Academic Editors: Alessandra Andrisani and Loris Marin
Background: Uterine smooth muscle tumors of uncertain malignant potential (STUMPs) are a rare tumor that represent a diagnostic challenge to both clinicians and pathologists. Hysterectomy is considered the definitive treatment in women who don’t desire to conceive anymore; while myomectomy is suggested in young women who desire to preserve their fertility. The aim of this review is to evaluate the reproductive outcomes in patients submitted to fertility sparing treatment and with a diagnosis of STUMP at the definitive pathological evaluation. Methods: We searched among electronic databases from inception of them through January 2022. The research was conducted using meshes created by the combination of relevant heading term, key words, and word variants for: “uterine smooth muscle tumor of uncertain malignant potential”, “fertility”, “pregnancy”. Results: Seven retrospective studies including 80 women desirous of conceiving after a diagnosis of STUMP were included in this systematic review. Among these, 33 (41.25%) women got pregnant at least once and we recorded a total number of pregnancies of thirty-nine. Almost all deliveries were performed by caesarean section. Two (6.1%) relapses were diagnosed. Patients were submitted to hysterectomy and STUMP was confirmed as the final pathological diagnosis. The median follow-up in patients who delivered live babies was 61 months after surgery. At the last follow-up, all patients were alive without evidence of disease. Conclusions: This review shows that pregnacy seems to be possible and safe after the diagnosis of STUMP. These women should undergo rigorous follow-up and consider hysterectomy after completion of their reproductive plan. This review could be a useful tool for the counseling and the management of women with STUMP who desire to keep their fertility.
Uterine smooth muscle tumors are subdivided into leiomyomas, benign lesions, and
leiomyosarcomas, malignant tumors, according to three histopathological features
proposed by Stanford in 1994: mitotic count, cytologic atypia, and tumor cell
necrosis [1]. Uterine smooth muscle tumors of uncertain malignant potential
(STUMPs) are a unclearly defined subcategory of uterine smooth muscle tumors. The
term “uterine smooth muscle tumors of uncertain malignant potential” was coined
by Kempson et al. [2] in 1973. It was used to define a group of
clinically malignant smooth-muscle tumors not yet distinguished from sarcomas
[2]. The 2014 World Health Organization (WHO) classification system has defined a
STUMP as “a smooth muscle tumors with features that preclude an unequivocal
diagnosis of leiomyosarcoma, although it does not fulfill the criteria for
leiomyoma, or its variants, and raises concern that the neoplasm may behave in a
malignant fashion and only the outcome will confirm its benign or malignant
nature” [3]. The histological parameters proposed are (one of these): (I) tumor
necrosis in atypical leiomyoma, (II) necrosis of uncertain type with
This review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) [8].
Electronic research of all related studies until July 2022 from inception was performed by two authors MA and CM. Research on Pubmed, Web of Science, and Scopus was carried out using the following keywords: “uterine smooth muscle tumor of uncertain malignant potential”, “fertility”, “pregnancy”. All extracted abstracts were independently reviewed by the two authors. The agreement on potential relevance was achieved by consensus of the authors. After the first selection, the researchers reviewed the full-text copies of selected articles and separately extracted relevant data regarding study characteristics and outcomes. All bibliographies were screened to find additional eligible studies. SC and GV checked the data extracted. Systematic reviews, meta-analyses, and original articles were included in the present review. Inclusion criteria were all English language publications reporting on fertility outcomes after diagnosis of STUMP in patients who underwent a fertility sparing surgery.
Studies evaluated as not in line with the aim of the study, case reports, non-English language articles were excluded. The histologic criteria used for the classification of uterine smooth muscle neoplasms were in accordance with WHO classification [3].
The electronic database research provided a total of 110 studies. Of whom, 103 studies were not included while seven studies were considered eligible for the analysis. Fig. 1 reported the study selection flow-chart.
