1 Department of Anaesthesiology and Intensive Care, University of Pécs, Medical School, Clinical Centre, 7624 Pécs, Hungary
2 Department of Laboratory Medicine, University of Pecs, Medical School, Clinical Centre, 7624 Pécs, Hungary
3 Central Laboratory, Szigetvar Hospital, 7900 Szigetvár, Hungary
4 Department of Medical Biology and Central Electron Microscopic Laboratory, University of Pécs, Medical School, 7624 Pécs, Hungary
†These authors contributed equally.
Academic Editor: Graham Pawelec
Abstract
Introduction: Exploration of novel and effective antiplatelet
strategies for the secondary prevention of ischemic stroke is utmost. Some
platelet derived microparticles (PMVs) in convalescent stroke subjects were found
to be predictive for the next vascular event. Patients with high-on-treatment
platelet reactivity (HTPR) had a significantly higher risk for ischemic stroke.
Here, we aimed to explore associations among circulating microparticles and
responsivness to antiplatelet (clopidogrel) therapy. Methods: A total of
18 patients on clopidogrel therapy due to secondary stroke prevention were
rospectively recruited into this study. Twenty age-matched healthy subjects
served as controls. Flow cytometric measurements of microparicles (MVs) and data
analysis were performed on Beckman-Coulter FC-500 cytometer with CXP software.
Besides, platelet aggregometry data were revealed. Both measurements were
performed in whole blood and from the lower and upper blood fractions separated
after 1-hour gravity sedimentation by the analogy with erythrocyte sedimentation
rate. Results: The total number of circulating MVs, and particularly the
platelet derived CD42
Keywords
- microvesicles
- platelet
- neutrophil
- ischemic stroke
- antiplatelet therapy
- clopidogrel
Stroke is a highly prevalent condition that puts a significant burden on most societies. It is the leading cause of adult disability, the second leading cause of dementia and the fourth leading cause of death worldwide [1]. The prevalence of stroke and stroke-related costs will undoubtedly rise as the ratio of aging population increases worldwide, making prevention and identification of early signs of recurrent ischemic episodes a priority [2]. Peripheral circulating microvesicles (MVs) are small particles (0.1–1.0 micrometer in diameter) derived from the membrane blebs of activated cells, it can be found in synovial fluid, tear, liquor, saliva, urine, breastmilk and in bronchoalveolar lavage as well due to peripheral microcirculation [3]. Circulating platelet MVs (PMVs) are the most abundant type of MVs found in human circulation and they express various platelet surface markers such as CD42a, CD42b, CD61, CD62P [4, 5]. Microvesicles have multiple biological functions: (i) antigen presentation; (ii) intercellular communication; (iii) immune reaction and (iv) RNA and protein delivery. Thus, they enable intercellular communication by delivering lipids, proteins and genetic material to nearby or distant cells and modulating the functions of these cellular targets [6, 7]. There is growing evidence that MVs are playing a pivotal role in regulation of hemostasis, inflammation and angiogenesis [8]. Previous studies suggest that a large increase in circulating platelet derived microvesicles (PMVs) have been observed in patients with cardiovascular disease [9]. Therefore, PMVs might be important biomarkers and tools in the identification of the risk of various recurrent cerebrovascular diseases [10]. Platelet antisedimentation rate (PAR) reflects the percentage of platelets crossing the midline of the blood column upwards during 1-hour gravity sedimentation [11]. One of our previous studies concluded that the PAR value was able to discriminate clopidogrel non-responders from responders [11]. Activation of neutrophils reflected by neutrophil antisedimentation rate (NAR) proved to be a sensitive predictor of recurrent ischemic cerebral episodes in post-stroke patients on clopidogrel [12].
The aim of this prospective pilot-study was to explore: (i) differences of circulating MVs of different origin, comparing convalescent ischemic stroke patients vs healthy controls; (ii) whether the function of platelets correlate with certain MVs in patients on antiplatelet (clopidogrel) therapy; (iii) which PMVs show association with the high-on-treatment residual platelet reactivity (non-responder state).
