1 Department of Cardiology, Cardiovascular Center, Beijing Friendship Hospital, Capital Medical University, 100050 Beijing, China
2 Department of Radiology, Beijing Friendship Hospital, Capital Medical University, 100050 Beijing, China
3 Beijing Key Laboratory of Metabolic Disorder Related Cardiovascular Disease, 100191 Beijing, China
4 Department of Geriatrics, Beijing Friendship Hospital, Capital Medical University, 100050 Beijing, China
Abstract
Background: Intramyocardial hemorrhage (IMH) is a result of
ischemia-reperfusion injury in ST-segment elevation myocardial infarction (STEMI)
after primary percutaneous coronary intervention (PPCI). Despite patients with
IMH show poorer prognoses, studies investigating predictors of IMH occurrence are
scarce. This study firstly investigated the effectiveness of regulatory T cell
(Treg), peak value of Creatine Kinase MB (pCKMB), high-sensitivity C-reactive
protein (hsCRP), and left ventricular end-systolic diameter (LVESD) as predictors
for IMH. Methods: In 182 STEMI patients received PPCI, predictors of IMH
were analyzed by logistic regression analysis. The predictive
ability of risk factors for IMH were determined by receiver operating
characteristic curves, net reclassification improvement (NRI), integrated
discrimination improvement (IDI) and C-index. Results: Overall, 80
patients (44.0%) developed IMH. All 4 biomarkers were independent predictors of
IMH [odds ratio [OR] (95% confidence interval [CI]): 0.350 (0.202–0.606) for Treg, 1.004 (1.001–1.006) for pCKMB, 1.060 (1.022–1.100) for hsCRP, and 3.329 (1.346–8.236) for LVESD]. After
propensity score matching (PSM), the biomarkers significantly predicted IMH with
areas under the curve of 0.750 for Treg, 0.721 for pCKMB, 0.656 for hsCRP, 0.633
for LVESD, and 0.821 for the integrated 4-marker panel. The addition of
integrated 4-marker panel to a baseline risk model had an incremental effect on
the predictive value for IMH [NRI: 0.197 (0.039 to 0.356); IDI: 0.200 (0.142 to
0.259); C-index: 0.806 (0.744 to 0.869), all p
Keywords
- ST-segment elevation myocardial infarction (STEMI)
- primary percutaneous coronary intervention (PPCI)
- intramyocardial hemorrhage (IMH)
- regulatory T cell (Treg)
- prediction
Current global guidelines for ST-segment elevation myocardial infarction (STEMI) recommend primary percutaneous coronary intervention (PPCI) as the gold standard of treatment [1, 2], and PPCI restores thrombolysis in myocardial infarction flow 3 (TIMI 3) in over 90% of patients. Despite the recovery of the epicardial coronary circulation, however, additional injury caused by PPCI such as microvascular injury, also known as the no-reflow phenomenon, cannot be ignored. Studies have confirmed that up to 40% to 50% of STEMI patients underwent PPCI may experience no-reflow phenomenon, including microvascular obstruction (MVO) and Intramyocardial hemorrhage (IMH) [3, 4]. Among them, ischemic injury of capillaries leads to the occurrence of endothelial gaps and loss of integrity of capillary wall, and extensive erythrocyte extravasation leads to IMH [5, 6]. Studies demonstrated that IMH was closely related to infarct size, MVO and impaired left ventricular (LV) function, and major adverse cardiac events (MACEs) [7, 8, 9, 10, 11, 12]. Therefore, accurate diagnosis of IMH is of great importance in the clinical. According to the recommendations of the guidelines, cardiac magnetic resonance (CMR) imaging is considered the reference diagnostic method for the evaluation of IMH [1, 13]. However, we found some disadvantages of CMR that should not be ignored in the process of practice. First of all, CMR is time-consuming, and it is dangerous for STEMI patients to go for such time-consuming test without electrocardiogram monitoring in acute phase. Second, for those patients with claustrophobia or other contraindications to CMR, it is not feasible to assess IMH by CMR. Finally, CMR is expensive, which will undoubtedly increase the cost of hospitalization for patients. Therefore, considering the above reasons, we tried to find a safe, simple and effective method to predict the presence of IMH. It is well known that myocardial ischaemia/reperfusion injury (MIRI) is a common cause of no-reflow [14], in which inflammatory response plays an important role [15, 16]. Bochaton et al. [17] analyzed 20 consecutive patients with STEMI-PPCI and found that high-sensitivity C-reactive protein (hsCRP) and neutrophils levels were higher in patients with IMH. In addition, although the innate immune response plays an I mportant role in ischaemia-reperfusion injury (IRI), T lymphocytes including T-helper 1 (Th1), Th2, Th17 and regulatory T (Treg) cells, are also involved in the pathogenesis of IRI.
In this study, we focused on the role of Treg cells in MIRI. As far as I know, Treg can be capable of suppressing the innate immune response by inhibiting the macrophage inflammatory phenotype and neutrophil function [18], thereby playing an anti-inflammatory effect in MIRI. Previous studies have reported that Treg can ameliorate IRI in kidney and brain [19, 20]. Recent studies have also reported the protective effect of Treg in mouse MIRI [21, 22]. In this study, we analyzed the circulating Treg level and other common laboratory indicators, and hypothesized that Treg individually or in combination with other indicators, such as left ventricular end-systolic diameter (LVESD), hsCRP and the peak value of Creatine Kinase MB (pCKMB), can be used to predict the presence of IMH in STEMI patients received PPCI.
The study population for this study was identified from the Cardiovascular
Center of Beijing Friendship Hospital. The data collection process was approved
by the Institutional Review Board of Beijing Friendship Hospital affiliated to
Capital Medical University and was in accordance with the Declaration of
Helsinki. Written informed consent was obtained from all patients. The inclusion
criteria for this study were STEMI patients within 12 h of symptom onset who
underwent PPCI at our hospital. The exclusion criteria included (1) previous
myocardial infarction or revascularization [PCI or coronary
artery bypass graft
(CABG)]; (2) atrial fibrillation;
(3) left ventricular ejection fraction (LVEF)
Blood samples were obtained on the following morning of the admission day, from all patients in a fasting state. A part of venous blood was prepared into peripheral blood mononuclear cells (PBMCs) by Ficoll density gradient method, and stored at –80 °C for the following flow cytometric analysis. The remaining blood sample was sent to the Central Laboratory of Beijing Friendship Hospital to be tested by professional laboratory physicians for other indicators, including hsCRP. In order to obtain the peak value of myocardial enzymes such as pCKMB, fasting venous blood was taken every morning within 5 days after PPCI to detect the levels of myocardial injury markers.
An ultrasound cardiogram was performed within 24 h after PPCI to obtain indicators of cardiac structure and function, such as LVESD and LVEF. Five to seven days after reperfusion, IMH was assessed by CMR using T2-weighted imaging.
For analysis of Treg, PBMCs were suspended in complete culture medium. The cell
suspension was resuscitated in an incubator set at 37 °C under a 5% CO
Treg commonly identified by their expression of CD4 and CD25 on the cell surface and the transcription factor Forkhead box P3 (Foxp3) in the nucleus [23]. For Treg analysis, the cells were incubated with Fluorescein isothiocyanate (FITC) anti-human CD4 and Allophycocyanin (APC) anti-human CD25. After the surface staining, the cells were stained with phycoerythrin (PE) anti-human Foxp3 for Treg detection after fixation and permeabilization. Isotype controls were given to enable correct compensation and confirm antibody specificity. All of the antibodies were from Biolegend. Stained cells were detected by the Attune NxT cytometer and analyzed by the FlowJo 10.0.7.2 software (Reachsoft, Beijing, China).
