1 No. 3 Department of Encephalopathy, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, 250011 Jinan, Shandong, China
2 Experimental Center, Shandong University of Traditional Chinese Medicine, 250355 Jinan, Shandong, China
3 College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, 250355 Jinan, Shandong, China
4 Department of Vertigo, Shandong Provincial Hospital Affiliated to Shandong First Medical University, 250021 Jinan, Shandong, China
Abstract
In clinical practice, selective serotonin reuptake inhibitors (SSRIs), a kind of Western medicine, are the primary treatment for depression, a complex mental illness. However, these treatments are associated with significant adverse reactions. With their many benefits and distinctive features, such as all-encompassing intervention and general control through several targets, processes, and pathways, the active components in traditional Chinese medicine (TCM) hold great promise for the treatment of depression. Autophagy plays a crucial role in the pathophysiology of depression, and its regulation has emerged as a potentially crucial management tactic. However, comprehensive evaluations of the link between depression and mitochondrial autophagy, as well as the therapeutic potential of TCM’s active components, remain limited. This review examined recent literature on autophagy and its role in depression, along with studies on the effects of TCM active ingredients. Furthermore, it highlighted the limitations of current research to offer insights to guide future fundamental studies and clinical treatments for depression.
Keywords
- depression
- antidepressant
- active ingredients of traditional Chinese medicine
- autophagy
- molecular mechanism
1. Major depressive disorder (MDD) is a prevalent and debilitating mental illness characterized by persistent sadness, loss of pleasure, suicidal tendencies, and various physical symptoms.
2. Autophagy plays an important role in the pathological development of MDD.
3. The active ingredients of traditional Chinese medicine can treat MDD by regulating autophagy.
Major depressive disorder (MDD), commonly referred to as depression, is a prevalent and debilitating mental illness characterized by persistent sadness, loss of pleasure, suicidal tendencies, and various physical symptoms. Due to its high lifetime incidence, recurrent nature, severe impairment, and chronic progression, depression is currently ranked as the fourth leading cause of disease burden worldwide by the World Health Organization [1]. The most used pharmacological treatments in clinical practice are selective serotonin reuptake inhibitors (SSRIs) and others. SSRIs exert their antidepressant effects by blocking the reuptake of 5-hydroxytryptamine (5-HT) at presynaptic membranes, specifically inhibiting 5-HT transporters, thereby extending and intensifying the effects of 5-HT [2, 3]. However, these medications are linked to significant side effects, including headaches, nausea, weight gain, and persistent sexual dysfunction. Moreover, most therapies have high non-response rates and delayed effects [4, 5, 6]. As a result, the development of safer and more effective antidepressants has become an urgent priority.
Due to its multi-component, multi-target, and multi-pathway effects, traditional Chinese medicine (TCM) represents a viable alternative for antidepressant treatment. Active compounds found in TCM, such as oridonin, baicalin, and quercetin, have shown strong antidepressant benefits with minimal adverse side effects [7], highlighting the vast potential of TCM in antidepressant treatment. For instance, research has found that Xiaoyao Pill, a Chinese patent medicine, can alleviate depressive symptoms through a mechanism of action involving regulation of DNA methylation [8].
Autophagy, an evolutionarily conserved metabolic process involving protein and organelle degradation, is crucial for maintaining cellular homeostasis [9]. Dysregulated autophagy plays an important role in the pathogenesis and development of MDD, making autophagy modulation a novel therapeutic strategy for its treatment. However, there is currently no systematic summary on the relationship between autophagy and MDD, nor of the antidepressant effects of TCM active ingredients through autophagy regulation.
This review summarized the mechanism of autophagy, its relationship with MDD, and the mechanism of active ingredients of TCM in treating depression via autophagy regulation, providing a scientific basis for future basic research and clinical applications.
Autophagy is the primary degradation pathway in eukaryotic cells, responsible for breaking down aging organelles and large molecular substances, such as invading viruses and bacteria, thereby removing obstacles to cell growth [10, 11]. Autophagy includes three main types: macroautophagy, microautophagy, and molecular chaperone-mediated autophagy. These processes rely on lysosomes to degrade and recycle cytoplasmic components.
