1 Department of Psychology, University of Bielefeld, 33501 Bielefeld, Germany
2 Department of Psychology, University of Kassel, 34127 Kassel, Germany
3 Clinic of Neurology, Klinikum Ernst von Bergmann, 14467 Potsdam, Germany
4 Department of Psychology, Humboldt Universität zu Berlin, 12489 Berlin, Germany
5 The George Institute for Global Health, University of New South Wales, 2042 Sydney, Australia
6 Faculty of Health and Care, The University of Central Lancashire, PR1 2HE Preston, UK
†These authors contributed equally.
Academic Editor: Imran Khan Niazi
Abstract
Background: Post-stroke depression (PSD) is the most frequent mental illness after stroke, affecting about 30% of stroke survivors and hampering rehabilitation outcome. While current guidelines recommend monitored antidepressant treatment (ADT) in PSD, the limited precision between the use and need of ADT in clinical practice remains underassessed and poorly understood. Methods: Depression according to DSM criteria and ADT was assessed in n = 294 stroke survivors from two German rehabilitation centers about one, six, and twelve months after stroke. At each measurement occasion, PSD and current use of ADT was assessed, leading to four subgroups: PSD (yes/no) and ADT (yes/no). Frequencies of ADT and PSD were examined and analyzed with regard to depression severity (minor/major). Intra-individual trajectories were used to assess the persistence in ADT over- and undertreatment from a longitudinal perspective. Results: After one, 6 and 12 months, 36.7%, 31.1% and 25.5% of stroke survivors fulfilled the criteria for depression. Across all measurement occasions, 53% of depressed stroke survivors did not receive ADT, while 12% of the non-depressed did. ADT between stroke survivors with major or minor depression differed at baseline but not thereafter. Between 15–40% of the depressed without ADT experienced persisting undertreatment and 25–50% the non-depressed with ADT had not fulfilled depression criteria at an earlier time point. Conclusions: Depression occurred in one in three stroke survivors. Among these, only one in two received ADT, irrespective of PSD severity after discharge. In contrast, one in eight stroke survivors without depressive disorder received ADT, about half of them in the absence of earlier PSD. In conclusion, we found evidence of both under- and overtreatment of PSD with ADT, which emphasizes the need for a more stringent implementation of current PSD guideline recommendations.
Keywords
- stroke
- depression
- treatment
- antidepressants
- rehabilitation
- serotonin reuptake inhibitors
Depression is a long-term complication of stroke affecting about 30% of all stroke survivors at any given point after stroke [1, 2]. Systematic reviews show that post stroke depression (PSD) is associated with worse rehabilitation outcome and higher mortality [3, 4]. Moreover, PSD has been found to prolong functional and vocational recovery, reduce life satisfaction [5], and render the use of rehabilitation services less efficient [6, 7, 8].
Previous evidence of clinical trials suggests that antidepressant treatment (ADT)—especially selective serotonin reuptake inhibitors (SSRI)—can be an effective agent to treat PSD or lower the risk to develop depressive symptoms after stroke [9, 10, 11, 12, 13]. Although treatment guidelines concordantly emphasize the need of early identification followed by swift and evidence-based treatment of PSD [14, 15, 16], PSD still remains underdiagnosed and undertreated [5, 17, 18]. With regard to ADT, evidence from register and community-based samples [19, 20, 21, 22], which capture the clinical practice, showed that the match between the need and the use of ADT in stroke survivors suffering from PSD is far from optimal (cf. Online Supplementary Table 1). In fact, previous studies [19, 20, 21] revealed that ADT had been received by only about 23–49% of stroke survivors with persisting and/or clinically relevant depressive symptoms between three and 12 months after the event. Moreover, amongst the stroke survivors with chronic PSD throughout the first year who did not receive ADT after three months, only 19% reported a change in their treatment, i.e., the start of ADT after the first year [20]. At the same time, of those stroke survivors with ADT, between 53–68% did not report depressive symptoms [19, 20, 21], with even 63% of them reporting no depressive symptoms at any prior measurement occasion [20]. This mismatch, or lack in precision of ADT selection, also seems to persist beyond the first year after stroke [22], with evidence [23, 24] showing that up to five years after stroke, only about 22–26% of depressed stroke survivors reported to receive ADT while 59–72% without PSD did receive ADT.
For the proportion of non-depressed stroke survivors with ADT, these results might indicate that the prescribed ADT was effective and might have been used as relapse prevention. Alternatively, it might suggest that ADT was effective but not (yet) terminated after remission, or that stroke survivors without PSD may have received ADT without clear indication. After stroke, especially SSRIs are used as ADT to facilitate other aspects of recovery (e.g., motor recovery) next to PSD, which may contribute to the described mismatch between the use and need of ADT. In fact, the FLAME-trial, which was published in 2011, suggested that the SSRI fluoxetine could promote functional recovery [25], which might have fostered an increased off-label use of SSRIs [26]. However, several more recent studies based on large samples could not replicate this effect [10, 11, 27]. Furthermore, while a potential off-label use might explain certain parts of the current mismatch in terms of overtreatment, it would not explain the current undertreatment of PSD with ADT, i.e., the striking proportion of stroke survivors with PSD who do not receive recommended ADT [19, 20, 21].