All patients were studied with a 3.0-T scanner (MAGNETOM Singovia; Siemens Healthcare, Erlangen, Germany) within 5–7 days after pPCI. All CMR data were evaluated by two experienced CMR analyst. The scan protocol was performed according to the guidelines of the Society of Cardiovascular Magnetic Resonance [24].
T2-weighted imaging was performed, and myocardium with a signal intensity
Continuous variables are presented as mean
According to the CMR results, patients were divided into IMH group (n = 80) and
no-IMH group (n = 102). The study patients had an average age of 58.0
| Total | No-IMH | IMH | p value | ||
| (n = 182) | (n = 102) | (n = 80) | |||
| Lym/PBMCs (%) | 69.5 (59.9, 77.3) | 69.7 (59.1, 78.6) | 69.2 (59.4, 76.3) | 0.522 | |
| CD4+ T cells/Lym (%) | 34.5 (27.3, 45.1) | 34.1 (26.5, 45.6) | 33.9 (27.6, 45.0) | 0.868 | |
| Treg/CD4+ T cells (%) | 1.0 (0.5, 1.5) | 1.3 (0.7, 1.8) | 0.8 (0.3, 1.1) | ||
| Age, years | 58.0 |
59.1 |
56.7 |
0.235 | |
| Male gender | 150 (82.4) | 84 (82.4) | 66 (82.5) | 0.979 | |
| BMI, kg/m |
25.9 |
26.1 |
25.7 |
0.346 | |
| SBP, mmHg | 124.9 |
125.8 |
123.9 |
0.628 | |
| DBP, mmHg | 77.1 |
77.3 |
76.8 |
0.805 | |
| Heart rate, bpm | 74.8 |
73.1 |
76.8 |
0.191 | |
| Medical history | |||||
| Current/ex-smoker | 132 (72.5) | 73 (71.6) | 59 (73.8) | 0.744 | |
| Diabetes mellitus | 63 (34.6) | 34 (33.3) | 29 (36.3) | 0.681 | |
| Hypertension | 119 (65.4) | 67 (65.7) | 52 (65.0) | 0.923 | |
| Stroke | 20 (11.0) | 11 (10.8) | 9 (11.3) | 0.921 | |
| Dyslipidemia | 139 (76.4) | 79 (77.5) | 60 (75.0) | 0.699 | |
| Antiplatelet agent | 16 (8.8) | 7 (6.9) | 9 (11.3) | 0.300 | |
| ACEI/ARB | 44 (24.2) | 31 (30.4) | 13 (16.3) | 0.027 | |
| Beta-blocker | 16 (8.8) | 11 (10.8) | 5 (6.3) | 0.284 | |
| Statins | 12 (6.6) | 6 (5.9) | 6 (7.5) | 0.662 | |
| Diagnosis at admission | |||||
| Anterior MI | 87 (47.8) | 41 (40.2) | 46 (57.5) | 0.020 | |
| In-hospital treatment | |||||
| PCI/CABG | 182 (100.0) | 102 (100.0) | 80 (100.0) | 1.000 | |
| Antiplatelet agent | 182 (100.0) | 102 (100.0) | 80 (100.0) | 1.000 | |
| ACEI/ARB | 79 (43.4) | 48 (47.1) | 31 (38.8) | 0.262 | |
| Beta-blocker | 146 (80.2) | 79 (77.5) | 67 (83.8) | 0.290 | |
| Statins | 159 (87.4) | 93 (91.2) | 66 (82.5) | 0.080 | |
| Hypoglycemic agents | |||||
| Metformin | 22 (12.1) | 11 (10.8) | 11 (13.8) | 0.542 | |
| AGI | 25 (13.7) | 16 (15.7) | 9 (11.3) | 0.388 | |
| Sulfonylurea | 7 (3.8) | 4 (3.9) | 3 (3.8) | 0.952 | |
| DPP-4i | 3 (1.6) | 2 (2.0) | 1 (1.3) | 0.709 | |
| SGLT-2i | 3 (1.6) | 1 (1.0) | 2 (2.5) | 0.424 | |
| Insulin | 8 (4.4) | 4 (3.9) | 4 (5.0) | 0.725 | |
| In-hospital time (d) | 8.9 |
8.7 |
9.3 |
0.144 | |
| Laboratory values | |||||
| WBC, 10 |
9.2 |
8.8 |
9.7 |
0.034 | |
| Hemoglobin, g/L | 147.8 |
145.7 |
150.3 |
0.154 | |
| hsCRP, mg/L | 4.8 (2.3, 15.4) | 3.5 (2.1, 8.7) | 8.0 (3.3, 23.2) | ||
| FPG, mmol/L | 6.3 (5.5, 8.9) | 6.0 (5.3, 8.3) | 6.7 (5.8, 9.4) | 0.009 | |
| RBG, mmol/L | 8.4 (7.2, 12.1) | 8.2 (7.0, 12.2) | 8.6 (7.3, 12.1) | 0.465 | |
| HbA1c, % | 6.6 |
6.4 |
6.7 |
0.102 | |
| Albumin, g/L | 41.7 |
41.1 |
42.4 |
0.053 | |
| ALT, U/L | 26.5 (18.0, 38.3) | 24.5 (17.0, 34.8) | 28.0 (19.3, 39.8) | 0.152 | |
| Creatinine, µmol/L | 70.8 |
70.0 |
70.5 |
0.663 | |
| eGFR, mL/min/1.73 m |
99.5 |
98.8 |
100.4 |
0.441 | |
| TC, mmol/L | 5.0 |
5.0 |
5.0 |
0.910 | |
| TGs, mmol/L | 1.6 (1.2, 2.4) | 1.6 (1.2, 2.5) | 1.6 (1.1, 2.2) | 0.579 | |
| LDL-C, mmol/L | 3.0 |
3.0 |
3.1 |
0.799 | |
| HDL-C, mmol/L | 1.00 |
1.00 |
0.99 |
0.832 | |
| Myocardial enzyme | |||||
| pCKMB, ng/mL | 189 (101, 348) | 137 (47, 294) | 244 (139, 486) | ||
| pMYO, ng/mL | 89 (49, 204) | 76 (40, 186) | 112 (59, 300) | 0.039 | |
| pTNI, ng/mL | 30 (26, 50) | 25 (13, 50) | 42 (33, 50) | ||
| pNT-pro BNP, pg/mL | 1433 (789, 2610) | 1131 (576, 2132) | 1952 (946, 3162) | 0.002 | |
| Echocardiography | |||||
| LA, cm | 3.81 |
3.80 |
3.82 |
0.813 | |
| LVEDD, cm | 5.0 |
4.9 |
5.1 |
0.054 | |
| LVESD, cm | 3.5 |
3.4 |
3.7 |
0.002 | |
| LVEF, % | 51.1 |
52.3 |
49.6 |
0.034 | |
| Angiography findings | |||||
| Multi-vessel/LM | 113 (62.1) | 65 (63.7) | 48 (60.0) | 0.607 | |
| Proximal LAD | 74 (40.7) | 36 (35.3) | 38 (47.5) | 0.096 | |
| CTO | 14 (7.7) | 7 (6.9) | 7 (8.8) | 0.635 | |
IMH, intramyocardial hemorrhage; Lym, Lymphocyte; PBMCs, peripheral blood mononuclear cells; Treg, regulatory T cell; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; MI, myocardial infarction; PCI/CABG, percutaneous coronary intervention/coronary artery bypass graft; AGI, alpha-glucosidase inhibitor; DPP-4i, dipeptidyl peptidase-4 inhibitor; SGLT-2i, sodium/glucose cotransporter-2 inhibitor; WBC, white blood cell; hsCRP, hypersensitive C-reactive protein; FPG, fasting plasma glucose; RBG, random blood glucose; HbA1c, glycated hemoglobin; ALT, alanine transaminase; eGFR, estimated glomerular filtration rate; TC, total cholesterol; TGs, triglycerides; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; pCKMB, the peak value of creatine kinase MB; pMYO, the peak value of myoglobin; pTNI, the peak value of troponin I; NT-pro BNP, N-terminal pro-brain natriuretic peptide; LA, left atrium; LVEDD, left ventricular end-diastolic diameter; LVESD, left ventricular end-systolic diameter; LVEF, left ventricular ejection fraction; LM, left main coronary artery; LAD, left anterior descending; CTO, chronic total occlusions.
