Background: Robert’s uterus is a rare müllerian duct anomaly described as an asymmetric septate uterus with a noncommunicating cavity. Its main presentation is recurrent cyclical abdominal pain. However, patients with Robert’s uterus may present with recurrent pregnancy loss and infertility. Case: We herein report a rare presentation of Robert’s uterus in a 23-year-old woman who suffered from primary infertility without a history of dysmenorrhea. Preoperative two-dimensional ultrasound (2D-US) suggested that the patient only had a partial septate uterus. A hysteroscopy found only the right side of the uterine cavity with a narrow channel while the left uterine cornua and left tubal ostium were not visualized. Intraoperative transabdominal 2D-US confirmed that there were two uterine cavities, a blind hemi-cavity, and a contralateral communicating hemi-cavity. Subsequently, the asymmetric septum was successfully removed by ultrasound-guided hysteroscopy. Conclusion: For patients diagnosed with septate uterus by 2D-US, three-dimensional ultrasound or magnetic resonance imaging is required to make a definitive diagnosis and to help with surgical planning. If results are inconclusive, intraoperative ultrasound-guided hysteroscopic metroplasty may be a reliable pathway for the definitive diagnosis and treatment of Robert’s uterus.
Robert’s uterus is a rare müllerian duct malformation first reported in 1970 by Robert [1]. Morphologically, the uterine cavity is asymmetrically divided into two cavities by an oblique septum: a noncommunicating blind uterine horn and a contralateral unicornuate uterine cavity which normally connects with the cervix. The oblique septum can completely obstruct the flow of menses leading to hematometra, retromenstruation and development of endometriosis. The main symptom is cyclic or chronic pelvic pain beginning at menarche. Here, we describe a case of Robert’s uterus presenting as primary infertility without any previous dysmenorrhea, and with hematometra in the blind uterine horn. Although this patient was preoperatively misdiagnosed as partial septate uterus, she was successfully diagnosed by intraoperative ultrasound and treated with ultrasound-guided hysteroscopic metroplasty.
A 23-year-old woman presenting with a 1-year history of infertility was diagnosed as partial septate uterus at a previous hospital. She was transferred to our hospital in March 2018 with a provisional diagnosis of partial septate uterus and was then scheduled for hysteroscopic septum resection. Her menstrual cycles were regular at a 28-day interval for 5 days and there was no history of dysmenorrhea.
Gynecologic examination showed a uterus of normal size and an anatomically normal vagina and cervix. Two-dimensional ultrasound (2D-US) revealed the following (Fig. 1A): the uterus was anterior; the contour of the fundus was smooth; the endometrium measured about 0.6 cm in thickness; the thickness of the septum at the fundal midline was about 0.4 cm; Y-shaped separation of the endometrium was noted at the endometrial cavity and the site of endometrial fusion was approximately 3.0 cm from the top of the fundus. Moreover, the bilateral ovaries and kidneys were normal. No effusion was found in the abdominopelvic cavity.
 Fig. 1.
Fig. 1.Ultrasound and hysteroscopic findings of the case. (A) Preoperative Sonogram. Transabdominal ultrasound images show the septum (arrowhead) dividing the uterine cavity into two parts; no connection between the right and left endometrium (white arrow) in the upper part of the uterus was detected. (B,C) Intraoperative sonogram. Images show that the right uterine cavity (white arrow) was filled with saline, but no anechoic area generated by saline was detected in the left cavity (black arrow). (D) The needle electrode was placed in the weakest point of the oblique septum and commenced resection of the septum.