In short, the above-mentioned studies suggest that both under- and overtreatment are common phenomena in the treatment of PSD, underlining existing recommendations that the selection for ADT should be more precise [5, 20]. Notably, most of these studies relied on cut-offs based depression severity scales [20, 21] or screening questions (e.g., “Do you feel depressed?”) [19, 22] to assess the presence of PSD (yes/no), which was then used to relate PSD to ADT. However, according to treatment guidelines, prescription of ADT should be based on clinical diagnoses or diagnostic criteria from established classification systems, like the Diagnostic and Statistical Manual of Mental Disorders (DSM) [28] and the International Classification of Diseases (ICD) [29]. However, it is yet to be examined if the assessment of PSD based on established classification criteria might explain parts of the current mismatch in ADT use in stroke survivors with or without PSD.
The primary aim of our study was to examine the relationship between PSD and ADT while applying DSM criteria of depressive disorders based on structured clinical interviews. Secondly, we examined if the frequency of ADT depends on the assessed depression severity. In our study, depression severity was diagnosed using the DSM categories “minor” (i.e., 2–4 depressive symptoms according to DSM, with at least one of them being depressed mood or loss of interest during a 2-week period) and “major” (i.e., more than five depressive symptoms according to DSM, also with depressed mood and/or loss of interest amongst them for a 2-week period). Although depression