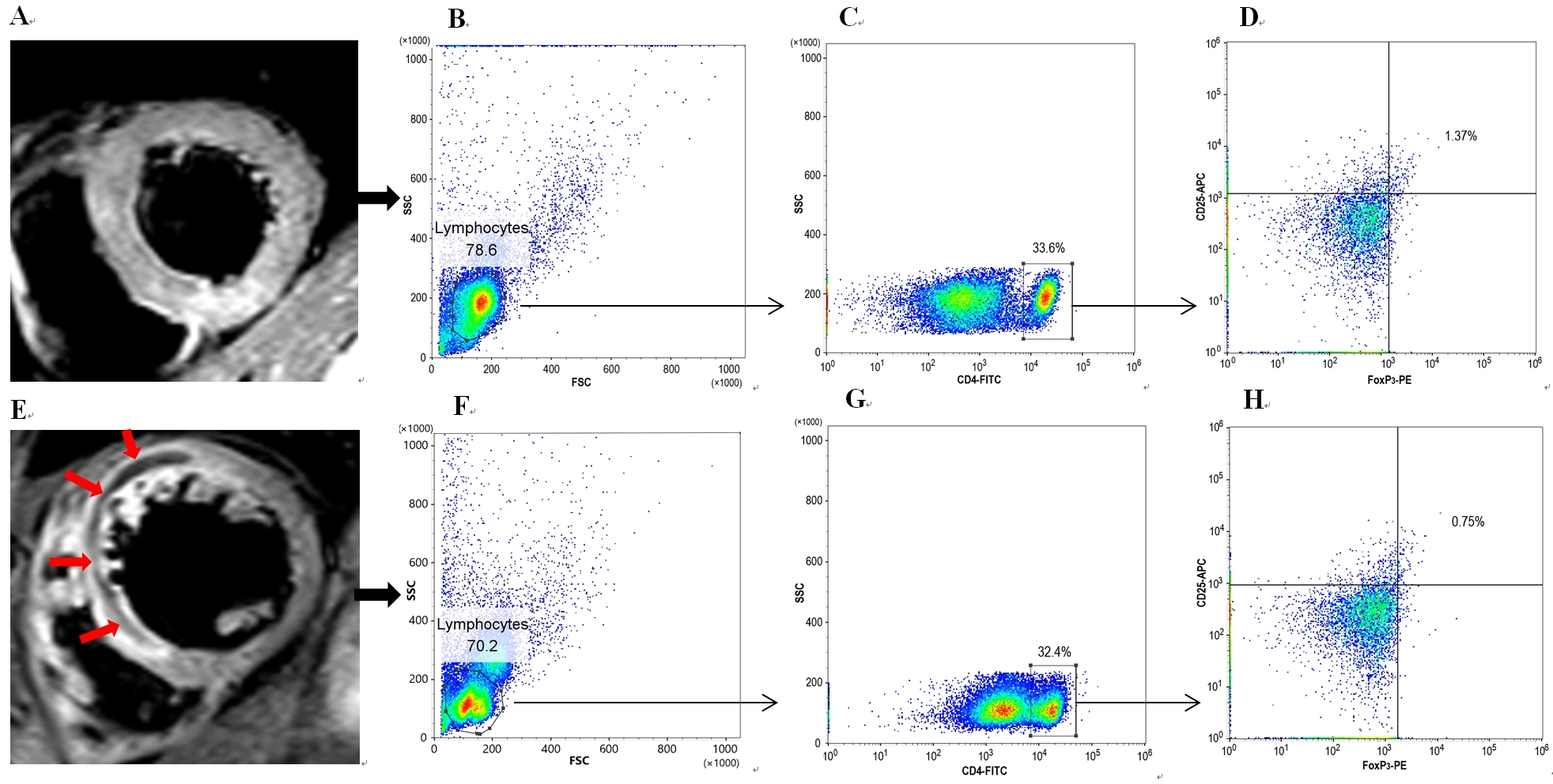
Fig. 1 showed the CMR images and flow scatter diagrams of representative cases of STEMI in patients with IMH group and no-IMH group, respectively. The hypoenhanced region in “panel E” (red arrows) was the area of IMH.
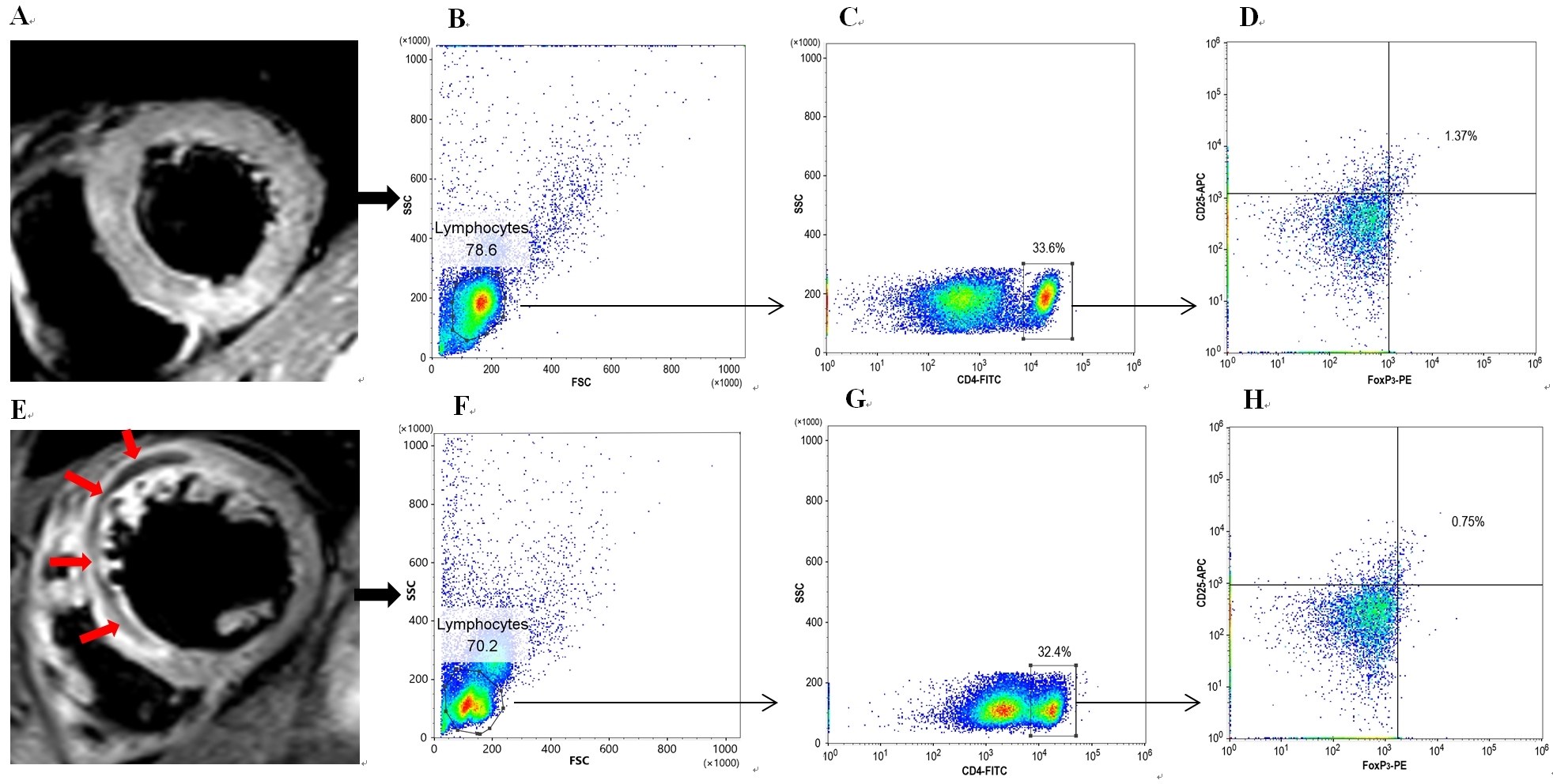 Fig. 1.
