Background: Concerning total laparoscopic hysterectomy (TLH), opening
the retroperitoneum and prophylactic ligation of both uterine arteries (UA) is
not a routine procedure during a simple hysterectomy and it is not practiced
widely in gynecology education. Methods: In this study, we tried to show
the prophylactic ligation of internal iliac artery anterior division (IIAD) and
provide hemostasis of UA at an anatomical plane where we considered it would be
easier to perform and relatively safer, in terms of distance, regarding ureteric
injury, in a prospective randomized controlled trial. Results: When this
technique was used the duration of the operation got longer approximately 3
minutes (min) (57.15
Hysterectomy is considered to be one of the most common gynecologic surgical procedures performed all around the world. The abdominal route is still the most frequently performed method but on the other hand laparoscopic hysterectomy trends are also rising, especially in challenging cases such as morbid obesity, having had previous surgeries, or large uteri [1, 2].
Excluding vaginal hysterectomy, whether the laparotomic or laparoscopic route is preferred, opening the retroperitoneum is not a routine procedure during a simple hysterectomy and it is not practiced widely in gynecology education.
Concerning total laparoscopic hysterectomy (TLH), in addition to many reported advantages, the peroperative blood loss was documented to be less in TLH especially when prophylactic ligation of both uterine arteries (UA) was performed in the beginning of the procedure [3, 4]. In previous studies, UA was sutured or ligated by applying hemoclips just after the division between the obliterated umbilical artery and this anatomical site is known to be adjacent to the ureter [3, 5]. It was reported that the prophylactic ligation of UA also has positive effects on peroperative and postoperative outcomes [3, 5]. However, dissection and ligation of UA at the point of its origin requires advanced surgical skills.
In terms of complications, ureteric injury is a remarkable morbidity during laparoscopic hysterectomy, occurring with a ratio about 0.7% [6]. One of the most common sites of injury is where it intersects the UA thus, the surgeon needs to be mindful when ligating the UA because the ureter passes beneath this artery and is at risk for injury [7, 8, 9].
In this study, we tried to show the prophylactic ligation of internal iliac artery anterior division (IIAD) and provide hemostasis of UA at a new anatomical 2 dimensional plane where we considered it would be easier to perform and relatively safer due to its distance regarding ureteric injury. This anatomical 2 dimensional plane which we named as “Delta 1 triangle” is a virtual retroperitoneal triangle that has not been specifically defined in the current literature. The borders of this triangle are anatomically formed by IIAD, UA and the ureter (Fig. 1).
 Fig. 1.
Fig. 1.Location of “Delta 1 triangle” (Right side).
The main reasons for coming up with this technique was to eventually utilize it to reduce blood loss in more complex hysterectomies and pelvic lymphadenectomy.
This prospective study aims to compare intraoperative and postoperative results in terms of operation duration, blood loss and complications when the IIAD was prophylactically ligated just before the origin of UA during total laparoscopic hysterectomy.
This multi-center, prospective randomized controlled trial was conducted at Ondokuz Mayis University Faculty of Medicine, Gynecology and Obstetrics Department, Samsun, Turkey and Duzce University, Faculty of Medicine, Gynecology and Obstetrics Department, Duzce, Turkey between 2017–2019.
Inclusion criteria were as follows; patients with clinically diagnosed myoma uteri, endometrial hyperplasia, benign adnexial mass and persistent menorrhagia that were planned for hysterectomy.
Exclusion criteria were as follows; patients with atherosclerotic disease and/or confirmed malign disease or patients suspected to have a malign disease based on preoperative foundings.
