Academic Editor: Giovanni DalCorso
Traditional herbal medicine is still used for basic healthcare by a significant portion of the population in developing countries. This study aimed to explore the medicinal plant’s diversity and to document related traditional knowledge in the Safi region of Morocco. We used semi-structured questionnaires to interview 222 informants living in the study area. To perform data analysis, we used quantitative indices like use value (UV), family use value (FUV), fidelity level (FL), the relative popularity level (RPL), rank of order priority (ROP), and informant consensus factor (ICF). We reported the ethnomedicinal uses of 144 medicinal plants belonging to 64 families. According to the findings, the dominating families were Lamiaceae (17 taxa), Asteraceae (15 taxa), and Apiaceae (12 taxa). The most commonly utilized plant part (48%) was leaves. The decoction was reported as the main preparation method (42%). Highly cited plant species were Marrubium vulgare (UV = 0.56), Salvia rosmarinus Spenn. (UV = 0.47), Thymus serpyllum (UV = 0.32), and Dysphania ambrosioides (UV = 0.29). Papaveraceae (FUV = 0.26), and Urticaceae (FUV= 0.23), Geraniaceae (FUV = 0.17), Oleaceae (FUV = 0.17), Lamiaceae (FUV = 0.17) had the highest family use-values. Gastrointestinal disorders (88%), respiratory diseases (85%), and anemia (66%) have the greatest ICF values. This study reveals the indigenous people’s reliance on plant-derived traditional medicine to prevent, alleviate, and treat a broad range of health concerns. Our findings will provide a scientific basis for ethnomedicinal legacy conservation and further scientific investigations aimed at new natural bioactive molecules discovery.
Since the dawn of civilization, plants and their extracts have been used medicinally in health care. Numerous shreds of evidence indicate that herbal medicines are the oldest and most widely used kind of therapy [1]. Despite the spectacular development of conventional medicine, phytotherapy is still the cornerstone of the traditional therapeutic arsenal in different populations worldwide [2, 3]. According to the World Health Organization (WHO), around 80% of the world’s population relies on traditional medicine, primarily of plant origin, to address their basic health care needs [4]. The widespread usage of traditional medicinal plants can be attributable to their efficacy, a lack of contemporary medical options, the high cost of biomedical services, a lengthy distance to public health centers, cultural beliefs, or a combination of all these reasons [5, 6, 7]. Based on medicinal plant uses in the indigenous systems of medicine, ethnobotanical research has been innovative in drug research and development [6]. Unfortunately, this traditional knowledge is getting lost from generation to generation [8, 9, 10]. To overcome the loss of this expertise and conserve and use these biological resources, the documentation of this knowledge is becoming increasingly important [11].
Because of its strategic geographical position, climatic circumstances, and geomorphological traits, Morocco has been dubbed one of the countries with the most floristic biodiversity in the North Africa region. In Morocco, over 4200 taxa, which represent 981 genera and 155 families, have been recognized, with 22% of them being endemic [12]. Furthermore, approximately 500 species have been reported to be in use as medicinal plants [13]. Together with its high biodiversity, Morocco has a long and rich tradition and expertise in the use of medicinal plants. Phytotherapy is well-rooted in the local culture. This traditional knowledge was acquired from classical Arab medicine, which was subsequently expanded and extended by many ethnic groups that arrived in the region, including Andalusians and European Jews [14, 15]. In recent decades, medicinal plants have gained increasing interest among Moroccan scientists. Since the pioneering studies of Bellakhder et al., [14, 16, 17] on Moroccan traditional pharmacopeia, several ethnopharmacological surveys emphasizing various components of health concerns (diabetes, hypertension, cancer, respiratory disorders, renal disease), or just recording the medicinal plants utilized by local inhabitants have been completed all around the country [18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36]. However, many geographical areas of this country were not concerned by these studies. Using quantitative indices (UV, FUV, FL, RPL, ROP, and ICF), the present study sought to provide the first ethnobotanical investigation of the traditional use of medicinal plants among local communities of Safi province (west-center of Morocco).
In our study, the majority of the respondents (97%) were from rural areas. Traditional medicine has a strong following in rural areas because of its remoteness from official health centers. Our findings support previous research that found that the rural community utilized and knew more about medicinal herbs than the urban group [37]. A similar trend was also observed in previous ethnomedicinal studies in Morocco [24, 26, 31].
