- Academic Editors
Background: The aim of this study was to determine the rates of
diagnostic and operative complications of gynecological laparoscopic procedures,
and identify risk factors for the occurrence of these complications.
Methods: This retrospective study included 680 women who underwent
gynecological laparoscopy for benign indications between 01 July, 2015, and 01
September, 2020, at Kanuni Sultan Süleyman Training and Research Hospital.
They were classified into diagnostic and operative laparoscopy groups.
Laparoscopic entry and operative complications were thoroughly analyzed. Mean
age, mean parity, history of previous surgery, operative time, amount of blood
loss, complication rates, and length of postoperative hospital stay were
compared. Results: There were significant differences between groups in
terms of mean age, parity, history of previous surgery, duration of surgery,
hemoglobin drop, length of surgery, and length of hospital stay (p
The term endoscopy is a combination of the Greek words “endo” and “skopein” and means “examination of the cavities in the human body”. Clinicians have always desired to clarify their diagnoses by looking at the cavities in the human body (endoscopy) along with palpation, auscultation, and percussion. These comprise the main aspects of physical examination [1]. Laparoscopy allows viewing of the organs in the abdominal cavity by placing a thin telescope through the abdominal wall. It is a minimally invasive surgical technique that allows access to the abdominal cavity and pelvis while avoiding large incisions in the skin.
The laparoscopy technique was initially used mainly for diagnostic purposes and a few simple surgical procedures, such as tubal ligation and tissue biopsy. Recently it has become an excellent alternative to open surgical procedures and is commonly preferred [2].
Laparoscopic surgery has a shorter recovery time, shorter hospital stay, less blood loss, faster return to daily activity, work, and social life, better cosmetic results, and lower complication rates than laparotomy. Studies have shown that general complication rates vary between 4%–41.21% [3, 4, 5]. Laparoscopic operations are a minimally invasive technique and have become the gold standard in many surgical procedures. However, it should be known that the complications that may occur in laparoscopic surgical procedures are considerable. Understanding this, all surgeons must be alert to complications and must be highly effective and competent in early diagnosis and treatment [6].
This study aimed to determine the diagnostic and operative complication rates in gynecological laparoscopic procedures as well as the risk factors that cause these complications.
In this retrospective study, we included patients who underwent laparoscopic surgery for benign gynecological reasons at Kanuni Sultan Süleyman Training and Research Hospital between 01 July 2015 and 01 September 2020. We divided the participants into diagnostic and operative laparoscopic surgery groups. Although the number of patients who underwent diagnostic laparoscopy (DL) in the first cohort was 97, 95 were potentially suitable for the study. Although the number of cases who underwent operative laparoscopy (OL) was 596, 585 were eligible to be included in the study. The surgical technique’s complexity was considered when creating the cohorts. Demographic and clinical characteristics such as age, parity, previous medical and surgical history, duration of surgery, amount of blood loss, surgery complication rates, and postoperative hospital stay were recorded and compared between the groups.
The management protocol (preparation and operative technique) was the same for the two groups. Patients who presented with primary or secondary infertility were evaluated for tubal patency in the diagnostic laparoscopy group along with tubal ligation, minor adhesiolysis, and treatment for early-stage endometriosis. Conservative treatment for ectopic pregnancy, salpingectomy, cystectomy, oophorectomy, pelvic abscess drainage, hysterectomy, myomectomy, and moderate and deep endometriosis were included in the operative group. Wang et al. [7] first used this grouping system to analyze the major complications of postoperative and diagnostic laparoscopy for gynecologic disease.
Following a 10 mm vertical incision in the umbilicus, the Verres needle (KARL STORZ SE & Co. KG, Tuttlingen, Baden-Württemberg, Germany) was inserted into the abdomen after the anterior abdominal wall was suspended upwards using underwear clamps. Fourteen mmHg pressure was utilized to create pneumoperitoneum. The abdominal cavity was entered with a 10 mm trocar followed by a 10 mm zero-degree telescope (KARL STORZ SE & Co. KG, Tuttlingen, Baden-Württemberg, Germany). Second and third incisions were performed in the avascular lower part of the abdomen, 3 cm medial to the anterior superior iliac spine, followed by insertion of 5 mm trocars. If additional access was required, a third 5 mm trocar was inserted on the patient’s left side at 12–13 cm above the umbilicus [8]. Instruments used included a zero-degree telescope, advanced bipolar electrocoagulation (Ligasure, Covidien, MA, USA), conventional bipolar electrocoagulation (KARL STORZ SE & Co. KG, Tuttlingen, Baden-Württemberg, Germany), monopolar hook (KARL STORZ SE & Co. KG, Tuttlingen, Baden-Württemberg, Germany), Cohen cannula (KARL STORZ SE & Co. KG, Tuttlingen, Baden-Württemberg, Germany) and a Rumi II uterine manipulator (Cooper Surgical Inc., Trumbull, CT, USA). The same surgical team completed all procedures.
