Academic Editor: Antonio Simone Laganà
Background: With the increased frequency of diagnosis of interstitial
pregnancy in the early first trimester, non-surgical management of unruptured
interstitial pregnancy has become an important issue. However, management of
unruptured interstitial pregnancy by uterine artery chemoembolization (UACE) with
dactinomycin has never been evaluated via a case series. Methods: With
this aim, a retrospective review of electronic chart records over a five-year
period was performed, and a series of cases of unruptured interstitial pregnancy
during the first trimester was extracted. Diagnostic procedures included
ultrasonography, magnetic resonance imaging (MRI), and laparoscopic examination,
if necessary. Conservative treatment regimen included UACE. Additional
administration of methotrexate (MTX) was considered when an insufficient decline
of serum
Ectopic pregnancy occurs when the fertilized ovum implants outside the endometrial cavity [1]. The reported incidence of ectopic pregnancy occurs in 1.3% to 2% of all pregnancies [1]. Therefore, ectopic pregnancies represent an important risk factor for maternal morbidity and mortality in early pregnancy. Implantation of the fertilized ovum in the fallopian tube accounts for approximately 95% to 99% of ectopic pregnancies [1], whereas other localizations, such as ovarian, cervical, abdominal, and hepatic implants, contribute to rare occurrences (1% to 4%) of ectopic pregnancy [1, 2].
Interstitial pregnancy is defined as a rare and potentially dangerous type of ectopic gestation involving implantation in the uterine interstitial portion of the fallopian tube [3, 4]. Interstitial pregnancies account for only 2% to 4% of tubal pregnancies [3]. However, it has been reported that the mortality rate is as high as 2.5%, which is seven times higher than that of typical ectopic pregnancies [4].
If rupture occurs in the interstitial portion of the uterus, which includes abundant blood supply from a complex pelvic vascular network composed of the uterine artery and anastomosing ovarian artery, definitive management involves life-saving intervention either by laparotomy or, more recently, laparoscopy [3]. However, for the management of hemodynamically stable cases without rupture, a wide range of surgical and non-surgical procedures are available [3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14].
With the recent development of diagnostic and therapeutic modalities, diagnosis of interstitial pregnancy in the early first trimester has become increasingly common [3]. Consequently, non-surgical management of unruptured interstitial pregnancy has become a prevalent issue [7, 11, 12, 13].
Previously reports demonstrated that uterine artery chemoembolization (UACE), which involves uterine arterial chemotherapy infusion followed by endovascular embolization, is a feasible option for managing interstitial pregnancy [4, 5, 6].
In the present study, the therapeutic value of UACE for the management of unruptured interstitial pregnancy diagnosed in the early first trimester was retrospectively evaluated in a case series.
This was a retrospective single-center study conducted at Gifu Prefectural Tajimi Hospital (Tajimi, Gifu, Japan). The inclusion period was from January 2014 to December 2018. Initially, cases that met the International Classification of Diseases related to ectopic pregnancy (633.10, 633.11, 633.20, 633.80, 633.81, 633.90) were retrieved from the hospital electronic chart record. A manual check of all records was performed to identify cases of interstitial pregnancies. Among cases of interstitial pregnancies, only unruptured interstitial pregnancies diagnosed in the early first trimester were extracted, and cases with advanced gestation calculated from the last menstrual period at initial evaluation were excluded.
Detailed information about each patient, including demographics, gynecological
and obstetrics history, and previous surgery, was retrieved from a review of
clinical records and diagnostic images. Concerning the characteristics of
interstitial pregnancies, dates of admission and discharge from the hospital,
initial level of
Only patients that were observed for at least a year after the completion of treatment were included. Informed written consent was obtained from the patients regarding the use of their data for the study and publication of their disease status and clinical characteristics. Protective measures were taken to conceal the identity of patients. The Institutional Review Board of Gifu Prefectural Tajimi Hospital approved the current study (IRB number: 2020-OG-3).
The datasets generated and analyzed during the current study are not publicly available, as they contain information that could compromise patient confidentiality. However, they are available from the corresponding author [A.T.] upon reasonable request.