The study protocol was approved by the University of Pécs Clinical Centre Regional and Institutional Research Ethics Committee (Ref. number: 6735, Clinical Trial No: NTC03679858). All procedures were performed in accordance with the ethical guidelines of the 1975 Declaration of Helsinki. Written informed consent was obtained from both patients and healthy volunteers. A total of 18 patients (median age at 66 years, 12 males) on antiplatelet therapy (75 mg clopidogrel once daily) due to secondary stroke prevention were prospectively recruited into this study. The selected patients with previous anterior circulation large artery atherothrombosis were on regular medical check-ups at the Outpatient Clinic of the Department of Neurology at the University of Pécs.
Venous blood samples were drawn with 21G needle after short strangulation from
an antecubital vein into closed blood collection system tubes with 3.2% (0.109
M) Na
The modified whole blood gravity sedimentation technique was developed for studying platelet and neutrophil sedimentation properties [11]. After a 1-hour gravity sedimentation, the upper and lower half of the venous blood column were separately removed from the EDTA and hirudin containing tubes and transferred into another EDTA and hirudin tube for further analysis (Fig. 1). The total blood cell count and the neutrophil (%) count were measured from the whole blood and after 1-hour gravity sedimentation from the upper and lower part of the blood on a Sysmex XN 9000 integrated automated haematology analyser (Sysmex Co., Kobe, Japan, 2017).
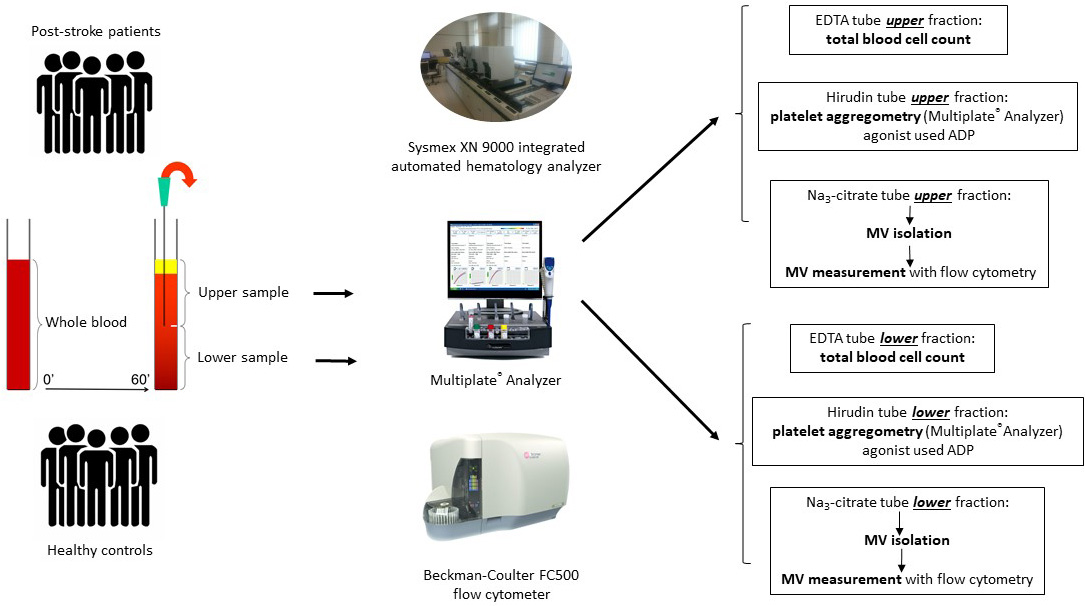 Fig. 1.
Fig. 1.Chart of sample preparation, separation of the upper and lower blood sample after 1-hour gravity sedimentation and further analytical process.