criteria in DSM-5 were not changed in comparison to DSM-IV-R, DSM-5 no longer allows a symptom-based categorization in minor and major depression [30]. However, both minor and major depression are usually included in the definition of PSD in recent systematic reviews [1, 2, 5] and are a relevant distinction for depression in the general population [31, 32] and for PSD [5, 33, 34, 35]. Moreover, the aforementioned studies assessing use of ADT [19, 20, 21, 22, 36] did not use the rather high threshold of the DSM-5 major depression diagnosis [25] or did not explicitly use the DSM-5 major depression diagnosis as inclusion criteria [10]. Also with regard to its relevance for the clinical practice, the disappearance of the minor depression category in DSM-5 was criticized [30]. We therefor used the DSM-5 criteria to assess depression while extending our analysis by using minor and major categories from DSM-IV-R to determine PSD severity. As a third aim of our study, proportions of PSD and ADT were analyzed from a longitudinal perspective to examine the persistence of a possible mismatch in ADT prescriptions.
Participants: Stroke survivors were recruited from two German
rehabilitation centers. The examined participants stem from the prospective
longitudinal “Berlin PSD study” (for a comprehensive description see [7, 37]).
Inclusion criteria were (1) occurrence of ischemic stroke diagnosed in medical
record within six months before baseline assessment, (2) sufficient verbal
comprehension as defined by a score of
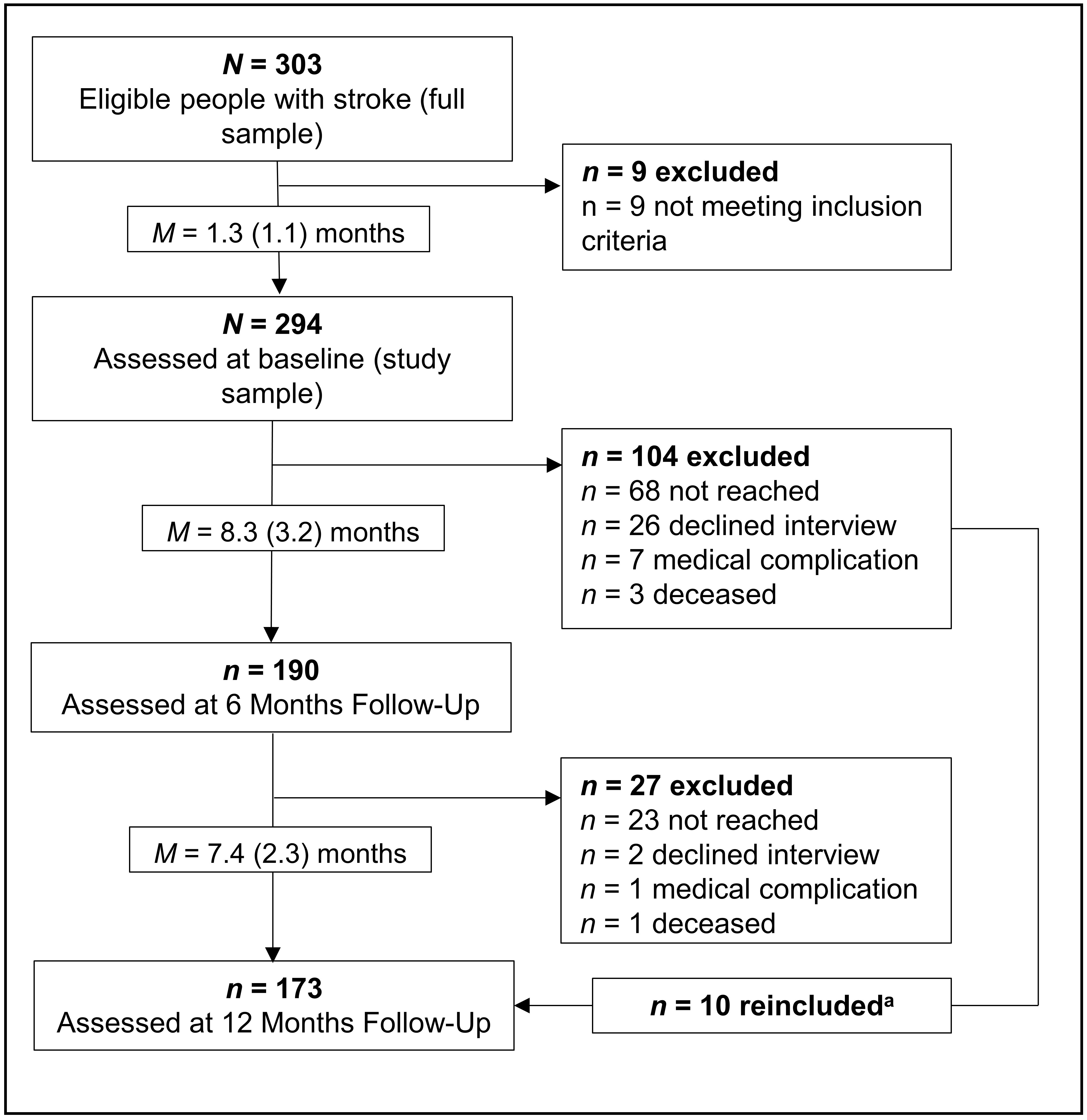
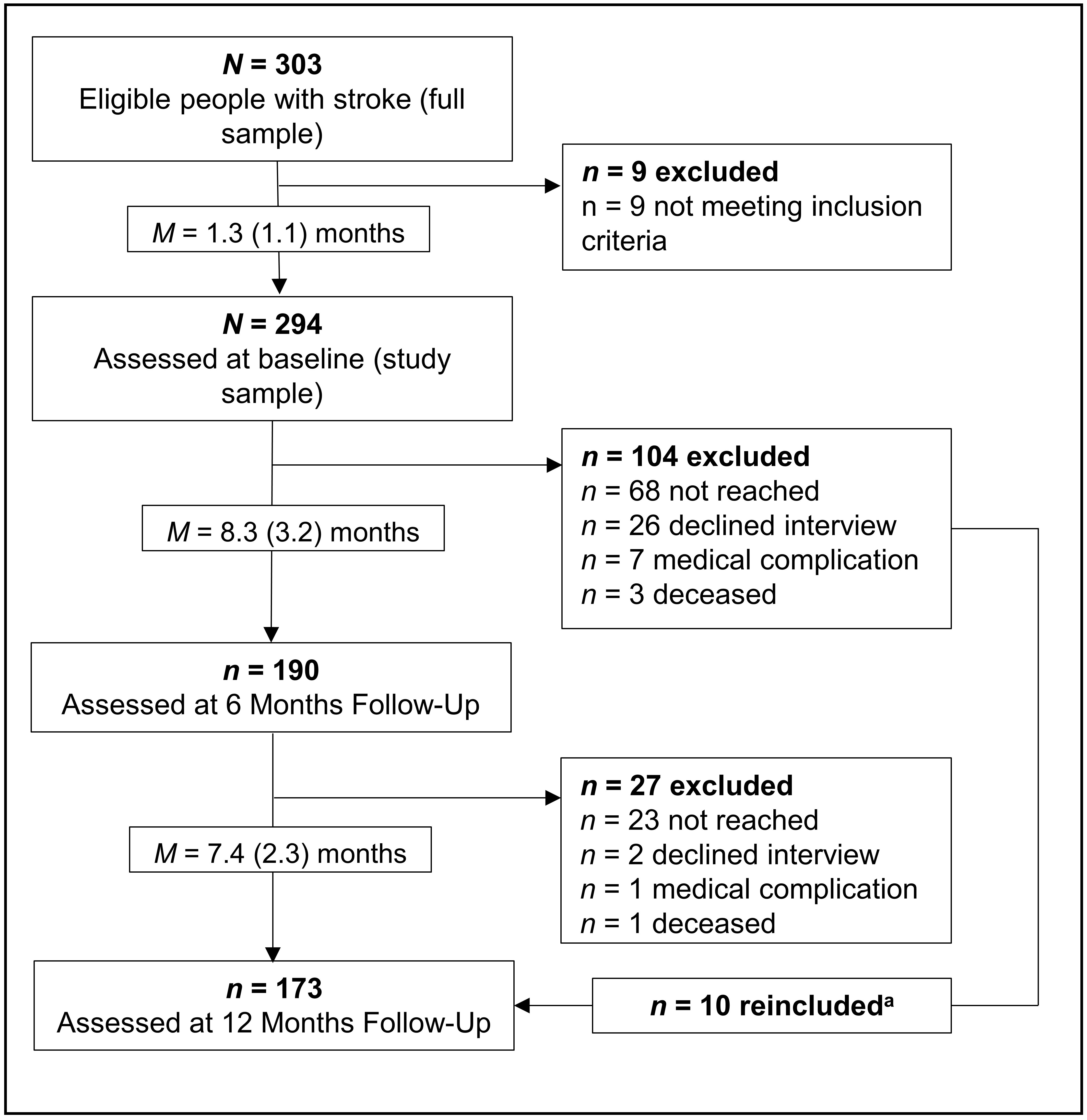 Fig. 1.
