatients and outpatients in their hospitals during
the pandemic. Only 29.9% of the respondents had access to a dedicated catheter
room for the treatment of COVID-19-positive ACS patients. Most respondents stated
that the COVID-19 pandemic had varying degrees of effect on the treatment of
acute ST-segment elevation myocardial infarction (STEMI), acute non-ST-segment
elevation myocardial infarction (NSTEMI), and unstable angina. Compared with the
assumed non-pandemic period, in the designed clinical questions, the selection of
coronary interventional therapy for STEMI, NSTEMI, and unstable angina during the
COVID-19 pandemic was significantly decreased (all p
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2, has rapidly spread and has resulted in considerable morbidity and mortality [1, 2, 3, 4]. The pandemic has severely affected healthcare systems around the world, and these systems have struggled to effectively prevent and treat COVID-19. Furthermore, there has been additional pressure because the pandemic has profoundly disrupted the clinical practice patterns of other common diseases.
The management of acute coronary syndrome (ACS) during the COVID-19 pandemic should be investigated to better understand the balance between the clinical benefits of treatment and the risk of viral transmission. Previous studies have found a significant increase in the morbidity and mortality of ACS patients owing to direct and indirect effects of the COVID-19 pandemic [5, 6, 7, 8, 9, 10, 11]. Although there has been an expert consensus on the interventional treatment of acute myocardial infarction during the COVID-19 pandemic [12], decision-making for ACS treatment during the pandemic has been problematic owing to different and unequal medical resources around the world. In particular, many hospitals do not have dedicated cardiac catheterization rooms for COVID-19 patients. At present, there is a lack of real-world data from large-sample randomized controlled trials to understand how COVID-19 has affected the clinical practice patterns of ACS. In this study, we conducted a questionnaire survey of cardiologists from 22 provinces in China to investigate their views on how the COVID-19 pandemic has affected their ACS treatment strategies.
The intended target population of the survey was cardiovascular department physicians who treat patients with ACS. An online survey was distributed via WeChat (Version 8.0.21, Tencent, Shenzhen, China) software to 300 cardiologists in 22 provinces in China (Supplementary Fig. 1) between April 1, 2022 and April 30, 2022. The clinician survey was completed anonymously, and all responses were submitted by April 30, 2022. The study was approved by the Ethics Committee of Renji Hospital affiliated with the School of Medicine, Shanghai Jiao Tong University (KY2022-096-A).
The survey was administered in Chinese and consisted of three parts (translated into English and available in Supplementary Material). In part 1, we collected the participants’ demographic information, including years of practice, subspecialty, hospital level, and province. Part 2 included questions regarding the severity of the COVID-19 pandemic in their province. Part 3 consisted of structured questions to gain insight into how the COVID-19 pandemic affected their ACS clinical practice patterns. The detailed questions in part 3 investigated how the participants treated acute ST-segment elevation myocardial infarction (STEMI), acute non-ST-segment elevation myocardial infarction (NSTEMI), and unstable angina during the pandemic. The treatment of unstable angina with high-risk stratification is similar to that of NSTEMI. Therefore, in the questions related to unstable angina, we specified the condition of “unstable angina with low-moderate risk stratification”. The survey required approximately 25 minutes to complete.
All statistical analyses were performed using SPSS 24.0 (IBM Corp, Armonk, NY,
USA). Categorical variables are reported as the number and percentage. Continuous
variables are expressed as the mean
Of the 300 clinicians invited, 211 (70.3%) completed the survey. The data were collected from physicians located in 22 provinces in China. Among the survey respondents, 82.5% were employed in tertiary hospitals, 52.1% reported more than 10 years of clinical cardiology practice, 61.1% had a subspecialty in coronary heart disease, and 46.4% were engaged in the interventional treatment of coronary heart disease (Table 1).