Platelet function test was performed in the whole blood and after 1 hour of
sedimentation from the upper and lower part of the hirudin anticoagulated blood
with a Multiplate® Analyzer (Roche Diagnostics, Mannheim,
Germany). Platelet aggregometry was uniformly carried out 60 minutes after blood
sampling using adenosine diphosphate (ADP; 6.5 M) as agonist [12]. Aggregation
level was expressed as the area under the curve (AUC). AUC was calculated by a
Multiplate® Analyzer using the product of aggregation unit (AU)
After a one-hour sedimentation the upper and lower part of the citrated blood
were centrifuged at 2500
| CD marker | Cellular origin | Fluorescent dye | Manufacturer |
| CD62P (P selectin) | Platelet | PE | Beckman-Coulter |
| CD41 (GPIIb/IIIa) | Platelet | Cy5 | Beckman-Coulter |
| CD42a (GPIb/V/IX) | Platelet | FITC | Becton-Dickinson |
| PAC1 (GPIIb/IIIa, near fibrinogen binding site) | Platelet | FITC | Becton-Dickinson |
| CD31 (PECAM-1) | Endothelial cell | PE | Becton-Dickinson |
| Annexin V | Recognize phophatydil-serine | FITC, Cy5 | Becton-Dickinson |
| Mouse IgG1 | Isotype control | FITC, PE, Cy5 | Becton-Dickinson |
| Abbreviations: Cy5, Cychrome5; FITC, fluorescein isothiocyanate; PE, phycoerythrin; Ig, immunoglobulin. | |||
Flow cytometric measurements and data analysis were performed on a
Beckman-Coulter FC-500 cytometer with CXP software (Version 2.3. Beckman Coulter Life Sciences, Indianapolis). The MV’s reference gate was
defined with Megamix beads (Biocytex). Side scatter, forward scatter and
fluorescence channels were set in a logarithmic scale. MV size gate was
determined between 0.5
Statistical analysis was performed using SPSS version 23.0 (IBM Corporation,
Armonk, NY, USA). Summary statistics of the participants were constructed using
frequencies and proportions for categorical data and as mean and standard
deviation (SD) for continuous variables. Conformity of data to normal
distribution was determined by histogram and Kolmogorov–Smirnov test. The
between-group difference was calculated with
A total of 18 convalescent ischemic stroke patients on clopidogrel (all patients
suffered from large vessel occlusion) and 20 age-matched healthy subjects were
recruited into this study prospectively. Demography of patients and healthy
controls and baseline laboratory parameters of the study population are
summarized in Table 2. There was no significant difference in regard to age and
gender. The total number of circulating microvesicles (p
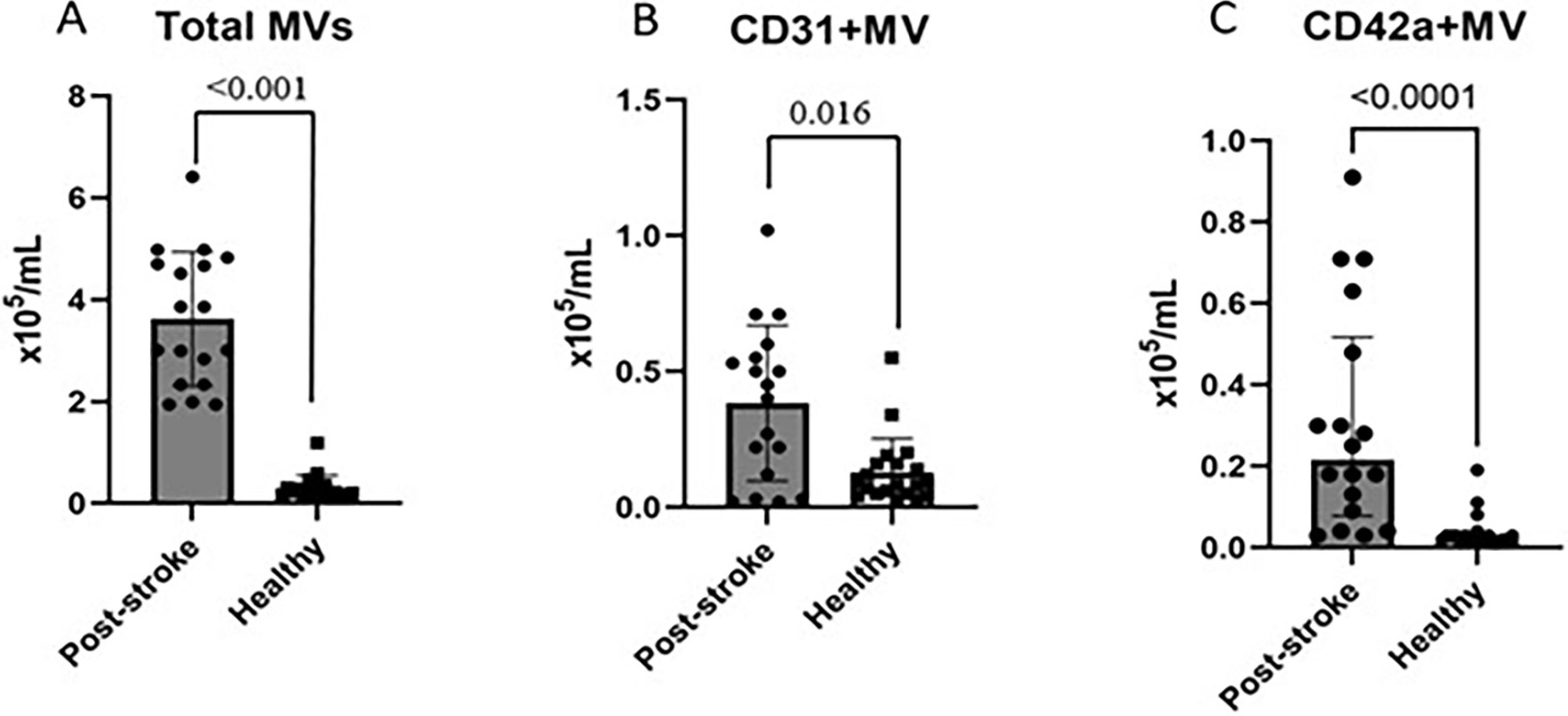 Fig. 2.
