Introduction: Multiparty is a long-standing problem for gynecologists around the world, since in places where multiparity is expressed, researchers are not able to fully examine it, most often because of socio-economic reasons. Objective: The aim of this research was to examine the influence of multiparty (delivery of six or more children ) on pathology of pregnancy and delivery. Materials and Methods: The study included women that were delivered at the Gynecological Clinic of Faculty of Medicine in Pristina during 1992 and 1993, a total of 12, 532. The analysis included impact of multiparity on pathology of pregnancy and delivery. Results: The analysis of the age of patients indicates that the highest number of patients was aged between 18 and 25 years. As an atypical phenomenon, the authors also presented a pelvic presentation, although it cannot be considered a pathological condition, but is listed here because it can give an increased number of birth complications. The percentage of cesarean section in multiparas is growing but not evenly. Multiparity certainly increases its incidence. The abruption of normally inserted placenta is more frequent in multiparas. Placenta previa is also more common in multiparas. Situs transversus indicates an increased number of internal turnings as well as cesarean section. Edema, proteinuria, hypertension (EPH) gestosis at multiparas regularly determines the end of pregnancy with cesarean section. Episiotomy is rare in multiparas. Rh incompatibility is not more frequent at multiparas. Multiparity is also correlated with pathological conditions associated with umbilical cord swelling. Multiparas experience more common bleeding during the third and fourth trimesters. Rupture of amnion is more common in multiparas. Hysterectomy after delivery is significantly dependent on parity. Conclusion: The limit for multiparty was set to delivery of six or more children. Multiparity certainly has an adverse effect on pregnancy. The pathology of pregnancy as well as complications during delivery were increased. Multiparity ultimately poses danger to the pregnant woman.
Multiparty is a long-standing problem for gynecologists around the world, since researchers are not able to fully examine it, most often due to socio-economic reasons. Countries in which studies on the topic of multiparity can be correctly conducted are highly developed, and multiparity occurs rarely or not at all. Therefore research on multiparty is always useful, given that it is most common in underdeveloped and unregulated countries [1-4].
When it comes to reproduction, it does not only implicate the possibility of fertilization. Certainly, reproduction includes a set of biological, cultural, religious, historical, social and many other factors [1, 5]. The family represents a very important social unit, which every new member must introduce into the biological and social hierarchy. There are differences in whether or not reproduction should be limited [3, 6, 7].
Doctors make reference to the harmfulness of uncontrolled reproduction. Furthermore, in the state, the fact is that in addition to healthy childbirths, the child should be allowed to develop normally from many other aspects, social, cultural, etc [2, 5, 6]. If the delivery does not go well, further aspects of life are become more and more complicated. In the period from 1992 to 1993, Kosovo and Metohija experienced the largest population growth not only in Serbia, but also in Europe. This area was multinational: Serbians, Montenegrins, Albanians, Gypsies, Turks, etc., and as such was suitable for objective research. The present authors therefore were able to set up well the research guidelines and collect quality data [2-4].
In determining all the parameters of this study, the authors only managed medical reasons, using adequate statistical data processing [3, 6].
The aim of work is to show the impact of multiparity on the pathology of pregnancy, as well as on delivery, including the way of completing delivery and birth complications, through an analysis of the collected data.
The study included all women who delivered a child at Gynecological Clinic of Faculty of Medicine in Pristina during 1992 and 1993 (a total of 12, 532). The limit for multiparty was set at six or more children.
In statistical data processing, the bifactorial analysis of variable quotients was used in addition to standard statistical indexes (ANOVA).
The analysis of the age of patients indicates that the highest number of patients was between 18 and 25 years (Figure 1).
 Figure 1.
Figure 1.— Age structure of maternity.
Biologically, the movement of childbirth at a younger age is understandable. Age over 45 years is the rarest.
Although pelvic presentation cannot be considered a pathological condition, it is certainly very important, because of the active participation of obstetricians in delivery and because of the increased perinatal morbidity and mortality (Figure 2).
 Figure 2.
Figure 2.— Pelvic presentation according to parity.
It is obvious that the frequency of a pelvic presentation is more frequent when parity is higher. This particularly culminates in patients with seven deliveries.
When it comes to the method of completing delivery with a pelvic presentation, it was common as in other births where the head of the fetus was predominant. It can see on the figure 3.
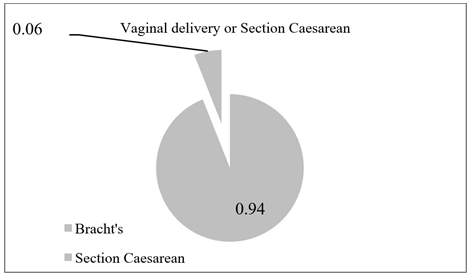 Figure 3.