| Characteristic | n (%) | |
| Years in practice (years) | ||
| 52 (24.6) | ||
| 6–10 | 49 (23.2) | |
| 11–20 | 85 (40.3) | |
| 25 (11.8) | ||
| Classification of employed hospital | ||
| Primary general hospital | 5 (2.4) | |
| Secondary general hospital | 15 (7.1) | |
| Tertiary general hospital | 174 (82.5) | |
| Cardiovascular hospital | 17 (8.1) | |
| Subspecialty (multiple choice) | ||
| Coronary heart disease | 129 (61.1) | |
| Arrhythmias | 107 (50.7) | |
| Congenital heart disease/structural heart disease | 22 (10.4) | |
| Heart failure | 62 (29.4) | |
| Hypertension | 70 (33.2) | |
| Dyslipidemia | 33 (15.6) | |
| Critical cardiovascular diseases | 55 (26.1) | |
| Cardiovascular diseases without detailed subspecialty | 53 (25.1) | |
| Other subspecialty | 12 (5.7) | |
| Subspecialty in interventional therapy (multiple choice) | ||
| Coronary artery intervention therapy | 98 (46.4) | |
| Electrophysiology | 85 (40.3) | |
| Cardiac device implantation | 76 (36.0) | |
| Interventional therapy for congenital heart disease | 18 (8.5) | |
| Interventional therapy for peripheral vascular diseases | 4 (1.9) | |
| Other interventional therapy | 3 (1.4) | |
| Not interventional physicians | 56 (26.5) | |
As shown in Fig. 1, 20.9% of the respondents stated that the province in which they worked reported more than 1000 new COVID-19 cases per day in the week before responding to the survey, and 16.6% worked in a city where more than 1000 new COVID-19 cases were reported per day in the week before the survey.
 Fig. 1.
Fig. 1.Severity of the COVID-19 pandemic in the respondents’ location. (A) Newly reported COVID-19 cases per day in the province of the respondents. (B) Newly reported COVID-19 cases per day in the city of the respondents.
A small proportion of respondents stated that there was little change in the numbers of inpatients and outpatients with ACS, and an even smaller proportion stated that there was an increase in the numbers of these patients. The majority of respondents stated that there was a reduction in the numbers of ACS inpatients and outpatients during the pandemic (Fig. 2). There were similar results to the question about the number of ACS patients who underwent coronary artery interventional therapy.
 Fig. 2.
Fig. 2.Effect of the COVID-19 pandemic on the numbers of ACS inpatients and outpatients. (A) Pandemic’s effect on the number of outpatients with ACS. (B) Pandemic’s effect on the number of inpatients with ACS. (C) Pandemic’s effect on the number of ACS patients who underwent coronary artery interventional therapy.
Only 63 (29.9%) of the respondents worked in hospitals that had dedicated catheter rooms for the interventional treatment of ACS patients who also had COVID-19; 148 (70.1%) did not have access to dedicated catheter rooms in which to treat ACS patients with COVID-19.
Only 9.9% of the respondents stated that the COVID-19 pandemic did not affect their STEMI treatment practices, whereas the majority believed that the pandemic had varying degrees of effect on STEMI treatment (Table 2).
| n (%) | ||
| Impact of COVID-19 pandemic on the treatment in STEMI | ||
| Almost no impact | 21 (9.9) | |
| Mild impact | 75 (35.5) | |
| Moderate impact | 79 (37.4) | |
| Serious impact | 36 (17.1) | |
| Impact of COVID-19 pandemic on the treatment in NSTEMI | ||
| Almost no impact | 24 (11.4) | |
| Mild impact | 74 (35.1) | |
| Moderate impact | 82 (38.9) | |
| Serious impact | 31 (14.7) | |
| Impact of COVID-19 pandemic on the treatment in unstable angina | ||
| Almost no impact | 24 (11.4) | |
| Mild impact | 75 (35.5) | |
| Moderate impact | 90 (42.6) | |
| Serious impact | 22 (10.4) | |
When asked “During the pandemic, what therapeutic strategies did you choose when a STEMI patient was within the reperfusion therapeutic time window but a COVID-19 test result was unavailable?”, nearly two-thirds (59.7%) of the respondents chose primary percutaneous coronary intervention (PCI), whereas 37.4% chose fibrinolytic therapy (Fig. 3A). A small proportion of respondents chose primary PCI or fibrinolytic therapy after the COVID-19 test result had become available, whereas 5.2% would transfer STEMI patients to other hospitals that had dedicated catheter rooms for COVID-19 patients.
