Academic Editor: Michael H. Dahan
Objective: To assess the accuracy of ultrasound in diagnosing acute appendicitis in pregnant women. Mechanism: The National Library of Medicine (MEDLINE, 1990–2020), Excerpta Medica Database (EMBASE,1946–2020) and the Cochrane Controlled Trials Register (CENTRAL) were used to extract articles that were published in English. A total of five studies involving 521 patients were selected. The DerSimonian and Laird random-effects model and Quality Assessment Tool for Diagnostic Accuracy (QUADAS-2) were used to analyze the data. Findings in brief: We identified 140 related articles and included 5 articles enrolling 521 patients. The values obtained using ultrasound for appendicitis during pregnancy were sensitivity of 0.62 (95% Confidence interval (CI): 0.43–0.78), the specificity of 0.91 (95% CI: 0.74–0.97), and the Positive Likelihood Ratio of 7.0 (95% CI: 2.5–19.7), the Negative Likelihood Ratio of 0.41 (95% CI: 0.27–0.63) and the Diagnostic Odds Ratio of 17 (95% CI : 6–49). Conclusion: Ultrasound had medium-level sensitivity and high specificity for the diagnosis of appendicitis in pregnant women.
Although acute appendicitis in pregnant women is uncommon, it is the primary cause of non-obstetric surgeries with an incidence rate of 1 in 1250–1500 pregnant women [1, 2, 3, 4]. Precise diagnosis of appendicitis is challenging as it shares several symptoms which may be considered normal during pregnancy. For example, nausea and vomiting may be recognized as morning sickness, and abdominal pain can be misdiagnosed as ectopic pregnancy. Moreover, the complex physiological processes operating during pregnancy might also make clinical signs of appendicitis obscure. For instance, the increscent uterus may displace appendix superiorly to out of the right lower quadrant in some pregnant women. Furthermore, Lee and his colleagues [5] reported that the rate of negative appendectomy is higher in pregnant women and is associated with increased risk of fetal loss and/or premature birth [6, 7]. In addition, negative appendectomy and has no substantial impact on decreasing the rate of perforated appendicitis [8]. Therefore, it is crucial for surgeons to diagnose appendicitis accurately, especially in pregnant women.
Several imaging examinations have improved diagnostic accuracy for appendicitis and have avoided unnecessary appendectomies [9]. Ultrasound has multiple advantages including the lack of destructive and ionizing radiations. In addition, ultrasound is a well-established and widely recommended imaging tool to check for the presence of appendicitis in pregnant women [10, 11]. However, the diagnostic performance of the ultrasound for acute appendicitis in pregnancy is not well understood. Some studies found that the sensitivity of the ultrasound was between 0.18 [12] and 0.79 [13], while the specificity was from 0.68 [14] to 0.99 [12]. Therefore, this study aims to investigate the sensitivity and specificity of ultrasound for the diagnosis of acute appendicitis in pregnant patients. We hypothesize that ultrasound is a useful test in the diagnosis of acute appendicitis for pregnant patients with medium sensitivity and high specificity.
We performed a systematic computerized search using The National Library of Medicine (MEDLINE), Excerpta Medica Database (EMBASE) and the Cochrane Controlled Trials Register (CENTRAL) databases. The query terms “acute appendicitis”, “pregnancy”, “diagnosis” and “ultrasound” were used. English articles published up until the end of June 2020 were reviewed. Totally 140 articles were reviewed.
Original research articles, retrospective studies and prospective studies were reviewed. The studies were selected if it involved pregnant women with suspected acute appendicitis and ultrasound was used as a diagnostic tool. In addition, study selection was based on the availability of FP (false positive), FN (false negative), TP (true positive) and TN (true negative).
The initial assessment of studies was based on the article title, abstract and availability of full text. Exclusion was applied for studies involving patients who did not match the review question or ultrasound was not used as a diagnosis tool, or if they were reviews, case reports, or if they did not provide the required data.
The quality and applicability of articles were evaluated by the Quality Assessment Tool for Diagnostic Accuracy (QUADAS-2) [15]. Four assessments including index test, flowing, patient selection, reference standard and timing were analysed.
The Review Manager (RevMan) (Version 5.4. The Cochrane Collaboration, 2020, London, United Kingdom) was used to perform the analyses and generation of the forest plot and risk of bias and applicability concerns graphs. Stata (revision 20 Mar 2013 copyright 1985–2001 StataCorp LP, College Station, TX, USA) was also used for evaluating heterogeneity and making summary receiver operating characteristic curve (SROC) curve. The sensitivity and specificity of data were assessed using DerSimonian and Laird random-effects model.
