Objective: By describing a case of vaginal foreign body misdiagnosed as cervical cancer in a female of reproductive age, gynecologists should be warned to be careful in the process of diagnosis and treatment. Materials and Methods: Retrospective review of the entire medical record of a female Tibetan patient who was misdiagnosed with cervical cancer. Results: The patient received hysteroscopy under general anesthesia. Two white plastic bottles for Yunnan Baiyao were found after separating the vaginal stenosis and after removing the vaginal foreign bodies, a smooth and complete cervix was found. Conclusion: This study suggests that gynecologists should be careful with physical examination, as they should ask patients more questions, and not limit their clinical thinking to common diseases, and thereby reducing misdiagnosis to the lowest possible.
Vaginal foreign body is not uncommon in clinic, occurring most commonly in young girls under the age of four years, frequently in adult patients with mental illness, and sometimes in normal adult women [1, 2]. Patients often present increased vaginal discharge accompanied by odor, vaginal bleeding, infection, chronic pelvic pain, dyspareunia, and other symptoms [3]. A lengthy retention time of foreign bodies can cause vaginal discharge accompanied by odor, the proliferation of granulation tissue, vaginal stenosis, and even atresia of the vagina, rectovaginal, urethrovaginal, and vesicovaginal fistulas in severe cases [4-7], which cause great physical and mental pain to patients. This case describes a female of reproductive age with vaginal discharge accompanied by odor of more than six months duration, misdiagnosed as cervical cancer that was due to the long-standing presence of a foreign body.
The 39-year-old female Tibetan patient (G1P0+1) was admitted to this hospital due to “vaginal discharge accompanied by odor for more than six months” on March 25, 2013. Six months ago, the patient presented vaginal discharge without obvious causes, accompanied by irregular vaginal bleeding, while no other discomforts including abdominal pain, hypourocrinia, frequent micturition or sense of fall-swell in the anus occurred. The patient was once treated with anti-infective therapy and symptomatic therapy in a people’s hospital of a county in Tibet, resulting in no improvement in symptoms. In the recent one month, the volume of vaginal discharge presenting as bloody fluid (similar to menstrual blood volume) increased and accompanied by odor, and 7-8 sanitary napkins were needed every day. More than 20 days ago, the patient visited a tumor hospital and was admitted due to “cervical cancer”. After admission, the patient received cervical tissue biopsy which suggested chronic cervicitis, and consequently subjected to leaving hospital without treatment. Half a month ago, the patient visited the outpatient department of this hospital. Physical examination revealed firm upper one-third of the vagina, contact bleeding, an inability to expose the cervix, obviously thickened and shortened bilateral uterus to the pelvic side wall, and no other abnormities. Cervical cancer was suspected, and cervical cytological examination was carried out, which suggested a few changes in atypical squamous cell of undetermined significance (ASCUS), and no detected endocervical cells. Transvaginal ultrasound demonstrated that the uterine body could not be seen, the anterior and posterior diameter of the cervix was 5.1 cm, morphology was abnormal, echoes were mixed and disorderly with evident posterior attenuation, and dotted and linear blood flow signals were detected. In addition, biopsy was performed and the pathological report showed chronic cervicitis accompanied by erosion. A week prior, the patient underwent vaginal wall biopsy in the outpatient operating room of this hospital, and intraoperative findings revealed that there was stale blood and odor in the vagina, the mucosa of the lower one-third of vagina was normal, the upper one-third of the vagina presented obvious stenosis, firm and contact bleeding, and the cervix could not be exposed. The multipoint biopsy of the vaginal wall demonstrated squamous papilloma with the presence of hyperplasia combined with suspected HPV infection. After the discussion of all departments, the patient was highly suspected to have cervical cancer. Four days prior, the patient received vaginoscopy in the outpatient department of this hospital because of no histological evidence: a vaginal speculum was inserted into the vagina by 5 cm; the vaginal apex was closed and could not be exposed, so a small slit in the vaginal apex was separated using a probe; after the probe was successfully inserted, apparent foreign body was detected, and metallic echoes were heard with percussion, which contributed to a consideration of a metal-like foreign body in the vagina. Therefore, pelvic frontal and lateral plane radiographs were conducted immediately, which revealed no metal-like foreign body. When asking medical history, the patient complained that she had not been pregnant after receiving hemostatic therapy in a local hospital in Tibet due to massive vaginal hemorrhage after spontaneous abortion more than ten years ago. The patient had regular menstruation, with hypomenorrhea and dysmenorrhea, and her last menstruation started began on March 1, 2013.
After admission, the patient received examinations under anesthesia. The patient had stable vital signs, and the laboratory examination of blood routine showed a RBC level of 2.53 × 1012/L, a HGB level of 64 g/L, HCT of 21%, and no other obvious abnormities. After her anemia was corrected by 4.5 units of red cell suspension, hysteroscopy was performed under general anesthesia on March 28, 2013. Intraoperative findings revealed that the lower one-third of the vagina was unobstructed and its mucosa was normal, the upper one-third of the vagina presented obvious stenosis, and the cervix could not be exposed. After the adhesion in the site of vaginal stenosis was separated with an expanding uterus stick, 20 ml of a dark red odorous secretion was expelled. Then, the hysteroscope was implanted through the separated vaginal apex, showing two white plastic bottles for Yunnan Baiyao (Figure 1), with a diameter of 3 cm and a height of approximately 4 cm for the larger one, a diameter of 2 cm and a height of 4 cm for the smaller one, and no bottle caps for both of them. The foreign bodies were removed using a vessel forceps. Then, the proliferation of vaginal mucosa and granulation tissue, minor exudative hemorrhage, no damage, and smooth and complete cervix were found. After the surgery, the symptoms of vaginal discharge disappeared, and the patient was cured and discharged.