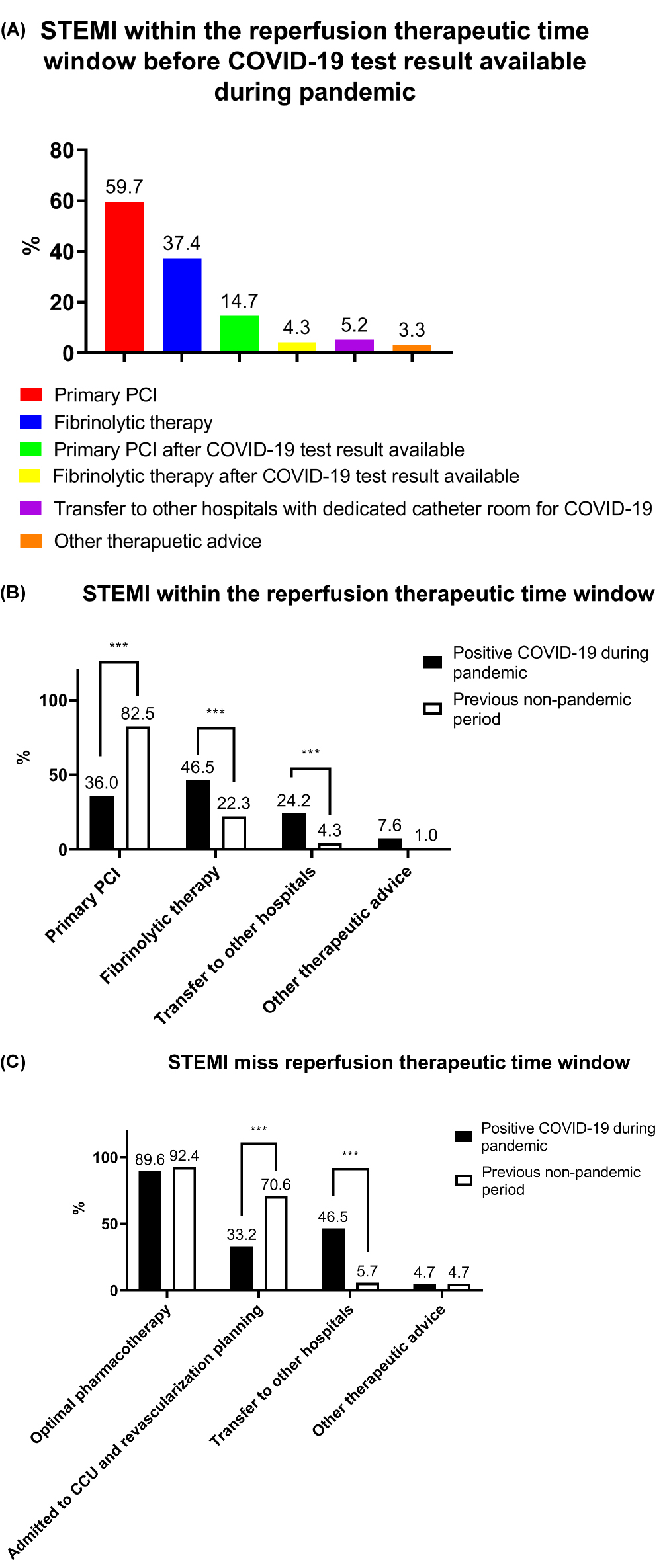 Fig. 3.
Fig. 3.Effect of the COVID-19 pandemic on STEMI clinical practice
patterns. (A) Respondents’ preferred reperfusion strategies for STEMI patients
who did not have an available COVID-19 test result. (B) Respondents’ preferred
reperfusion strategies for STEMI patients
within the reperfusion therapeutic time
window. (C) Respondents’ preferred treatment options for STEMI patients who had
missed the reperfusion therapeutic time window. PCI, percutaneous coronary
intervention; CCU, cardiac care unit; *** p
For STEMI patients who were within the reperfusion therapeutic time window and
were positive for COVID-19, 36.0%, 46.5%, and 24.2% of the respondents chose
primary PCI, fibrinolytic therapy, and the transfer of patients to another
hospital with a dedicated catheter room, respectively. These results were
significantly different from the response to a similar question and option set,
but under the assumption of the previous non-pandemic period (all p
For STEMI patients who missed the reperfusion therapeutic time window and had a
positive COVID-19 test result, 89.6%, 33.2%, and 46.5% of the respondents
chose optimal pharmacotherapy, admit to the cardiac care unit and
revascularization planning, and transfer to another hospital, respectively.