Fig. 1.CMR examples with or without IMH burden and their circulating Treg frequencies. Panels (A–D) show a case without IMH burden who is diagnosed as acute anterior myocardial infarction. Panels (E–H) show a case with IMH burden who is also diagnosed as acute anterior myocardial infarction. The red arrows in panel (E) represent the region of IMH. According to panels (D) and (H), the Treg frequency in patients with IMH (0.75%) is significantly lower than that in patients without IMH (1.37%). CMR, cardiac magnetic resonance imaging; IMH, intramyocardial hemorrhage; Treg, regulatory T cell.
Table 2 showed the results of the univariate and multivariate logistic
regression analyses. In univariate analysis, decreased Treg frequency, increased
hsCRP, pCKMB and LVESD were significantly associated with IMH, as were decreased
LVEF, no previous use of ACEI/ARB, anterior MI diagnosed at admission, increased
WBC, FPG and pTNI. Correlation analysis showed that pCKMB was significantly
correlated with pTNI (r = 0.623, p
| Univariate | p value | Multivariate | p value | ||
| OR (95% CI) | Adjusted OR (95% CI) | ||||
| Treg/CD4+ T cells (%) | 0.387 (0.245, 0.613) | 0.350 (0.202, 0.606) | |||
| Age, years | 0.985 (0.960, 1.010) | 0.234 | |||
| Male gender | 1.010 (0.468, 2.179) | 0.979 | |||
| Medical history | |||||
| ACEI/ARB | 0.444 (0.214, 0.921) | 0.029 | 0.504 (0.213, 1.192) | 0.119 | |
| Diagnosis at admission | |||||
| Anterior MI | 2.012 (1.111, 3.650) | 0.021 | 2.066 (0.962, 4.425) | 0.063 | |
| WBC, 10 |
1.128 (1.008, 1.263) | 0.036 | |||
| hsCRP, mg/L | 1.048 (1.019, 1.078) | 0.001 | 1.060 (1.022, 1.100) | 0.002 | |
| FPG, mmol/L | 1.141 (1.027, 1.267) | 0.014 | 1.042 (0.915, 1.187) | 0.537 | |
| Myocardial enzyme | |||||
| pCKMB, ng/mL | 1.004 (1.002, 1.006) | 1.004 (1.001, 1.006) | 0.002 | ||
| pMYO, ng/mL | 1.001 (1.000, 1.003) | 0.123 | |||
| pTNI, ng/mL | 1.105 (1.063, 1.149) | ||||
| pNT-pro BNP, pg/mL | 1.001 (0.998, 1.002) | 0.261 | |||
| Echocardiography | |||||
| LVESD, cm | 2.978 (1.438, 6.165) | 0.003 | 3.329 (1.346, 8.236) | 0.009 | |
| LVEF, % | 0.960 (0.923, 0.997) | 0.037 | 1.054 (0.996, 1.115) | 0.069 | |