Fig. 1.Participation and attrition across all three measurement
occasions. Values in brackets show standard deviations.
| Baseline (T0) characteristics (n = 294) | M (SD) | |||
| Age | 63.78 (10.82) | |||
| Education (years) | 11.37 (3.06) | |||
| ADL (Barthel-Index) | 85.72 (20.29) | |||
| Stroke severity (mNIHSS) | 3.85 (3.52) | |||
| % (n) | ||||
| Previous depression (% yes) | 13.6% (40) | |||
| Gender (% female) | 40.1% (118) | |||
| Subgroup characteristics | Baseline (T0) | 6-months (T1) | 12-months (T2) | |
| n = 294 | n = 190 | n = 173 | ||
| % DSM-5 Depression [minor/major] | 35.7% [18.0/17.7] | 31.1% [15.8/15.3] | 25.5% [14.5/11.0] | |
| D+ | 105 (35.7%) | 59 (31.1%) | 44 (25.4%) | |
| ADT+ | 39 (37.1%) | 20 (33.9%) | 16 (36.7%) | |
| ADT– | 66 (62.9%) | 32 (54.2%) | 19 (43.2%) | |
| NA | - | 7 (11.9%) | 9 (20.5%) | |
| D– | 189 (64.2%) | 131 (68.9%) | 129 (74.6%) | |
| ADT+ | 29 (15.3%) | 12 (9.2%) | 14 (10.9%) | |
| ADT– | 159 (84.1%) | 106 (80.9%) | 98 (75.9%) | |
| NA | 1 (0.5%) | 13 (9.9%) | 17 (13.2%) | |
| Note: M, mean; SD, standard deviation; mNIHSS, modified National Institute of Health Stroke Scale; ADL, Activities of Daily Living were assessed using the Barthel-Index; NA, missing value. Proportions of the two groups D+ and D– refer to the sample of the corresponding measurement occasion, proportion of ADT+ and ADT+ within these two groups refer to the corresponding sample size of the D+/D– group. | ||||
Procedure: After given informed consent, baseline (T0) assessments of stroke survivors took place during their in-patient rehabilitation M = 6.8 (SD = 3.7) weeks after stroke and at planned intervals of six (T1) and 12 months (T2) later. Participants did not receive compensation. Baseline assessments were conducted by trained neuropsychologists in the respective rehabilitation clinic. Follow-up interviews (T1, T2) were conducted by trained psychology students (B.Sc., M.Sc.) via telephone. Participants were considered as dropouts if they could not be reached seven times over the course of several weeks. Participants were re-included when reached at the next follow-up assessment (cf. Fig. 1).
Measures: In addition to baseline demographic variables, depression was diagnosed at all three measurement occasions according to DSM-5 criteria [28] using structured clinical interviews [40]. Use of antidepressants was extracted from medical records at baseline and assessed via semi-structured telephone interviews at six- and 12-months follow-up. If medication intake was not managed by the stroke survivors themselves, information from relevant caregivers was used. ADM was SSRI for the majority (about 70%) of stroke survivors. Reported ADM classes were: SSRI, selective serotonin and norepinephrine reuptake inhibitors (SSNRI), noradrenergic and specific serotonergic antidepressants (NASSA), tri- and tetracyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAO) (cf. Online Supplementary Table 1).
