Wandering spleen is a rare disease resulting from weakness or absence of the ligaments that hold the spleen in its normal position. The hormonal changes and physiologic splenomegaly that occur during pregnancy can induce ligamentous laxity of the spleen. Generally, wandering spleen is easily diagnosed because it is found in an abnormal position upon abdominal computed tomography (CT). However, wandering spleen in the left upper quadrant may be more challenging to diagnose. The treatment for wandering spleen is surgery with the goal of saving the spleen. Presented here is a case of a 34-year-old postpartum female who visited the emergency department of our hospital with severe epigastric pain. Abdominal CT revealed a whirl sign of the spleen located in the left upper quadrant without splenic infarction. She was discharged with the diagnosis of non-specific abdominal pain because her symptoms improved despite her abnormal CT findings. However, she returned to the hospital with abdominal pain after 1 week. Abdominal CT was performed and revealed splenic infarction. If diagnosis is delayed, the spleen cannot be spared due to the development of splenic infarction. Therefore, if the abdominal CT of postpartum women suggests wandering spleen (i.e., whirl sign), a surgical consultation is essential.
Wandering spleen is a rare disease with an incidence lower than 0.2% that results from weakness or absence of ligaments that keep the spleen situated in a normal left upper quadrant abdominal position [1, 2]. As ligament support is weakened, hilar torsion of the spleen can occur, eventually resulting in splenic infarction. The causes of this disease have not been clearly identified, but the disease has been classified into the congenital and acquired types.
During pregnancy, the positions of the internal organs change and abdominal pressure increases as the fetus grows. The development of splenomegaly may cause the ligaments of the spleen to separate [3]. Here, we present a rare case of postpartum splenic infarction due to wandering spleen one month after delivery.
A 34-year-old female visited the emergency department of our hospital with severe epigastric pain, nausea, and vomiting for 1 day. We found out that she had underwent appendectomy 4 years before her visit, and gave birth 1 month prior to her visit. Also, she had esophagogastroduodenoscopy 2 weeks before the visit due to epigastric soreness and it showed no specific findings. So, through these past history, we excluded both the appendicitis and gastric ulcer from the diagnosis. Her vital signs were blood pressure, 130/80 mmHg; pulse rate, 84; respiratory rate, 20; and temperature, 39 ℃. The physical examination results were significant for mild epigastric tenderness. The laboratory studies disclosed the following values: white blood cell count, 7.88 × 103/μL (normal range 4 × 103 to 10 × 103/μL); hemoglobin level, 13.4 g/dL (normal range 13 to 17 g/dL); platelet count, 217 × 103/μL (normal range 150 × 103 to 450 × 103/μL); blood urea nitrogen, 10.7 mg/dL (normal range 8 to 20 mg/dL); creatinine, 0.8 IU/L (normal range 0.5 to 1.2 IU/L); aspartate aminotransferase, 21 IU/L (normal range 5 to 45 IU/L); alanine aminotransferase, 32 IU/L (normal range 0 to 40 IU/L); and total bilirubin, 0.57 IU/L (normal range 0.2 to 1.2 IU/L).
Although pain was alleviated with medication, an abdominal computed tomography (CT) was performed to exclude intra-abdominal adhesion since the patient had a previous appendectomy and presented with severe abdominal pain. The abdominal CT revealed heterogeneous parenchymal enhancement of the spleen and a whirl sign of the splenic hilum (Figure 1). The general surgeon examined the patient and, upon pain relief, the patient was discharged. The diagnosis at discharge was non-specific abdominal pain.
 Figure 1.
Figure 1.— Abdominal CT at the time of the initial visit revealed heterogeneous parenchymal enhancement of the spleen and a whirl sign of the splenic hilum (arrow: whirl sign).