IMH, intramyocardial hemorrhage; STEMI, ST-segment elevation myocardial infarction; PPCI, primary percutaneous coronary intervention; OR, odds ratio; CI, confidence interval; Treg, regulatory T cell; ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; MI, myocardial infarction; WBC, white blood cell; hsCRP, hypersensitive C-reactive protein; FPG, fasting plasma glucose; pCKMB, the peak value of creatine kinase MB; pMYO, the peak value of myoglobin; pTNI, the peak value of troponin I; NT-pro BNP, N-terminal pro-brain natriuretic peptide; LVESD, left ventricular end-systolic diameter; LVEF, left ventricular ejection fraction.
In addition, IPTW was also used to assess the predictive effect of the above
risk factors on the occurrence of IMH. IPTW analysis also showed that Treg
frequency [OR (95% CI): 0.371 (0.217–0.635), p
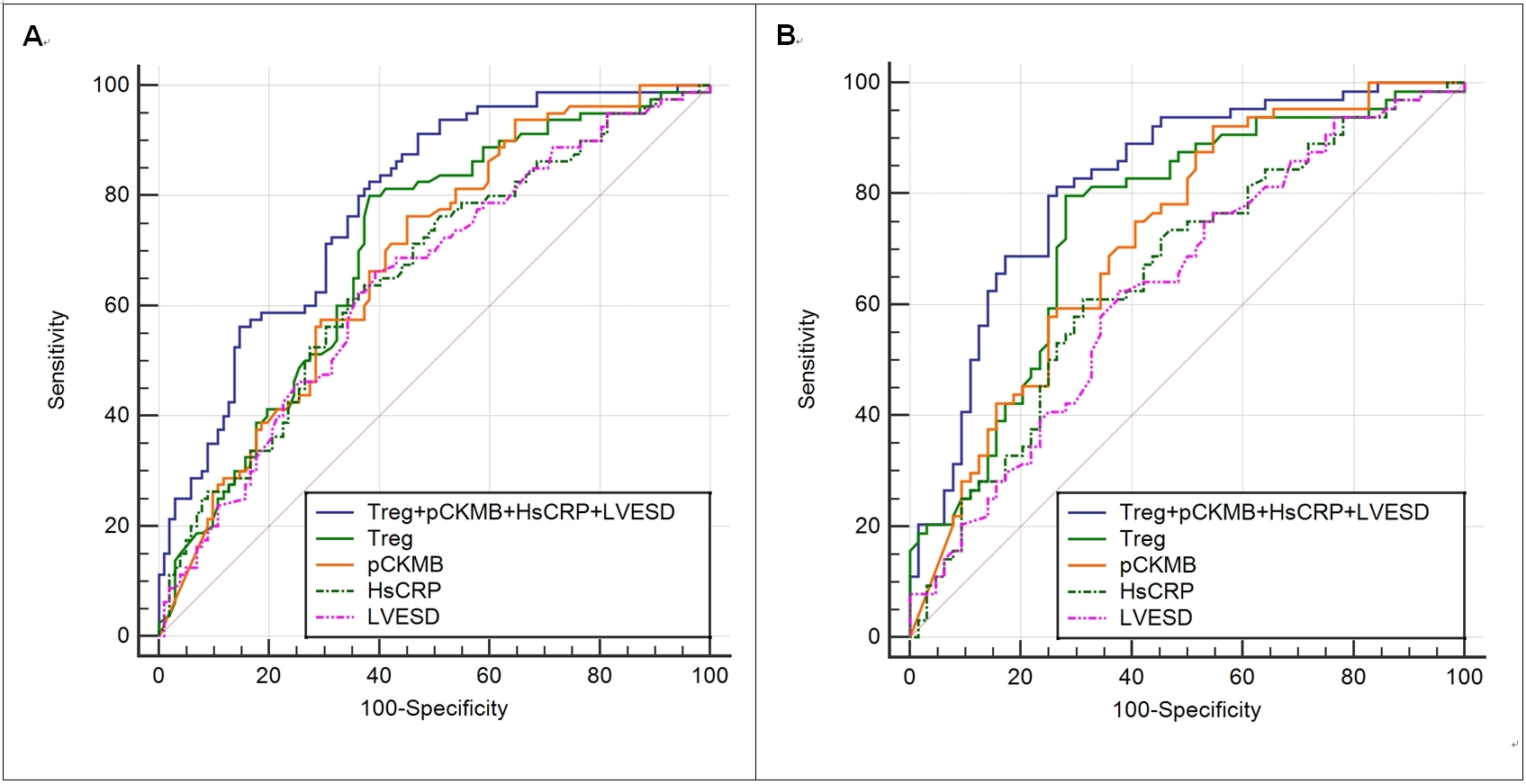
Before PSM, the results of the ROC analysis detailed in Table 3 and Fig. 2
revealed that all 4 biomarkers significantly predicted the presence of IMH (area
under the ROC curve [AUC]: Treg 0.701, pCKMB 0.684, hsCRP 0.658, and LVESD 0.646;
all p
| Cutoff value | AUC | 95% CI | p value | Sensitivity | Specificity | Youden index | ||
| Pre-matching | ||||||||
| LVESD, cm | 3.52 | 0.646* | 0.566–0.726 | 0.001 | 0.663 | 0.608 | 0.270 | |
| hsCRP, mg/L | 5.74 | 0.658* | 0.579–0.738 | 0.613 | 0.657 | 0.270 | ||
| pCKMB, ng/mL | 137.5 | 0.684* | 0.608–0.761 | 0.763 | 0.549 | 0.312 | ||
| Treg, % | 1.07 | 0.701* | 0.625–0.777 | 0.800 | 0.618 | 0.418 | ||
| Treg + pCKMB + hsCRP + LVESD | -/- | 0.786 | 0.721–0.851 | 0.825 | 0.618 | 0.443 | ||
| Post-matching | ||||||||
| LVESD, cm | 3.52 | 0.633* | 0.537–0.729 | 0.009 | 0.625 | 0.625 | 0.250 | |
| hsCRP, mg/L | 5.20 | 0.656* | 0.561–0.751 | 0.002 | 0.609 | 0.687 | 0.297 | |
| pCKMB, ng/mL | 73.2 | 0.721* | 0.633–0.809 | 0.922 | 0.453 | 0.375 | ||
| Treg, % | 1.07 | 0.750 | 0.663–0.836 | 0.797 | 0.719 | 0.516 | ||
| Treg + pCKMB + hsCRP + LVESD | -/- | 0.821 | 0.747–0.894 | 0.813 | 0.734 | 0.547 | ||
Note: Compared with Treg + pCKMB + hsCRP + LVESD *p
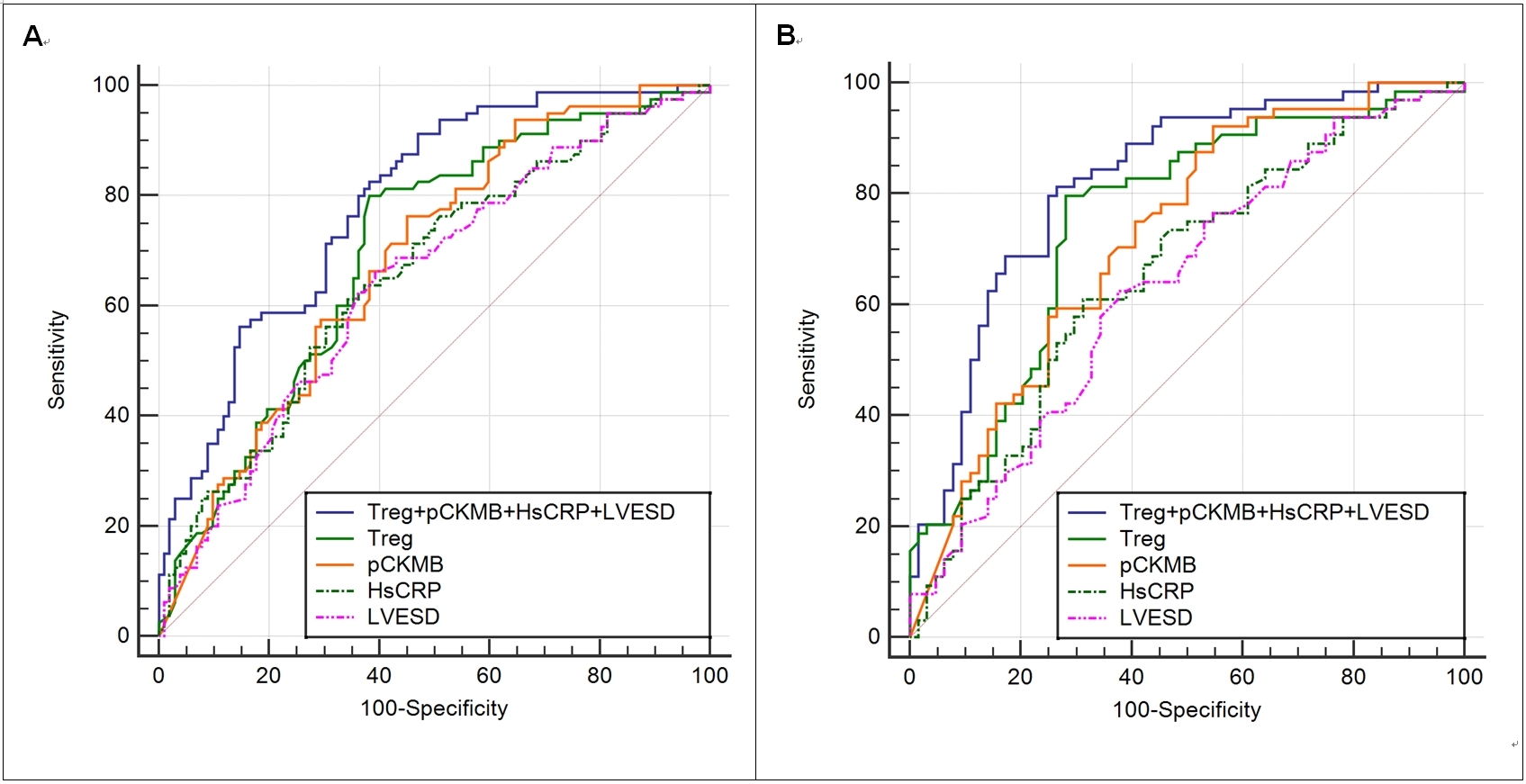 Fig. 2.
Fig. 2.Pre-(A) and postmatching (B) ROC curve analysis of Treg, pCKMB, hsCRP and LVESD for the prediction of IMH. Treg, regulatory T cell; hsCRP, hypersensitive C-reactive protein; pCKMB, the peak value of creatine kinase MB; LVESD, left ventricular end-systolic diameter; IMH, intramyocardial hemorrhage; ROC, the receiver operating characteristic.