Microautophagy can be further classified into selective, non-selective, and endosomal autophagy. Its key mechanism involves the lysosomal membrane forming arm-like or petal-like protrusions that envelop cytoplasmic material or organelles for degradation [12]. Heat shock cognate protein 70 (HSC70) and other proteins selectively break down proteins with KFERQ-like domains, facilitating molecular chaperone-mediated autophagy. These proteins are transferred to lysosomes via lysosomal receptors for degradation [13]. Cytoplasmic components primarily reach lysosomes by mega-autophagy, also referred to simply as autophagy. This process involves the engulfment and degradation of organelles and cellular components inside a double-membrane framework. This complex, multi-step membrane transport process can be divided into the stages of initiation, nucleation, elongation, fusion, and degradation [14]. Mitophagy is a specific form of autophagy dedicated to tagging, removing, and recycling damaged or depolarized mitochondria. In addition, mitophagy plays a role in clearing excess organelles, such as sperm mitochondria, following fertilization [15].
In patients with MDD, dysregulated expression of autophagy-related genes has been identified in blood monocytes [16], along with abnormalities in the AKT1 and mammalian target of rapamycin (mTOR) signaling pathways, both of which are essential for autophagy regulation [17, 18]. Over and beyond that, alterations in extracellular vesicle mRNA in postpartum depression patients have been found to be enriched in genes potentially associated with autophagy. Disrupted extracellular vesicle mRNA communication related to autophagy may contribute to the pathological development of postpartum depression [19]. A bioinformatics analysis further identified autophagy-related genes, such asG protein-coupled receptor 18 (GPR18), pyruvate dehydrogenase kinase 4 (PDK4), neuregulin 1 (NRG1), and EPH receptor B2 (EPHB2), as potential diagnostic markers for MDD, with GPR18 possibly playing a role in its pathogenesis [20].
Neuroinflammation is an essential part of the pathophysiology of depression. Evidence from animal models supports the involvement of autophagy dysregulation in the development of depression. The autophagy process is related to the activation of NOD-like receptor pyrin domain-containing 3 (NLRP3) inflammasomes. Mice with dysfunctional lysosomes in the autophagy-lysosome pathway may exhibit depressive-like behavior, increased synthesis of pro-inflammatory molecules, and interference with the breakdown of NLRP3 inflammasomes [21]. Depression is exacerbated by the NLRP3 inflammasome, a multiprotein complex that triggers inflammatory cell death and caspase-1-mediated pro-inflammatory cytokines including interleukin-1
Neuronal survival and function are also critical in depression. In a chronic restraint stress (CRS) depression model, autophagic cell death of neural stem cells (NSCs) led to hippocampal neuron damage in mice [23]. Similarly, in a corticosterone (CORT)-induced mouse model, excessive neuronal autophagy in the dentate gyrus (DG) increased the expression of autophagy related gene 5 (ATG5), resulting in excessive degradation of brain-derived neurotrophic factor (BDNF); It also significantly reduced the proliferation of NSCs, neural progenitor cell (NPCs), adult cells, as well as the migration and survival of recently formed neurons in DG. Knocking down ATG5 in neurons alleviated these effects and improved depressive-like behaviors in mice [24]. Notably, obesity has been demonstrated to reduce autophagy in a high-fat diet-induced obese mice model by boosting mTOR phosphorylation and inhibiting AMP-activated protein kinase (AMPK) phosphorylation, which results in depressive-like behaviors [25].
In summary, both clinical studies and animal models consistently reveal pathological autophagy imbalances in depression, indicating a close relationship between autophagy and depression. Regulating autophagy is one of the important key strategies for antidepressant treatment.