Women with suspected ectopic pregnancy were initially evaluated by transvaginal
ultrasonography and measurements of the serum
When definitive diagnosis of interstitial pregnancy was difficult to determine but was suspected on initial ultrasonography, MRI was performed to locate the gestational sac. If necessary, three-dimensional computed tomographic angiography (3D-CTA) was performed to assess the degree of uteroplacental neovascularization [5, 6]. After the images of each case were cooperatively evaluated by gynecologists and diagnostic radiologists, a consensus was made on the diagnosis and strategy for individual management.
Criteria for MRI diagnosis of interstitial pregnancy were a thickened endometrium without signs of gestation in the uterine cavity and identification of a gestational sac-like structure within the muscular layer of the uterine cornus adjacent to the uninterrupted junctional zone [5, 6].
When the precise location of a gestational sac-like structure could not be determined even with the addition of MRI, exploratory single-port laparoscopy through an umbilical incision [17] was performed. If isthmic tubal pregnancy was confirmed, thus eliminating the possibility of interstitial pregnancy, laparoscopic excision of the affected fallopian tube was planned. If interstitial pregnancy was confirmed, either laparoscopic excision of gestational products was completed, or diagnostic laparoscopy followed by chemoembolization was performed based on the surgeon’s decision while considering the patients’ wish according to the informed consent. Depending on the site where gestational products were identified, interstitial pregnancy was further classified into proximal [6] or distal interstitial pregnancy [5].
If immediate uterine devascularization with cytotoxic drugs was deemed necessary to remove interstitial gestational products, urgent digital subtraction angiography was performed. After a vascular mass derived from interstitial gestational products was confirmed, the branch of the uterine artery supplying the interstitial pregnancy was selectively catheterized under fluoroscopic guidance [5, 6].
UACE was performed by infusing dactinomycin (0.5 mg/body; Cosmegen; Merck & Co., Inc., Whitehouse Station, NJ, USA) intra-arterially, followed by endovascular embolization using gelatin sponge particles (Serescue; Nippon Kayaku Co., Tokyo, Japan) as reversible embolization materials [5, 6].
After UACE, serial measurements of the serum
Of 125 women with ectopic pregnancy, eight consecutive cases (6.4%) were identified as interstitial pregnancies (Fig. 1). Gestational age was calculated based on the last documented menstrual period. Four cases with ruptured interstitial pregnancy, which were managed by laparoscopic surgery, were excluded from the current study.
 Fig. 1.
Fig. 1.Flow diagram of the classification of ectopic pregnancies experienced from 2014 to 2018. Of 125 ectopic pregnancies, unruptured interstitial pregnancy was diagnosed in the early first trimester of pregnancy in four cases. One case was managed by laparoscopic cornuostomy due to concerns about cornual rupture because of thinning of the myometrium (inset, arrow). Two cases were successfully managed solely by uterine artery chemoembolization (UACE), while another case required systemic methotrexate administration after UACE to achieve complete resolution.
Unruptured interstitial pregnancy was diagnosed in four women in the early first trimester of gestation. In one case with thinning of myometrial tissue detected under laparoscopic vision, laparoscopic cornuostomy was performed because of concerns about rupture, and this case was excluded (Fig. 1). The other three cases were initially managed by UACE and were included in the current investigation. The clinical course of each case is described below.
A 30-year-old, gravida 3, para 2 woman (Fig. 2) was referred at 6 weeks and 2 days of gestation because her physician suspected an ectopic pregnancy after she presented with amenorrhea following spontaneous conception.
 Fig. 2.