Three days following admission, hysteroscopic metroplasty with ultrasound guidance was done under general anesthesia. On a diagnostic hysteroscopy, the following was noted: the uterine cavity had a small-diameter narrow channel and the ostium of the right fallopian tube was covered by endometrial polyps; the left side of cornua uteri was obscured. Intraoperative ultrasound showed two closely separated endometrial cavities. A thin isoechoic septum, measuring about 0.4 cm between the two endometrial cavities, was displayed. In addition, the right cavity was filled with echogenic fluid generated by saline, while no anechoic area was detected in the left cavity (Fig. 1B,C). We concluded that the left uterine cavity may be completely occluded by the septum. The resectoscope was inserted into uterine cavity by dilating the cervical canal gradually with a cervical dilator. With the guidance of ultrasound, the needle electrode was placed in the weakest location of the septum and moved horizontally to the other side (Fig. 1D). Once the echogenic gas caused by the resection of septum was detected by ultrasound at the left uterine cavity, it meant the septum had been penetrated. With the puncture point as the center, the resection area was gradually expanded and the strong echogenic gas in the left uterine cavity gradually increased (Fig. 2A). After accessing the left uterine cavity, a thick oblique septum was recognized extending from the fundus midline to the left side of the internal cervical os, completely blocking the left cavity. Then the incision of the septum was continued and extended to the uterine fundus (Fig. 2B). The left cavity was relatively small compared with the right one and the ostium of the left fallopian tube could be seen at the left cornua uteri. With these findings, a diagnosis of Robert’s uterus was made. The oblique septum was then resected completely by loop electrode and the uterine cavity was restored roughly (Fig. 2C,D). Following the reinjection of distention fluid into the uterine cavity, the sonogram showed the disappearance of isoechoic septum (Fig. 3A), and after extracting the distention fluid, the shape of uterine cavity was generally restored to normal (Fig. 3B). Foley’s catheter was placed in the uterine cavity and 5 mL saline was filled in the sacculus to facilitate drainage and prevent adhesion. Ultrasonography after three months showed that the uterine cavity shape was closer to normal.
 Fig. 2.
Fig. 2.The oblique septum was resected gradually. (A) Transabdominal transverse image showing a small amount of strong echo in the left uterine cavity (white arrow) indicating that the needle electrode has just penetrated the oblique septum. With the increase of cutting range, the echogenic gas in the left uterine cavity (black arrow) increased gradually. (B) After revealing the left uterine cavity, the incision of the septum was continued and extended to the uterine fundus. (C) Transabdominal sagittal and transverse images show that the echogenic gas (black arrow) has filled the uterine cavity, indicating that most of the oblique septum has been removed. (D) Resection of the remaining septum using a ring electrode; the uterine cavity was restored roughly.
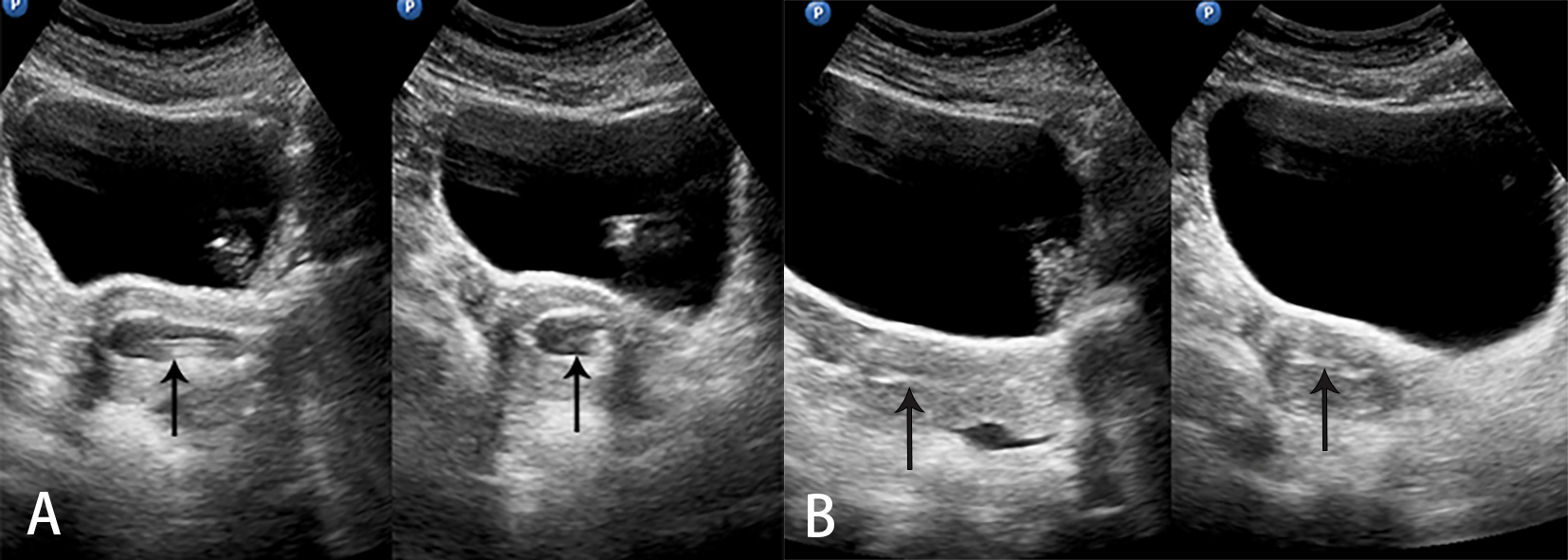 Fig. 3.