Flavonoids, a class of naturally occurring polyphenolic compounds, are widely distributed throughout the plant kingdom [26]. One well-known flavonoid, quercetin, possesses immunoprotective, antiviral, antioxidant, neuroprotective, and cardioprotective properties [27]. A study demonstrated that quercetin inhibits NLRP3 inflammasome activation mediated by mitochondrial reactive oxygen species (mtROS) in microglia by promoting mitochondrial autophagy, thereby preventing neuronal damage and offering potential therapeutic effects for depression [28]. Another flavonoid, baicalin, which is extracted from the root of Scutellaria baicalensis, has antidepressant properties by enhancing NIX-mediated mitochondrial autophagy through direct AMPK binding and activation of the AMPK/peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1
Apigenin, a flavone found in plants such as chamomile, onions, fruits, and salvia plebeia [31], has shown antidepressant effects [32]. Zhang et al. [33] found that apigenin promoted autophagy via the AMPK/mTOR pathway in a CRS mouse model, alleviating depression. Silibinin, a key component of the silymarin complex extracted from the seeds of milk thistle (Silybum marianum) [34], upregulates BDNF/TrkB pathway activity and restores autophagy balance in the hippocampus, exerting antidepressant effects [35]. Kaempferol-3-O-sophoroside, a primary component of Crocus sativus (saffron), interacts with AMPK to stimulate BDNF production and autophagy, achieving antidepressant effects [36].
Terpenoids, also known as isoprenoids, are natural isoprene-based compounds that play essential roles in metabolic processes across all organisms [37]. By preventing the connection between NLRP3 and NIMA related kinase 7 (NEK7), oridonin, a naturally occurring terpenoid present in several TCMs, reduces autophagy damage and neuroinflammation [38, 39]. It also activates autophagy to inhibit NLRP3 inflammasomes, thereby alleviating lipopolysaccharide (LPS)-induced depression [40].
Patchouli alcohol, a tricyclic sesquiterpene extracted from Pogostemon cablin, has anti-inflammatory effects [41]. Recent research indicates that it inhibits autophagy, repairs synapses, and restores autophagic flux in the hippocampus by activating the mTOR signaling pathway in chronic unexpected mild stress (CUMS) rats, hence demonstrating an antidepressant effect [42]. Andrographide, the main component of Andrographis paniculata [43], alleviates CUMS-induced depressive-like behaviors in rats by upregulating autophagy [44].
Saponins, naturally occurring compounds present in various plants and TCMs, exhibit a wide range of therapeutic effects [45]. Extracted from Radix Paeoniae Rubra, total paeony glycoside (TPG) restores mitochondrial function, inhibits inflammation-mediated pyroptosis, and activates autophagy to repair neuronal damage, all of which greatly aid antidepressant treatment [46]. The primary active ingredient in ginseng, Ginsenoside Rg1 (Rg1), has demonstrated potential in the prevention and treatment of neurological disorders, including depression [47]. According to Wang et al. [48], Rg1’s antidepressant action included modifying the Cx43 autophagy-lysosomal and ubiquitin-proteasome pathways. Furthermore, by stimulating the BDNF-mTORC1 pathway, controlling autophagy, and improving hippocampus synaptic plasticity, ginseng total saponins and fuzi total alkaloids work in concert to produce antidepressant effects [49].
The human diet is abundant in polyphenols, a family of bioactive substances with phenolic structures [50]. Resveratrol is a key nutrient and a natural plant-derived antitoxin that helps plants defend against environmental stress and pathogen invasion [51]. Previous reports have shown that resveratrol can treat depression by regulating the hypothalamic-pituitary-adrenal (HPA) axis, alleviating neuroinflammation, and promoting neurogenesis [52]. In terms of regulating autophagy, Tabassum et al. [53] found that resveratrol (RSV) can regulate the expression of the Sirtuin-1 (SIRT1)/peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1
Alkaloids are naturally occurring metabolites with diverse regulatory effects on the body [55]. Alkaloids derived from TCM have been reported to have antidepressant effects. For instance, berberine, extracted from Rhizoma coptidis, has recently been found to exert antidepressant effects by inhibiting neuroinflammation, modulating neural plasticity, and regulating tryptophan metabolism [56, 57]. Lotus plumule, a traditional Chinese food, is rich in alkaloids, sterols, water-soluble polysaccharides, and various micronutrients, all of which provide numerous health benefits [58]. By controlling BDNF-mediated endoplasmic reticulum stress and autophagy, Chen et al. [59] showed via network pharmacology and experimental confirmation that natural alkaloids from lotus plumule mitigated LPS-induced depressive-like behavior.