Figure 3.— Pelvic presentation according to parity,
The number of cesarean sections and the percentage increase with parity, although, this number does not increase evenly (Figure 4). At first, this unevenness may be illogical.
Certainly, by processing data, the authors concluded that multiparity increases the indication for cesarean section.
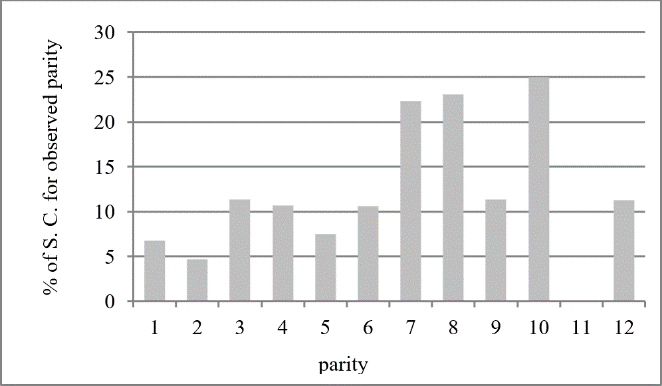 Figure 4.
Figure 4.— Number of cesarean sections according to parity.
Abruption of the normally implanted placenta is convincingly more common in multiparas (Figure 5). Situs transversus, like complication of delivery indicates an increased in the number of cesarean sections as well (Figure 6). Larger number of deliveries is also in correlation with Section Caesarean. Placenta previa is more common at multiparas. The number of cesarean sections with placenta previa can be seen in Figure 7.
 Figure 5.
Figure 5.— Abruption of the normally implanted placenta according to parity.
 Figure 6.
Figure 6.— Cesarean section at situs transversus at parity at 100%.
 Figure 7.
Figure 7.— Cesarean section for placental praevia.
Edema, proteinuria, hypertension (EPH) gestosis in multiparous is almost always followed by the termination of pregnancy. Because of this, cesarean section is much more common in multiparas (Figure 8). Episiotomy is also more common in primiparas than multiparas. This is somewhat simple and logical explanation (Figure 9).
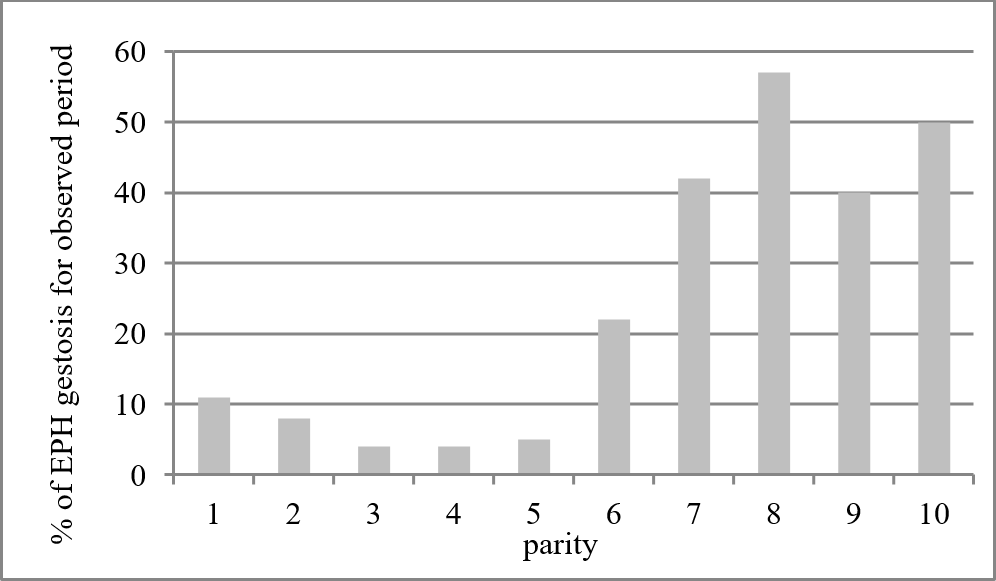 Figure 8.
Figure 8.— Cesarean section at EPH gestosis ccording to parity.
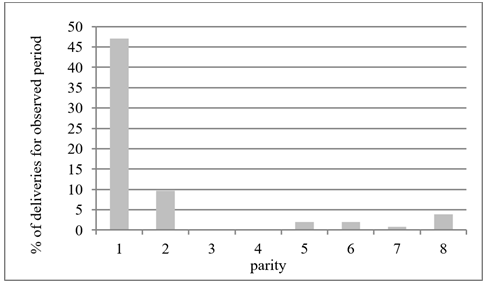 Figure 9.