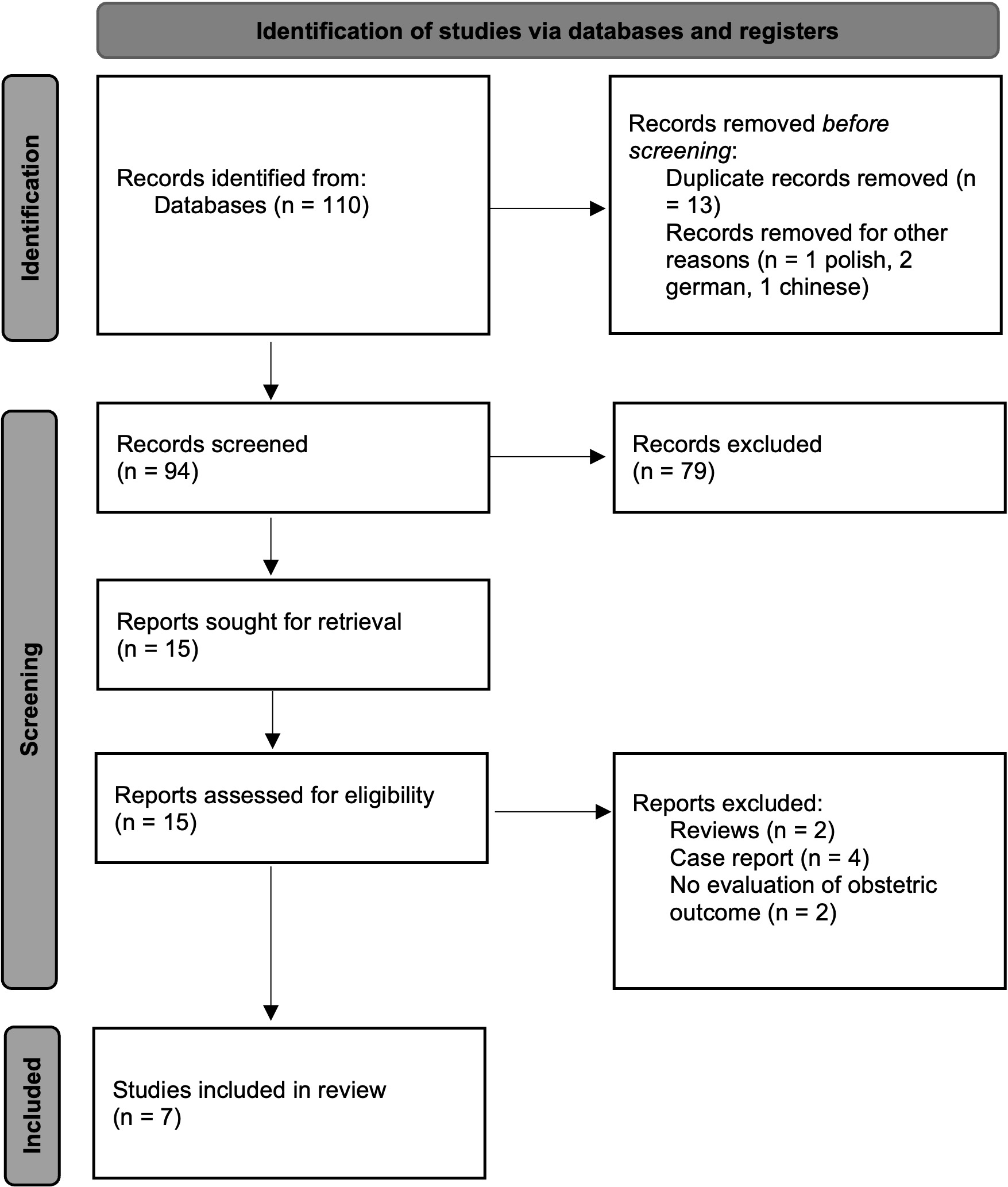 Fig. 1.
Fig. 1.Study selection flow diagram (in accordance with PRISMA 2020 flow diagram) Outcomes Measurement.
The primary objective was to assess the fertility outcomes after diagnosis of a STUMP in patients who underwent a fertility sparing surgery. The secondary objectives were to evaluate the characteristics of surgery and of patients who were desirous of conceiving after the diagnosis of STUMP and the recurrence rate of the disease among patients who became pregnant.
The collected data were presented in its clinical and demographic characteristics using descriptive statistics methods. Qualitative variables were presented as frequencies and percentages. Quantitative variables were summarized as mean and median.
A total of 110 titles were extracted using the above-mentioned keywords; then, we removed 13 duplicate records and 4 studies not in English language. After the first electronic database investigation 15 studies were extracted by the end of first revision and finally, a total of seven studies were identified as eligible following matched revision (Prisma Flow Diagram, Fig. 1), including 80 cases. All the studies were retrospective. The studies were published between 2018 and 2021.
