Academic Editor: Sandro Gerli
Background: Immigrants face various problems in accessing healthcare
because of lacking medical insurance. This study retrospectively evaluated the
effect of insurance on the prenatal care and the obstetric outcomes of immigrants
in South Korea. The main objective was to compare the obstetric complications
between uninsured and insured immigrants, and the secondary objective was to
compare the prenatal care and maternal nutrition during pregnancy.
Methods: Using data from the hospital records, we compared the perinatal
outcomes of insured and uninsured women who delivered at Buchoen St. Mary’s
Hospital between 2010 and 2020, including the sociodemographic data, prenatal
care, obstetric outcomes, and maternal nutrition. The association between
insurance status and the various perinatal outcomes of immigrants was assessed
using multivariate logistic regression, adjusting for potential confounding
variables. Results: In total, 320 immigrant women were included, and 52
(16%) were uninsured. Uninsured immigrants had fewer numbers and a later
initiation of prenatal care visits (7.75
South Korea has been experiencing significant international immigration every year. The number of immigrants and long-term residents has nearly doubled from 1,395,077 in 2010 to 2,524,626 in 2019 [1]. Among them, fertile women aged between 20 and 44 years represented 58% in 2019 [2]. The number of married female immigrants with Korean husbands living in South Korea has also been increasing and is expected to increase even further because of the specific nature of the South Korean population structure [3]. Because of the rapid growth of international marriages in Korea, the live birth rate for international marriages per total birth rate increased from 4.3% in 2010 to 5.9% in 2019 [1]. Given that a vast majority of immigrants in their childbearing years moved to Korea for marriage or work, it is necessary to plan and execute obstetric care services to meet the needs of this group.
In South Korea, universal health insurance is provided to almost all Koreans, and most prenatal care and delivery procedures are covered by insurance. Immigrants can receive insurance benefits when they acquire Korean nationality, marry a Korean, or secure a legal job in Korea. Their insurance benefits are similar to those of the native Koreans. In contrast, illegal immigrants cannot acquire medical insurance. As such, they are required to pay for their prenatal care and delivery.
Immigrant women are often at risk of poor pregnancy outcomes [4, 5], and multiple factors are implicated, with insurance status being one of the most important factors. However, the evidence on the pregnancy outcomes of immigrant women according to insurance status is still unclear and controversial. Many immigrants and migrant women in Canada and the United States receive less than the recommended level of care due to their lack of public health care coverage [6]. In addition, uninsured migrant women in the United States who lack prenatal care have almost a four-fold risk of having low birth weight babies and a seven-fold risk for preterm deliveries [6]. Several Canadian studies have also reported that uninsured women have poorer perinatal outcomes in general [7, 8]. However, other report has shown no significant differences with respect to low birth weight rates, preterm delivery rates, and overall maternal complications [9]. Until now, most of the research has been conducted on immigrants in America or Europe and not in South Korea or other Asian countries, such as Singapore, Taiwan, and Japan, experiencing a dramatic increase in the influx of immigrants from developing countries [10, 11]. In addition, few studies have investigated the difference in the maternal nutrition status of insured and uninsured immigrants.
Therefore, the main objective of this study was to investigate whether obstetric complications were similar between uninsured immigrants and insured immigrants in Korea. The secondary objective was to assess whether perinatal care and maternal nutrition were similar between the two groups.
This was a retrospective cohort study involving pregnant immigrant women who gave birth between January 2010 and December 2020 at Bucheon St. Mary’s Hospital. Data was extracted from the electronic medical records system. Participants were identified through perinatal databases, and their medical records were reviewed. Their data were analyzed for demographic information, prenatal care, obstetric complications, and maternal nutrition. This study was approved by the Institutional Review Board of the Catholic University of Korea (HC21RISI0018), which waived the need for written informed consent from the participants because this was a retrospective study, and the data were analyzed anonymously.
All immigrants who gave birth during the study period were included in this study. We excluded those who did not deliver in this hospital or had an abortion (delivery before 20 weeks of gestation). Health insurance status was easily identified using the hospital’s electronic medical codes. The study’s insured population was defined as the patients who acquired health insurance before delivery. These included women who married Korean men or workers, temporary workers, or visitors with legal visas. The uninsured population comprised illegal immigrants or foreigners who refused to pay for the regular insurance contributions. Bucheon St. Mary’s Hospital is a university community tertiary hospital located in a metropolitan area where many foreigners and immigrants reside. We developed a charity program for medical help and financial support for pregnant immigrants. Most of the uninsured population was asked if they were willing to receive financial assistance based on their financial status after receiving counseling.