Figure 9.— Type of delivery with episiotomy.
In the case of Rh incompatibility, the authors did not expect a slight change in relation to parity. Here, they could only assume that multiparity would affect Rh incompatibility due to a possible greater possibility of Rh isoimmunization (Figure 10). Rh isoimmunization can be a crucial factor in deciding to terminate the pregnancy. A decision would be made to avoid the possibility of damaging fetuses in cases of this type of high-risk pregnancy. Multiparity is also in correlation with the pathological conditions associated with wrapping the umbilical cord (Figure 11).
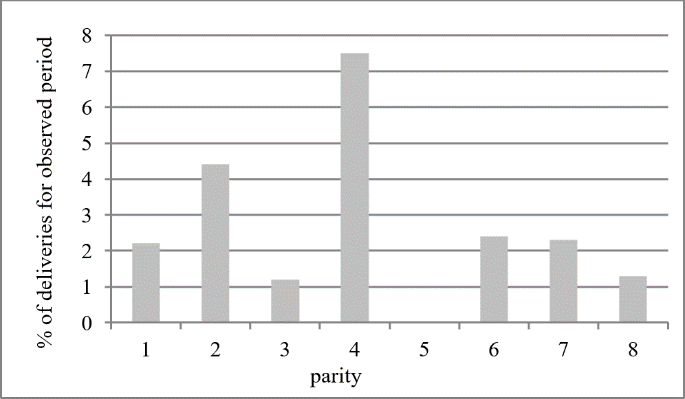 Figure 10.
Figure 10.— Rh incompatibility and parity.
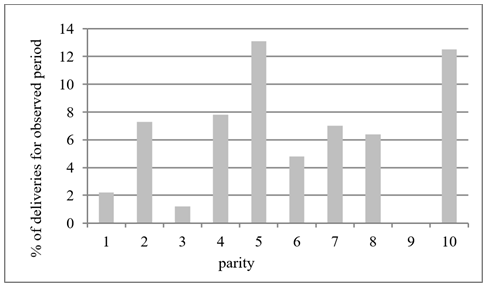 Figure 11.
Figure 11.— Wrapping umbilical cord and parity.
Multiparas experience more common bleeding in the third and fourth trimesters (Figure 12). The most common bleeding occurs due to decreased contractility of the uterus, hypotonia or atonia. It may also occur due to retention of cotyledone of placenta. Multiparity leads to early rupture of amnion because of the weakness of the lower segment of the uterus, especially the internal uterine mouth, which is damaged by previous deliveries (Figure 13). Sometimes in multiparas, even with the smallest contractions, there is a prolapse of amnion and swelling of the amniotic fluid.
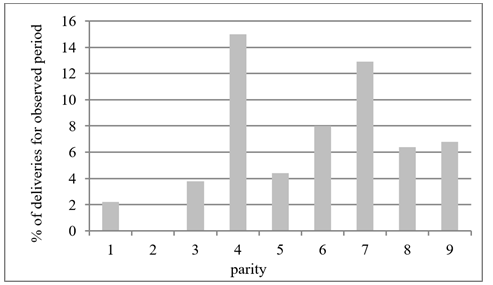 Figure 12.
Figure 12.— Bleeding during delivery according to parity.
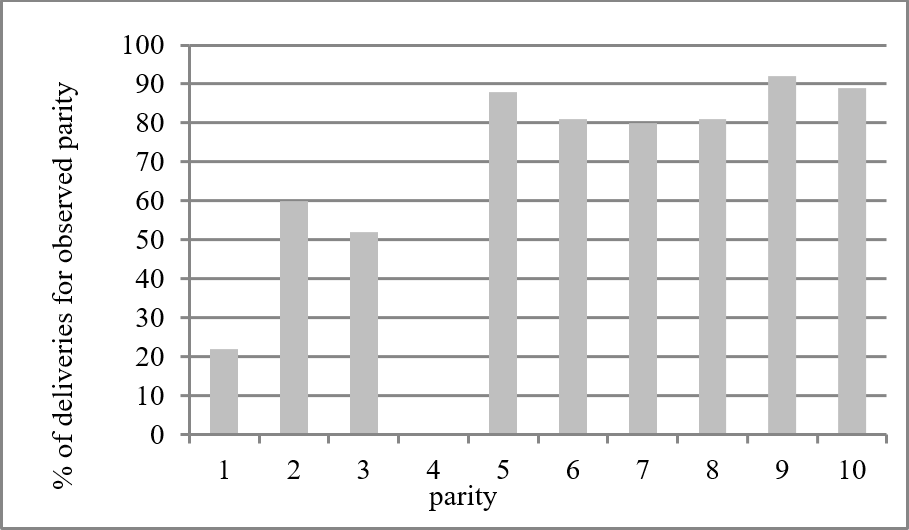 Figure 13.