Concerning sex, both women and men use traditional medicine. However, this use is more common among women (70% vs. 30% for men). This finding supports the view that women are the principal holders of medicinal plant knowledge. In Morocco, very few studies dealing with gender differences in the ethnobotanical knowledge of medicinal plants exist [38, 39]. As is the case for many cultural domains, healing is heavily gendered in Morocco [22, 40, 41] and depends mainly on gendered social roles and experiences [40, 42]. Women are more knowledgeable about the uses of medicinal plants due to the role they play in the process of drying, storing, and preparing recipes for the care of family members at the household level [15]. Therefore, some medicinal plants known only by housewives have been documented in Moroccan rural contexts [43].
Concerning the age of the participants in the survey, 74% of the interviewers were between 30 and 60 years old. Older people (those over the age of 65) account for 24% of the population. Young people (between 20 and 30 years old) represent only 2% of the interviewers. These proportions are indicative of generational differences in knowledge about medicinal plants. Our results indicate that knowledge of medicinal plants is mainly passed orally (80%) (Table 1). Previous studies conducted in Morocco and other Mediterranean countries have reported similar findings with an average age of people practicing traditional phytotherapy often exceeds 50 years [6, 21, 24, 31]. Nevertheless, the vertical transmission of this knowledge between generations is now diminishing. Young people seem to have a weak belief in traditional medicine. It may result from changing lifestyles through modernization and urbanization or the development of modern medicine [9, 10, 37].
| Percentage | ||
|---|---|---|
| Residence | Rural | 97% |
| Urban | 3% | |
| Age range | [20–30] | 2% |
| [30–40] | 13% | |
| [40–50] | 28% | |
| [50–60] | 33% | |
| 24% | ||
| Gender | Women | 70% |
| Men | 30% | |
| Women’s age range | [20–30] | 3% |
| [30–40] | 14% | |
| [40–50] | 28% | |
| [60–50] | 32% | |
| 23% | ||
| Men’s age range | [20–30] | 2% |
| [30–40] | 9% | |
| [40–50] | 26% | |
| [50–60] | 27% | |
| 36% | ||
| Educational level | Illiterate | 75% |
| Koranic school | 8% | |
| Primary | 11% | |
| Secondary | 3% | |
| University | 3% | |
| Access to modern medicine | Yes | 97% |
| No | 3% | |
| Use of modern medicine | Yes | 76% |
| No | 24% | |
| Preference of traditional or modern medicine | Traditional | 57% |
| Modern | 15% | |
| No preference | 28% | |
| Source of traditional Medicinal Knowledge | Inherited | 80% |
| Sociocultural contact | 14% | |
| Personal experience | 4% | |
| Media | 2% | |
Regarding the educational background, 75% of the interviewers were illiterate. The remaining 25% of the informants were divided between primary schooling (11%), informal schooling (8%), and secondary schooling (3%), while 3% of the interviewers had graduate levels. Our results report that illiterate people seem to be more accustomed to using medicinal plants, whereas educated people have very little interest in learning and practicing ethnobotanical knowledge. Other studies in Morocco [24, 27, 29] and abroad have reported a similar tendency [44, 45, 46, 47].
Table 2 displays the results of the field documentation, which are organized alphabetically by botanical name, family, and pertinent information. Our research revealed knowledge of 144 helpful plants from 64 families. In terms of identified taxa, the Lamiaceae (17 taxa), Asteraceae (15 taxa), Apiaceae (12 taxa), Fabaceae (8 taxa), Poaceae (6 species), Solanaceae (6 taxa), and Cucurbitaceae (5 taxa) were the most dominating families (Fig. 1). Understanding how people choose plants for therapeutic purposes has long been a focus of ethnobotany. Studies suggesting non-random selection of medicinal plants are becoming more common. Asteraceae, Lamiaceae, and Apiaceae are the most abundant families in Moroccan flora (Asteraceae 500 taxa, Lamiaceae 210 taxa, and Apiaceae 160 taxa) [48]. Shrubby plants are overrepresented in the herbal inventory, which is probably related to their accessibility to the year, compared to annual or biennial taxa that disappear during the summer months. This might justify, at least in part, why some families’ species have become so widely used in medicine as they’re more easily obtainable or abundant locally [49, 50, 51]. Our findings are consistent with earlier ethnobotanical investigations that have found similar relevance to these families [26, 29, 35, 39, 52, 53]. Similarly, investigations conducted in other Mediterranean nations revealed a similar result [46, 54, 55, 56, 57]. Aside from ecological availability, the physicochemical properties and organoleptic characteristics of Lamiaceae, Asteraceae, and Apiaceae, which drive their activity, may explain their predominance in the local ethnobotanical inventory [58, 59, 60, 61, 62, 63].