The patient returned to the hospital with left-side abdominal pain and nausea after 1 week. The initial vital signs were stable: blood pressure, 120/84 mmHg; pulse rate, 96; respiratory rate, 16; and temperature, 36.4 ℃. The physical examination results were significant for tenderness at the left-side abdomen, without rebound tenderness. The laboratory findings, however, were not significant, as follows: white blood cell count, 6.83 × 103/μL (normal range 4 × 103 to 10 × 103/μL); hemoglobin level, 13.5 g/dL (normal range 13 to 17 g/dL); platelet count, 193 × 103/μL (normal range 150 × 103 to 450 × 103/μL); blood urea nitrogen, 9.8 mg/dL (normal range 8 to 20 mg/dL); creatinine, 0.7 IU/L (normal range 0.5 to 1.2 IU/L); aspartate aminotransferase, 20 IU/L (normal range 5 to 45 IU/L); alanine aminotransferase, 22 IU/L (normal range 0 to 40 IU/L); total bilirubin, 0.57 IU/L (normal range 0.2 to 1.2 IU/L); and lactate, 0.81 mmol/L (normal range 0.5 to 2.0 mmol/L).
An abdominal CT was conducted and revealed splenomegaly and splenic infarction (Figure 2). Thus, a laparoscopic splenectomy was performed and spleen infarction due to splenic torsion was discovered (Figure 3). Antibiotic chemoprophylaxis and vaccination against Haemophilus influenza, meningococcus and pneumococcus were prescribed. The patient was discharged 5 days after the surgery without any complication.
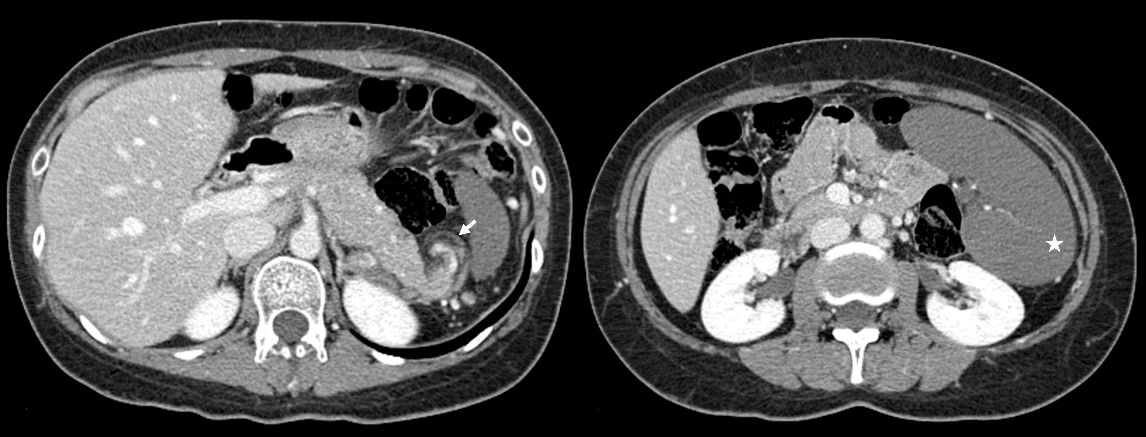 Figure 2.
Figure 2.— Abdominal CT at the time of the second visit revealed splenomegaly and splenic infarction (arrow: whirl sign, asterisk: splenic infarction).
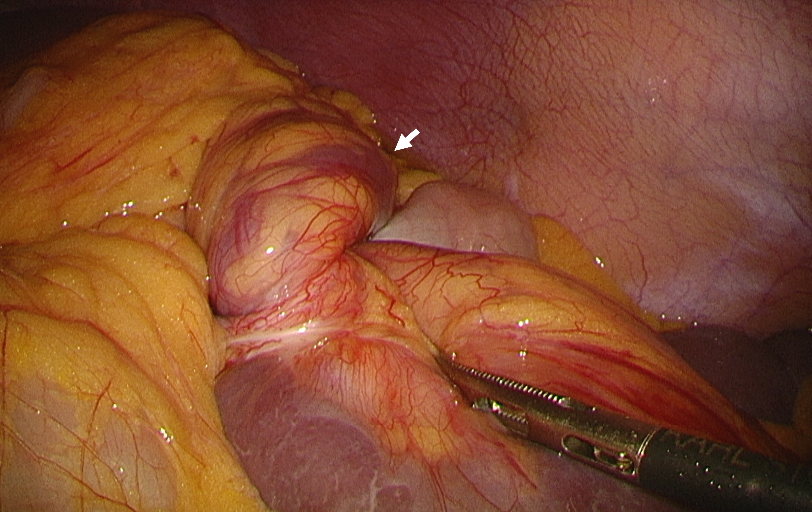 Figure 3.