Fig. 2.Case 1: Proximal interstitial pregnancy managed by uterine
artery chemoembolization (UACE) after diagnosis by magnetic resonance imaging
(MRI). (A) Coronal T2-weighted MRI showing suspected gestational products with a
diameter of 8 mm (arrow) in the proximal portion of the right interstitial
uterine wall adjacent to the junctional zone. (B) Coronal three-dimensional
computerized tomographic angiographic image in the arterial phase showing a
prominent vascular mass (arrow) being fed by the right uterine artery and
anastomosing left uterine artery in the right cornual region. (C) Digital
subtraction angiography showing gestational products (arrow) supplied by the
right uterine artery. (D) Changes in the serum
At the initial referral, the serum
After MRI-based diagnosis of an unruptured proximal interstitial pregnancy of
the right fallopian tube, UACE was performed for immediate devascularization of
gestational products (Fig. 2C, arrow). The serum
A 30-year-old, gravida 2, para 0 woman (Fig. 3) was referred at 6 weeks and 5
days of gestation under suspicion of ectopic pregnancy after conception by
ovulation induced with clomiphene citrate followed by hCG injection. At triage,
the serum
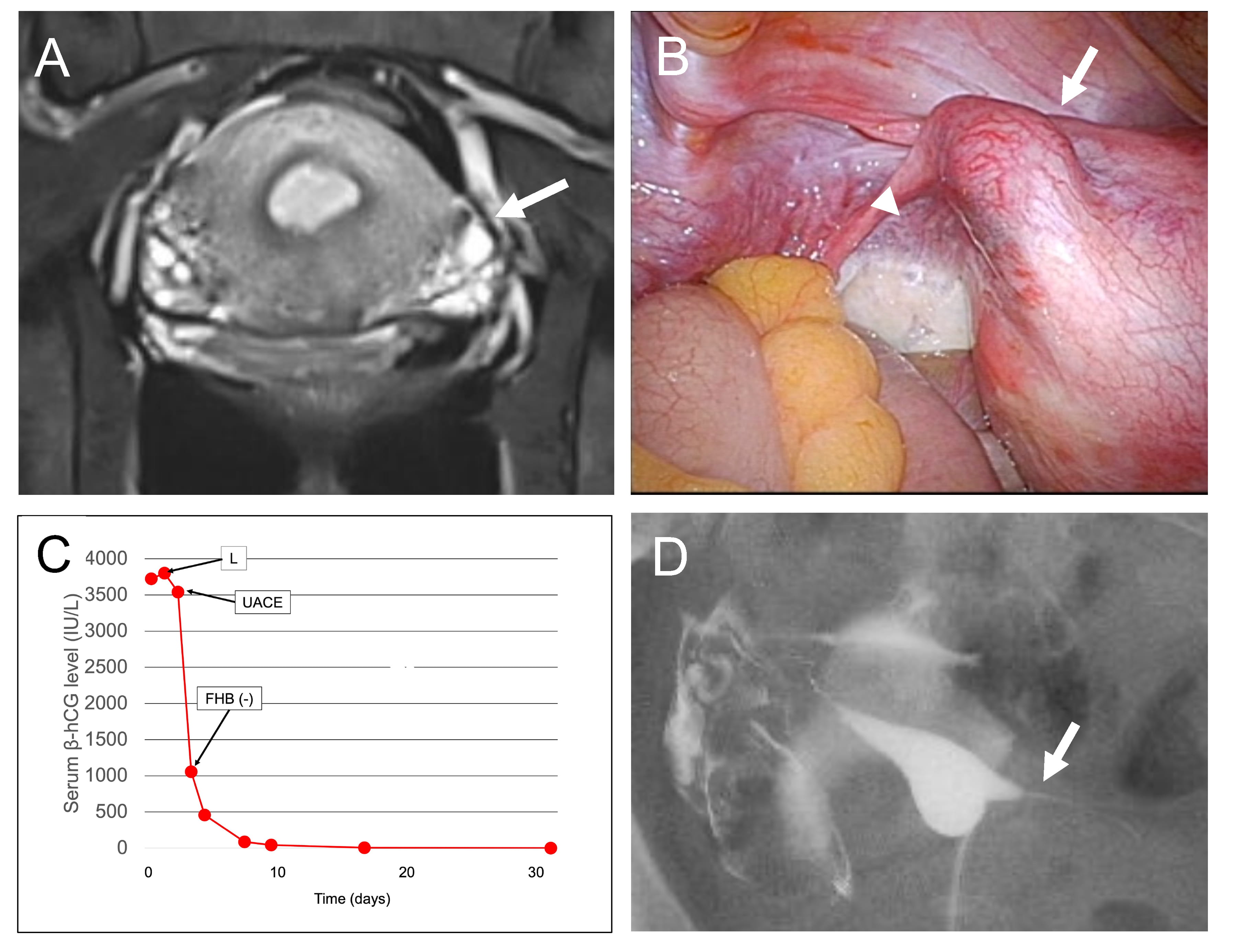 Fig. 3.