The night prior to surgery, all patients received enemas for mechanical colon cleansing. All procedures were performed under general anesthesia in the dorsal lithotomy position. One gram of cefazolin was administered to all patients 1 hour before and the six hours after the operation. All patients had a Foley catheter and an orogastric tube. We discharged patients who had spontaneous urination and defecation after surgery and had no significant complaints. Operative time was determined from the first umbilical incision to the removal of the primary trocar. Length of hospital stay was determined from the day of the procedure to the day of discharge. All patients were followed for one month after surgery.
The study comprised female patients between the ages of 18 and 75 who underwent gynecological laparoscopy for benign reasons (uterine myoma, adenomyosis, cervical intraepithelial neoplasia, endometrial polyp, para ovarian cyst, benign ovarian cyst, endometrial hyperplasia, atrophic endometrium, endometrioma) and who had complete records.
Patients who underwent gynecological laparoscopy and had cancer discovered in the specimen as well as those with incomplete records were excluded from the study.
SPSS 24.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical
calculations in the study. Chi-square or Fisher’s exact tests was used to examine
categorical variables presented as frequencies and percentages. The Mann-Whitney
or Student t-test was used as appropriate for continuous variables and
presented as mean
The study comprised 680 patients between the ages of 18 and 75 years. The
demographic and clinical information of the participants included in the study
are presented in Table 1. The mean ages of patients who underwent diagnostic
laparoscopy (DL) and operative laparoscopy (OL) were 26.2
| Characteristics | Diagnostic laparoscopy | Operative laparoscopy | p |
| n = 95 (13.9%) | n = 585 (86.1%) | ||
| Age (y) |
26.2 |
37.3 |
0.01* |
| BMI (kg/m |
25.7 |
26.2 |
NS |
| Parity |
0.2 |
1.84 |
0.001* |
| Previous medical and surgical history | (n) % | (n) % | |
| Cesarean section | 7 (7.4%) | 89 (15.2%) | 0.001* |
| Laparoscopy | 4 (4.2%) | 23 (3.9%) | NS |
| Other surgeries | 2 (2.1%) | 17 (2.9%) | NS |
| Endometriosis | 4 (4.2%) | 24 (4.1%) | NS |
| Pelvic inflammatory disease | 4 (4.2%) | 26 (4.4%) | NS |
| Duration of surgery (min) | 20 |
92.2 |
0.001* |
| Pre-and postoperative mean hemoglobin drop (g/dL) | 0.32 |
1.44 |
0.001* |
| Length of hospital stay (d) | 1.2 |
2.4 |
0.01* |
The operative indications are shown in Table 2. The most common indications were hysterectomy, tubal patency, cystectomy, and salpingectomy. Details regarding the complications of the laparoscopic procedure are presented in Table 3. A total of 28 (4.11 %) complications occurred; conversion from laparoscopy to laparotomy occurred in 5 (0.73%) patients, bladder perforation in 4 (0.58%), and need for blood transfusion in 4 (0.58%) patients. Of 28 (4.11%) complications, 8 (1.17%) were encountered during abdominal entry of the Veress needle or trocar at the beginning of the laparoscopic procedure. Fig. 1 demonstrates how a ROC analysis was used to determine the cut-off for complications. Complications dramatically increased, particularly in gynecological laparoscopic procedures lasting longer than 110 minutes, with a 68.5% sensitivity and 69.1% specificity (Table 4).