Figure 3.— Wandering spleen was confirmed on laparoscopy. There was no adhesion to the surrounding structures and the spleen was found twisted three times around its vascular pedicle (arrow: twisted splenic pedicle).
Normally, the spleen is located in the left upper quadrant of the abdomen, inside the 9th-11th intercostal spaces, and is fixed by five ligaments: the lienorenal, splenocolic, splenophrenic, gastrosplenic, and phrenicocolic ligaments [4]. When these ligaments become weak or are absent, the spleen becomes free to move in a state called “wandering spleen” or “ectopic spleen”, first described in 1854 [5]. As there are arteries, veins, lymphatics, and nerves in the splenic hilum, hilar torsion can occur, which can cause splenic infarction with acute abdominal pain. Wandering spleen is commonly located in an abnormal position, such as the periumbilical area, but it can also be located in the normal left upper quadrant. In the present case, the spleen was located in the left upper quadrant of the abdomen and, if hilar torsion had not occurred, it would have been misdiagnosed.
Although wandering spleen occurs very rarely, it is usually congenital, with 1/3 of the cases happening in children below the age of 10 years [6]. In adults, it may be caused by trauma, pregnancy, or splenomegaly [7]. The hormonal changes and physiologic splenomegaly that occur during pregnancy can induce ligamentous laxity of the spleen [8]. In addition, as the intra-abdominal pressure increases due to pregnancy, especially in multipara, laxity of abdominal wall could be allied with dependency and elongation of the pedicle [8]. The clinical features may vary from asymptomatic to chronic and vague pain or acute pain due to torsion [8]. In the present case, the patient had acute epigastric pain, which subsided after medication. However, acute-onset abdominal pain recurred after 1 week. It is likely that the spleen torsion was naturally addressed but reoccurred after 1 week. Since the patient experienced abdominal pain 1 month after the delivery, the wandering spleen may have developed during pregnancy by hormonal change and increased intra-abdominal pressure, and remained asymptomatic until presentation at the hospital.
The diagnosis of wandering spleen is based on radiological findings rather than clinical features. The best imaging tool is contrast-enhanced CT. Usually it is easily diagnosed because most of the time the wandering spleen is located in areas other than left hypochondrial region, the normal position. In addition, vascular engorgement, whirling of the vascular pedicle, and splenomegaly due to hyper-congestion may also appear [9]. In the present case, the diagnosis was challenging due to the normal position of the spleen on the initial CT. The diagnosis was made after observation of hilar torsion found in the follow-up CT image taken a week later.
The treatment of choice for wandering spleen is surgery, with two methods usually considered: splenectomy and splenopexy [10, 11]. Splenopexy is a spleen-preserving strategy that is used to prevent post-splenectomy septicemia in children [12]. Splenectomy is performed in adults when splenic torsion, infarction, thrombosis, or malignancy are suspected [13]. Splenic torsion is a life-threatening emergency requiring immediate surgery. In the present case, the patient was initially discharged from the hospital because her symptoms improved, even though she had hilar torsion of the spleen as seen on the abdominal CT image. She returned to the hospital 1 week later with relapsed abdominal pain and splenic infarction. Therefore, splenic torsion, even if asymptomatic, warrants hospitalization and surgical observation.
A limitation of this study is that it remains unclear when wandering spleen developed. It may have developed congenitally and presented with no symptoms, or it may have been related to pregnancy. Even if it occurred congenitally, the hormonal changes or intra-abdominal structural changes of pregnancy might have influenced its development.
Wandering spleen can often occur in reproductive-aged women, especially during pregnancy or the postpartum period. CT scan should be done if there is doubt. Even if abdominal CT shows normal localization of the spleen, wandering spleen should be suspected if whirling of the hilum of the spleen is observed. If diagnosed or suspected, surgical consultation is essential.
The patient provided written informed consent to publish her anonymous data in the present case report. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Soonchunhyang University Bucheon Hospital (approval number: 2019-04-012).
This work was supported by the Soonchunhyang University Research Fund.
The authors declare no conflict of interest.