Fig. 2.
Comparison of the total count of MVs (2A), the CD31
| Observed parameters | Post-stroke patients (n = 18) | Healthy controls (n = 20) | p-value | ||
| Age | 66 (60–70) | 57 (49–63) | 0.078 | ||
| Male/Female | 2/6 | 10/10 | 0.298 | ||
| MVs (×10 |
whole blood | upper sample | lower sample | whole blood | |
| Total MVs | 3.43 (2.34–4.70) | 1.79 (1.37–2.82) | 1.53 (0.96–1.89) | 0.22 (0.13–0.37) | |
| CD31 |
0.43 (0.12–0.55) | 0.25 (0.10–0.46) | 0.07 (0.03–0.155) | 0.08 (0.04–0.16) | 0.016 |
| CD42a |
0.21(0.09–0.48) | 0.13 (0.07–0.32) | 0.05 (0.02–0.10) | 0.02 (0.01–0.03) | |
| CD41 |
0.25 (0.13–0.56) | 0.15 (0.10–0.53) | 0.04 (0.03–0.10) | 0.15 (0.09–0.25) | 0.251 |
| CD62P |
0.48 (0.09–0.85) | 0.26 (0.07–0.59) | 0.15 (0.03–0.24) | 0.17 (0.09–0.33) | 0.105 |
| PAC-1 |
0.009 (0.009–0.03) | 0.008 (0.007–0.02) | 0.003 (0.002–0.007) | 0.01 (0.009–0.02) | 0.515 |
| MVs, microvesicles ( | |||||