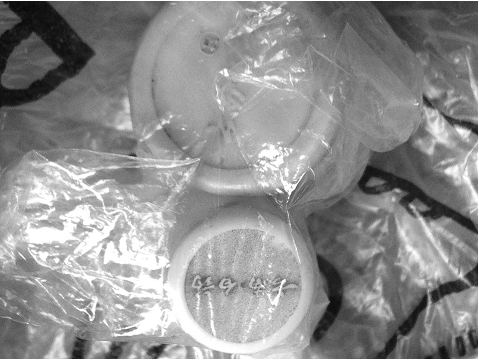 Figure 1.
Figure 1.— Two white plastic bottles for Yunnan Baiyao.
There is a wide variety of foreign bodies, commonly, including vegetables, batteries, pins, hairpins, plastic pen caps, plastic bottle caps, sex toys, etc. There are two cases of adult vaginal foreign body reported in domestic and foreign literatures that are similar to the case in the present report. Ahmidat et al. [8] reported a case of clinically suspected cervical carcinoma. The patient was a 21-year-old female coming from Thailand, who complained of vaginal discharge and vaginal contact bleeding. After admission, physical examination revealed that there was foul liquid flowing out of the vagina, the cervical size was irregular, and a suspected inflammatory mass in the cervix was detected under the vaginoscope. When asking of her medical history, the patient complained of vaginal discharge and transvaginal exhaust two years ago. Barium enema examination showed a rectovaginal fistula. B-mode ultrasonography suggested abnormal cervical morphology, mixed and disorderly echoes with a size of 5.7 × 6.3 cm, and a suspected tumor. However, no abnormities were detected in the uterine body or the fundus of uterus. Additionally, pelvic MRI showed a large cervical polyp involving the vaginal fornix and no lymph node metastasis. After a multidisciplinary discussion, it was decided to perform hysteroscopy, colonoscopy, and cystoscopy under general anesthesia for this patient, to obtain evidence for histological diagnosis. However, a plastic bottle cap was found in the posterior vaginal fornix of the patient intraoperatively. After removing the foreign body, the edema of vaginal mucosa, cervical swelling, contact bleeding, and an apparent fistula between the vagina and the rectum were observed. Then, transabdominal and rectal repair of vaginal fistula was conducted, and the anterior lip of the cervix was collected for biopsy. Postoperative pathological examination suggested acute cervicitis.
In 2015, Ciebiera et al. [9] reported a 73-year-old patient with breast cancer and a history of tamoxifen treatment. In recent two years, the patient visited doctors due to urinarytract infection, genital tract infection accompanied by vaginal discharge, odor, and abdominal pain for many times. A variety of broad-spectrum antibiotic therapies did not achieve good efficacy; however, no attention was drawn from doctors and causes of disease were not further explored. Before this admission, cervical cytological examination suggested chronic cervicitis. After admission, the physical examination revealed that there was foul secretion flowing out of the vagina, and a nodular hard mass was detected in the posterior vaginal fornix. The patient refused vaginal speculum examination and transvaginal ultrasonography. Transrectal ultrasonography revealed inhomogeneous cervical echoes (size, approximately 63 × 58 mm), and a mass with inhomogeneous and abundant blood flow signals (size, 32 × 18 mm) in the vaginal fornix. After a discussion of the medical group, it was decided to carry out surgical resection of vaginal lesion for this patient. Intraoperatively, a cervical mass that was suspected as cervical carcinoma was found. However, after separating and cutting open surrounding adhesive tissue, a plastic shampoo bottle cap was discovered in the mass. The vaginal lesion of this patient was misdiagnosed as metastatic tumor of breast cancer by attending doctors due to a clear history of breast cancer and tamoxifen treatment.
The patient in the present report denied a history of inserting foreign bodies into the vagina. It was speculated that the foreign bodies were left in the patient’s vagina during the hemostatic therapy in a local hospital in Tibet due to massive vaginal hemorrhage after spontaneous abortion more than ten years ago. Because of normal menstruation, poor local medical conditions, and patient’s lack of medical knowledge, the patient did not go to hospital to receive any examinations. Ten years later, she visited a doctor due to upper vaginal infection, and was misdiagnosed as cervical carcinoma by her clinical manifestations and gynecological examination results. The patient underwent physical examination and vaginoscopy for many times in tumor hospital and in the present hospital, and received biopsy for three times for the cervix could not be exposed, all of which, however, did not draw high attention. Furthermore, the clinical thinking of doctors was limited. They did not consider why the cervix of a woman of child-bearing age with completely normal lower vaginal mucosa could not be exposed.
Through reporting this case, gynecologists should be warned: (1) they should not be careless to leave foreign bodies in the body of patients during the process of diagnosis and treatment, causing pain to patients; (2) they should be more careful with physical examination, ask more questions, and not limit their clinical thinking to common diseases, and thereby reducing misdiagnosis to the maximum extent.