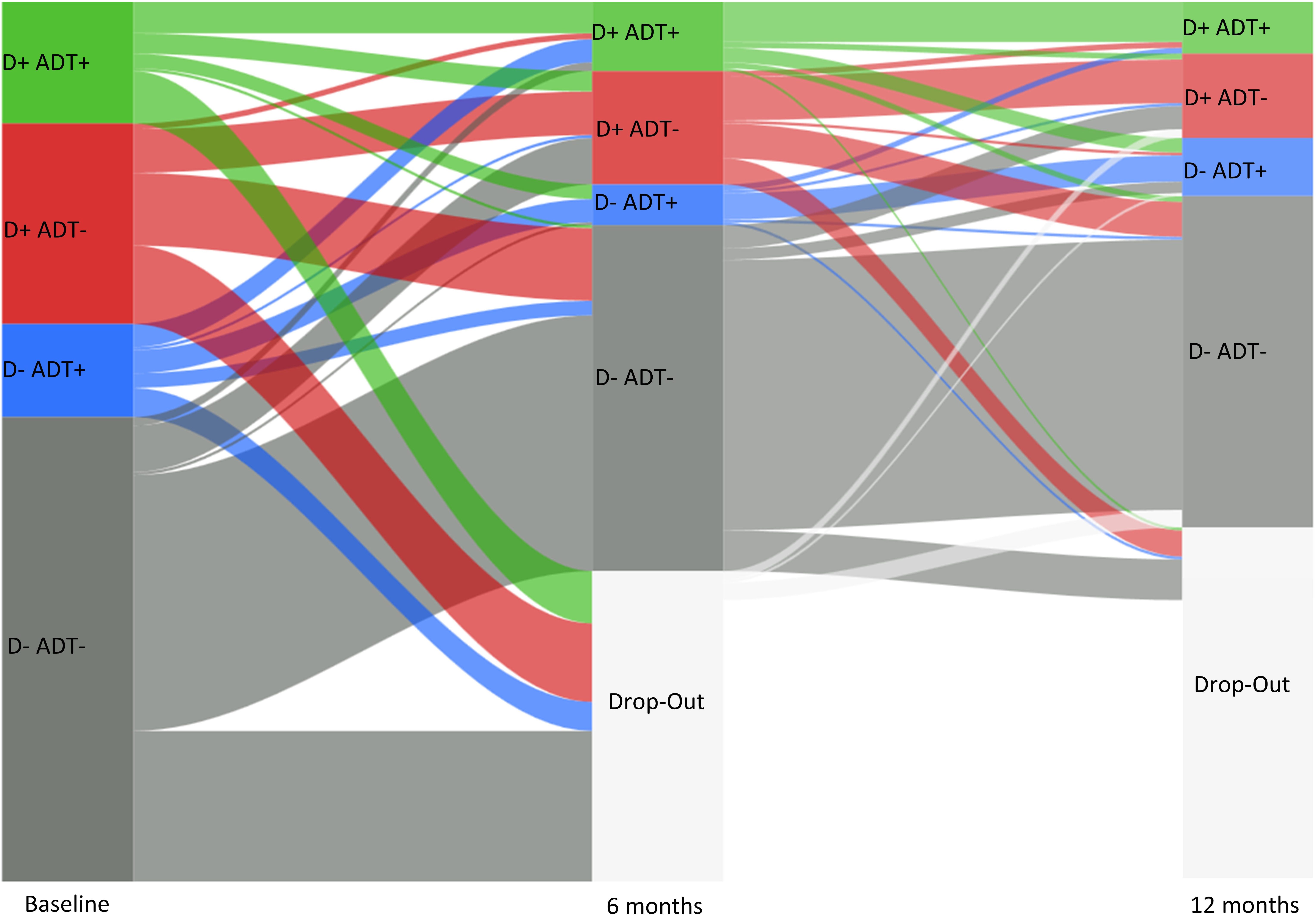
Statistical analysis: Depression rates according to DSM criteria (minor
and major), and use of ADT were determined for each assessment. Longitudinal
(i.e., intra-individual) trajectories of the four subgroups (depression: D+/D–,
antidepressant treatment: ADT+/–) were visualized using a Sankey-chart [41].
Trajectories of non-depressed stroke survivors receiving ADT at follow-up were
traced back to evaluate indication and persistence of ADT.
Dropout and missingness: Complementary dropout and missingness analyses
were performed using logistical regression models to investigate if stroke
survivors’ participation (yes/no) or ADT missingness depended on: demographics
(age and sex), ADT at admission and discharge, clinical variables (stroke
severity, activities of daily living and previous depression) and DSM depression
diagnosis at the previous time point. For ADT missingness previous participation
in one or two of the follow-up(s) was additionally included into the analysis.