In the 15 studies selected, a total of 280 patients had a diagnosis of STUMP, including 130 women who underwent hysterectomy (46.4%) (Table 1, Ref. [9, 10, 11, 12, 13, 14, 15]; Fig. 2). 80 (53%) of 150 women submitted to myomectomy with a final pathologic diagnosis of STUMP were desirous of conceiving. In all cases, the diagnosis of STUMP was made with the histological examination, following the criteria of the WHO classification [3]. Table 1 shows the characteristics of the included studies. The median age at surgery was 31 (range: 28–36) years. Of these, 33 (41.25%) women achieved at least one pregnancy. Median time interval from operation to pregnancy was 19 (range: 12–21.5) months; this information was not available in three studies. The total amount of pregnancies was thirty-nine. Two miscarriages were reported. Five women had ongoing pregnancy at the time of the last follow-up. Among the women who got pregnant, myomectomy was performed by three different approaches: laparoscopically in 9 cases, laparotomically in 19 cases and through hysteroscopy in two patients. In 3 cases this information was not reported.
| Study | Study design | Total pts in the study (n) | Pts submitted to FSS (n) | Pts submitted to FSS and with desire of conceive (n) | Pts who had pregnancy (n) | Median age at surgery (yrs) | Median time intererval from operation to pregnancy (mos) | Live birth (n) | Recurrence in pts who had pregnancy (n) | Median follw-up (pts who delivered live baby) (mos) |
| Ha, 2018 [13] | Retrospective study | 19 | 7 | 5 | 4 | 31.5 | 21.5 | 3 | 0 | 61 |
| Şahin, 2019 [11] | Retrospective study | 57 | 27 | 10 | 7 | 30 | n.r. | 7 | 2 | n.r. |
| Karataşlı, 2019 [14] | Retrospective study | 28 | 3 | 3 | 1 | 34 | 12 | 1 | 0 | 44 |
| Huo, 2020 [9] | Retrospective study | 67 | 38 | 35 | 7 | 29 | 20 | 7 | 0 | 45 |
| Shim, 2020 [10] | Retrospective study | 62 | 48 | 19 | 10 | 31 | n.r. | 10 | 0 | n.r. |
| Zhang, 2021 [15] | Retrospective study | 31 | 21 | 6 | 2 | 28 | 18 | 2 | 0 | 62.5 |
| Ning, 2021 [12] | Retrospective study | 16 | 6 | 2 | 2 | 36 | n.r. | 2 | 0 | 74.5 |
| TOTAL | 280 | 150 | 80 | 33 | 31 | 19 | 32 | 2 | 61 | |
| n, number; pts, patients; FSS, fertility sparing surgery; Yrs, years; Mos, months; n.r., not reported. | ||||||||||
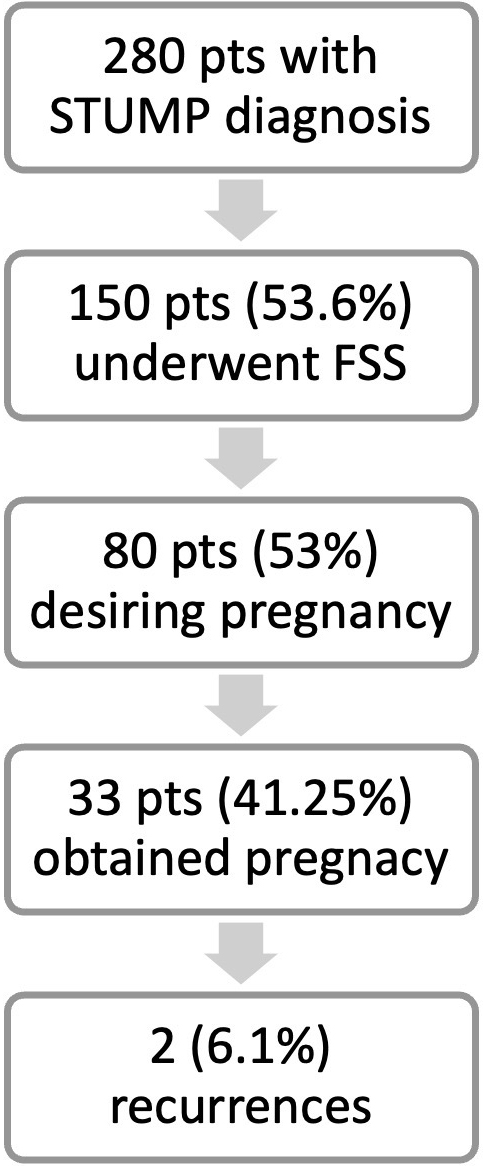 Fig. 2.