Significantly fewer respondents chose revascularization planning in this scenario
than in the period before the COVID-19 pandemic (p
Regarding the treatment of NSTEMI patients, 11.4% of the respondents stated that the COVID-19 pandemic had no effect on the treatment of NSTEMI, and the remainder thought the pandemic had varying degrees of effect (Table 2).
For NSTEMI patients with a positive COVID-19 test result, 90.5%, 33.7%, and
43.1% of the respondents chose optimal pharmacotherapy, revascularization
planning according to risk stratification, and transfer to another hospital with
a dedicated catheter room, respectively. The selection of revascularization
planning and transfer to another hospital was significantly different from that
in the non-pandemic period (all p
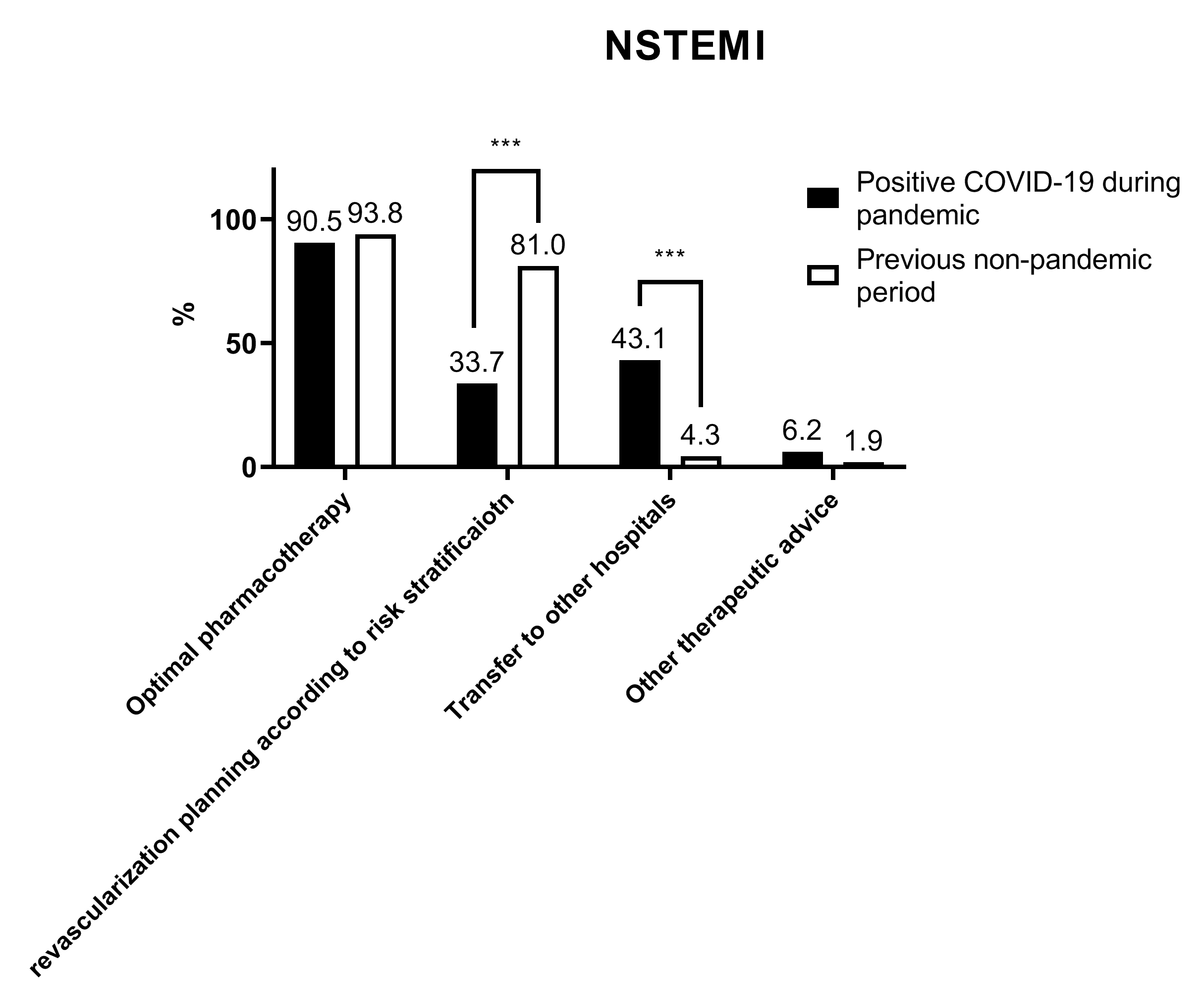 Fig. 4.