We analysed the correlation between MVs and aggregometry data. The platelet
aggregation in the whole blood (area under the curve, AUC) measured by
Multiplate® in patients taking clopidogrel, but not in
age-matched healthy controls, showed a significant negative correlation with the
total number of MVs (
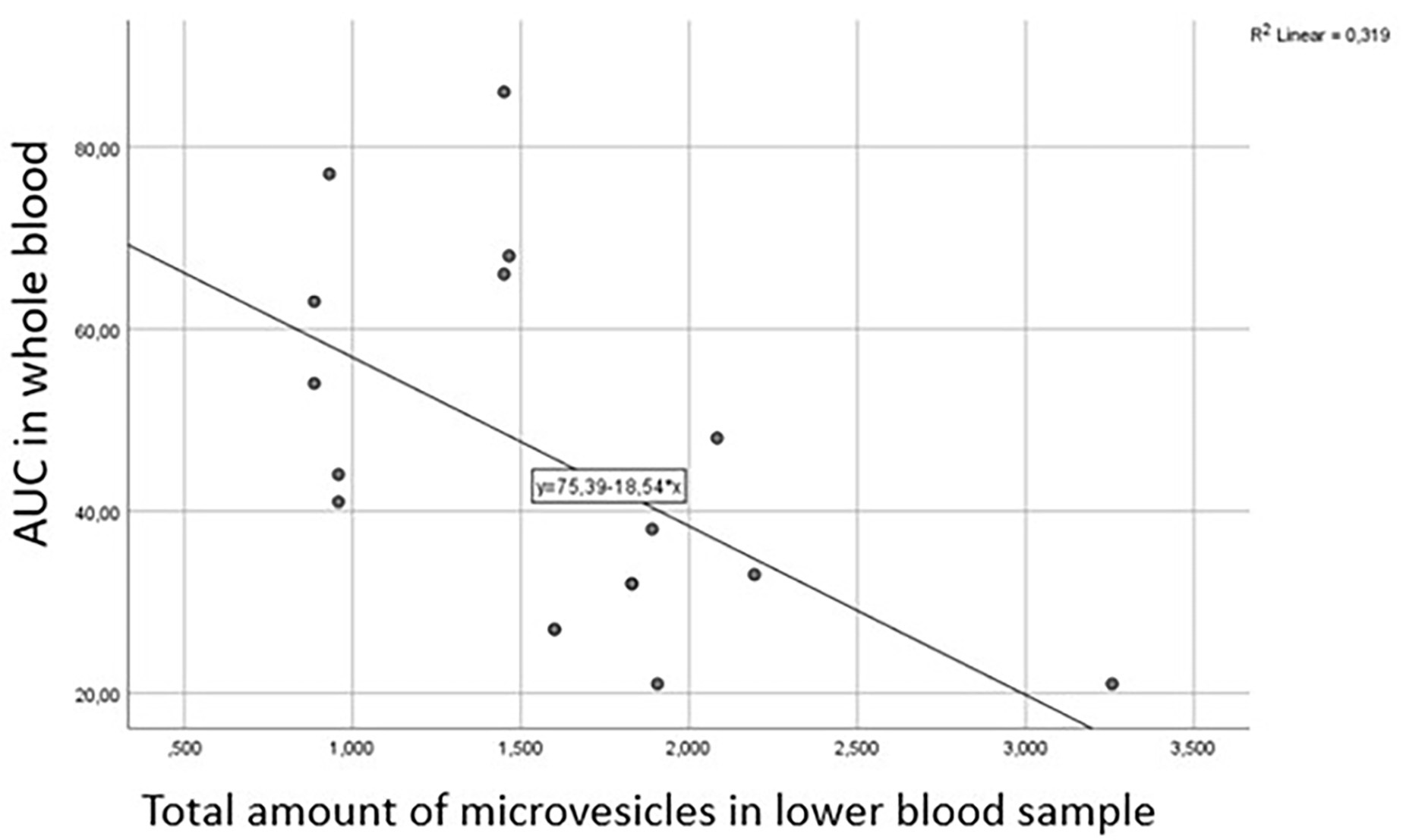 Fig. 3.
Fig. 3.
Correlation between the area under the curve (AUC) in
whole blood measured by Multiplate® and total number of
microvesicles (
Next, we explored the potential associations between MVs and aggregometry data
(area under the curve, AUC and velocity respectively) obtained from clopidogrel
responders and non-responders based on the previously defined cut-off value (AUC:
53). Both the AUC and the velocity in the whole blood showed negative correlation
with the total number of MVs (
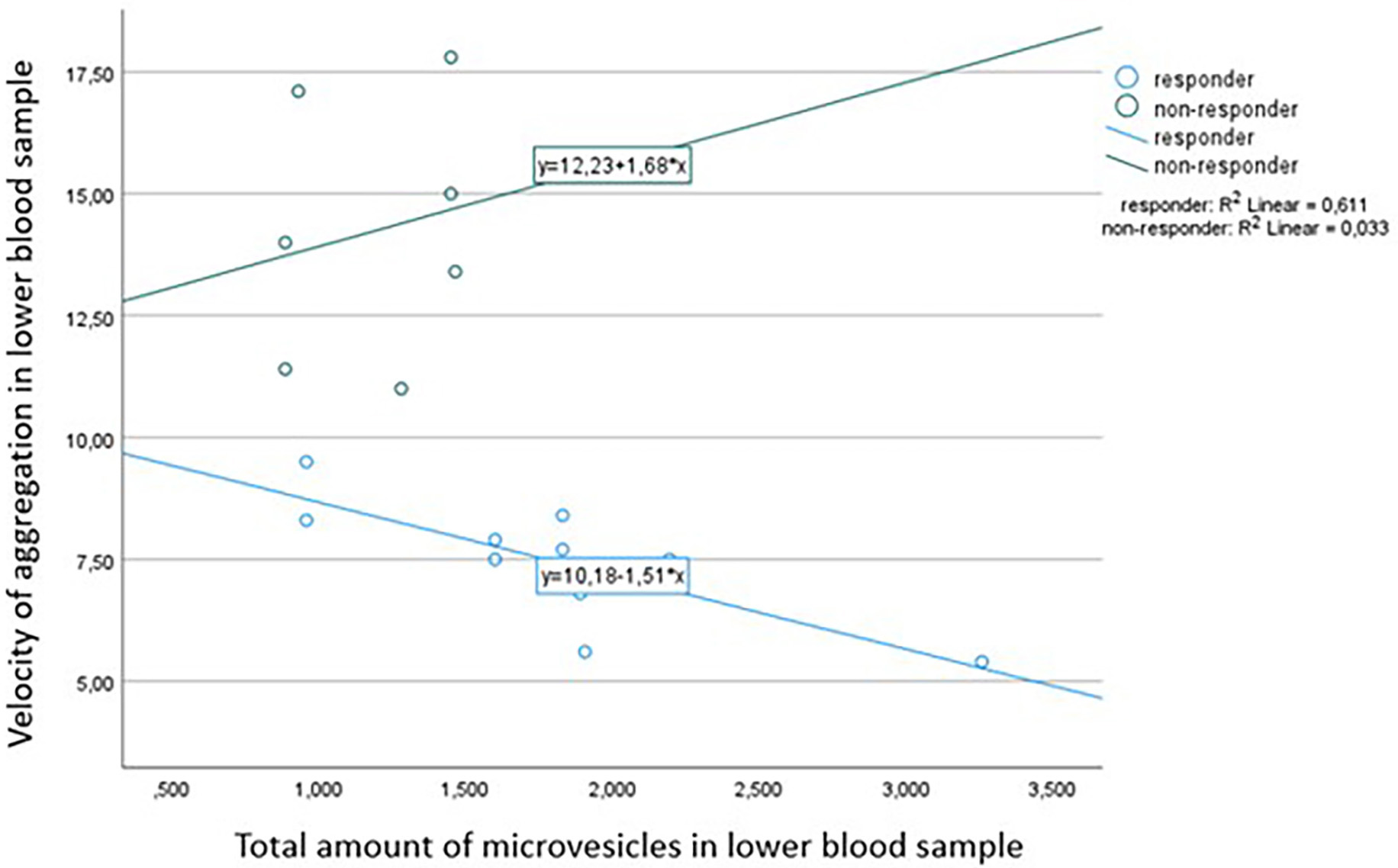 Fig. 4.
Fig. 4.Correlation between velocity measured by