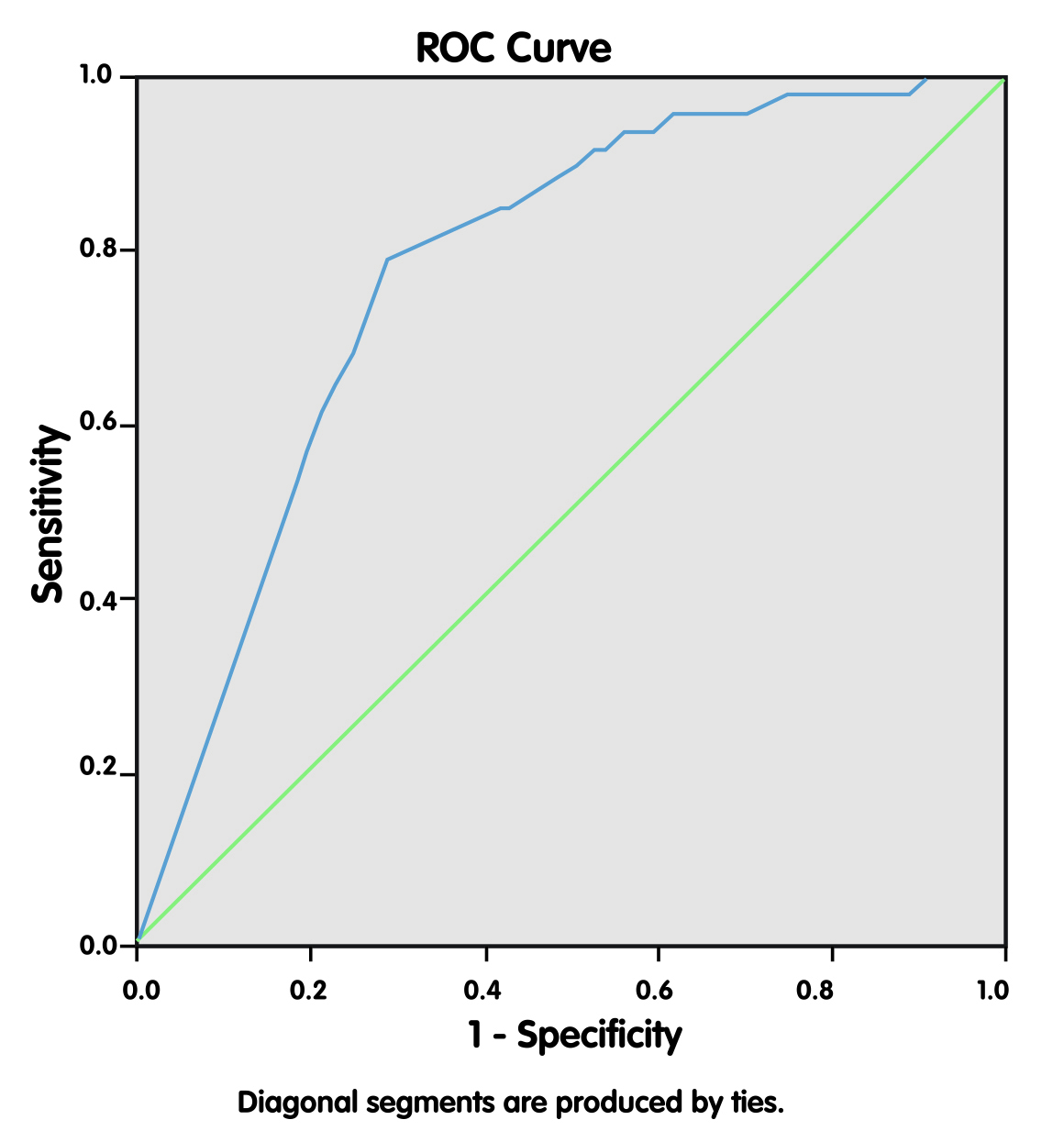 Fig. 1.
Fig. 1.Receiver operating characteristic (ROC) curve showing the relationship between operation times and complication rates.