A total of 110 patients who underwent total laparoscopic hysterectomy and bilateral salphingoooferectomy (TLH + BSO) were included in the study. Five patients were lost to follow up. The patients were randomized into two groups according to computer generation upon admittance to the clinics for surgery, 53 patients that were operated without IIAD ligation formed the control group (ligation negative group) and 52 patients with prophylactic IIAD ligation formed the study group (ligation positive group). The patients were compared based on demographic data such as age, body mass index (BMI), parity and indications for surgery. The peroperative and postoperative outcomes were compared between the ligation negative group [LN (-)] and ligation positive group [LN (+)] (Fig. 2). Complications encountered during the course of the procedure were classified as major vascular injuries, urinary tract injuries, conversion to laparotomy and bowel injuries. Complications after the procedure were described as vaginal cuff dehiscence, pelvic abscess and ileus. The total time of operation was defined as the time from the placement of the first trocar until the successful closure of the vaginal cuff. Blood loss during the operation was measured by subtracting the volume of aspirated fluid from the irrigation fluid at the end of the procedure.
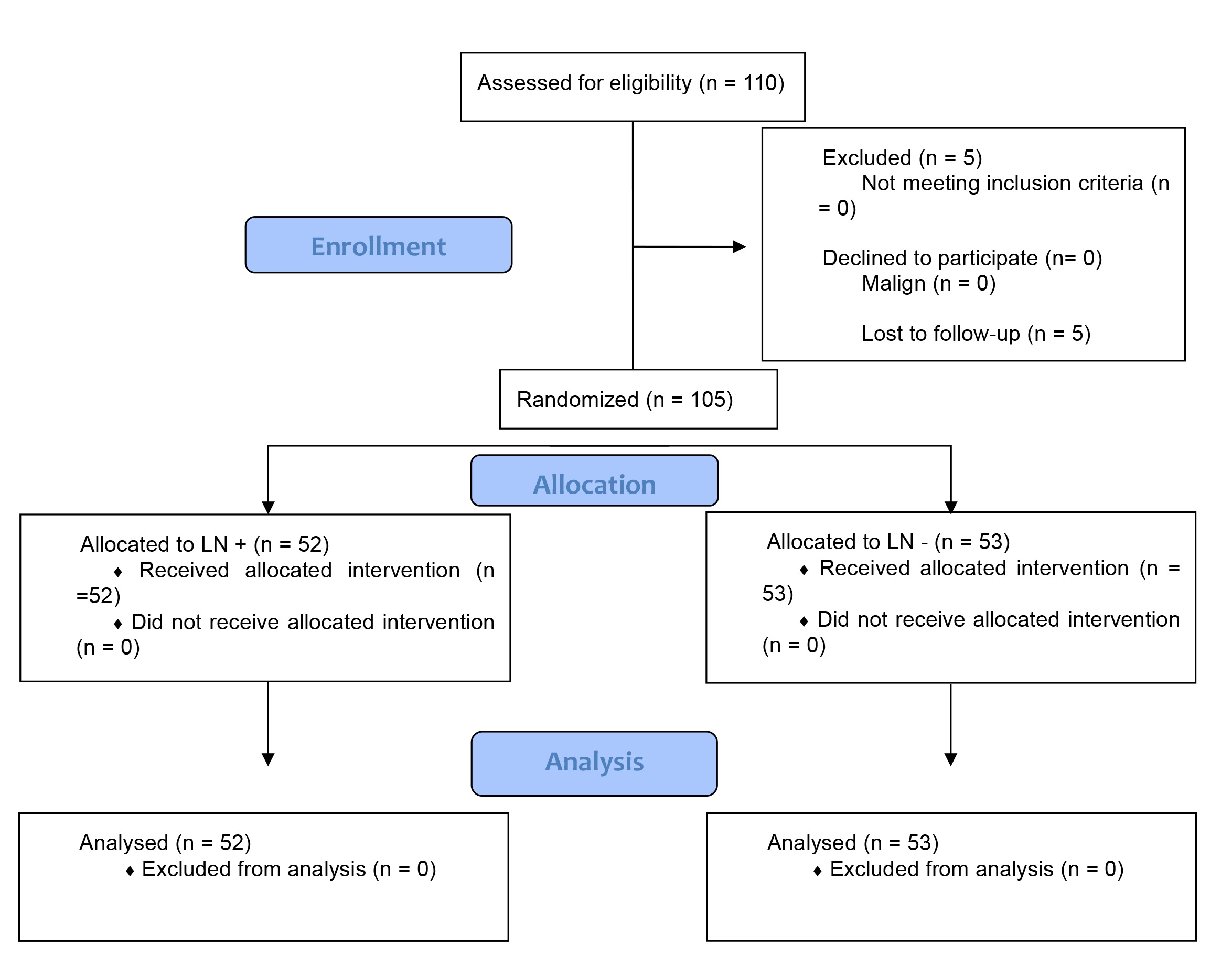 Fig. 2.