Fig. 3.Case 2: Distal interstitial pregnancy managed by uterine artery
chemoembolization (UACE) after laparoscopic diagnosis, followed by a successful
pregnancy outcome. (A) Coronal T2-weighted magnetic resonance imaging showing
suspected gestational products with a diameter of 8 mm (arrow) in the left
lateral angle of the uterine corpus, suggesting a radiological diagnosis of left
isthmic pregnancy rather than interstitial pregnancy. (B) Single-port
laparoscopic view showing an enlarged left interstitial portion (arrow)
protruding from the uterine cornu median to uteroovarian ligament (arrowhead),
indicating that gestational products exist in the distal portion of the
interstitial fallopian tube. (C) Changes in the serum
A gestational sac with a positive FHB in the left adnexal region adjacent to the uterus (data, not shown) was detected upon ultrasonographic examination. Coronal T2-weighted MRI revealed a gestational mass-like structure with a diameter of 8 mm (Fig. 3A, arrow) at the left lateral angle of the uterine corpus, which led to a radiological diagnosis of left isthmic pregnancy rather than interstitial pregnancy.
A single-port laparoscopic view revealed an enlarged left interstitial portion (Fig. 3B, arrow) medial to the utero-ovarian ligament (Fig. 3B, arrowhead) protruding from the interstitial portion, which indicated that gestational products exist in the distal interstitial portion of the fallopian tube.
Since early rupture was deemed improbable, UACE was performed for
devascularization of gestational products. One day after UACE, there was a
decrease in the serum
Two years later, spontaneous conception occurred (side of ovulation unknown), followed by an uneventful vaginal birth at 38 weeks and 3 days of gestation resulting in a healthy, 2972 g female infant with Apgar scores of 9 and 10 at 1 and 5 minutes, respectively.
A 42-year-old, gravida 2, para 0 woman (Fig. 4) was referred at 6 weeks and 4 days of gestation under suspicion of right interstitial pregnancy with a positive FHB after conception by in vitro fertilization and embryo transfer.
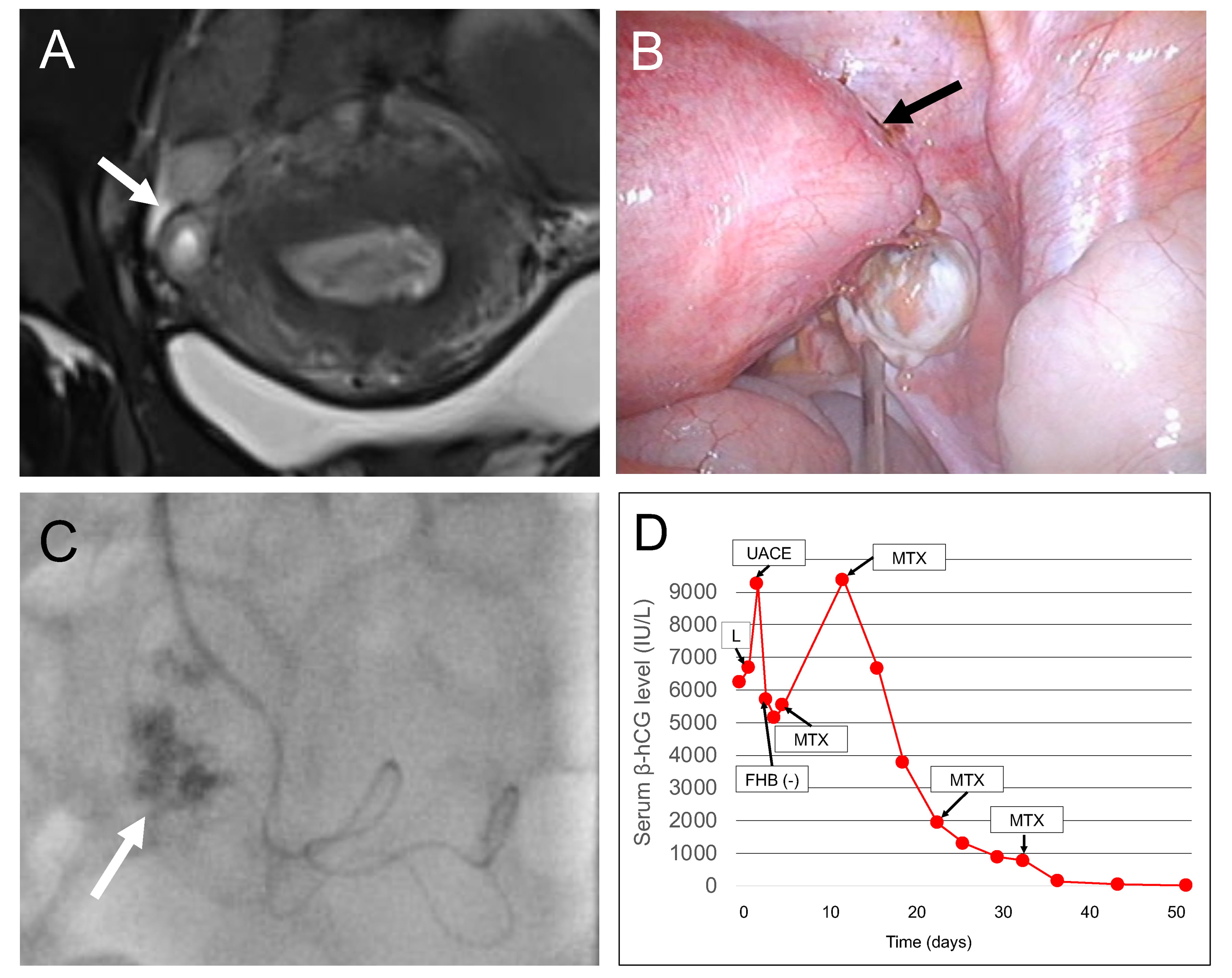 Fig. 4.
Fig. 4.Case 3: Distal interstitial pregnancy managed by uterine artery
chemoembolization (UACE) after laparoscopic diagnosis, followed by systemic
methotrexate administration. (A) Coronal T2-weighted magnetic resonance imaging
showing suspected gestational products with a diameter of 7 mm (arrow) covered by
a thin layer of myometrium in the right lateral angle of the uterine corpus.
Radiological diagnosis indicated distal interstitial pregnancy, although isthmic
tubal pregnancy could not be excluded. (B) A single-port laparoscopic view
showing an enlarged right cornual portion indicated that gestational products
exist in the distal portion of the interstitial fallopian tube. (C) Digital