Fig. 2.Summary of results. n, number; pts, patients; FSS, fertility sparing surgery.
Eleven pregnancies have been obtained through assisted reproductive technologies: 10 by in vitro fertilization and one by intrauterine insemination.
All deliveries were performed by caesarean section except for one. In this last case the woman, who had lastly a vaginal birth without any complication, underwent a hysteroscopic myomectomy.
Three patients were submitted to total hysterectomy with bilateral salpingo-oophorectomy at the time of the cesarean section in order to minimize the risk of relapse [9]. One woman, who satisfied her wish of maternal desire, was submitted to hysterectomy due to leiomyoma and adenomyosis afterwards [10].
Two (6.1%) relapses were recorded among patients who became pregnant; one woman underwent previous abdominal myomectomy and the other a previous hysteroscopic myomectomy. Both were submitted to total hysterectomy and STUMP was confirmed as the final pathologic diagnosis. One relapse occurred as intramural tumor and the other as submucosal tumor [11]. No cases of recurrence as sarcoma have been recorded.
The median follow-up in patients who delivered live babies was 61 (range: 44–74.5) months after surgery. At the last follow-up, all patients were alive without evidence of disease.
In the current review, we summarized the reproductive outcomes of patients diagnosed with STUMP and submitted to fertility sparing treatment.
About 0.01% of women submitted to surgery for a presumed diagnosis of uterine leiomyoma have an incidental diagnosis of STUMP at finally pathological evaluation [16]. It is most frequently diagnosed in premenopause, at an average age of 44 years, with a range from 20 to 75 years [7], therefore also in women desiring fertility.
In the literature, there are not large number of studies with STUMPs and, consequently, the clinical behavior of these tumors still needs to be clarified. They represent a diagnostic challenge to both clinicians and pathologists. Women with STUMP have signs and symptoms like those of uterine leiomyomas and leiomyosarcomas, i.e., pelvic pain, pelvic mass, abnormal uterine bleeding, compression of adjacent organs and secondary anemia, infertility, dysmenorrhea, and abnormal vaginal discharge [17, 18, 19]. About 45% of cases are asymptomatic and the uterine mass is diagnosed during a routine gynaecological examination [20].
Due to the lack of specific symptoms and preoperative diagnostic methods, STUMP is diagnosed postoperatively according to histological findings and to Stanford criteria of atypia, mitotic index, and type of necrosis. It is diagnosed when the tumor has any unusual combinations of these 3 characteristics but does not satisfy the criteria for leiomyosarcoma [21]. Due to the STUMP rarity and its challenging diagnosis, a review made by a pathologist highly skilled in the field of soft tissues gynaecological neoplasms is mandatory.
Surgery represents the standard therapy. Total hysterectomy by vaginal, laparotomic, laparoscopic or robotic approach is the gold standard definitive treatment if fertility is completed, whereas myomectomy is considered an acceptable treatment option for women who still desire offspring. Treatment planning for STUMP suffers from the inability to make a preoperative diagnosis, therefore, in case of incidental finding of STUMP during myomectomy and no desire for offspring, hysterectomy should be proposed. As in the case of other gynaecological malignancies, when considering a conservative management approach, the characteristics of the patient should be evaluated to select the therapeutic approach that perfectly fits for the patients [22]. Myomectomy does not appear to be associated with an increased risk of recurrence [10, 11, 23, 12]. In case of minimally invasive surgery, morcellation must be avoided to prevent the risk of diffuse peritoneal implants [7]. No information on possible morcellation was reported in the recorded cases performed laparoscopically in our review. Although a widespread consensus has not been reached yet, several authors have suggested to delay hysterectomy once childbearing is completed [7, 24] in patients treated with myomectomy. Huo [9] argued that delayed hysterectomy until recurrence could be safe. Women must be counselled about the different option and the inconclusive data to tailor the treatment, balancing fertility versus the risk of recurrence and tumor metastasis. Vilos et al. [21] reported as 14.6% of patients who underwent hysterectomy following initial myomectomy had residual lesion. Our data showed that the proportion of women who underwent myomectomy who did not desire to conceive was very wide (almost 50%). These data raise a pivotal question: considered that hysterectomy is currently the gold standard treatment how should we manage women with diagnosis of STUMP after an incomplete surgery who do not look for pregnancy? Presumably in these cases, we recommend offering total hysterectomy in order to reduce to zero the risk of residual STUMP [19].