Afterward, we analyzed the basic characteristics of the pregnant immigrants. The
total number of deliveries and the number of deliveries by immigrants was
analyzed by year. The number of uninsured and insured immigrants was also
analyzed by year. We compared the demographic, clinical, socioeconomic data,
obstetric complications, prenatal care, and maternal nutrition of the uninsured
and insured immigrants. Obstetric complications included intrauterine growth
restriction (IUGR; birth weight
The adequacy of prenatal care was estimated based on the number of antenatal visits, the Kessner index (KI) [3, 12], and gestational age at the first prenatal care visit. The KI includes information on the start of prenatal care, the total number of consultations, and the length of pregnancy. Adequacy was evaluated using three levels (adequate, intermediate, and inadequate). To be rated adequate on the KI, prenatal care must have started before gestational week 14 with at least nine prenatal care visits for a normal-length pregnancy. Prenatal care is categorized as inadequate if the first visit occurred after gestational week 28 or if there were fewer than four prenatal visits. For the other combinations that did not fall into either of these categories, prenatal care was considered intermediate.
Maternal nutrition was evaluated according to maternal body mass index (BMI)
before pregnancy, adequacy of weight gain during pregnancy, and anemia before
delivery. In 2009, the Institute of Medicine published revised gestational weight
gain guidelines based on pre-pregnancy BMI ranges for underweight, normal weight,
overweight, and obese women. Adequate gestational weight gain was defined as
follows: 12.5–18 kg for underweight women, 11.5–16 kg for women with normal
weight, 7–11.5 kg for overweight women, and 5–9 kg for obese women [13].
Maternal anemia was defined as Hb level
After extracting the data, a data quality management process was executed in a standardized manner, according to the data table specifications. To increase data reliability, the relevant data were manually reviewed and compared with the original data. When a direct chart review was required, only the responsible researchers could access the data.
All statistical analyses were performed using SPSS version 20 (SPSS Inc.,
Chicago, IL, USA). The chi-square test or Fisher’s exact test was used for
categorical data, and Student’s t-test or the Wilcoxon rank-sum test was
used for continuous variables. The results are presented as mean
A total of 320 pregnant immigrants were included in the study. Among them, 52 (16%) were uninsured, while 268 (84%) had medical insurance. Forty-five (14%) women received financial support, with 43 of them being uninsured. Vietnamese immigrants comprised the highest number of immigrants who received financial support (N = 27, 60%).
The number of total deliveries in this hospital barely changed from 316 in 2010 to 325 in 2020 (Fig. 1A). However, the number of deliveries by immigrants increased by almost 10 times (from 6 in 2010 to 57 in 2020). In effect, the proportion of the deliveries of immigrants to the total deliveries increased abruptly during the study period. The number of insured immigrants and uninsured immigrants was compared by year (Fig. 1B), and both showed increasing trends. However, the ratio of uninsured to insured immigrants also increased.
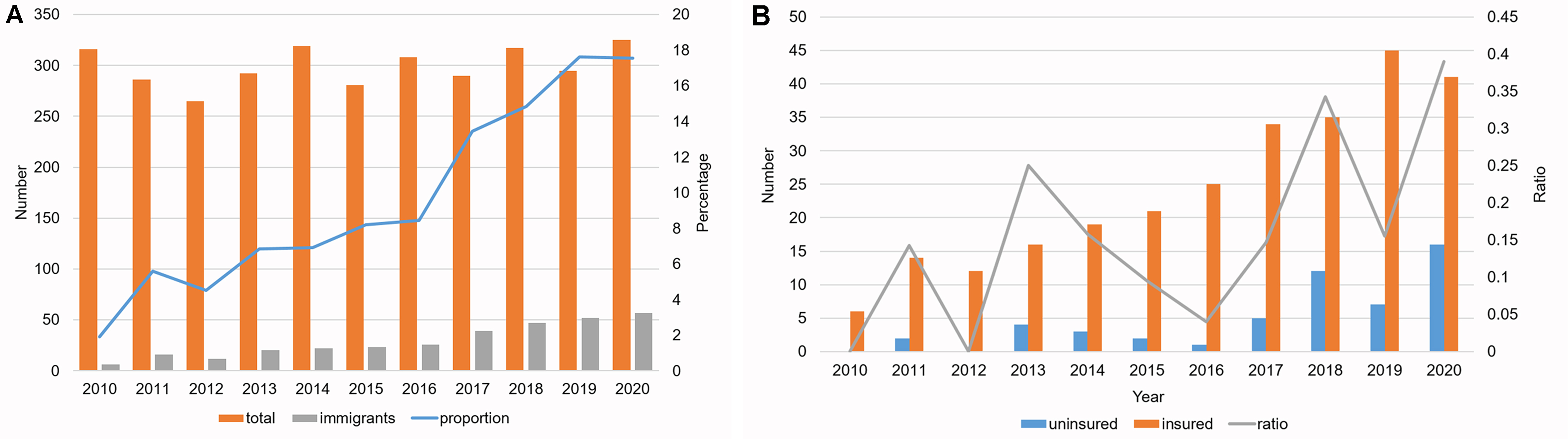 Fig. 1.