Fig. 2.Flow diagram of the selection, enrollment and randomization of the participants.
All laparoscopic hysterectomies were performed by the first and second authors under general anesthesia and the patients were placed in a lithotomy position. A urinary catheter and nasogastric tube were both placed in all the patients before the operation. The surgeries were carried out at 30° Trendelenburg position and under 14 mm Hg pneumoperitoneum after the first trocar placement. A manipulator was used to elevate the uterus from the pelvic floor during surgery. After creating pneumoperitoneum and a 10-mm trocar sleeve placement through the umbilicus, a 10-mm telescope was passed through this sleeve. Two 5-mm trocar sleeves were placed in both hypochondrium regions lateral to the rectus abdominis muscle and inferior epigastric vessels in the outer one-third of the distance between the anterior superior iliac spine and umbilicus and one 5-mm trocar sleeve was placed in between [10].
In the LN (+) group of patients, the round ligament was divided and dissected
using an ultrasonic scalpel (Harmonic Ace®, Ethicon Endo-Surgery
Inc.; Cincinnati, OH, USA) to reveal the anterior leaf of broad ligament.
Hemostasis was achieved in the infundibulopelvic ligament (IP) via a
vessel-sealing device (LigaSure
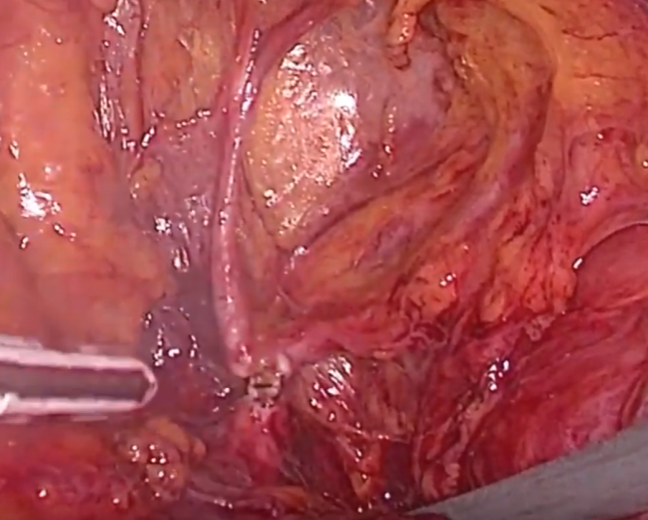 Fig. 3.
Fig. 3.The “Delta 1” retroperitoneal triangle and ligation point for providing hemostasis in UA (Left side).
As shown in Fig. 1 and Fig. 3, the trajectory of the related arteries and ureter is
easily visible to localize the assumed ligation point. The distance between the
ureter and the point where the vessel-sealing device was planned to be used is
about 22
 Fig. 4.
Fig. 4.Illustration of the origin of UA [11] and the ligation point of IIAD in our study, referred to as “ * ” sign.
The anterior and posterior sheets of the peritoneum were unfolded to expose. The bladder was dissected from the lower segment of the uterus and superior portion of the vagina. Using the tissue fusion device, the remaining distal end of UA was then coagulated and divided on both sides.
Before colpotomy, the vaginal cuff was fixated using a single late absorbable suture that was passed in a purse string fashion previously described by Bakay K as a novel technique in cuff closure approach.