| Family | Taxa | Vernacular names | Status (place of origin) | Folk uses | UR | Parts used | Mode of preparation | UV | FUV |
| Aizoaceae | Carpobrotus edulis (L.) N.E.Br. | Balsamo | Introduced (South Africa) | Skin infection, skin burn and eczema. | 05 | Leaves, stem | Poultice, powder | 0.0225 | 0.0252 |
| Alliaceae | Allium porrum L. | Korita | Native | Digestive troubles, diarrhea, colds | 08 | Leaves, Roots | Poultice, powder, decoction | 0.0360 | 0.0360 |
| Amaranthaceae | Chenopodiastrum murale (L.) S.Fuentes, Uotila | ||||||||
| Borsch | Talkouta | Native | Fatigue, weakness, pale or yellowish skin eczema | 03 | Root, leaves, seeds | Poultice, decoction, maceration | 0.0135 | 0.1531 | |
| Dysphania ambrosioides (L.) Mosyakin | |||||||||
| Clemants | Mkhinza | Introduced (America) | Colds, antitussive, asthma, headache, respiratory infections, carminative, fever, oral infections, anxiety, digestive diseases | 65 | Leaves, Whole plant, seeds | Poultice, decoction, maceration, infusion | 0.2928 | ||
| Anacardiaceae | Pistacia brevifolia Gand. | Meska lhorra | Native | Kidney stones, renal pains, digestive problems | 02 | Infusion, decoction | 0.0090 | 0.0090 | |
| Apiaceae | Ammi majus L. | Tlilan | Native | Cough, influenza, colds, skin disease, skin burn | 06 | Leaves, seeds | Poultice, decoction, powder | 0.0270 | 0.0638 |
| Ammodaucus leucotrichus Coss. | Camoun Essofi | Native | Diarrhea, digestive troubles, reproductive system, stomach ache, anxiety | 12 | Leaves, seeds | Decoction, infusion, powder | 0.0541 | ||
| Apium graveolens L. | Krafas | Native | Urinary disorders, kidney stones, aphrodisiac | 04 | Leaves, roots | Decoction, Maceration | 0.0180 | ||
| Apium nodiflorum (L.) Lag. | Ziyata | Native | Digestive problems | 01 | Leaves, roots | Decoction, Powder | 0.0045 | ||
| Carum carvi L. | Karwya | Introduced (Eurasia) | Sedative, bronchitis, colds, stomach ache, diabetes | 12 | Seeds | Infusion, decoction | 0.0541 | ||
| Coriandrum sativum L. | Kosbar | Native | Diabetes, intestinal pains, stomach ache, cancer | 10 | Leaves, stems, seeds | Decoction, Powder | 0.0450 | ||
| Eryngium campestre L. | Nougir | Native | Intestinal pains, digestive troubles | 05 | Leaves, seeds, fruits | Infusion, Maceration | 0.0225 | ||
| Ferula communis L. | Klakh | Native | Antispasmodic, aphrodisiac, magic | 24 | Flowers, leaves | Decoction, Infusion | 0.1081 | ||
| Foeniculum vulgare Mill. | Naffaa | Native | Respiratory disease, oral hygiene | 28 | Flowers, fruits, leaves | Infusion, decoction, Powder | 0.1261 | ||
| Petroselinum crispum subsp. crispum. | Maadnos | Native | Digestive pains, renal disorders, aphrodisiac, hypertension | 30 | Roots, leaves | Decoction, Maceration | 0.1351 | ||
| Pimpinella anisum S.G.Gmel. | Habat Hlawa | Introduced (Turkey to Caucasus) | Aphrodisiac, menstrual pains, asthma, diabetes | 03 | Seeds | Decoction | 0.0135 | ||
| Ridolfia segetum (L.) Moris | Tabch | Native | Jaundice, weakness | 35 | Seeds | Powder | 0.1577 | ||
| Apocynaceae | Apteranthes europaea (Guss.) Murb. | Daghmous | Native | Urine retention, diabetes | 15 | Stem | juice | 0.0675 | 0.0540 |
| Nerium oleander L. | Defla | Native | Oral infection, headache, abortive, diabetes, eczema | 09 | Leaves | Infusion, poultice | 0.0405 | ||
| Araceae | Arisarum simorrhinum Durieu | Yerni | Native | Skin diseases, skin burn | 04 | Roots | Poultice | 0.0180 | 0.0180 |
| Araliaceae | Hedera helix L. | Lwaya | Native | Weakness, wound-healing | 02 | Leaves | Decoction, poultice | 0.0090 | 0.0090 |
| Arecaceae | Chamaerops humilis L. | Doum | Native | Digestive problems, diabetes | 01 | Leaves | Infusion | 0.0045 | 0.0068 |