After PSM, the age, gender, BMI, medical history (ACEI/ARB), diagnosis at
admission (anterior MI), and FPG were not statistically different between the 2
groups. ROC analysis (Table 3, Fig. 2) still showed that the discriminatory
capability of the 4-biomarker panel was good (AUC 0.821, 95% CI 0.747–0.894)
and stronger than that of the pCKMB, hsCRP and LVESD [with AUC values of 0.721
for pCKMB, 0.656 for hsCRP, and 0.633 for LVESD] (*p
Table 4 showed that compared with the LVESD, hsCRP, pCKMB and Treg, the addition
of the combined index (Treg + pCKMB + hsCRP + LVESD) significantly improved the
reclassification and discrimination ability beyond the baseline risk model with
NRI of 0.197, and IDI of 0.200 (both p
| Category-free NRI | IDI | C-index | |||||||
| Index | 95% CI | p value | Index | 95% CI | p value | Index | 95% CI | p value | |
| Baseline risk model | Ref. | Ref. | 0.661 | 0.580 to 0.741 | |||||
| +LVESD | 0.046 | –0.068 to 0.161 | 0.428 | 0.037 | 0.010 to 0.064 | 0.008 | 0.695 | 0.617 to 0.772 | |
| +hsCRP | 0.058 | –0.101 to 0.217 | 0.476 | 0.027 | 0.003 to 0.052 | 0.030 | 0.685 | 0.607 to 0.763 | |
| +pCKMB | 0.195 | 0.023 to 0.368 | 0.027 | 0.067 | 0.030 to 0.103 | 0.725 | 0.651 to 0.799 | ||
| +Treg | 0.178 | 0.005 to 0.352 | 0.044 | 0.093 | 0.053 to 0.132 | 0.747 | 0.677 to 0.181 | ||
| +Combined | 0.197 | 0.039 to 0.356 | 0.015 | 0.200 | 0.142 to 0.259 | 0.806 | 0.744 to 0.869 | ||
Baseline risk model including diagnosis at admission (anterior myocardial infarction), FPG, ACEI/ARB used before admission and LVEF. Combined index represents Treg, pCKMB, hsCRP combined with LVESD. NRI, net reclassification improvement; IDI, integrated discrimination improvement; CI, confidence interval; Treg, regulatory T cell; ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; hsCRP, hypersensitive C-reactive protein; FPG, fasting plasma glucose; pCKMB, the peak value of creatine kinase MB; LVESD, left ventricular end-systolic diameter; LVEF, left ventricular ejection fraction.
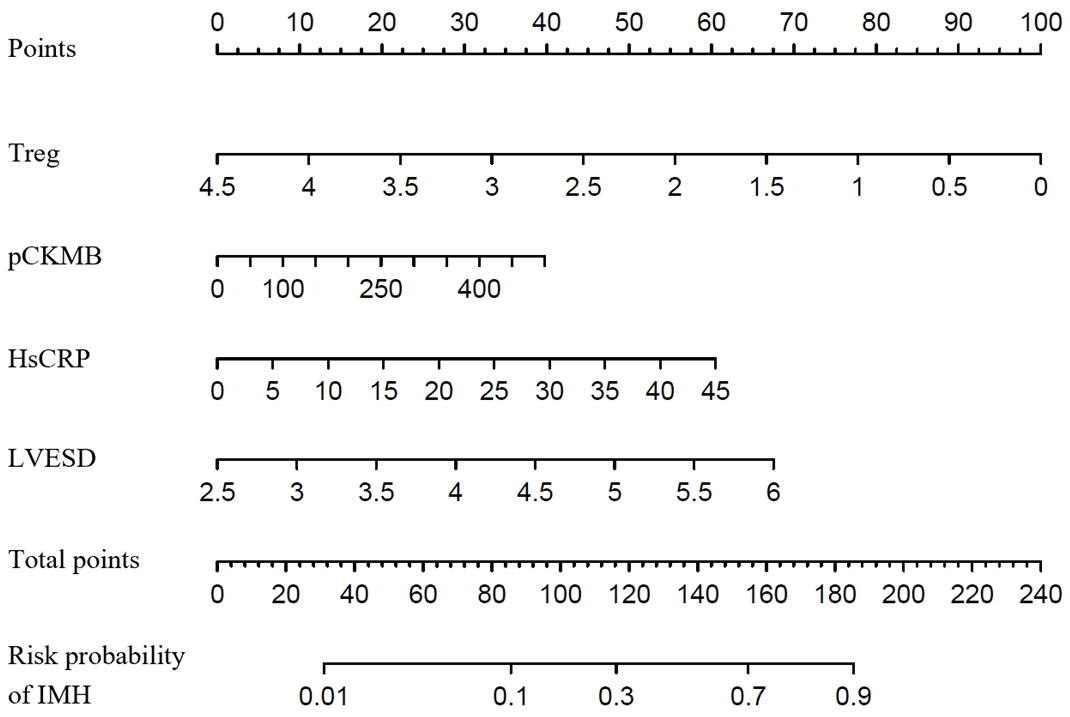
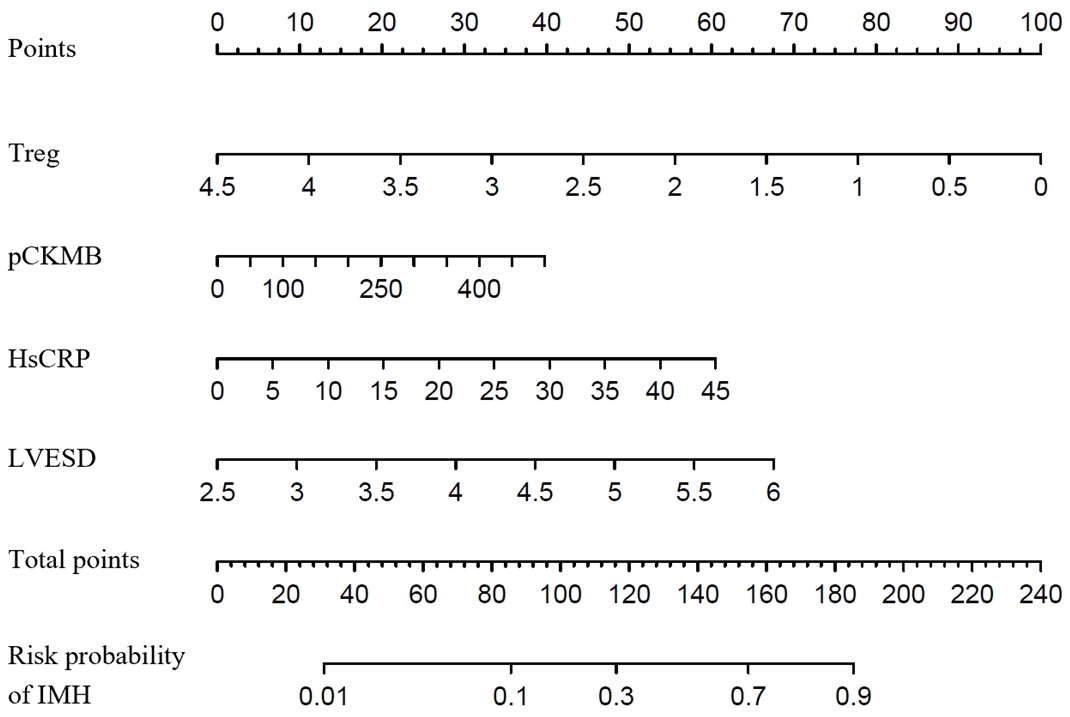 Fig. 3.