Multiplate® aggregometry and total number of microvesicles
(
Activation-induced conformational epitope on CD41/CD61 complex positive
(PAC-1
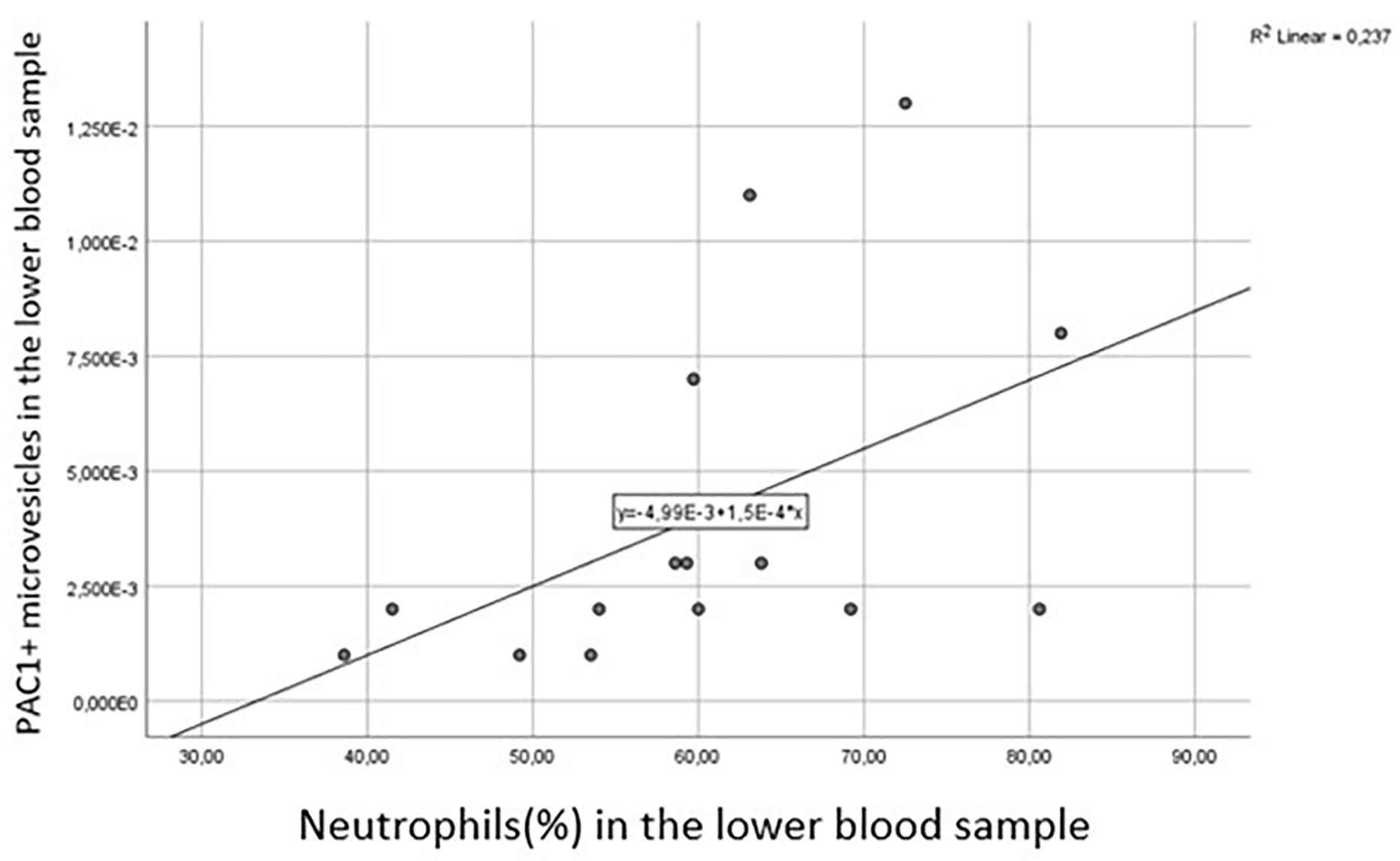 Fig. 5.
Fig. 5.
Correlation between platelet derived PAC1
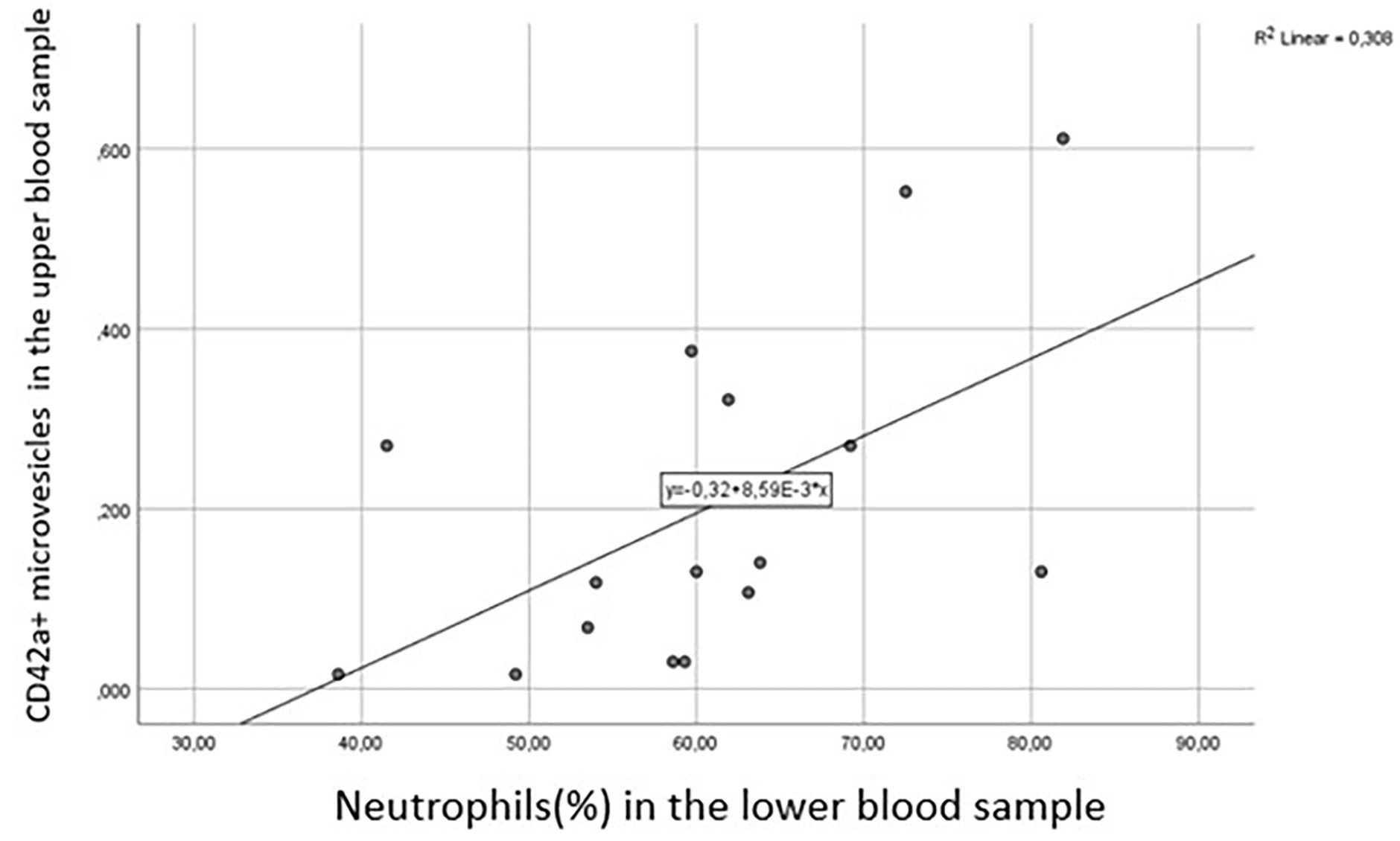 Fig. 6.
Fig. 6.
Correlation between platelet derived CD42a
In accordance with a recently published meta-analysis [15], we found that the
total number of circulating microvesicles, endothelial-derived CD31
We presumed that the quality (origin) and number of circulating microvesicles
might affect the response to clopidogrel in post-stroke patients. Although we did
not observe any correlation between the platelet aggregometry reflected by AUC
and the total number of MVs in the whole blood of post-stroke patients, we
discovered a negative correlation between AUC
Interestingly, Rosinska et al. [17] revealed no relationship between