Fig. 1.Prevalence of pregnant immigrant women. (A) and their insurance status during 2010 to 2020. (B) Data are expressed as percent or means.
The number of insured immigrants and uninsured immigrants was also compared by nationality (Fig. 2). The number of deliveries by immigrants from China, Vietnam, and Philippine were comprised of 85% of total deliveries by total immigrants. Chinese immigrants accounted for the highest number of immigrants and the highest percentage of insured immigrants (56%). Vietnam immigrants were the second largest number of immigrants and the largest number of immigrants without insurance (54%).
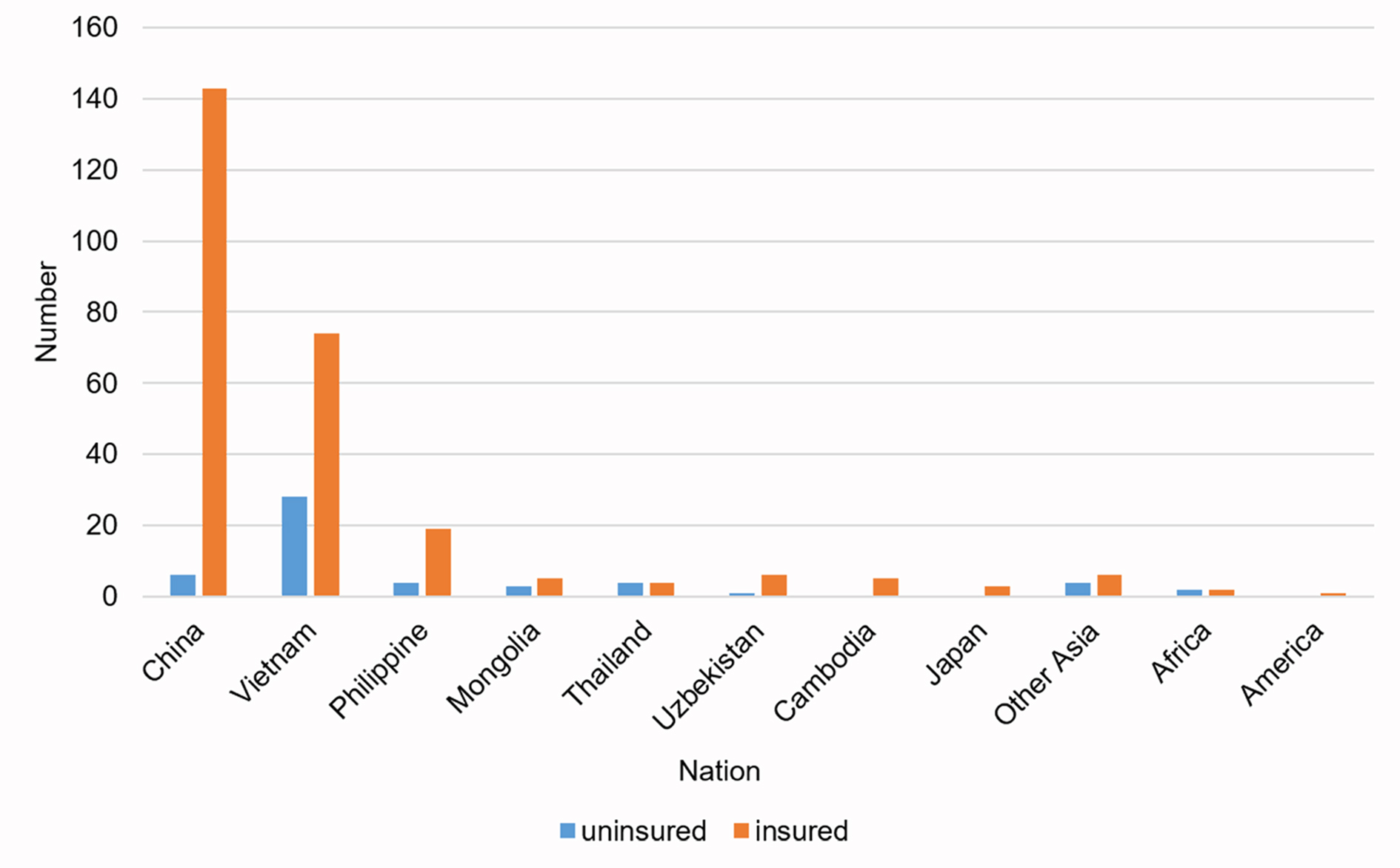 Fig. 2.