subtraction angiography showing gestational products (arrow) supplied by the
right uterine artery. (D) Changes in serum
At the initial examination, the serum
Radiological diagnosis strongly indicated a distal interstitial pregnancy, although isthmic tubal pregnancy could not be completely excluded. Thereafter, single-port laparoscopy revealed a swollen right interstitial portion (Fig. 4B, arrow), which confirmed the diagnosis of right distal interstitial pregnancy, and pelvic adhesion due to peritoneal endometriosis was identified.
Since immediate rupture was deemed improbable, UACE was performed for
devascularization of gestational products (Fig. 4C, arrow). One day after UACE,
there was an immediate decrease in the serum
In this case, infertility therapy was resumed four months after UACE but was eventually terminated due to a complication of severe tubo-ovarian abscess at transvaginal oocyte retrieval.
In replacing traditional laparotomy, early diagnosis of interstitial pregnancy before rupture makes various minimally invasive methods of treatment possible [3]. These medical management approaches include expectant management [3]; laparoscopic surgery [9] with reversible occlusion of uterine arteries and cornuostomy for advanced cases [18]; hysteroscopic management [6, 10, 14]; medical cytotoxic management [11] with mifepristone [12]; and endovascular therapy [8] with cytotoxic infusional chemotherapy [4].
Although such procedures, which can be performed independently or in combination [3], yield favorable outcomes with a satisfactory success rate, some adverse outcomes have been reported. In cases managed by laparoscopic surgery, interstitial rupture in subsequent gestation may lead to severe maternal and fetal morbidity [3], whereas in cases treated with expectant, medical, or endovascular therapy, incomplete resolution of the gestational tissue might require emergency surgical intervention due to interstitial rupture associated with significant hemorrhaging [19].
Based on our limited experiences with UACE for the management of unruptured interstitial pregnancies [5, 6], precise localization of gestational tissue by diagnostic imaging evaluations are needed to obtain successful outcomes. For diagnosis of interstitial pregnancy at early gestational age, transvaginal ultrasonography with color-flow mapping is the first modality of choice [15]. Furthermore, three-dimensional ultrasound can precisely detect localization of the gestational sac to the interstitial portion of the fallopian tube [16].
However, when ultrasonography to differentiate interstitial pregnancy from an eccentrically implanted intrauterine pregnancy is inconclusive, it has been shown that MRI has a superior space-resolving ability compared to routine ultrasonography, as it can reveal a gestational sac-like structure within the myometrium [5, 6].