Fig. 3.The proposed nomogram for predicting the risk probability of IMH. Treg, regulatory T cell; hsCRP, hypersensitive C-reactive protein; pCKMB, the peak value of creatine kinase MB; LVESD, left ventricular end-systolic diameter; IMH, intramyocardial hemorrhage.
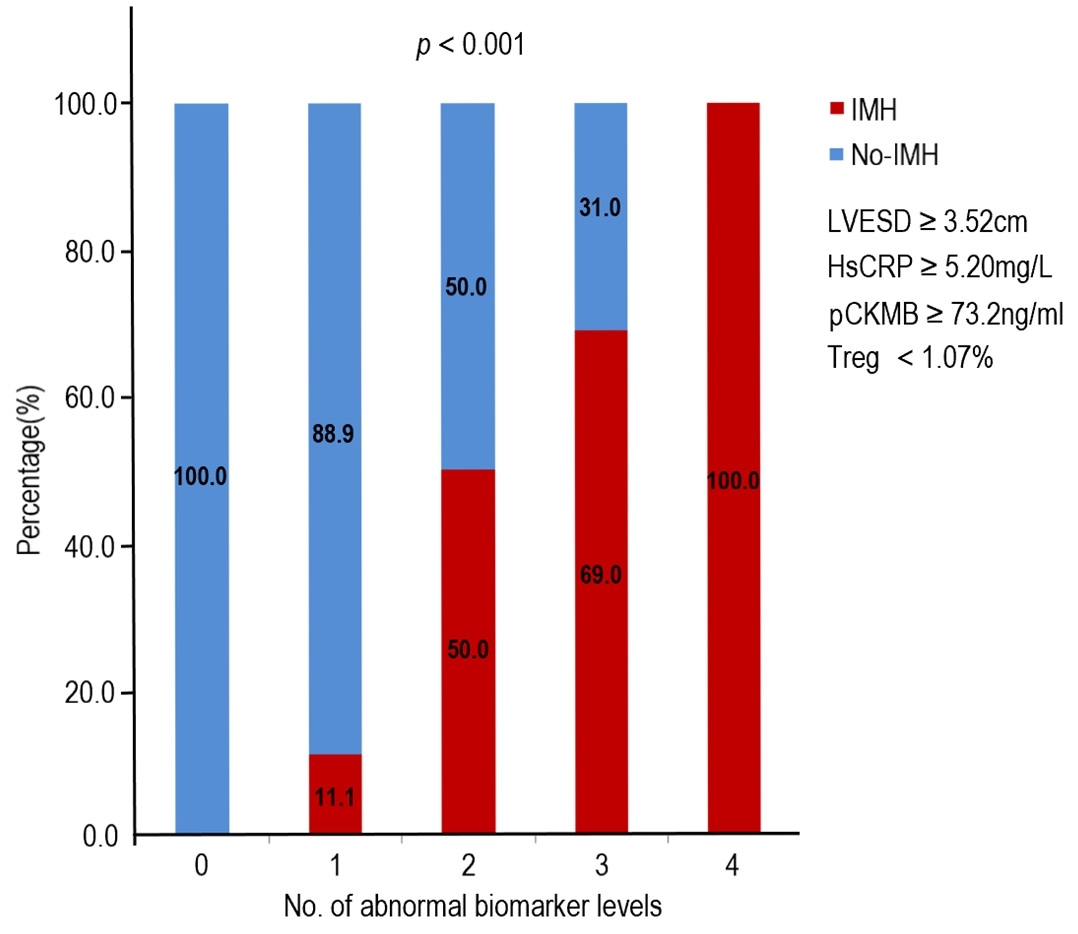
Fig. 4 shows the relationship between the risk of IMH and the number of
abnormal biomarker levels. Based on the cutoff value, biomarker levels are
defined as normal or abnormal. The risk of IMH increased with the number of
abnormal biomarker. The odds of IMH were increased by 11-fold
or 39-fold respectively, if patients presented with abnormal levels of 2 or
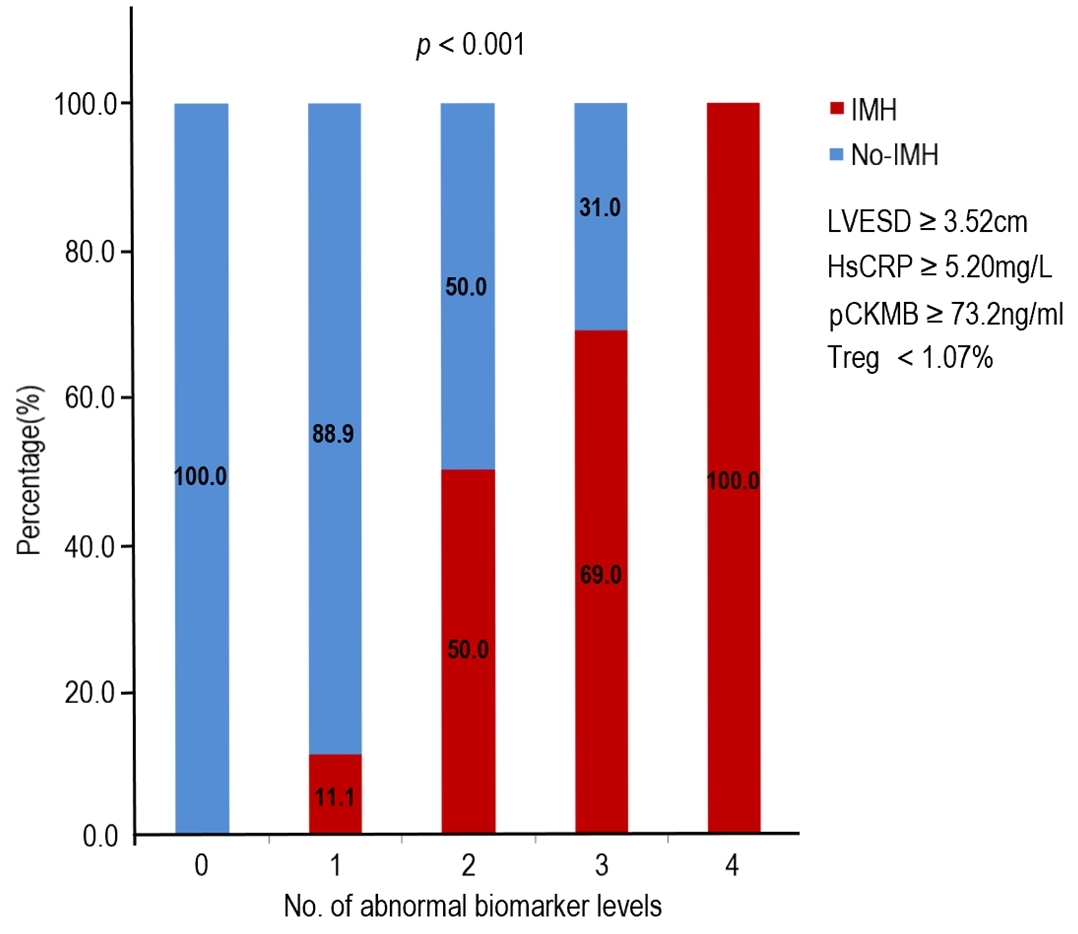 Fig. 4.