Fig. 2.Distribution of the participants according to nationality and insurance status.
The study participants’ baseline characteristics and prenatal care are reported
in Table 1, with a comparison between insured and uninsured immigrants. In terms
of the baseline characteristics, the uninsured immigrants were associated with a
lower percentage of primiparous women (48.1% vs. 62.7%, p = 0.049),
having Korean husbands (0 vs. 50.4%, p
| Uninsured (n = 52) | Insured (n = 268) | p-value | ||
| Sociodemographic characteristics | ||||
| Age at delivery, y | 29.23 |
29.79 |
0.526 | |
| Primiparous | 25 (48.10) | 168 (62.7) | 0.049 | |
| GA at delivery, wks | 38.06 |
37.64 |
0.36 | |
| Educational level | 0.13 | |||
| None to primary school | 2 (3.85) | 8 (3.00) | ||
| Middle to high school | 15 (28.8) | 100 (37.3) | ||
| University or higher | 7 (13.5) | 54 (20.1) | ||
| Partner characteristics | ||||
| No partner | 3 (5.8) | 4 (1.5) | 0.417 | |
| Korean husband | 0 (0) | 135 (50.4) | ||
| Korean language skills | 0.005 | |||
| None | 31 (59.6) | 96 (35.8) | ||
| Low | 2 (3.9) | 9 (3.4) | ||
| High | 19 (36.5) | 163 (60.8) | ||
| Employed state | 2 (3.8) | 10 (3.73) | 0.907 | |
| Smoker | 1 (1.9) | 0 (0) | 0.023 | |
| Financial support | 43 (82.7) | 2 (0.7) | ||
| Prenatal care | ||||
| No. of prenatal care visits | 7.75 |
12.45 |
||
| Adequate | 14 (26.9) | 171 (63.8) | ||
| Intermediate | 9 (17.3) | 49 (18.3) | ||
| Inadequate | 29 (55.8) | 48 (17.9) | ||
| First visit of prenatal care | ||||
| 1st trimester | 19 (36.5) | 179 (66.8) | ||
| 2nd trimester | 1 (1.92) | 14 (5.22) | ||
| 3rd trimester or no antenatal care | 14 (26.9) | 11 (4.10) | ||
| GA, gestational age; No, number. Values are expressed as mean | ||||
Table 2 shows the obstetric outcomes and the maternal nutrition of the
immigrants. Comparing the mode of delivery between the uninsured and insured
immigrants, emergency cesarean section and cesarean section without medical
indication were not statistically different. In the vaginal delivery group,
perineum laceration and operative vaginal delivery were significantly higher
among the uninsured immigrants. However, composite obstetric complications did
not differ significantly between the two groups. Maternal nutrition was evaluated
according to the proportion of maternal anemia and maternal weight gain. Maternal
anemia and pre-pregnancy obesity were not significantly different between the two
groups. The uninsured immigrants gained more weight than the insured immigrants
during pregnancy (14.1
| Uninsured (n = 52) | Insured (n = 268) | p-value | |||
| Obstetric outcome | |||||
| Mode of delivery | |||||
| Cesarean section | 25 (48.1) | 147 (54.9) | 0.37 | ||
| Planned cesarean section | 9 (36.0) | 46 (31.3) | 0.641 | ||
| Emergency cesarean section | 11 (44.0) | 79 (53.7) | 0.367 | ||
| Cesarean section without medical indication | 3 (12.0) | 21 (14.3) | 0.76 | ||
| Vaginal delivery | 27 (51.9) | 121 (45.1) | 0.37 | ||
| Operative vaginal delivery | 8 (29.6) | 14 (11.6) | 0.017 | ||
| Male fetus | 24 (46.2) | 151 (56.3) | 0.177 | ||
| Birth weight, kg | 3.13 |
2.99 |
0.185 | ||
| IUGR (Birth weight |
19 (7.10) | 2 (3.80) | 0.387 | ||
| Macrosomia (birth weight |
0 (0.00) | 12 (4.50) | 0.12 | ||
| 1-minute Apgar score |
10 (19.2) | 55 (20.5) | 0.832 | ||
| 5-minute Apgar score |
2 (3.8) | 15 (5.6) | 0.606 | ||
| Preterm delivery ( |
5 (9.60) | 53 (19.80) | 0.082 | ||
| Stillbirth | 1 (1.90) | 5 (1.90) | 0.978 | ||
| Congenital malformation | 1 (1.90) | 6 (2.20) | 0.887 | ||
