In 1908, Fritz Frank, a German obstetrician, introduced a supravesical extraperitoneal cesarean section (EPCS) in the pre-antibiotic era, called suprasymphysic cesarean section, after which Latzko described the paravesical approach. In both cases, it is necessary to perform blunt dissection and distortion of urinary bladder where vesical nervous and venous plexus cross in the vesicouterine space. This technique was for decades reserved for septic conditions, protracted dystocia, and intra-abdominal adhesions after severe past infections and plastic peritonitis [1]. Although EPCS has been used for more than a century and evaluated in numerous literature reports along with description of potential complications, in recent years it has been revived in several papers and recommended as an outpatient procedure with minimal complications [2].
Twenty years ago, Stark introduced a minimalist transperitoneal approach to cesarean section with bladder omission without peritonization, which has become a state-of-the-art technique worldwide. Habek has introduced his own modification without bladder catheterization, without bladder omission and peritonization, but with rapid recovery of operated mothers with results comparable to those reported by the authors of the modified extraperitoneal technique [3]. According to the obstetric surgical philosophy, placental percretism in the bladder will occur if the bladder is retracted through a hysterotomy, which is necessary in EPCS and Dörffler cesarean section technique. Current pandemic of cesarean sections performed outside the given framework of good clinical practice is accompanied by a consequent increase in invasive malplacentation with an increase in maternal morbidity and mortality due to obstetric shock and destruction of pelvic organs and the need for mutilating pelvic surgery [4].
In our own work, we did not notice invasive malplacentation into the bladder in subsequent pregnancies with Stark’s (Misgav Ladach) technique and Habek’s modification, while all mothers with invasive malplacentation underwent Dörffler technique, which is the preparation (omission) of the bladder and vesicouterine plication (Fig. 1), i.e., covering isthmic hysterotomy [5]. To the best of our knowledge, there are no published papers on the incidence of placental percretism and cesarean section techniques, EPCS in particular, although invasive malplacentation has been described in corporeal cesarean section and uterine myoma enucleation.
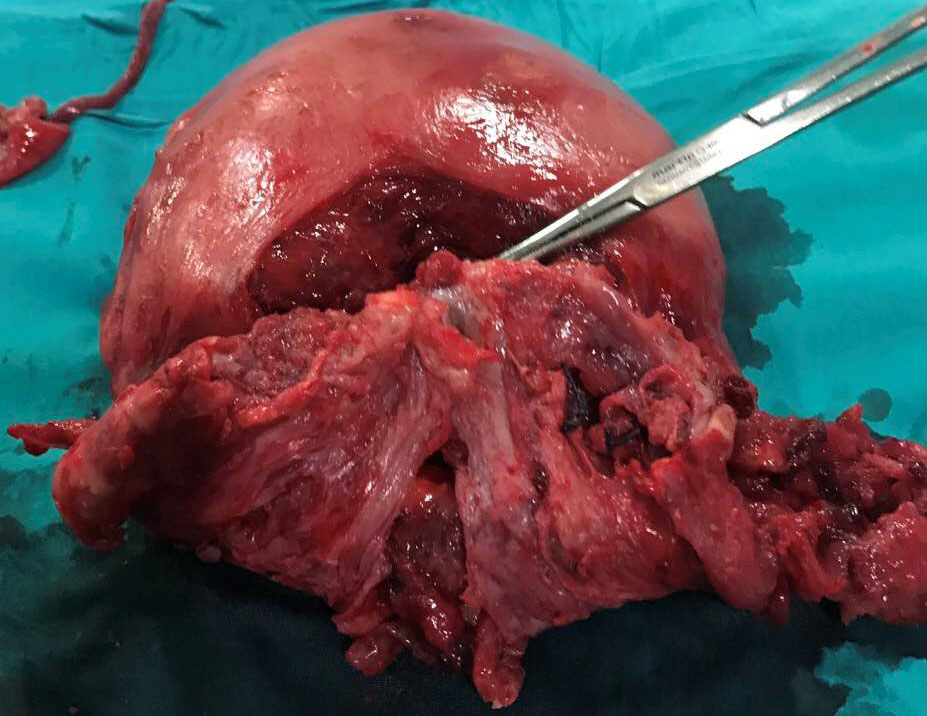 Fig. 1.
Fig. 1.Praevial placental percretism into urinary bladder with destroyed lower uterine segment after bladder plication.
Therefore, as clinicians-operators, we must ask ourselves whether EPCS may be a major risk factor for invasive bladder malplacentation due to surgical technique. Future studies should demonstrate justification of EPCS for future pregnancies, not just the current favorable and safe effect of surgery compared to the existing surgical techniques. Thus, the possible recommended techniques of revitalization of old techniques will get a professional, scientific but also ethical component, bona fide for our pregnant women and by preventing the possible occurrence of conflicts of operative obstetrics thesis-antithesis.
DH conceived, designed and wrote designed the paper.
Not applicable.
Not applicable.
This research received no external funding.
The author declares no conflict of interest. DH is our Guest Editor, given his role as Guest Editor, had no involvement in the peer-review of this article and has no access to information regarding its peer-review.