Fig. 4.Respondents’ preferred treatment for NSTEMI patients. *** p
A total of 88.6% of the respondents thought that the COVID-19 pandemic had varying degrees of effect on the treatment of unstable angina patients with low-moderate risk stratification (Table 2).
Regarding the treatment of unstable angina patients with low-moderate risk
stratification who were positive for COVID-19, only 17.1% of the respondents
chose the invasive strategy, whereas 57.4% preferred optimal pharmacotherapy and
to delay invasive procedures; 38.4% chose transfer to another hospital with a
dedicated catheter room. These results were significantly different from the
response to a similar question and option set, but under the assumption of the
previous non-pandemic period (all p
 Fig. 5.
Fig. 5.Respondents’ preferred treatment for unstable angina patients
with low-moderate risk stratification. *** p
As shown in Table 3, the selection of primary PCI and fibrinolytic therapy for
STEMI patients within the reperfusion therapeutic time window but without a
COVID-19 test result were significantly different among the participating
cardiologists who had different daily numbers of newly reported COVID-19 cases in
their cities (all p
| Daily number of newly reported COVID-19 cases in the cities of respondents | p-value | |||||
| 11–100 | 101–500 | 501–1000 | ||||
| Option of primary PCI for STEMI patient within the reperfusion therapeutic time window but a COVID-19 test result was unavailable, n (%) | 90 (61.2) | 15 (71.4) | 4 (100.0) | 3 (75.0) | 14 (40.0) | 0.039 |
| Option of primary PCI for STEMI patients within the reperfusion therapeutic time window and positive for COVID-19, n (%) | 59 (40.1) | 7 (33.3) | 2 (50.0) | 1 (25.0) | 7 (20.0) | 0.232 |
| Option of revascularization plan for STEMI patients who missed the reperfusion therapeutic time window and positive for COVID-19, n (%) | 55 (37.4) | 4 (19.0) | 2 (50.0) | 1 (25.0) | 8 (22.9) | 0.249 |
| Option of revascularization plan for NSTEMI patients and positive for COVID-19, n (%) | 55 (37.4) | 7 (33.3) | 0 (0.0) | 2 (50.0) | 7 (20.0) | 0.174 |
| Option of revascularization plan for unstable angina patients and positive for COVID-19, n (%) | 31 (21.1) | 3 (14.3) | 0 (0.0) | 0 (0.0) | 2 (5.7) | 0.157 |
| Option of fibrinolytic therapy for STEMI patient within the reperfusion therapeutic time window but a COVID-19 test result was unavailable, n (%) | 46 (31.3) | 6 (28.6) | 1 (25.0) | 2 (50.0) | 24 (68.6) | 0.001 |
| Option of fibrinolytic therapy for STEMI patients within the reperfusion therapeutic time window and positive for COVID-19, n (%) | 61 (41.5) | 7 (33.3) | 1 (25.0) | 2 (50.0) | 27 (77.1) | 0.002 |
The characteristics of the participating cardiologists, including classification
of employing hospital, years in cardiology practice, subspecialty, and
subspecialty in interventional therapy, had no impact on their selection of
interventional therapy and fibrinolytic therapy for ACS patients (all p
The COVID-19 pandemic is having a marked effect on clinical practices around the world. In this multicenter survey of cardiologists in China, most stated that the COVID-19 pandemic had varying degrees of effect on their ACS diagnosis and treatment practices. During the pandemic, only 29.86% of the respondents had dedicated catheter rooms in their hospitals for the interventional treatment of ACS patients. Compared with the treatment choices in the period before the COVID-19 pandemic, the respondents’ choice of interventional treatments for ACS during the pandemic was reduced.