| Neonatal resuscitation | 8 (15.40) | 23 (8.60) | 0.129 | ||
| Gestational diabetes | 1 (1.90) | 24 (9.00) | 0.084 | ||
| Preeclampsia | 1 (1.90) | 16 (6.00) | 0.234 | ||
| Placenta abruption | 1 (1.90) | 7 (2.60) | 0.771 | ||
| Perineum laceration | 3 (5.80) | 2 (0.70) | 0.008 | ||
| Postpartum bleeding | 3 (5.80) | 8 (3.00) | 0.313 | ||
| PRC transfusion | 6 (11.50) | 17 (6.30) | 0.184 | ||
| Placenta previa | 3 (5.80) | 9 (3.40) | 0.402 | ||
| 32 (61.5) | 175 (65.3) | 0.604 | |||
| Maternal nutrition | |||||
| Nausea and poor oral intake | 2 (11.1) | 40 (37.8) | 0.135 | ||
| Maternal anemia | 5 (9.6) | 32 (11.9) | 0.631 | ||
| Pre-pregnancy BMI | 0.1 | ||||
| Underweight | 4 (7.7) | 46 (17.2) | |||
| Normal weight | 38 (73.1) | 179 (66.8) | |||
| Overweight | 10 (19.2) | 33 (12.3) | |||
| Obese | 0 (0) | 10 (3.7) | |||
| Weight gain during pregnancy | 14.08 |
12.39 |
0.029 | ||
| 0.062 | |||||
| Undernutrition | 14 (26.9) | 110 (41.0) | |||
| Adequate | 18 (34.6) | 93 (34.7) | |||
| Overnutrition | 20 (38.5) | 65 (24.3) | |||
| GA, gestational age; IUGR, intrauterine growth restriction; No, number. Values are expressed as mean | |||||
Table 3 shows the crude and adjusted associations between insurance status and
perinatal outcomes. The uninsured immigrants were more likely to have less than
adequate prenatal care (OR, 4.79; 95% CI, 2.47–9.27; p
| Unadjusted OR | Adjusted OR | ||||||
| OR | (95% CI) | p value | OR | (95% CI) | p value | ||
| Less-than-adequate Kessener index (KI) | Insured | 1.00 | 1.00 | ||||
| Uninsured | 4.79 | 2.47–9.27 | 5.18 | 2.54–10.53 | |||
| Perineum laceration | Insured | 1.00 | 1.00 | ||||
| Uninsured | 8.14 | 1.33–50.00 | 5.77 | 0.87–38.15 | 0.069 | ||
| CI, confidence interval; OR, odds ratio. Values are expressed as odds ratio (95% confidence interval). | |||||||
The univariate analysis showed that the uninsured immigrants were associated with less prenatal care, increased risk of perineum laceration, and more weight gain than the insured immigrants. However, after adjusting for confounding factors, the absence of insurance was independently associated with inadequate prenatal care. In contrast to the primary hypothesis, there were no significant differences in obstetric complications and maternal nutrition.
Similar to previous studies, our study showed that insurance status was affected by ethnicity and nationality as women from a specific country can benefit more from medical care than other groups. In one study from Canada, the uninsured group included a greater percentage of Caribbean women, whereas the insured group included a greater percentage of South Asians [9]. Our study also showed that most immigrants were from China, and most (96%) of the Chinese women had insurance. Previous studies conducted in Korea and America found that women from China were the most likely to participate in medical services, such as regular health screening [14, 15, 16]. We assumed that immigrants with a well-organized social network would receive more medical benefits by the exchanging information and methods regarding medical care. The study of favorable birth outcomes of Latin mothers in America (Latina paradox) argued that social support networks could mitigate the adverse effects of poverty on birth outcomes [17]. According to a previous study, immigrants from China and Vietnam had the largest social network in South Korea [18]. We assumed that their large social network could explain the fact that the Chinese were the most insured, and the Vietnamese were the most financially supported.