All calculations were performed in the R environment (Version 4.1.0, R Foundation for Statistical Computing, Vienna, Austria [42]). For
logistical regressions, the package lme4 [43] was used. Significance level was
set at p
Dropout rates were 35.4% (n = 104) at 6 months and 9.8% (n =
17) at 12 months follow-up (cf. Table 1 and Fig. 2) and did not differ across
subgroups. Logistic regression models showed that neither participation
nor missingness in ADT depended on demographic, clinical variables, or DSM
depression diagnosis at the preceding measurement occasion (Participation: T1:
all p
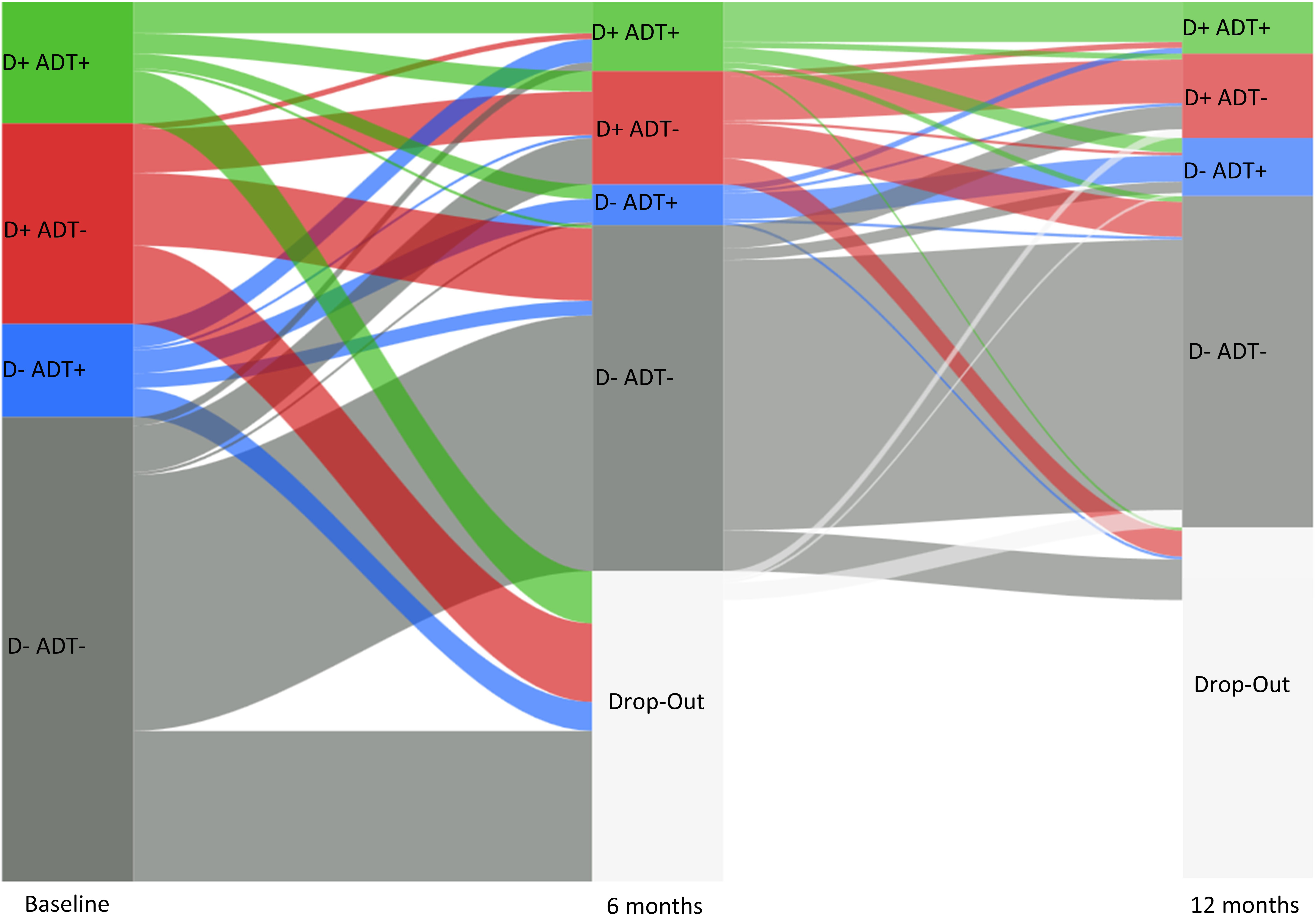 Fig. 2.
Fig. 2.Transitions among the subgroups of depressed (D+) and non-depressed (D–) stroke survivors with (ADT+) and without antidepressant treatment (ADT–) over the three measurement occasions baseline (T0), 6 months (T1) and 12 months (T2) follow-up.
Prevalence of PSD based on DSM criteria for depressive disorder [in brackets: minor/major] was 30.8 [16.1/14.7]% across all three measurement occasions with T0: 35.7 [18.0/17.7]%; T1: 31.1 [15.8/15.3]%; T2: 25.5 [14.5/11.0]%. Relative frequencies of the four subgroups for all measurement occasions are shown in Table 1 with corresponding trajectories of stroke survivors across and within those subgroups visualized in Fig. 2. Compared to the full baseline sample, stroke survivors with PSD and ADT (Group D+/ADT+) constituted 13.3%, and 37.1% of the D+ group. The D+/ADT+ group constituted 10.5% (33.9% of the D+ group) at T1, and 9.3% (36.7% of the D+ group) at T2. Stroke survivors who were not depressed but did receive antidepressants (D ADT+) comprised 9.9% of the full baseline sample (15.3% of the D– group), and 6.3% (9.2% of D– group) and 8.1% (10.9% of D– group) for T1 and T2, respectively. Those neither depressed nor receiving antidepressant (D+/ADT–) included 54.1% of the baseline sample (84.1% of D– group), 55.8% (80.9% of D– group) at T1 and 56.7% (75.9% of D– group) at T2. Stroke survivors who were depressed but did not receive antidepressants (D+/ADT–) comprised 22.4% of the full baseline sample (62.9% of the D+ group), and 16.8% (54.2% of D+ group) and 10.9 (43.2% of D+ group) for T1 and T2, respectively.