The only species in the genus Euryale within the botanical family Nymphaeaceae is the annual watery herbaceous plant Euryale ferox Salisb [60]. Extracts of Euryale ferox Salisb. can improve the AMPK pathway and correct autophagy abnormalities associated with depression, thereby alleviating depressive-like behavior induced by CUMS [61]. Radix Polygalae, a famous Chinese herbal medicine, has been widely used for centuries in traditional practices for its expectorant, nourishing, calming, and antipsychotic properties [62]. Evidence suggests that its active ingredient, polygalae radix oligosaccharide esters, can alleviate depression by regulating gut microbiota [63]. Additionally, in behavioral despair mice and CRS-induced rats, Radix Polygalae extract has shown strong antidepressant efficacy, most likely by enhancing autophagy and reducing neuroinflammation [64].
Morinda officinalis is one of the four famous Southern Chinese herbs, and its oligosaccharides are one of its main active ingredients. These oligosaccharides have been shown to treat depression by regulating the intestinal microbiota [65]. Recent studies have also found that Morinda officinalis oligosaccharides upregulate Mfn2 expression to activate the PI3K/Akt/mTOR pathway-mediated mitochondrial autophagy, thereby clearing damaged mitochondria in astrocytes and treating an animal model of hypertension with depression [66]. Salvia miltiorrhiza is one of the commonly used herbs in TCM and has attracted increasing interest in many medical areas [67]. It has been demonstrated that salvianolic acid B, an active component isolated from Salvia miltiorrhiza, controls autophagy and causes the clearance of NLRP3, resulting in neuroprotective and depressive effects (Fig. 1 and Table 1 (Ref. [28, 30, 33, 35, 36, 39, 42, 44, 46, 48, 53, 59, 61, 64, 66])).
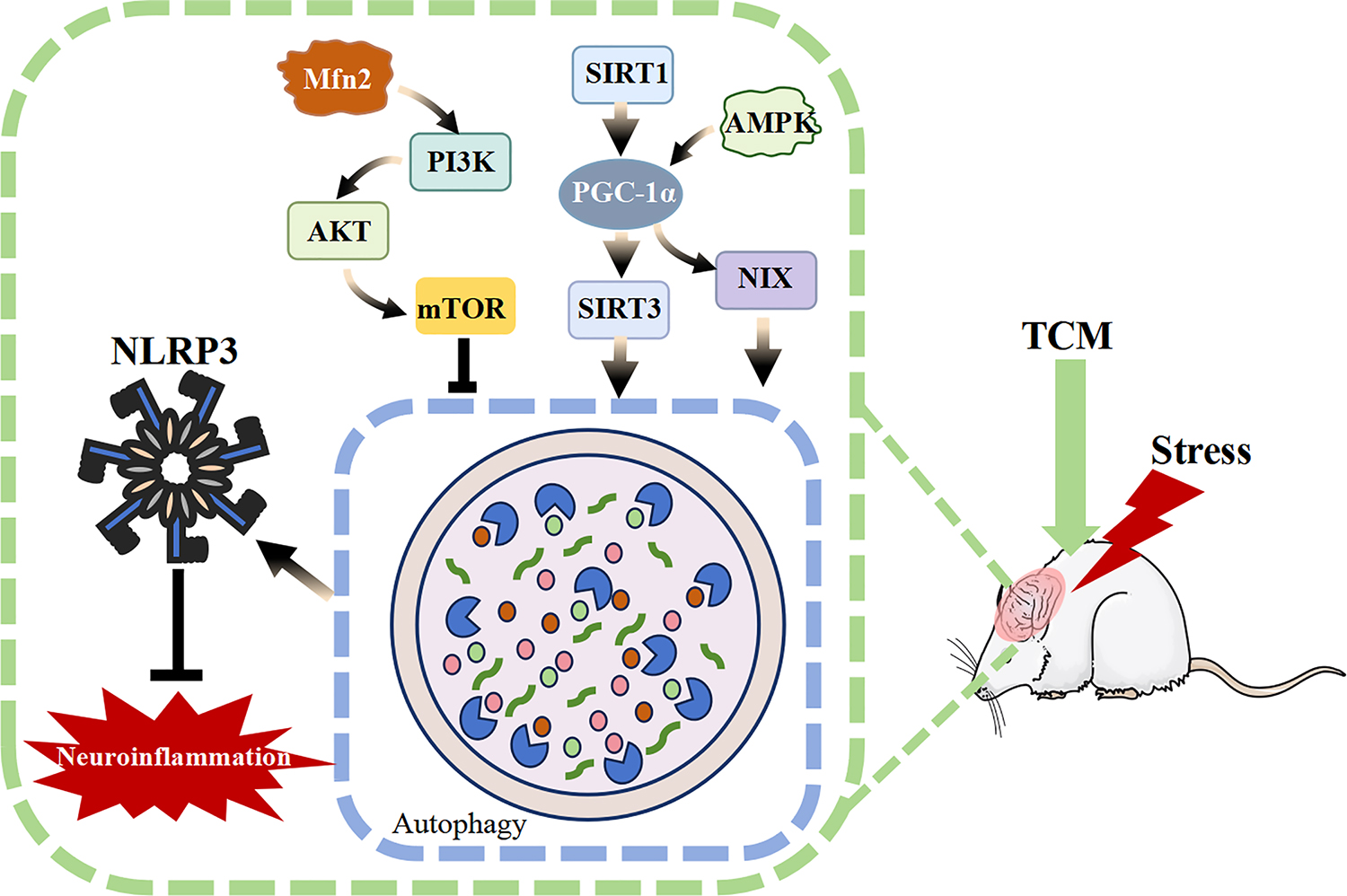 Fig. 1.
Fig. 1. Mechanism of action of active ingredients in traditional Chinese medicine. AMPK, AMP-activated protein kinase; mTOR, mammalian target of rapamycin; SIRT1, sirtuin-1; SIRT3, sirtuin-3; NLRP3, NOD-like receptor pyrin domain-containing 3; TCM, traditional Chinese medicine; NIX, NIP3 like protein X; PI3K, phosphoinositide 3-kinase; AKT, protein kinase B; Mfn2, mitofusin 2 protein.