Fig. 3.The oblique septum has been completely removed. (A) Transabdominal sagittal (left panel) and transverse (right panel) images show that echogenic fluid filling the uterine cavity (black arrow). (B) After extracting the distention fluid, the uterine cavity (black arrow) regains its normal shape.
Robert’s uterus is a rare congenital Müllerian duct anomaly (MDA) first described by Robert in 1970 [1]. It is characterized by a condition whereby the uterine oblique septum asymmetrically divides the uterine cavity into a non-communicating blind hemi-cavity and a contralateral unicornuate uterine cavity. After menarche, the menstrual blood in the blind cavity accumulates gradually due to its inability to be discharged, causing hematometra, hematosalpinx, and sometimes endometriosis [2]. The main symptom is gradually increased cyclic pelvic pain beginning at menarche. Musset and Poitout characterized Robert’s uterus as including: (i) primary dysmenorrhea; (ii) discordance due to normal laparoscopic appearance and hysterographic appearance of the unicornuate uterus; and (iii) absence of anomalies of the urinary system [3]. However, this conventional view was challenged by new findings. Yang et al. [4] reported a case of Robert’s uterus with an ipsilateral renal anomaly. In addition, Wang et al. [5] reported a case of Robert’s uterus without a history of dysmenorrhea and the patient in question was suspected of uterine malformation due to recurrent miscarriages. According to the American Society for Reproductive Medicine (ASRM) classification, Robert’s uterus is a rare type of class VB. The European Society of Human Reproduction and Embryology (ESHRE) and the European Society for Gynecological Endoscopy (ESGE) classification describes this anomaly as a complete septate uterus with unilateral cervical aplasia (U2bC3V0); however, there is no explanation for the diagnosis of unilateral cervical aplasia [6]. Ludwin et al. [7] speculated that the origin of this defect may be segmental agenesis of the isthmus (presence of external indentation) with a lack of reabsorption of the septum between upper regions of the müllerian ducts. At present, the classification of this anomaly is still debatable and further study in the etiopathogenesis of Robert’s uterus is necessary.
Robert’s uterus consists of three main clinical types: (i) with large hematometra in the blind hemi-cavity and acute pelvic pain; (ii) with an inactive blind hemi-cavity without hematometra and recurrent miscarriages; (iii) with small hematometra in the blind hemi-cavity [8]. Our case can be categorized as the second type. This patient did not have any previous dysmenorrhea; ultrasound examination only found only two closely separated endometrial cavities and a smooth fundal contour. In addition, no characteristics of hematometra, hematosalpinx, or endometriosis were detected. Based on the negative features on the sonogram, previous examinations misdiagnosed it as a partial septate uterus. Singhal et al. reported a woman with a 26-week pregnancy in the blind cavity of Robert’s uterus. She did not have any preceding history of dysmenorrhea. Hysterotomy followed by extraction of the macerated stillborn fetus and ipsilateral tubal ligation was performed. There was no collection in the blind cavity on ultrasonogram six weeks postoperatively, and still no symptom of dysmenorrhea or cyclic lower abdominal pain three months after the surgery, suggesting that the endometrium lining the blind cavity was only partly functional, insufficient to cause menstrual blood retention but enough to support a pregnancy [9].