| Indications | n = 680 (100%) |
| Tubal patency | 95 (13.9%) |
| Tubal ligation | 76 (11.2%) |
| Minor adhesiolysis | 20 (2.9%) |
| Early-stage endometriosis | 17 (2.5%) |
| Cystectomy | 89 (13.1%) |
| Conservative treatment of ectopic pregnancy | 40 (5.8%) |
| Salpingectomy | 75 (11.1%) |
| Oophorectomy | 39 (5.7%) |
| Pelvic abscess | 14 (2.1%) |
| Moderate endometriosis | 17 (2.5%) |
| Laparoscopy-assisted vaginal hysterectomy | 26 (3.8%) |
| Hysterectomy | 160 (23.5%) |
| Deep endometriosis | 5 (0.7%) |
| Characteristics | n = 28 | Mode of laparoscopy | Associated pelvic condition and history of surgery | Indication for laparoscopy |
| Subcutaneous emphysema | 2 | Diagnostic laparosvopy 1 case | No risc | Tubal patency |
| Operative laparoscopy 1 case | Cystectomy | |||
| Preperitoneal emphysema | 2 | Operative laparoscopy 2 cases | Adhesions 2 cases | Moderate endometrioma |
| Omentum damage | 2 | Operative laparoscopy 2 cases | History of surgery 2 cases | Adenomyosis |
| Inferior epigastric vessel injury | 2 | Operative laparoscopy 2 cases | No risc | Leiomyoma |
| Bleeding (requiring blood transfusion) | 4 | Operative laparoscopy 4 cases | History of surgery 1 cases | Leiomyoma |
| Bladder injury | 4 | Operative laparoscopy 4 cases | History of cesarean 3 cases, | Leiomyoma |
| History of pelvic surgery 1 case | ||||
| Conversion to Laparotomy | 5 | Operative laparoscopy 5 cases | Adhesions 2 cases, | Leiomyoma |
| Transfusion required bleeding 3 cases (hemorrhage) | ||||
| Postoperative ileus | 1 | Operative laparoscopy 1case | Adhesions 1 case | Leiomyoma |
| Bowel injury | 1 | Operative laparoscopy 1 case | Adhesions 1 case | Adenomyosis |
| Gynecological laparoscopic interventions | AUC (95% CI) | Cut-off value | p-value | Sensitivity | Specificity |
| Complication | 0.725 (0.672–0.777) | 110 minutes | 0.0001 | 68.5% | 69.1% |
AUC, area under the curve; 95% CI, 95% confidence interval.
A direct relationship was observed between the duration of surgery and the complication rates. This study revealed that problems dramatically increased, particularly in gynecological laparoscopic procedures lasting longer than 110 minutes. However, regardless of the type of laparoscopic procedure, significant complications had arisen before the procedure or during the insertion of the abdominal trocars. The initial stage of laparoscopy, such as pneumoperitoneum formation and placement of trocars, should be performed carefully. Furthermore, even in the simplest forms of laparoscopic surgery, complications may occur before the operation begins or during the abdominal insertion of trocars.
Although laparoscopic surgery is becoming common in gynecology, complications are frequently noted. It has been reported that laparoscopic gynecological surgeries intraoperative and postoperative complication rates were 5.6% and 6.5%, respectively [9]. The complication rate in operative laparoscopy cases ranges from 0.2% to 10.3% [10].
In this study, of the 28 complications that occurred, 5 (0.73%) developed during the insertion of the Verres needle and the primary trocar. This rate is compatible with the rate of 0.05%–2.8% published in the literature [11]. An inferior epigastric vessel injury occurred in 3 (0.44%) cases during conversion to laparotomy, indicating the importance of paying attention to the placement of accessory trocars. Uterine perforation occurred in 1 (0.14%) patient during the placement of a uterine manipulator. However, the operation was completed with no other problems. Complications related to abdominal entry are rare; however, the associated mortality rate is 13% [12]. The complication rate was significantly higher in the advanced laparoscopy group (n = 17 (9.88%)), with 24 of the 28 complications (85.71%) occurring in the major and advanced surgery groups. The advanced laparoscopy group had a complication rate of ~10, ~6, and ~4 times higher than the diagnostic, minor, and major laparoscopy groups.
Furthermore, 3 patients underwent conversion from laparoscopy to laparotomy in the advanced laparoscopy group. History of a previous abdominal surgery increases the conversion rate from laparoscopy to laparotomy [13]. The main associated concerns are the injuries at the entrance to the abdomen and complications caused by adhesiolysis [14]. The rate of diffuse subcutaneous emphysema is 2.3% as reported in the literature [15]. This condition occurs owing to the inability of the needle to reach the abdominal cavity when inserted horizontally into the abdomen. The 0.29% rate noted in our study could be attributed to increased surgical experience, and the emphysema regressed spontaneously within a day without treatment.