| Classification | Active ingredients of TCM | Molecular formula | CAS NO. | Main molecular mechanisms | References |
| Flavonoids | Quercetin | C15H10O7 | 117-39-5 | Promoting mitochondrial autophagy to inhibit mtROS mediated NLRP3 inflammasome activation in microglia | [28] |
| Baicalin | C21H18O11 | 21967-41-9 | Activate AMPK/PGC-1 | [30] | |
| Apigenin | C15H10O5 | 520-36-5 | Promoting autophagy through the AMPK/mTOR pathway | [33] | |
| Silibinin | C25H22O10 | 22888-70-6 | Upregulation of BDNF/TrkB pathway activity has alleviated autophagy imbalance in the hippocampus | [35] | |
| Kaempferol-3-O-sophoroside | C27H30O16 | 19895-95-5 | Combining with AMPK to promote BDNF production and enhance autophagy | [36] | |
| Terpenoids | Oridonin | C20H28O6 | 28957-04-2 | Blocking the interaction between NLRP3 and NEK7 to inhibit neuroinflammation and autophagy damage | [39] |
| Patchouli alcohol | C15H26O | 5986-55-0 | Inhibiting autophagy, repairing synapses, and restoring autophagic flow in the hippocampus by activating the mTOR signaling pathway | [42] | |
| Andrographolide | C20H30O5 | 5508-58-7 | Regulating autophagy | [44] | |
| Saponins | Total paeony glycoside | Not Applicable | Not Applicable | Activating autophagy, restoring mitochondrial function, and reducing inflammation mediated pyroptosis to repair neuronal damage | [46] |
| Ginsenoside Rg1 | C42H72O14 | 22427-39-0 | Regulating the ubiquitin proteasome and autophagy lysosomal degradation pathways of Cx43 | [48] | |
| Polyphenols | Resveratrol | C14H12O3 | 501-36-0 | Regulating the expression of SIRT1/PGC-1 | [53] |
| Alkaloids | Natural alkaloids from lotus plumule | Not Applicable | Not Applicable | Regulating BDNF mediated endoplasmic reticulum stress and autophagy | [59] |
| Herbal extracts | Extract of Euryale ferox Salisb | Not Applicable | Not Applicable | Regulating the AMPK pathway to improve autophagy | [61] |
| Radix Polygalae extract | Not Applicable | Not Applicable | Promoting autophagy and inhibiting neuroinflammation | [64] | |
| Other types | Morinda officinalis oligosaccharides | Not Applicable | Not Applicable | Upregulation of Mfn2 expression to activate PI3K/Akt/mTOR pathway mediated mitochondrial autophagy | [66] |
mtROS, mitochondrial ROS; BDNF, brain-derived neurotrophic factor; NEK7, NIMA related kinase 7; Cx43, connexin 43; PGC-1α, PPARγ coactivator 1-alpha.