More than 80% of the respondents stated that during the pandemic there had been a substantial reduction in the numbers of ACS inpatients, outpatients, and patients undergoing catheter interventional therapy for ACS. This may have been because some ACS patients were worried about contracting COVID-19, and some patients with mild symptoms may have chosen to take medicine at home instead of going to the hospital. COVID-19 directly affects the development of thrombotic coronary obstruction and can lead to myocardial infarction through several mechanisms, such as inducing an inflammatory storm, a hypercoagulable state, or thrombosis, or through viral infiltration of myocardial cells or other immunologic mechanisms [13, 14, 15, 16, 17]. Previous clinical studies have demonstrated that ACS morbidity and mortality have significantly increased during the COVID-19 pandemic [5, 6, 18, 19]. The early treatment of ACS, especially for acute myocardial infarction, considerably benefits a patient’s prognosis. During the pandemic, the early transfer, early diagnosis, and early therapeutic interventions for ACS patients have been enormously challenging.
Although the COVID-19 pandemic currently affects the entire world, ACS presents with high morbidity and mortality and therefore should not be ignored. Moreover, a close relationship exists between ACS deterioration and COVID-19 virus infection at the pathophysiological level [20]. Respiratory failure caused by COVID-19 will aggravate the insufficiency of oxygen supply to the myocardium, thereby triggering and worsening myocardial infarction. Another critical mechanism implicated in the association between COVID-19 and ACS is the pro-inflammatory state. The inflammatory storm caused by COVID-19 plays a crucial role in eliciting an inflammatory pattern that may trigger ACS. Thus, the incidence of ACS in COVID-19 cases is correspondingly increased [21, 22]. A recently published meta-analysis found that ST-segment elevation can present in patients with COVID-19 regardless of pre-existing obstructive coronary artery diseases (CAD). COVID-19 patients without pre-existing obstructive CAD had increased diffuse ST-segment elevation and diffuse left ventricular wall-motion abnormality [23]. Saririan M et al. [24] reported an international case series of patients with confirmed COVID-19 infection and suspected STEMI, and none of the patients had obstructive coronary disease upon coronary angiography. Post-mortem histology demonstrated focal myocardial ischemia in one case, but there was no evidence of atherothrombosis or myocarditis [24]. Therefore, the COVID-19 pandemic has increased the incidence and deterioration of ACS in people with or without a confirmed history of CAD.
In patients with COVID-19 infection, the development of myocardial injury may lead to circulatory dysfunction and systemic imbalance of the oxygen supply, which can lead to the patient’s deterioration. Barman HA et al. [25] demonstrated that the incidence of myocardial injury could be as high as 24.7% among hospitalized COVID-19 patients. Compared with COVID-19 patients without myocardial injury, those with cardiac injury had a higher mortality rate and increased frequencies of requiring the intensive care unit (ICU), developing acute kidney injury, and developing acute respiratory distress syndrome [25]. Patients with pre-existing chronic coronary syndrome (CCS) have a significantly increased probability of myocardial injury and in-hospital death compared with patients without previous CCS, and patients with myocardial injury have a significantly increased mortality compared with patients without previous CCS. COVID-19 patients with coronary heart disease have higher rates of complications, in-hospital mortality, and frequency of renal replacement therapy than those without coronary heart disease [26, 27].
Coagulation derangement and thromboembolism are the major determinants of cardiovascular event involvement in COVID-19 patients. Severe COVID-19 is also associated with increased proinflammatory cytokine concentrations, which subsequently elicit coagulation activation and thrombin generation. Post-mortem findings in patients with COVID-19 have found microvascular thrombotic deposits in small vessels of the lungs and other organs [28]. These micro-macro thromboses can lead to hypoxemia and progress to a more severe status [29]. The hypercoagulable state associated with COVID-19 potentially increases the risk of thromboembolic complications [28, 30]. Tang N et al. [31] performed a retrospective study in China that included 449 patients with severe COVID-19 infection. It demonstrated that the prophylactic application of heparin significantly reduced mortality in patients with COVID-19-associated coagulopathy, especially in patients with increased concentrations of D-dimer. Schiavone M et al. [32] also found that in-hospital heparin administration was associated with a better chance of survival to hospital discharge. However, patients who received pre-hospitalization oral anticoagulation appeared to have more frequently developed acute hypoxemic respiratory failure and had a higher mortality rate. The exact mechanisms underlying the role of anticoagulant treatment and heparin in COVID-19 require further exploration.
