Academic Editor: Michael H. Dahan
Background: The typical treatment of the International Federation of Gynecology and Obstetrics 2018 stage IB2 cervical cancer is radical hysterectomy. With the trend of delayed childbearing, the importance of fertility sparing in the treatment of women with cervical cancer has drawn attention. Case: We report a case of stage IB2 cervical cancer treated by neoadjuvant chemotherapy with quick cisplatin-VP 16 followed by robotic radical trachelectomy. Conclusions: Neoadjuvant chemotherapy (NACT) using platinum-based therapy with cisplatin and trachelectomy performed through the vagina or abdominal approach was used in most previous cases. We successfully performed NACT with quick cisplatin-VP 16, followed by robotic radical trachelectomy in stage 1B2 cervical cancer. Further studies are needed to accumulate cases and outcomes of fertility-preserving treatment techniques.
Cervical cancer is the fourth most common malignancy in women worldwide [1], and peak incidence is between ages 35 and 45 years [2]. With the trend of delayed childbearing, the importance of fertility sparing in the treatment of women with cervical cancer has drawn attention.
Although the typical treatment of the International Federation of Gynecology and
Obstetrics (FIGO) 2018 stage IB2 cervical cancer is radical hysterectomy,
neoadjuvant chemotherapy (NACT) can be performed for downstaging, followed by
radical trachelectomy for fertility preservation. We report a case of cervical
cancer stage IB2 successfully treated by a combination of quick cisplatin (90
mg/m
A 29-year-old nulliparous single woman presented to a local clinic for national health checkup. She was taking immunosuppressants for Crohn’s disease. She reported intermittent vaginal bleeding for a few months but did not seek medical advice. Her Papanicolaou test revealed atypical squamous cells that cannot be excluded as a high-grade squamous intraepithelial lesion (HSIL). She was referred to the Gynecologic Department of Saint Vincent’s Hospital in January 2021.
Per speculum, she was found to have a 3
 Fig. 1.
Fig. 1.Per speculum examination of vagina showing the tumor mass (before the neoadjuvant chemotherapy).
A biopsy of the tumor showed moderately differentiated squamous cell carcinoma. On immunohistochemistry, the tumor cells were positive for P16, and Ki-67 was seen in 70%. Human papilloma virus (HPV) 16, 43, and 70 were detected on real-time PCR. She had not received HPV vaccination.
Extensive radiological investigations were performed in an attempt to clarify
the penetration range and possible metastasis of the tumor. Pelvic magnetic
resonance imaging (MRI) revealed the diameter of the tumor to be 3.7
 Fig. 2.
Fig. 2.Axial T1-weighted fat suppressed magnetic resonance imaging of the pelvis; before (left) and after (right) the NACT showing near complete resolution of the lesion.
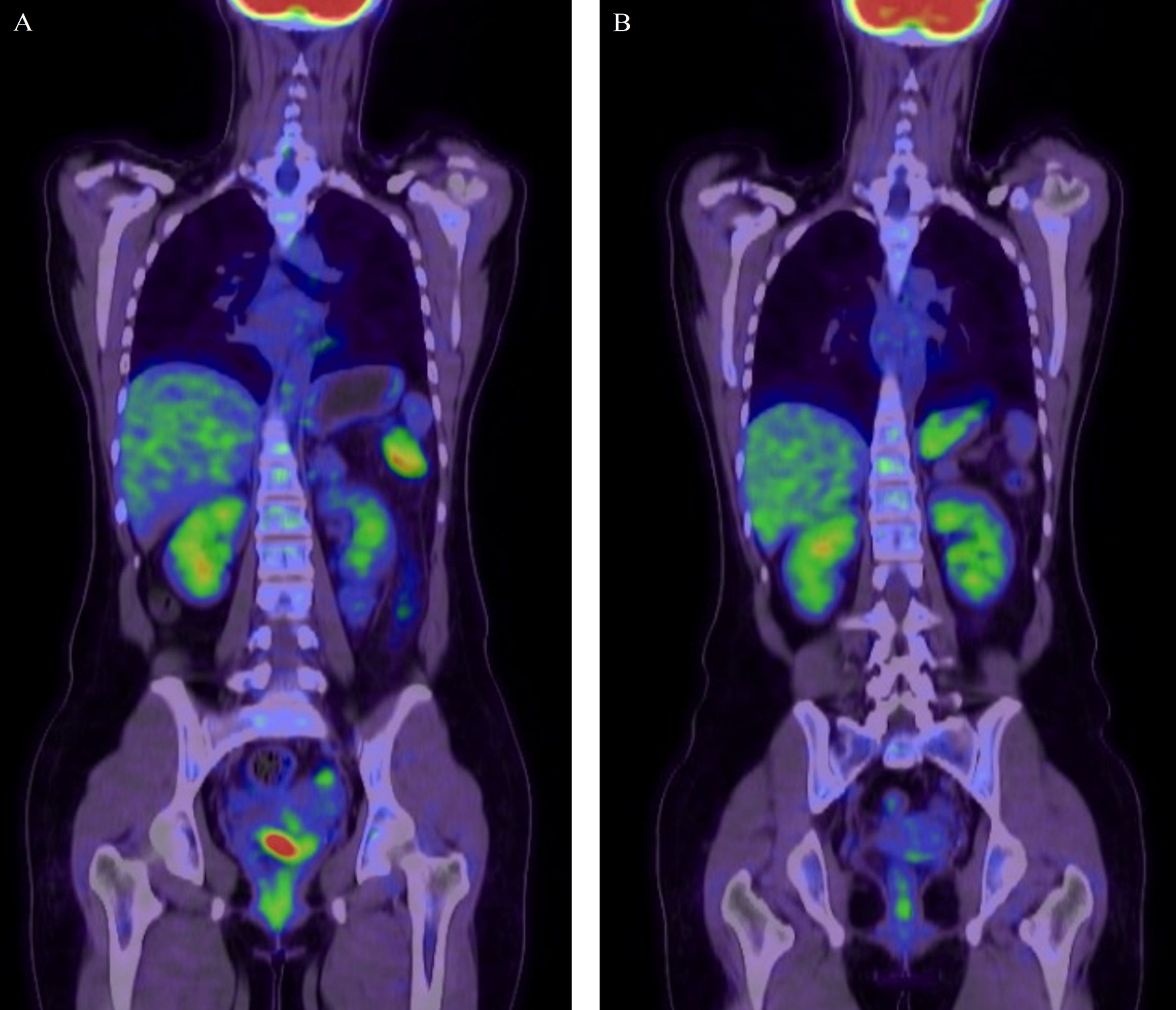 Fig. 3.
Fig. 3.Coronal fused fluorodeoxyglucose (FDG) positron emission
tomography (PET)/computed tomography (CT) images. Before (left) and after
(right) the NACT showing near complete resolution of the lesion. The focal FDG
uptake of uterine cervix significantly decreased in intensity (SUV max: 11.34