Afterwards the vaginal wall was completely separated from the cervix using an ultrasonic scalpel above the uterosacral ligaments and after specimen removal was completed, tying loose ends of the previously passed suture firmly closed the vault and concluded the procedure [12].
Considering a potential risk of 10% loss to follow-up, we intended to randomize
110 patients. Descriptive statistics for continuous variables are expressed as
mean
A total of 105 patients underwent TLH. Patients were divided into two groups:
ligation positive group LN (+) (n = 52) and ligation negative group LN (-) (n =
53). The groups were similar with respect to age (p = 0.387 and
p
Weight of specimens (uteri) removed were measured by the department of pathology.
| Ligation (+) (n = 52) | Ligation (−) (n = 53) | p values | ||
| Age | 51.28 |
49.32 |
0.387 | |
| Body mass index | 28.72 |
30.49 |
0.412 | |
| Nulliparity | 5 (9.6%) | 4 (7.5%) | 0.741 | |
| Previous c/s | 11 (21.2%) | 9 (17.0%) | 0.384 | |
| Previous pelvic surgery | 7 (13.5%) | 6 (11.3%) | 0.485 | |
| Indications for surgery | ||||
| Myoma uteri | 17 (32.7%) | 12 (22.6%) | 0.281 | |
| Endometrial hyperplasia | 10 (19.2%) | 16 (30.2%) | 0.259 | |
| Benign adnexial mass | 7 (13.5%) | 4 (7.5%) | 0.359 | |
| Persistent menorrhagia | 18 (34.6%) | 21 (39.7%) | 0.687 | |
| * p | ||||
There was a statistically significant difference in operating times between two
groups. Duration of operation was found to be longer in the ligation positive
group (57.15
There were no intraoperative complications encountered in the ligation positive group. However, two patients in the ligation negative group had urinary tract injury (n = 2, 3.77%). A bladder perforation in one patient was managed laparoscopically without any further complications (n = 1, 1.9%). The other urinary tract injury was a ureter laceration (n = 1, 1.88%) and there was a need for conversion to laparotomy in the ligation negative group (n = 1, 1.88%).
There was no need for conversion to laparotomy in the ligation positive group but there was the need to convert to an open approach in two patients in the ligation negative group (n = 2, 3.77%). Laparotomy was performed in a patient with ureter laceration (n = 1, 1.88%) and in a patient due to uncontrolled hemorrhage from the uterine artery trace (n = 1, 1.88%).
One patient in the ligation positive group developed postoperative subileus and one patient in the ligation negative group developed pelvic abscess which were both successfully treated medically (n = 1, 1.9%, n = 1, 1.88%). All patients were discharged at day 2 and were put on regular follow up at day 7, day 30 and day 180 (Table 2).
| Ligation (+) (n = 52) | Ligation (−) (n = 53) | p values | ||
| Duration of operation (min) | 57.15 |
53.66 |
0.018* | |
| Blood loss (mL) | 73.84 |
113.96 |
0.001* | |
| Weight of uterus (g) | 201.38 |
219.64 |
0.153 | |
| Intra-operative complications | ||||
| Urinary tract injury | 0 | 2 (3.77%) | 0.252 | |
| Vascular injury | 0 | 1 (1.88%) | 0.494 | |
| Bowel injury | 0 | 0 | N.A | |
| Post-op complications | ||||
| Cuff dehiscence | 0 | 0 | N.A | |
| Pelvic abscess | 0 | 1 (1.88%) | 0.495 | |
| Ileus | 1 (1.9%) | 0 | 0.505 | |
| Convert to laparotomy | 0 | 2 (3.8%) | 0.252 | |
| * p | ||||
Internal iliac artery (IIA) ligation is a safe, rapid and very effective method of controlling bleeding from the genital tract, even in the most catastrophic situations, especially where no definitive bleeding point is detectable [13]. Bilateral internal iliac artery ligation reduces pelvic blood flow by 49% and pulse pressure by 85% resulting in venous pressures in the arterial circuit, thus promoting hemostasis [14]. Within seconds of ligation, blood enters the collaterals in retrograde fashion. Collateral arterial circulation will make up for the blood that was previously being supplied by the internal iliac artery. The main artery that collateral circulation comes from is the deep femoral artery [15]. Various anastomoses aid in re-vascularizing the internal iliac artery area such as superior gluteal artery and lateral femoral circumflex artery, obturator artery and medial femoral circumflex artery. In females, blood also flows to the uterus via the ovarian artery and after bilateral internal iliac artery ligation reproductive potential is not significantly affected, and it is still possible to have term pregnancies in many of the cases [16, 17, 18].