We also found a significant decrease in the use of coronary interventions for STEMI, NSTEMI, and unstable angina during the COVID-19 pandemic. There may be multiple reasons for this phenomenon. In most cities around the world, medical care for cardiovascular events is provided by general hospitals. Treating ACS patients who have COVID-19 poses a risk of disease transmission to other patients and the medical staff. Owing to the distribution of healthcare resources, not all hospitals are equipped with dedicated cardiac catheter rooms for COVID-19 patients, which is likely why 36.0% of the respondents choose primary PCI for COVID-19-positive STEMI patients who were within the reperfusion therapeutic time window, whereas 46.5% choose fibrinolytic therapy for these patients. In the early stage of myocardial infarction, thrombolytic therapy is an important alternative to primary PCI. Fibrinolysis using urokinase, streptokinase, or alteplase remains the primary reperfusion strategy for STEMI in many developing countries [33, 34]. Therefore, while constrained by the COVID-19 pandemic, medical institutions without dedicated cardiac catheter rooms can prioritize fibrinolytic therapy for COVID-19-positive STEMI patients.
Early coronary interventional therapy, especially primary PCI for acute myocardial infarction, considerably improves ACS patients’ prognosis. Although the survey results showed that the proportion of cardiologists who choose fibrinolytic therapy for STEMI increased during the pandemic, patients will probably have a recurrent coronary event after thrombolytic therapy; thus, selective PCI is still needed for most STEMI patients who have previously undergone fibrinolytic therapy [35, 36]. The current expert consensus is that primary PCI remains the standard of care for STEMI patients during the COVID-19 pandemic at hospitals equipped with dedicated catheter rooms in which this treatment can be provided promptly [12]. From this perspective, the treatment of ACS during the pandemic has depended on not only the clinical competence of the physician but also the availability of medical resources. Countries and regions with sufficient resources can allocate dedicated catheter rooms for COVID-19-positive ACS patients.
This study had several limitations. First, this was a multicenter clinician survey conducted in China, and differences in healthcare resource distributions and the COVID-19 pandemic severity among regions may have led to biased responses. Second, the clinical conditions of ACS patients often change. Thus, clinicians cannot always adhere to the diagnostic and therapeutic guidelines; rather, they must customize individualized treatment plans for different conditions. For this reason, the responses stated by the clinicians in the questionnaire may not completely reflect the actual management practices. Furthermore, the COVID-19 vaccines have played an important role in mitigating the pandemic and may profoundly impact the management of ACS patients. The main objective of this study was to investigate the perceptions of cardiologists regarding how the COVID-19 pandemic has affected the clinical practice patterns for ACS, and thus we did not collect information on vaccines in this survey. Additionally, the study findings need to be confirmed by further clinical studies.
The ongoing COVID-19 pandemic has had a profound effect on ACS clinical practice patterns. During the pandemic, the application of coronary interventional therapy decreased, whereas pharmacotherapy, especially fibrinolytic therapy for COVID-19-positive STEMI patients, was often stated as the best option by the participating cardiologists.
FH drafted the initial manuscript. MHZ and LHZ contributed to the study design and manuscript review. WSC, JRG, ZPD, EPL, LSS, XFH, XLX, DZZ, and GFH contributed to the clinical data collection and analysis. AHL and JFH provided support and assistance in data extraction. YY and JP approved the final manuscript as submitted.
The study was approved by the Ethics Committee of Renji Hospital affiliated with the School of Medicine, Shanghai Jiao Tong University (KY2022-096-A).
We thank all of the cardiologists who participated in this multicenter clinician survey and devoted their effort and time to it during such a challenging pandemic.
This work was supported by the Shanghai Municipal Key Clinical Specialty (shclczdzk06204).
The author declares no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