140 articles were identified from the initial search and were assessed based on titles and abstracts. Eventually, 5 studies were included for analysis in this study (Fig. 1) [12, 13, 14, 16, 17]. The key parameters of included studies are listed in the Table 1 (Ref. [12, 13, 14, 16, 17]).
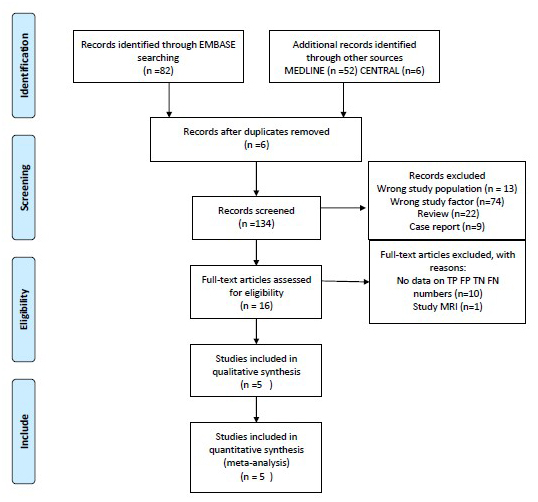 Fig. 1.
Fig. 1.The process of study selection.
| Study ID | Publication type | Study type | Sample size | Average age | Risk of bias | Sonographer experience | AA prevalence (%) | Ultrasound sensitivity (%) | Ultrasound specificity (%) |
| Yoav 2019 [14] | Full text | Retrospective | 86 | 31.3 | High | Not state | 67 | 69 | 68 |
| Abbas 2015 [16] | Full text | Retrospective | 36 | 27.29 | High | High | 86 | 61 | 80 |
| Lior 2016 [17] | Full text | Retrospective | 66 | 28 | High | Not state | 79 | 65 | 86 |
| James 2018 [13] | Full text | Retrospective | 216 | 25.8 | High | High | 82 | 79 | 92 |
| Joseph 2015 [12] | Full text | Retrospective | 117 | Not available | High | High | 9.4 | 18 | 99 |
The five selected studies were retrospective and involved 521 participants, of which studies involving pregnant women seeking diagnosis of appendicitis were included. All trials were single medical center. Pathological test after appendectomy was used to determine the diagnosis performance of ultrasound and served as the standard reference.
Of the five selected studies, three studies compared the working performance of ultrasound for the diagnosis of acute appendicitis in pregnant versus non-pregnant subjects [14, 16, 17]. One study explored whether performing a delayed repeat of ultrasound could increase the diagnostic yield [13]. Another study compared the diagnosis accuracy between ultrasound and Magnetic Resonance Imaging (MRI) [12].
All selected studies were retrospective studies by obtaining the information from hospital digital records. None of the article used consecutive or random sampling method for selection of patients and all included certain patients (the number of patients ranged from 2 [13] to 25 [14]) who meet the included criteria but had no record for ultrasound. The ultrasound was applied before operation; therefore, results of the index test were deciphered without a reference standard. Four out of five studies [12, 13, 16, 17] mentioned that ultrasound results were interpreted by experienced radiologists. Three studies [12, 13, 17] gave reasons for categorization using pre-specified thresholds. None of the five studies explained whether the pathology results were interpreted independently of the index tests. All the participants who were applied with ultrasound diagnosis receive the same pathology test.
To diagnose appendicitis in pregnancy, the ultrasound sensitivity was 0.62 (95%
CI: 0.43, 0.78), the specificity was 0.91 (95% CI: 0.74, 0.97), the Positive
Likelihood Ratio was 7.0 (95% CI: 2.5, 19.7), the Negative Likelihood Ratio was
0.41 (95% CI: 0.27, 0.63) and the Diagnostic Odds Ratio was 17 (95% CI: 6, 49).