Regarding UA ligation, Poojari VG et al. stated that they used late
absorbed suture material in ligating UA prior to TLH or used bipolar energy
modality for coagulation and they also observed that the duration of operation
got approximately 11 minutes longer with this technique but peroperative
hemorrhage decreased substantially. However, the authors warned that there was a
risk of ureteral trauma when the suturation point was far into the uterus [4].
Similarly, Lee JE et al. [5] used hemostatic clips for hemostasis in UA.
They stated that clip application was resistant against inflammation but it
raised the cost per case by USD 10.70 [5]. Kale A. et al., found out
that hemorrhage was significantly low (p
This anatomical point is in close proximity to ureters and requires a surgical intervention that would necessitate further dissection cranially from IIAD to reach UA [3, 4, 5].
On the other hand we observed that IIAD which lies in a more proximal and elevated plane is easier to reach and more distant to the ureters compared to UA.
In addition, Peters et al. [11] suggested that the entire trace and exit point should be observed retroperitoneally for a safe hemostasis in UA ligation. The reason for this is that in about 20% of the cases, it is possible for UA to originate from superior gluteal, internal pudendal, or obturator artery [19].
Unilateral or bilateral ligation of the internal iliac arteries decreases blood flow to the bladder, which shows a complete recovery two weeks postoperatively in rat models [20]. Bilateral internal iliac artery ligation causes a temporary decrease in blood flow to the pelvic organs but the reduction is not great enough to induce necrosis histologically [21]. Most of the complications due to ligation of IIAD are seen in old patients with atherosclerotic disease [22].
Serial Doppler studies show that IIAD ligation does not block uterine and ovarian perfusion, and even reduces the impedance of the uterine arteries [23]. It was estimated that internal iliac artery ligation has minimum operative complications and a short learning curve [24].
In our study, when this technique was used the duration of the operation got
longer approximately 3 minutes (min) (57.15
In this method, not only we found out that it is easier to ligate IIAD compared to other surgical techniques focusing on UA but it also allows for better control of the retroperitoneal area during the procedure therefore minimizing the risk of surgical complications such as ureter damage.
Moreover, as was hypothesized, IIAD ligation dramatically reduced blood loss during the operation therefore verifying its utilization in more complex hysterectomies and pelvic lymphadenectomy of which we obtained promising results in another trial.
The ligation of IIAD in this method was applied in a far and safe distance from ureters by forming “Delta 1 triangle” enabling a successful ligation and hemostasis that can be ensured despite anatomic variations in UA origin.
Nevertheless, there is obviously a need for extensive, prospective, randomized and controlled studies for the routine application of this technique whose positive effects we have identified on peroperative results.
KB: designed the research study and performed the research, provided help and advice on writing. AY: designed the research study and performed the research, provided help and advice on writing. ÜK: designed the research study and performed the research, provided help and advice on writing. IY: provided help and advice on writing. ŞH: provided help and advice on writing. AB: analyzed the data. DG: provided help and advice on writing. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Ondokuz Mayis University Medical Faculty Ethics Committee, OMU KAEK 2017/42, ODM.0.20.08/706-814.
Thanks to all the peer reviewers for their opinions and suggestions.
This research received no external funding.
The authors declare no conflict of interest.