Based on these clinical findings and investigations, the patient was diagnosed
with cervical cancer, stage FIGO IB2. The patient desired preservation of her
fertility, and primary neoadjuvant chemotherapy followed by radical robotic
trachelectomy was decided after a multidisciplinary team meeting. Among the
regimens allowed by the Korean insurance system, it was decided to use the quick
cisplatin-vp 16 regimen because it has relatively tolerable ovarian toxicity. She
received four cycles of NACT in total, and response evaluation was performed
after every two administrations. The first two NACT were cisplatin 60 mg/m
She then underwent robotic-assisted laparoscopic radical trachelectomy and sentinel lymph node biopsy which has been recently reported to be reasonable in early stage cervical cancer [3]. The stiff trendelenburg down position was changed to supine position and vaginal cuff resection and repair was performed with vaginal approach. Irrigation of vagina and pelvic cavity was performed rigorously before repairing the vaginal stump. The use of uterine manipulator presents a theoretical possibility of tumor injuries and peritoneal seeding. Therefore, we used Bora’s uteirne manipulation instrument (BUMI) (Sejong medical, South Korea), to reduce the incidence of peritoneal seeding from broken tumor fragments [4]. The results from the LACC trial has questioned the safety of minimally invasive surgery (MIS) for early stage cervical cancer [5]. However, the LACC trial mainly explored conventional laparoscopy. The safety of robot assisted surgery in early cervical cancer is not yet established.
Five intraoperative frozen sections of the right internal iliac node, endocervical cut margin, parametrium, and vaginal wall were obtained, and no specimen revealed malignancy. Permanent pathological findings moderately differentiated squamous cell carcinoma confined to the transformation zone, with a width of 7 mm and a depth of 2.5 mm invasion (Fig. 4).
 Fig. 4.
Fig. 4.Microscopic histology (
Depending on a tumor’s stage and histopathology, several fertility-sparing modalities are practiced today, and one of the available options is NACT, followed by radical trachelectomy. Many studies have found this technique to be a safe, feasible, alternative approach to radical hysterectomy or concurrent chemoradiation therapy (CCRT) in properly selected early-stage patients seeking fertility preservation, with equal disease-free and overall survival rates [6, 7, 8].
NACT using platinum-based therapy with cisplatin and trachelectomy performed through the vagina or abdominal approach was used in most previous cases. We successfully performed NACT with quick cisplatin-VP 16, followed by robotic radical trachelectomy in stage 1B2 cervical cancer. Further studies are needed to accumulate cases and outcomes of fertility-preserving treatment techniques.
The design of study and Responsible Surgeon was done by JY. The reference collection and manuscript preparation was done by AL, SK, SO and JL. Description on pathological findings was prepared by SI and radiological findings and significance were described by HAK.
Ethics committee approval was exempted due to the nature of the study (VC21ZISI0146).
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