When an MDA is suspected, evaluation and diagnosis are mainly based on imaging modalities, including hysterosalpingography (HSG), magnetic resonance imaging (MRI), and ultrasound (US). HSG provides excellent information for the evaluation of the uterine cavity and fallopian tubes, but not the external uterine contour, so it cannot differentiate between Robert’s uterus and hemi-uterus with or without a rudimentary cavity. Furthermore, the patients under examination are inevitably exposed to ionizing radiation. MRI has the advantages of noninvasive, multiplanar capability and, excellent soft-tissue characterization, and as such is the best modality to demonstrate the uterine septum, normal external fundal contour, hematometra and hematosalpinx [10]. Accordingly, MRI is the “gold standard” for diagnosing Robert’s uterus. 2D-US provides a convenient and real-time way of displaying uterine anomalies, but fails to adequately show the coronal plane of the uterus. Thus, it is difficult to distinguish Robert’s uterus with large hematometra in blind hemi-cavity from a functional rudimentary uterine horn. Moreover, Robert’s uterus without hematometra in blind hemi-cavity can also be easily misdiagnosed as a septate uterus. Three-dimensional ultrasound (3D-US) is capable of displaying the coronal plane of the uterus and showing both the internal and external contours of the uterine fundus. 3D-US has a good level of agreement with MRI in diagnosing uterine malformations based on ESHRE–ESGE consensus [11]. Additionally, modern ultrasound techniques, such as three-dimensional saline contrast sonohysterography, can be useful for a precise diagnosis of Robert’s uterus, surgery planning, guidance for hysteroscopy, and postoperative assessment [4, 8]. Nonetheless, the patient in our report did not undergo further 3D-US or MRI since all ultrasonic features before surgery indicated a diagnosis of partial septate uterus. We advise that it is difficult to distinguish Robert’s uterus without hematometra from the partial or complete septate uterus by the 2D-US, and that further evaluation via 3D-US or MRI is necessary.
Surgical correction is an effective intervention for Robert’s uterus and most uterine oblique septa can be successfully removed hysteroscopically. The minimally invasive hysteroscopic metroplasty is usually monitored by ultrasonography, laparoscope, or both. A prospective study showed that real-time US guidance, compared with laparoscopic guidance, is a non-invasive and low-cost technique during the performance of operative hysteroscopy and can completely visualize the whole thickness of the uterine wall, entirely resect the septa, simultaneously show the abdominal and intrauterine cavities and avoid uterine perforation [12]. The outcome of the present case also suggests that ultrasound-guided hysteroscopic metroplasty is a suitable procedure. Moreover, intraoperative US monitoring can also remedy the underdiagnosis made preoperatively. In our case, only the right uterine cavity was found by hysteroscopy, which was inconsistent with ultrasonic manifestations. When distention fluid was perfused into the uterine cavity, no echogenic fluid could be detected in the left cavity. Based on ultrasound and hysteroscopy findings, a diagnosis of Robert’s uterus was considered. Although the echogenic gas caused by cautery can interfere with the observation of the electrode, the presence of echogenic gas in the left uterine cavity suggests that the needle electrode had penetrated the oblique septum. Further cautery was thus suspended in order to avoid injury of the contralateral uterine wall and decrease the risk of perforation. Subsequently, reinjection of the intrauterine distending medium was able to further discern the morphology of the uterine cavity and the extent of septal resection.
Robert’s uterus without hematometra in blind hemi-cavity is easily misdiagnosed preoperatively as partial or complete septate uterus. Additional imaging methods, such as 3D-US or MRI, are typically required to provide accurate diagnostic information for complicated uterine anomalies. If the definitive diagnosis is not made preoperatively, intraoperative ultrasound-guided hysteroscopic metroplasty may be a reliable modality for the diagnosis and treatment of Robert’s uterus.
YHG and DYW designed the research study. JCW and CS wrote the manuscript. CS and QH edited the image. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
This study was approved by the Ethics Committee of Shandong Provincial Hospital (SWYX:NO.2021203). Due to the retrospective design of the study an informed consent is not applicable.
Thanks to all the peer reviewers for their opinions and suggestions.
This research was supported by the Scientific Research Foundation of Shandong Provincial Hospital Affiliated to Shandong First Medical University (2020FY006).
The authors declare no conflict of interest.