Forest plots of sensitivity and specificity and the analysis for SROC were shown
in Figs. 2,3 respectively. High variation was observed in the specificity (I
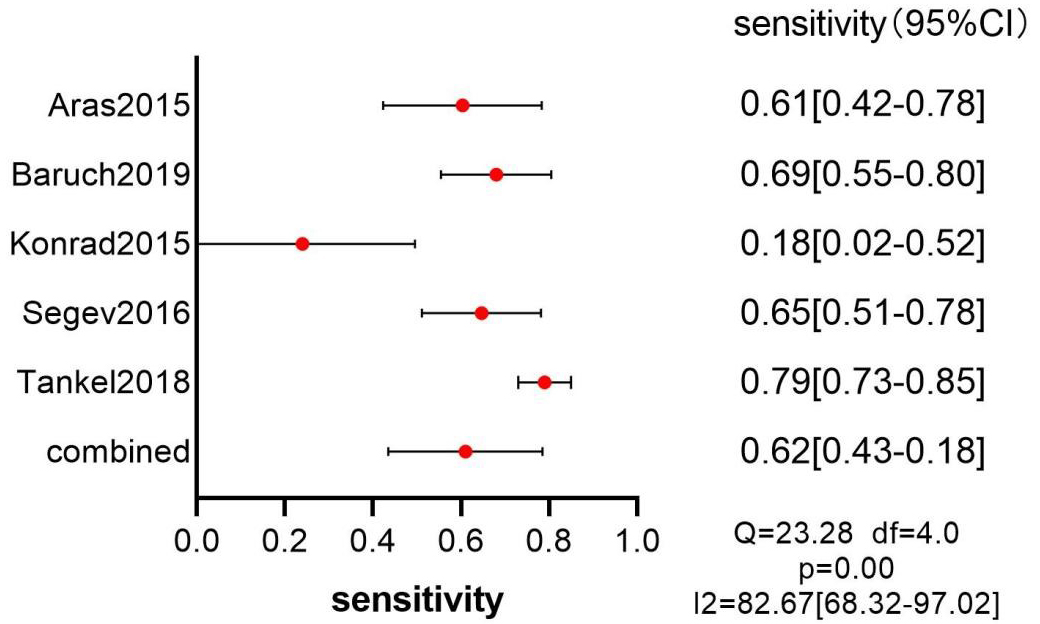 Fig. 2.
Fig. 2.Forest plot-sensitivity of ultrasound.
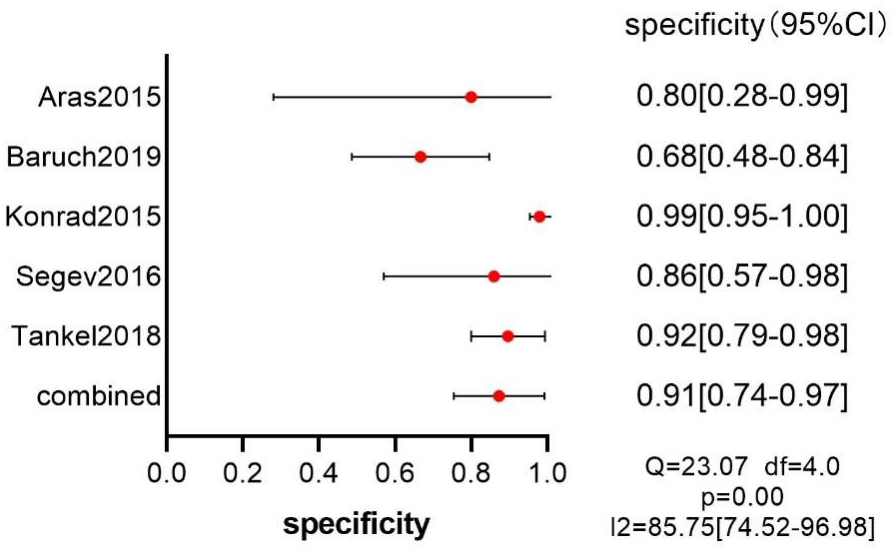 Fig. 3.
Fig. 3.Forest plot-specificity of ultrasound.
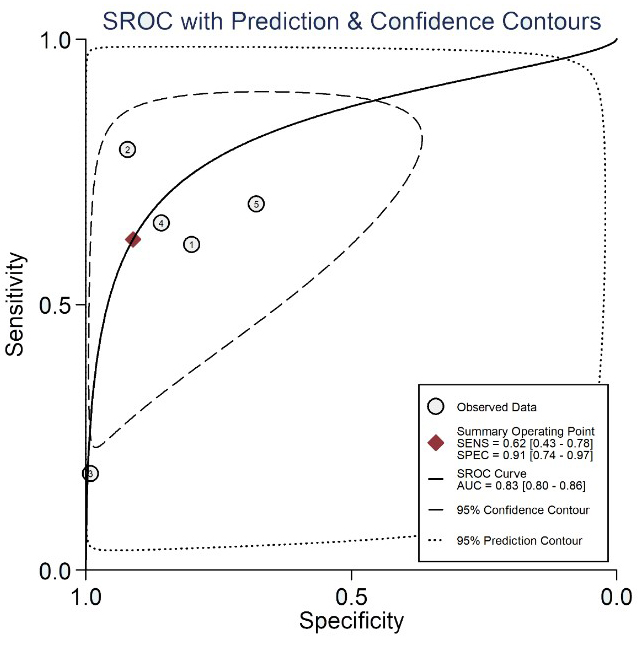 Fig. 4.