circulating microvesicle number and platelet aggregation in post-stroke patients
on aspirin (ASA), suggesting that residual platelet reactivity is not affected by
MVs in the presence of ASA. Nevertheless, elevated concentrations of
PAC-1
Another important aspect that arises in connection with platelets and PMVs is
their role in immune processes. Importantly, we observed positive correlations
between PAC1
Limitations of our study are the following: (i) small sample size; (ii) variance in time elapsed between the index event and the blood sampling; (iii) only patients taking clopidogrel were recruited, but other antiplatelet agents would be worth investigating in the future.
Based on our findings, the identification and quantification of circulating MVs
may allow us to monitor the response to antiplatelet therapy with P2Y12
antagonists (e.g., clopidogrel), providing a novel opportunity to identify
non-responder patients thus allowing an individually tailored antiplatelet
strategy. Besides, links among platelet derived MVs, particularly CD42a
DS, EE and TM conceived, designed and coordinated the study, participated in acquisition, and interpretation of data. DS drafted the manuscript. MT-F performed the laboratory measurements. MT-F and TM participated in the statistical analysis. AM, TM took part in manuscript revision. All authors read and approved the manuscript.
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by Local Ethics Committee of the University of Pécs (Ref. number: 6735, Clinical Trial No: NTC03679858). Informed consent was obtained from all subjects involved in the study.
Our thanks go to all the patients and staff who participated in this research.
The study was supported by EFOP-3.6.3-VEKOP-16-2017-00009 at the University of Pécs.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.fbl2705158.