The conception rate in our review is less than in previous studies that reported the conception rate (53–60%) after myomectomy for leiomyomas [25, 26, 27]. No previous study evaluated the conception rate after surgery of STUMP. No conclusion can be reached due to the small number of cases that try to conceive after fertility sparing surgery with diagnosis of STUMP.
Regarding the modality of delivery, almost all these patients underwent a cesarean section to decrease the risk of uterine rupture with vaginal delivery after myomectomy, although the latest evidence indicates that labour could be feasible [28].
Actually, there is a lack of consensus about the appropriate follow-up after STUMP diagnosis [7]. In patients submitted to fertility sparing surgery, special attention may be paid to the uterus, which accounts for one-third of local recurrences. During follow-up of these patients, it is necessary to exclude the presence of new uterine masses or the growth of lesions already existent. Evaluation for STUMP relapse should be performed always before pregnancy is planned.
STUMP is a slow-growing tumor that relapses after an average of 51 months [7] following the initial diagnosis. In the manuscript of Sahin et al. [11], the time to disease recurrence was not reported so in literature there was any information about time to disease recurrence after pregnancy.
The recurrence rate reported in literature is very variable. STUMPs can recur either as STUMP or as leiomyosarcoma (in about 32% of cases), influencing the subsequent therapeutic choices, ranging from simple surgical excision to oncological treatments [20]. In our review, no case of recurrence as leiomyosarcoma has recorded.
The recurrence rate after pregnancy shown in our review is lower than the generic rate (7.3–14%) reported in most of studies [11, 23, 13] but similar to that found by Karataşlı et al. [14] (3.7%). Pregnancy does not seem to influence the rate of recurrence, although the sample is too small to reach any conclusions. The median age at diagnosis of our review is 31 years. Some studies considered the young age as a risk factor for STUMP recurrence [23, 29] but our data do not confirm this data, according to Basaran et al. [30] finding.
The optimal treatment for recurrent STUMP has not been established; surgical management is the first choice while the role of adjuvant therapy is less clear, and very few studies have been performed. Only two patients experienced relapse as uterine STUMP in our review, and both were submitted to hysterectomy and were disease-free during the follow up.
The limits of this review are represented by the small number of cases who tried to conceive and who reach a pregnancy, and the retrospective design of all the studies included. The creation of a national/international registry of STUMPs would be useful to investigate this rare tumour both in women submitted to fertility sparing and standard treatment. This would allow obstetrical and prognostic outcomes to be studied prospectively in large series and to verify if pregnancy influences the prognosis in these patients. A centralised histological review by a dedicated pathologist would be necessary in order to avoid incorrect diagnoses that could invalidate the results. In addition, a prospective study could help to identify molecular differences in STUMP with different clinical behavior and perhaps to find which cases are more aggressive; this could be very useful for counseling women who want fertility-sparing treatment and to save the uterus in patients with a low risk of recurrence.
On the other hand, it is the first review that analyzed the obstetric outcomes in patients with STUMP diagnosis, submitted to fertility sparing treatment. The strengths of this review are the long follow-up and the extensive information on obstetrical outcomes. Our study could be useful for clinicians who daily have to advise patients on the ontologically best treatment but also respect their fertility desire.
This review shows that pregnancy may be possible and safe after the diagnosis of STUMP, and it could be a useful tool for the counseling and the management of women with STUMP who desire to keep their fertility, although future prospective studies will be required to obtain definitive conclusions.
MA, SC, VP, SR and AE designed the theme of the review. MA, CR, VAC and CM searched and retrieved the relevant literature and wrote the first draft. MLV and SiP drafted the figure and table. SP, GV and RG reviewed and suggested corrections. All authors have read and approved the final manuscript.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest. Stefano Cianci is serving as one of the Editorial Board members and Guest editors of this journal. Carlo Ronsini is serving as one of the Guest editors of this journal. Roberta Granese is serving as one of the Editorial Board members of this journal. We declare that Stefano Cianci, Carlo Ronsini and Roberta Granese had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to Alessandra Andrisani and Loris Marin.