Depression severity and ADT: At baseline, the frequency of ADT in minor
or major depressive disorder differed significantly (
Persistence of PSD and ADT: Longitudinal analyses showed that 47.6% of depressed stroke survivors (D+ group) at T1 were already depressed at baseline, and 29.5% were depressed throughout the first year. Moreover, 78.1% of stroke survivors receiving ADT at T1, already reported ADT at baseline, and 16.9% received ADT throughout the complete first year.
PSD undertreatment: Proportions of depressed stroke survivors without ADT (D+/ADT– group) were 62.9% (T0), 54.2% (T1) and 43.2% (T2). From longitudinal perspective, trajectory analyses showed that of the 47.6% with T1 and baseline depression (see above), 18.7% did not receive ADT at either baseline or T1. For T2, a total of 29.5% of depressed stroke survivors reported depression throughout both previous measurement occasions while 25.4% did not receive ADT at either T1 or T2 and 4.5% at both.
PSD overtreatment: Proportion of non-depressed stroke survivors with ADT (D–/ADT+ group) were 15.3% (T0), 9.2% (T1) and 10.9% (T2). Longitudinal analysis showed that for T1, 4.6% of non-depressed stroke survivors (D– group) reported to receive ADT at both baseline and T1. For T2, 2.3% of non-depressed stroke survivors reported to have received ADT across all measurement occasions, and 3.9% when only baseline (but not T1) was taken into account. Moreover, 6.2% received ADT at either T1 or T2 without having reported PSD at all.
The primary aim of this study was to examine the relationship between PSD and ADT by applying DSM criteria of depressive disorders based on structured clinical interviews. Confirming previous research, one in three stroke survivors developed PSD throughout the first year after stroke [1, 2, 5]. Across all measurement occasions, our results showed that only about one in two depressed stroke survivors received ADT over the first year after stroke, emphasizing previous research which indicated that PSD is still significantly undertreated [5, 15, 19, 20]. Furthermore, our results showed significant overtreatment across all measurement occasions, given that about one in eight stroke survivors received ADT without reporting depressive symptoms. This also is in line with previous evidence assessing this aspect of the known mismatch between PSD and ADT [17, 19, 20].
Our secondary aim was to assess if ADT was associated with the severity of PSD based on the DSM categories of minor and major depression. In our sample, ADT was linked to PSD severity at baseline, but not at the two follow-ups throughout the first year after stroke. This means that stroke survivors with major depression were more likely to receive ADT than those with minor depression in the rehabilitation clinic, but not thereafter. ADT represents an effective agent for PSD treatment [9, 10, 11, 12] and is part of established stroke guidelines recommendations [14, 15]. Moreover, previous studies showed an association between more severe PSD and higher treatment rates, possibly due to easier detection and a higher need [7, 45]. Therefore, our findings indicate that with regard to severity, the mismatch between ADT and PSD might be more pronounced in later parts of the medical supply chain or clinical practice, which more likely do not have a primary focus on PSD and its consequences for stroke survivors. This result may also be interpreted as a more cautioned prescription of ADT for stroke survivors with more severe PSD during later stages. This caution may stem from a risk of polypharmacy or from the uncertainty, whether depression severity might be artificially inflated by somatic symptoms of depression (e.g., loss of appetite or insomnia) [46]. At this point, the distinction between a phenomenological and etiological perspective on PSD should be considered. From an etiological standpoint, even the same phenomenological manifestation of PSD and general depression (i.e., the manifestation of the same depression symptoms) would not necessarily imply the same causes, risk factors and corresponding treatment [47]. In fact, the degree of overlap between the etiology of PSD and general depression is part of the ongoing debate about the etiology of PSD [5, 47, 48, 49, 50]. Recent etiological models of PSD suggest a complex and time-dependent combination of biological and psychosocial factors [5, 35, 47, 50]. While substantial parts of potential etiological mechanisms remain to be deciphered [5, 47, 50], recent meta-analyses showed that the five most established risk factors for PSD (physical disability, stroke severity, cognitive impairment, history of depression and social support) show a considerable overlap to risk factors for general depression (i.e., a history of depression and social support) [2, 3]. From a more phenomenological perspective, the question if criteria for depression can be used to diagnose PSD is related to the question if stroke survivors and people without stroke show distinct symptom profiles [34, 46, 51, 52]. Different symptom profiles in these two populations would suggest that a different set of criteria to diagnose PSD or depression would be necessary. With high-quality studies relying on precise assessment methods, large samples and relevant comparison groups, the accumulating evidence suggested that PSD symptom profiles do not differ from depression in other (somatic) illnesses or depression in the general population [34, 51]. While these findings do not suggest that PSD and general depression are caused by the same factors, they partly imply that PSD can also be detected using established depression instruments, given sufficient individual cognitive and language capacities. This timely detection may in turn facilitate the reduction of undertreatment [15, 19, 50].