Figure 13.— Early rupture of amnion and parity.
Hysterectomy has been reported in high-parity women in six and seven deliveries. This group included the largest number of patients. This operation is also more often performed in women with more deliveries. Hysterectomy was performed in 75 women. Previous cesarean section occurred for the first time in 23 patients. Second and third times included incomplete rupture of uterus in 16 patients, and apoplexia uteroplacentari also in 16 patients. Abruptio placentae occurred in eight women and placenta acreta in eight as well.
Because of disseminated intravascular coagulopathy. hysterectomy was performed in four women. The difference between individual parities is statistically significant and is determined by applying the contingency table and the Χ2 test.
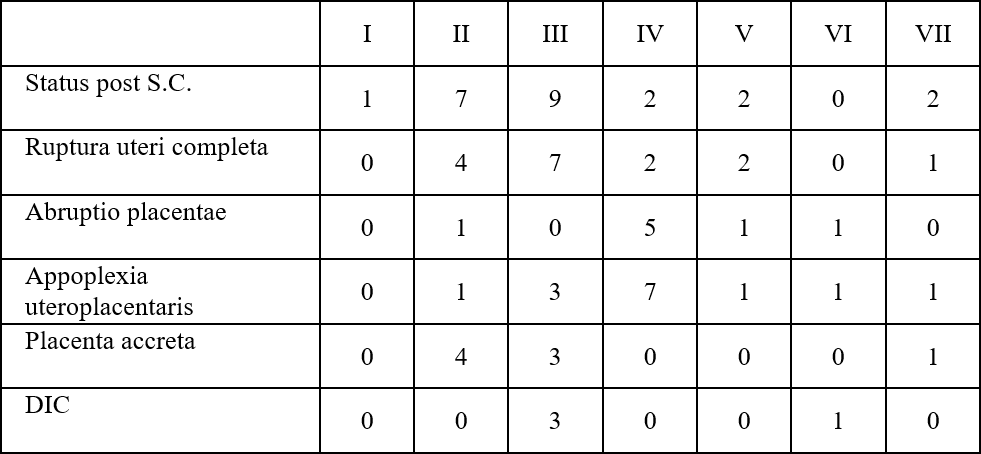 Figure 14.
Figure 14.— Cause of hysterectomy (absolute frequency).
 Figure 15.
Figure 15.— Hysterectomy after delivery according to parity.
The age structure of the mother is indicative of asymmetry towards a younger age. It is biologically understandable. Also, women most often deliver between the ages of 18 and 25 [1, 2]
The number of EPH gestosis increases with multiparity. This increase is not even, but it is common [3].
Pelvic presentation is more frequent when the parity is higher. This is the mostly prevalent inpatients with seven births. The authors did not find a medical explanation for this information [1, 4].
In most cases, pelvic presentation was completed by birth with Bracht manual assistance, and in 6% of cases, a cesarean section was performed [5, 6].
The abruption of normally inserted placenta is more frequent in multiparas [6, 7], and so is the number of situs tranversus, with the corresponding obstetric intervention of cesarean section [5, 6]
The EPH gestosis in multiparas is almost always completed by cesarean section, which is by far the most common in multiparas with EPH gestosis than in all other patients.
Multiparity is alsop correlated with pathological conditions associated with umbilical cord swelling [5-7]. They are also more prone to bleeding during the third and fourth trimesters [2, 3, 6]. This usually occurs due to decreased contractility of the uterus, hypotonia or atonia [4, 6, 7]. It may also occur due to retention of cotyledone of placenta [5, 6].
Rupture of amnion is more common at multiparas [5-7]. Hysterectomy after delivery is also significantly dependent on parity [4, 5, 7]
In conclusion, multiparty - giving birth to six or more children, represents from medical point of view, a higher level of danger both for newborns and pregnant women. Perinatal morbidity and mortality have been increasing and are at high-risk for a women during pregnancy, delivery, and puerperium, which pose a threat to the woman’s life. The presented facts, verified and proved by most up-to-date statistical methods, should be taken into account by family members, as well as other factors that could influence people’s behavior in the field of reproduction from educational to religious and social institutions.