Fig. 4.Association of the number of abnormal biomarker levels based on the identified cutoff values and the risk of IMH. Treg, regulatory T cell; hsCRP, hypersensitive C-reactive protein; pCKMB, the peak value of creatine kinase MB; LVESD, left ventricular end-systolic diameter; IMH, intramyocardial hemorrhage.
| No.of Abnormal Biomarkers | No-IMH | IMH | OR (95% CI) | p value |
| 35 (92.1) | 3 (7.9) | 1 | -/- | |
| 2 | 16 (50.0) | 16 (50.0) | 11.7 (3.0–45.8) | |
| 13 (22.4) | 45 (77.6) | 40.4 (10.7–152.8) | ||
Cutoff values for abnormal biomarker levels were LVESD
This study firstly explored the predictive ability of Treg individually or in
combination with other 3 biomarkers, including pCKMB, hsCRP and LVESD, for IMH in
STEMI patients underwent PPCI. The major findings were these: (1) in STEMI
patients received PPCI, IMH group had lower level of Treg frequency than no-IMH
group; (2) Treg frequency, pCKMB, hs-CRP and LVESD were independent risk factors
for IMH; (3) the discriminatory capability of the 4-biomarker panel (combination
of Treg, pCKMB, hsCRP and LVESD) for IMH was stronger than those of the biomarker
individually, except Treg; and (4) increased number of abnormal biomarkers led to
a significant increase in the risk of IMH (Treg
Acute myocardial infarction, including non-ST elevated myocardial infarction and STEMI, is the leading cause of cardiovascular disease and mortality worldwide [25]. In STEMI, the coronary artery is often acutely completely blocked, and it is pivotal to open the infarct-related artery (IRA) urgently. Therefore, the preferred treatment strategy for STEMI patients within 12 h of symptom onset is coronary revascularization by PPCI in combination with antithrombotic therapy [1, 2]. However, despite the IRA’s epicardial flow has been restored, a sizable proportion of patients continue to experience hypoperfusion of myocardial tissue after PPCI, called no-reflow phenomenon. IMH is a form of no-reflow phenomenon resulting from the extensive erythrocyte aggregation and extravasation because of the damaged endothelial walls [5, 6]. IMH can be visualized by T2-weighted CMR because breakdown products of hemoglobin are paramagnetic and influence regional magnetic tissue properties [26]. However, not all patients are suitable for CMR to clarify the presence of IMH, such as those with serious condition or contraindications. Therefore, we urgently need to find a simple and effective method to predict the presence of IMH. Carrick et al. [11] revealed that IMH was a better predictor of adverse events after myocardial infarction than MVO. Husser et al. [27] found that the incidence of MACEs was significantly higher in the IMH group than in the non-IMH group. In addition, the Kaplan-Meier analysis showed that the MACE-free survival was significant prolonged in patients without IMH, and IMH is a predictor of poor myocardial remodeling [27]. In addition, Amier et al. [3] also demonstrated that IMH was associated with larger myocardial infarct size, greater MVO range, and lower LVEF. Therefore, in this study, we analyzed various indexes of myocardial enzymes and left ventricular structure, and found that pCKMB and LVESD were independent predictors of IMH. Although the molecular mechanisms involved in the initiation and progression of MIRI are still not completely understood, accumulating evidences have suggested that excessive inflammation plays a predominant role in it [15, 28]. And Carrick et al. [11] also found that IMH was associated with markers of inflammation, including peak monocyte count and peak neutrophil count. In this study, we also found that inflammatory markers were significantly higher in patients with IMH than in patients without IMH, and hsCRP was an independent predictor of IMH. Considering that Treg cells have been verified to playing an anti-inflammatory effect in MIRI by inhibiting the macrophage inflammatory phenotype and neutrophil function in animal experiments [18, 21, 22], we hypothesized that the circulating Treg levels are related to the presence of IMH in STEMI patients. The final results were consistent with our expectation that Treg is a protective factor of IMH and can independently predict IMH occurrence in STEMI patients received PPCI. Moreover, we proposed for the first time that Treg can be combined with pCKMB, hsCRP and LVESD to predict the presence of IMH. These findings not only indirectly indicated that Treg may have a certain protective effect on human MIRI, but also provided us with a simpler method to predict IMH than CMR, especially for those who can’t finish the CMR. Considering that previous studies have reported that adoptive transfer of Tregs is beneficial in kidney, brain, liver and myocardial ischaemia/reperfusion (I/R) injury [19, 20, 29, 30], we can assume that adoptive transfer of Tregs can significantly reduce the occurrence of IMH in STEMI patients received PPCI. In the future, we will do a lot of work to confirm the scientific hypothesis that adoptive transfer of Tregs may be an effective biologic therapy for the prevention or treatment of IMH after myocardial infarction.
Limitations of the study are as follows. First, it was a single-center study with a small sample size. Therefore, the research results obtained need to be further verified by a large sample size and multi-center study. Second, because the laboratory parameters are measured only once, there may be potential bias due to measurement error. Third, this study did not include the follow-up data, and it is not clear whether Treg levels can predict prognosis of STEMI patients. In future work, we will not only continue to expand the sample size to confirm the stability of the conclusions, but also collect the follow-up data to further explore the impact of Treg level on the prognosis.
In a word, the current study firstly showed that Treg individually or in combination with pCKMB, hsCRP, and LVESD can effectively predict the presence of IMH in STEMI-PPCI patients.
IMH, intramyocardial hemorrhage; STEMI, ST-segment elevation myocardial infarction; PPCI, primary percutaneous coronary intervention; Treg, regulatory T cell; pCKMB, the peak value of Creatine Kinase MB; hsCRP, high-sensitivity C-reactive protein; LVESD, left ventricular end-systolic diameter; NRI, net reclassification improvement; IDI, integrated discrimination improvement; PSM, propensity score matching; IPTW, inverse probability weighting; TIMI, thrombolysis in myocardial infarction flow; MVO, microvascular obstruction; LV, left ventricular; MACEs, major adverse cardiac events; CMR, cardiac magnetic resonance; MIRI, myocardial ischaemia/reperfusion injury; IRI, ischaemia-reperfusion injury; Th1, T-helper 1; Th2, T-helper 2; Th17, T-helper 17; CABG, coronary artery bypass graft; LVEF, left ventricular ejection fraction; eGFR, estimated glomerular filtration rate; PBMCs, peripheral blood mononuclear cells; Foxp3, transcription factor Forkhead box P3; FITC, fluorescein isothiocyanate; APC, allophycocyanin; PE, phycoerythrin; SD, standard deviation; AAR, area at risk; ROC, receiver operating characteristic; ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; WBC, white blood cell; FPG, fasting plasma glucose; pMYO, the peak value of myoglobin; pTNI, the peak value of troponin I; pNT-pro BNP, the peak value of N-terminal pro-brain natriuretic peptide; AUC, area under the ROC curve; IRA, infarct-related artery.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
YZ participated in the design of the project, the implementation of basic experiments, the statistics of data and the writing of manuscripts. HG, LL and SYL participated in the acquisition of data and the revision of the manuscript. YH, JSL, BH and DHL participated in the data analysis of CMR and the drafting of the content of CMR. HC and WPL contributed discussion and edited the manuscript. HWL provided funding support, designed the study and revised the discussion section of the manuscript. All authors read and approved the final manuscript.
The study data collections were approved by the Institutional Review Board of Beijing Friendship Hospital affiliated to Capital Medical University (Approval No. DR20190043), and written informed consent was obtained from all patients.
We sincerely thank all staffs who have contributed to this subject.
This work was supported by the National Key R&D Program of China (Grant No.2021ZD0111000), the National Natural Science Foundation of China (Grant No.82070357) and Beijing Key Clinical Subject Program.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.rcm2407205.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.