Multiple studies have reported that the bladder is the most frequently injured visceral organ in laparoscopy [16, 17, 18], ranging between 0.03% to 0.24% of cases. Prolonged use of the monopolar energy source, improper placement of the uterine manipulator, or trocar entry from the suprapubic region may result in bladder injury [19]. In our study, bladder injury occurred during the dissection of the anterior peritoneum from the bladder during a total laparoscopic hysterectomy in 3 patients with a previous history of abdominal surgery. All 3 complications were managed at the time of occurrence. While laparoscopic bladder repair was performed in 2 patients, laparotomy was performed in 1 of the patients as the defect was unsuitable for laparoscopic repair. Bladder catheterization was continued for ten days for all 3 patients. No vesicovaginal or ureterovaginal fistulae were observed during the postoperative follow-up period.
It has been reported that a higher level of experience is associated with lower complication rates [20]. One report has 214 complications noted in 3724 laparoscopic procedures. The complication rate was 0.31% for diagnostic laparoscopy and 3.2% for sterilization surgeries, with an overall complication rate of 5.8% [21]. It was reported that 34 of 3572 patients who underwent laparoscopy between 1996 and 2003 were converted to laparotomy (0.95%). The complication rate was significantly higher in the advanced laparoscopy group (1.88%), with a total complication rate of 4.88% [22]. It was reported that 7 (1.39%) of 503 patients who underwent laparoscopy between 2003 and 2006 were converted to laparotomy, and the overall complication rate was 3.37% [23]. Compared with laparotomy, laparoscopy has a lower overall complication rate [24]. The overall complication rate in gynecological laparoscopy was 1.96% [25].
In our study, of the 680 laparoscopic procedures, conversion to laparotomy was required in 3 (0.44%) cases due to bleeding and bladder perforation, and our overall complication rate was 4.11%. Therefore, prevention and early diagnosis are essential during laparoscopic procedures [26].
The laparoscopic approach is widely preferred in early-stage endometrial cancer [27]. Laparoscopic cervical cancer trials clearly showed that minimally invasive radical hysterectomy is associated with worse survival [28]. It has been understood that the 5-year survival rates for early-stage endometrial cancers are no different from total abdominal hysterectomy when factors such as the necessity of lymph node dissection are considered [29]. Unfortunately, laparoscopic hysterectomy has worse outcomes than open hysterectomy in cervical cancer, regardless of stage [30]. Metastases at port entry sites have been reported in oncological cases undergoing laparoscopic surgery [31]. Laparoscopic operations of myomas with malignant potential yield poor results even if morcellation is not applied. Therefore, laparoscopic morcellation of myomas with uncertain diagnoses is not recommended [32].
During laparoscopic surgery, complications may occur before the operation begins or during the abdominal insertion of trocars.
The laparoscopic complication rates vary according to the difficulty and complexity of the procedure. There is a direct relationship between procedure difficulty and complication rates. More studies are needed to add to the results obtained from this single-center study.
The information used in this study was carefully gathered. A major weakness of this study is the short follow-up duration. The investigation was retrospectively conducted in a single tertiary care center in Turkey which impacts the generalizability of the study, as well as the capacity to identify causal correlations.
A direct relationship was observed between the duration of surgery and the complication rates. This study found that problems dramatically increased, particularly in gynecological laparoscopic procedures lasting longer than 110 minutes. However, regardless of the type of laparoscopic procedure, significant complications had arisen before the procedure or during the insertion of the abdominal trocar.
Due to patient privacy, information about all participants is not publicly published. All data is stored in our archive with the permission of the patients. If there are justified reasons, patient data can be shared by the corresponding author within ethical rules.
AB, OU designed the study, collected the data, used statistical calculations to process the data, interpreted the results, and made discussions based on the literature. Both authors contributed to editorial changes in the manuscript. Both have approved the final version of the manuscript to be published. Both authors read and approved the final manuscript.
We started the study after receiving ethical approval from the ethics committee of Istanbul Kanuni Sultan Süleyman Training and Research Hospital with the decision numbered KAEK/2021.11.314 at its meeting on 26.11.2021. We strictly complied with the Declaration of Helsinki at all stages of the study. Since the study design was retrospective, we did not obtain informed consent from the patients. Each patient gave written informed consent before surgical treatment.
The authors thank Ejear English editing service for the premium English editing.
This research received no external funding.
The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