Fig. 4.SROC (Summary Receiver Operating Characteristic Curves) of the ultrasound with prediction & confidence contours.
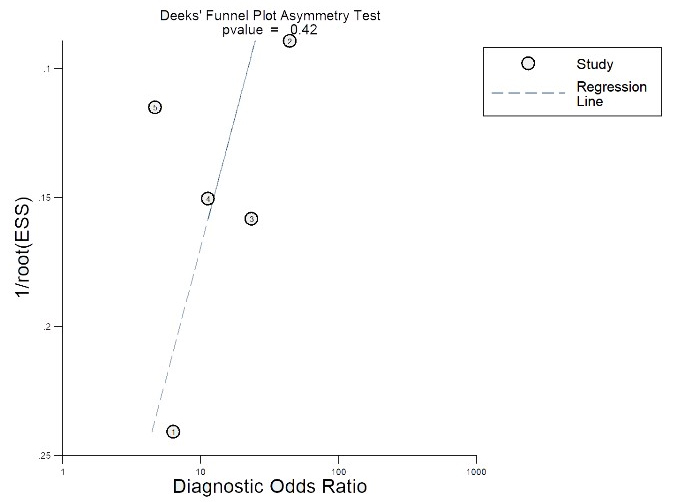 Fig. 5.
Fig. 5.Deeks’ Funnel Plot Asymmetry Test.
Meta-analysis studies [18, 19, 20] showed that the sensitivity as well as
specificity of the ultrasound for the diagnosis of acute appendicitis were
69%–83.1% and 81%–93% respectively. Moreover, ultrasound is widely
available, economical, and imposes no adverse ionizing radiation [12]. However,
Yoav et al. [14] showed that ultrasound examination of pregnant women
might provide an inconclusive data (43.3% vs. 11.1%, p
The sensitivity of CT is 91–98.5% and the specificity is 90–98% [21, 22, 23]. The excellent performance on diagnosis makes CT the most widely used examination in general population with suspected appendicitis. However, CT is not recommended for pregnant women due to its radiation. The consequence of radiation exposure in fetuses is mostly based on observations rather than original research which is banned due to ethical issues [24].
Kave and his colleagues [25] reported that MRI had sensitivity of 91.8% whereas the specificity of 97.9% in diagnosing appendicitis in pregnant women. According to Saini et al. [26], the technical cost of MRI was more expensive than that of ultrasound. The use of a class C drug called gadolinium makes the safety of MRI uncertain according to the Food and Drug Administration [27]. Therefore, MRI is only used if the ultrasound results are inconclusive, for suspected appendicitis during pregnancy [27].
In this meta-analysis, the sensitivity and specificity for ultrasound in diagnosing of appendicitis during pregnancy were 62% and 91%, respectively. It was reported that an optimized ultrasound algorithm significantly improved the diagnoses of appendicitis made by ultrasound, and the diagnosis performance might be further improved when operated by experienced radiologists [28, 29]. Moreover, Leichtle and his colleagues [30] reported that obesity was associated with increased rate of incorrect results from ultrasound, and Hoffmann et al. [31] found that intra-abdominal air could foil image acquisition.
There are a few limitations in our study. All five articles included were retrospective studies. The five articles only included patients with suspected appendicitis that also underwent appendectomy. The information for pregnant patients who underwent ultrasound test but without the appendectomy was missing and no follow up information was obtained. All those factors might make the TP and FP lower than actual numbers. Moreover, those articles [32, 33, 34, 35, 36] provided the sensitivity and specificity values but not TP, FP, TN or FN values from the revision.
In summary, data of this meta-analysis revealed that ultrasound had a medium-level sensitivity and high specificity on the diagnosis of acute appendicitis in pregnant women.
YLL wrote the manuscript, conducted the statistical analyses, and retrieved data from medical database. SKL retrieved data and reviewed the final manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Not applicable.
We are very grateful to all people that helped us in the process of writing this manuscript. In addition, we would like to thank the anonymous reviewers who have helped to improve the paper.
This research received no external funding.
The authors declare no conflict of interest.