Our third aim was to analyze PSD and ADT from a longitudinal (i.e., intra-individual) perspective to examine the persistence of a possible mismatch in over- and undertreatment of PSD with ADT. This longitudinal assessment allows us to more closely approach the perspective and experience of an individual stroke survivor during the first year. With respect to undertreatment, we found that about 45% of stroke survivors experienced undertreatment on at least one of three measurement occasions during their first year after stroke. Moreover, undertreatment persisted in about 40% of all depressed stroke survivors during the first six months, and about 15% throughout the complete first year. Again, possible reasons may be caution of clinicians regarding the risk of polypharmacy, and/or uncertainty about the efficacy and safety of antidepressant treatment.
With respect to overtreatment, our longitudinal analyses showed that about 10% of all non-depressed stroke survivors reported to receive ADT at least once during the first year. The most likely explanation for this might be off-label use of ADT to promote other aspects of recovery (e.g., motory recovery) which has previously been suggested [25, 26], or that ADT was continued as a maintenance therapy after remission. Notably, our data collection took place from 2011 to 2016 and therefore after the 2011 published FLAME trial [25], which suggested that the SSRI fluoxetine could promote functional recovery, but before the more recent results from several large trials, which could not find evidence in support for this therapy approach [10, 11, 27]. Thus, albeit the recognition of this new evidence suggests that off-label use of ADT can be expected to decrease, it might yet have contributed to the overtreatment in our sample. At the same time, the early use of SSRI could play a role in PSD prevention, as shown in a recent meta-analysis [13]. The authors found that early SSRI therapy significantly lowers PSD incidence (prevention) but to the disadvantage of increased risk of bone fractures and nausea. This aspect might play a role in future guidelines towards more tailored ADT for certain high-risk groups of stroke survivors. Another explanation might be the continuation of ADT as maintenance therapy [53]. But even this explanation could only account for half of the cases in this group since of all non-depressed with baseline ADT, overtreatment persisted in 50% of stroke survivors after six months, and in about 20% throughout the complete first year. In other words, about one in eight stroke survivors experiences overtreatment of PSD, of which half of all these stroke survivors were without PSD at any point in time during the first six months, and one in five during the complete first year. Thus, our results also indicate considerable overtreatment in PSD, as suggested by previous research [17]. Lastly, we found similar proportions with which under- (40% and 15%) and overtreatment (50% and 20%) of PSD persisted throughout the first six and 12 months after stroke.
The following limitations of our study should be considered: Sample size was
limited compared to register- or community-based studies [19, 20, 21]. Dropout rates
from baseline to first follow-up were about 30%, and about 10% thereafter,
which is comparable to other rehabilitation based samples [3, 5]. Post-hoc, we
addressed dropout by assessing whether stroke survivors participation was
predicted by clinical, demographic or stroke-related factors, which it did not.
Secondly, during follow-up we could not assess ADT in all participating stroke
survivors, resulting in missing values for ADT. To control for potential bias, we
tested post-hoc if the availability of ADT was related to any other variables,
which was not the case. Nevertheless, the smaller number of data points might
have limited statistical power and biased the proportions between ADT and PSD for
the follow-up assessments. To address the potential limitation in statistical
power, we re-analyzed all
In summary, the present article extends previous evidence about the mismatch in treatment of PSD with ADT by using structured clinical interviews to diagnose PSD according to DSM criteria. In our sample, we found evidence for significant under- and overtreatment which persisted to a substantial extent throughout the first year. These aspects underline the known recommendations for early and routine screening for depressive symptom to reduce undertreatment [5], but also the need for repeated assessments to detect delayed onsets and reduce potential overtreatment. Moreover, we could show that the mismatch of ADT and PSD might be more pronounced after in-patient rehabilitation has ended, which calls to further assess reasons for this phenomenon in post-acute segments of stroke survivors rehabilitation. In short, our findings suggest that identification and treatment of post-stroke depression should be more precise, including targeted screening, evidence-based treatment, and application of follow-up protocols bridging the transition from inpatient to outpatient settings in clinical practice.
All authors contributed to the study’s conceptualization, design and methodology. KW, MV and SL contributed to the original draft. Data analysis was carried out by MV, data visualization by SL, final editing and reviewing by KW and MH. All authors contributed to revisions and have read and approved the final manuscript.
All participants in this study gave their informed consent for inclusion before their study participation. The study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee at the Department of Psychology of the Humboldt-University Berlin (Reg.-No 2010-13).
We would like to express our gratitude to Johanna Möbus, Christa Letsch, Anna-Lewin Richter, Inga Pontow and Yasmina Giebeler for their continuous help during data collection. We also want to thank the participating stroke survivors for allowing us to interview them during their (often difficult) rehabilitation process and our peer-reviewers for their constructive and helpful comments on this manuscript.
The Berlin PSD study was supported by the Humboldt-Universität zu Berlin structured graduate program “Self-Regulation Dynamics Across Adulthood and Old Age”. The funding had no role in planning, implementation or writing of this research or manuscript.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.jin2104108.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.