Similar to previous studies, our study also showed that uninsured women had less frequent prenatal care and late initiation of prenatal care. More than half of the uninsured immigrants received inadequate prenatal care in Canada, and 6.5% received no prenatal care at all [2]. European data also showed that a lack of health insurance was an important risk factor for inadequate prenatal care [19]. Financial and socio-cultural barriers could explain the inequalities. Interestingly, most of the uninsured women received inadequate prenatal care despite receiving financial assistance. Therefore, we assumed that even after resolving the financial barriers, this trend might persist unless the social or cultural barriers are not removed. In another study in Taiwan, although more than 90% of immigrants were enrolled in the universal health insurance system, nearly one-third of them still had difficulty accessing medical services [20]. There are multiple social or cultural barriers that may serve as obstacles. In our study, uninsured immigrants were less likely to have Korean husbands and excellent Korean language skills, resulting in a lack of information on accessing medical services. In addition, since most of those who were uninsured were illegal immigrants, some explained that the fear of being deported may have led to suboptimal prenatal care [21]. Future research and government policies should be conducted to understand the socio-cultural barriers faced by uninsured immigrants and explore methods to reduce them. Educational interventions targeting general practices can be a solution, which has been proven to increase participation in cervical cancer screening among immigrants [22].
Many studies have shown that inappropriate prenatal care can increase poor obstetric outcomes [6]. We hypothesized that the uninsured immigrants would have poor obstetric outcomes due to improper prenatal care. However, contrary to our hypothesis, we found no difference in complications between the uninsured and insured groups during pregnancy. Different studies conducted in different countries have reported mixed results [17], and the reasons for the mixed evidence on obstetric outcomes in immigrant women are unclear. However, we can assume that there were various confounding variables in the relationship between immigrants and obstetric complications. Some reports argued that immigrants had poor obstetric outcomes, while others stated that immigrant women had better outcomes because they were younger and had healthier lifestyles, in comparison with non-immigrant women [17]. This suggests that various socioeconomic and cultural factors could play important roles as confounding variables in determining obstetric outcomes. It may also be related to the immigrants’ ethnicities and nationalities. Immigrants in Europe and Americans comprised numerous Africans, but those in South Korea were mainly from China and Southeast Asia. The prevalence of obstetric complications and various sociodemographic factors, such as obesity and maternal age, that could affect obstetric complications may vary according to ethnicity. Financial support to the uninsured immigrants in this study may be another reason for the similar obstetric outcomes. In the study of a charity providing medical assistance to around 500 undocumented pregnant immigrants in need, they found that social assistance partially improved their prenatal outcome compared to uninsured immigrants [23]. We assumed that the uninsured immigrants in this study also had improved perinatal outcomes due to the financial assistance.
This study had several limitations. First, the study was limited by its small sample size. The small sample size and low prevalence of some complications resulted in a wide 95% CI in the multivariate analysis. As such, the results of this study were not representative of the whole of South Korea or other Asian countries, though it could be applied to large cosmopolitan areas where many immigrants reside. Second, the study was a retrospective study, and some data were missing. Third, the socioeconomic data collected were based on self-report, which could not be validated. Finally, this study did not include data on some potential confounders, such as length of residency in Korea and family income level, which could be associated with perinatal outcomes. The failure to adjust to these possible confounders might have affected our findings.
Despite these limitations, our study had several strengths. This study was the first to evaluate the effect of insurance on prenatal care and obstetric outcomes in South Korea and Asia. In addition, we evaluated maternal nutritional status based on insurance status for the first time.
This study showed that the uninsured immigrants received inadequate prenatal care, but this did not result in more obstetric complications. Future research should increase the sample size and focus on the effect of insurance on perinatal outcomes by controlling for other dependent factors, such as the degree of acculturation and length of stay in the host country. In addition, government policies should be implemented to lessen the disparity and inequality in the prenatal care of immigrants.
YSJ—data collection, manuscript writing; JSU—project development, manuscript writing; KEL—data curation, methodology; SJK—data management, manuscript review; JES—study design, data analysis, manuscript writing. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
This study was approved by the Institutional Review Board of the Catholic University of Korea (HC21RISI0018), which waived the need for written informed consent from the participants because this was a retrospective study, and the data were analyzed anonymously.
We would like to express our gratitude to all those who helped us during the writing of this manuscript.
This research received no external funding.
The authors declare no conflict of interest.