However, in the current study dealing with cases during the early first trimester, which therefore had small-size gestational products, the diagnostic ability of MRI was limited when distal interstitial pregnancy was suspected, as in Cases 2 and 3, mainly because the uterine interstitial portion had a complex curved structure that could not be visualized well by conventional three-directional slices of MRI.
In such cases, exploratory laparoscopy is needed to achieve a final diagnosis of interstitial pregnancy, as it has been shown that many interstitial pregnancies are not practically diagnosed before surgery, with 56% to 71% of interstitial pregnancies mistaken for other types of ectopic pregnancy before surgery [3].
Spontaneous miscarriage is a common pregnancy outcome, whether the pregnancy is
intrauterine or ectopic in location. Consequently, expectant management of distal
tubal pregnancies is a treatment option when a spontaneous decline of serum
Similarly, expectant management of interstitial pregnancy has been successful in
some cases [1]. However, complications include persistent pain requiring surgical
excision even after successful management, catastrophic rupture and associated
maternal morbidity and death, an unpredictable course to resolution even with
declining serum
In the current case series, retrospective speculation supposed that, especially
in Case 2, expectant management could be an option because there was some degree
of spontaneous decline in the serum
Concerning the efficacy of UACE in resolving interstitial gestational products
in three of the current cases, Cases 1 and 2 were successfully managed by UACE
alone, whereas Case 3, re-elevation of the
Re-elevation of the serum
Therefore, if interstitial gestation products receive more blood from the
anastomosing ovarian artery than uterine arteries, complete resolution might not
be achieved solely by UACE. Consequently, in such cases, additional MTX
administration should be considered along with careful monitoring of interstitial
rupture after poor decline of the serum
Concerning uterine integrity with a focus on preserving future fertility after UACE, in Case 2, in which the patient reported a wish to retain fertility, UACE was successful, and hysterosalpingography after resolution of the gestation products showed restored patency of the affected fallopian tube followed by a successful pregnancy outcome after spontaneous conception, although the laterality of ovulation resulting in conception was not determined. More cases on this issue are required to validate the current findings so that reproductive and pregnancy outcomes in women undergoing different treatment approaches for interstitial pregnancy can be investigated, as different outcomes have been demonstrated for tubal ectopic pregnancies for which different management approaches were used [1].
At present time, the risk of recurrent interstitial pregnancy in subsequent gestation remains uncertain in cases with unruptured interstitial pregnancy treated with UACE due to the limited number of cases that were evaluated in the current study. However, important issues were raised by this study, which should be validated by an accumulation of future cases.
In the current cases, precise diagnosis in the early first trimester (all within six weeks of gestation) allowed unruptured interstitial pregnancy to be treated by UACE with or without subsequent systemic MTX administration; however, whether or not more advanced gestational cases with larger gestational products can be managed by the current procedure is unclear.
Based on our limited experience, laparoscopic surgery with or without endovascular therapy, as shown in our previous report [17], seems more appropriate for such cases than UACE due to the increased risk of a catastrophic outcome caused by interstitial rupture during conservative management [19].
Because several diagnostic and therapeutic modalities in addition to routine ultrasonography were used for management of these cases, the extra medical expenses present another concern regarding the studied treatment option. Further development of the modality, including the increased role of three-dimensional ultrasound, with an improvement of diagnostic ability are needed to overcome the challenges that we have encountered in our department.
The findings from this small case series suggest that UACE is a feasible, minimally invasive option for treating unruptured interstitial pregnancy diagnosed in the early first trimester in order to preserve the uterine structure and function, especially in women who wish to remain fertile.
AT and WK contributed to the conception of the study. AT, SI, ST, and WK contributed significantly to data analysis. AT wrote the manuscript. SI, ST, and WK helped in data collection. AT performed the analysis with constructive discussions. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
All subjects gave their informed consent for inclusion before participation in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Gifu Prefectural Tajimi Hospital (IRB number: 2020-OG-3).
We would like to thank Enago (https://www.enago.jp) for English language editing.
This research received no external funding.
The authors declare no competing interests. AT is the Editorial board member of this journal, given his role as Editorial board member, AT had no involvement in the peer-review of this article and has no access to information regarding its peer-review.