Major depressive disorder (MDD) is one of the most prevalent chronic, recurring, and incapacitating mental disorders. It is characterized by prolonged psychological distress, pain, feelings of worthlessness, sleep and appetite disturbances, and an increased risk of suicidal thoughts and behaviors [68]. Since its pathophysiology remains unclear and there are currently no sufficiently effective intervention strategies to successfully prevent or totally reverse the condition, MDD continues to provide a serious challenge to contemporary medicine [69]. TCM offers therapeutic benefits through its multi-component, multi-targets, and multi-pathway. Certain bioactive compounds extracted from TCM, such as flavonoids, terpenoids, saponins, polyphenols, alkaloids, herbal extracts, have been shown to exert antidepressant effects by regulating autophagy. These active ingredients hold significant potential for the treatment of MDD.
However, clinical studies investigating whether TCM’s active components can alleviate depression in MDD patients remain limited, with most research still confined to animal or cell models. Moreover, numerous TCM active substances face challenges such as low solubility, poor stability, and difficulty crossing the blood-brain barrier. Further research is needed to determine whether these active components can successfully target organs associated with MDD. The majority of research primarily focuses on molecular mechanisms, with insufficient scrutiny of the toxicological properties and potential adverse consequences of TCM’s active constituents. Furthermore, the stability and consistency of the chemical constituents in certain Chinese medicinal materials are compromised by ambiguous quality control requirements, thereby limiting their clinical applicability and complicating the investigation of their pharmacological actions. Moreover, the specificity of TCM’s active compounds in relation to autophagy remains inadequately elucidated, necessitating further research to ascertain whether these chemicals can precisely target autophagy. More critically, the conflicting findings regarding the increase or inhibition of neuronal autophagy in antidepressant therapy suggest that these results may be contingent upon the functional state of neurons during depression treatment.
Thus, clinical assessment of the effectiveness and side effects of TCM’s active components in treating MDD patients should be a primary focus of future research. Furthermore, comprehensive toxicity studies on TCM and the establishment of more rigorous quality control standards are imperative. To enhance the therapeutic effects of active components in target organs and further increase the concentration and duration of medications in the central nervous system, research on targeted delivery methods for TCM should also be intensified. That being said, our goal is to better understand the processes of depression and autophagy as well as the action routes of TCM by integrating spatial multi-omics approaches with single-cell sequencing. The mechanism by which TCM’s active components control autophagy should be elucidated using reverse validation techniques, such as the use of blockers or gene knockouts. Further preclinical and clinical research remains essential to comprehensively evaluate the impact of antidepressant treatments on autophagy, which is fundamental to the development of TCM-based antidepressants.
TCM, Traditional Chinese Medicine; SSRIs, selective serotonin reuptake inhibitors; HSC70, heat shock homologous protein 70; MDD, Major depressive disorder; mTOR, mammalian target of rapamycin; IL-1
Concept – ZL, KW, MZ; Design – ZL, KW, MZ; Supervision – ZL, KW, MZ; Resources – ZL, KW, MZ; Materials – ZL, KW, MZ; Data Collection and/or Processing – DC, KX, RS, XL; Analysis and/or Interpretation – LZ, DC, KX, RS, XL; Literature Search – LZ; Writing – LZ; Critical Review – ZL, KW, MZ. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Not applicable.
Not applicable.
This study was supported by the Science and Technology Development Program of Jinan City (Nos. 202019027 and 202134007).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