| Phoenix dactylifera L. | Nkhal | Native | Diabetes, hypertension, digestive problems, skin diseases | 02 | Leaves, seeds, fruits | Decoction | 0.0090 | ||
| Aristolochiaceae | Aristolochia baetica L. | Bereztam | Native | Eczema, skin diseases, skin burn, digestive problems, intestinal infections | 34 | Roots | Decoction | 0.1532 | 0.1532 |
| Asparagaceae | Drimia maritima (L.) Stearn | Elbassila | Introduced (Europe) | Cancer | 21 | Roots, seeds, fruits | Poultice, Powder | 0.0946 | 0.0946 |
| Asphodelaceae | Aloe succotrina Weston | Ssabra | Introduced (South Africa) | Skin infections, skin burn | 06 | Leaves, Roots | Poultice, decoction, infusion | 0.0270 | 0.0855 |
| Asphodelus fistulosus subsp. fistulosus | Barwag | Native | Digestive problems, infections, cold, eczema | 32 | leaves | Raw, decoction, poultice | 0.1441 | ||
| Asteraceae | Anacyclus pyrethrum (L.) Lag. | Taqndiche | Native | Analgesic, skin inflammation, digestive and intestinal disorders | 02 | Leaves, roots | Decoction, Powder | 0.00901 | 0.0135 |
| Artemisia absinthium L. | Chiba | Native | Abdominal pains, skin problems, swelling, edema, loss of hair | 43 | Aerial parts, Flowers | Decoction, Infusion | 0.1937 | ||
| Artemisia herba-alba Asso | Chih | Native | Diabetes, skin problems, intestinal pains, swelling | 25 | Aerial parts, flowers | Decoction, Infusion | 0.11261 | ||
| Artemisia mesatlantica Maire | Chih EL-Khrayssi | Endemic | Abdominal pains, digestive problems, aerophagia, diarrhea, skin diseases, eczema, infection, wound healing | 12 | Aerial parts, seeds, | Infusion, Decoction, fumigation (Bkhour) | 0.0541 | ||
| Calendula officinalis L. | Jamra | Native | Anemia, weakness, jaundice, bad breath | 07 | Aerial parts, | Infusion, decoction | 0.0500 | ||
| Centaurea maroccana Ball | Nougir | Native | Appetite, digestion, anemia, weakness | 03 | Leaves, Stems | Decoction, powder, Infusion | 0.01351 | ||
| Chamaeleon gummifer (L.) Cass. | choûk el-eulk | Native | Headache, purgative, cosmetic, abortive, skin burn, aerophagia; bloating, , liver disease, antispasmodic | 10 | Aerial parts, roots | Decoction, maceration, powder | 0.0450 | ||
| Cynara cardunculus L. | khorchaf | Native | Stomach ache, vomiting, heartburn, diarrhea, cosmetic | 07 | Leaves, bulb | Decoction, maceration | 0.0315 | ||
| Daucus carota L. | Khyzo | Native | Asthma, appetite stimulant, weakness, anemia, rheumatism | 01 | Seed | Powder | 0.0045 | ||
| Echinops glaberrimus DC. | Taskra | Introduced (Egypt, Palestine, Saudi Arabia) | Diuretic, diabetes, stomach ache, Eczema, skin burn, skin infection | 48 | Roots, seeds | Decoction, poultice | 0.2162 | ||
| Lepidium sativum L. | Habarchad | Introduced (Europe to Central Asia) | Respiratory infections, constipation, urine retention, cough | 06 | Seeds | Decoction, powder, infusion | 0.0270 | ||
| Leuzea acaulis (L.) Holub | Tafgha | Native | Renal pains, Stomach ache | 19 | Roots, fruits leaves | Decoction, infusion, poultice | 0.0856 | ||
| Matricaria chamomilla L. | Babounj | Native | Hypertension, diabetes, wound healing, labor pains, cosmetic | 35 | Aerial parts, flowers | Decoction, infusion, poultice | 0.1577 | ||
| Scolymus hispanicus L. | Garnina | Native | Asthma, digestive troubles, diabetes | 16 | Roots, stems, leaves | Decoction, infusion, Powder | 0.0721 | ||
| Silybum marianum (L.) Gaertn. | Choka Hmar | Native | Bacterial infection, dysentery, tuberculosis, typhoid, antitoxic, food poisoning | 02 | Fruits | Decoction, maceration, infusion | 0.0090 | ||
| Brassicaceae | Brassica nigra (L.) W.D.J.Koch | Bu Hammo | Native | Aphrodisiac, asthma, influenza, cold, wound healing, constipation | 02 | Fruits | Poultice, decoction, Infusion | 0.0090 | 0.0495 |
| Brassica rapa L. | Left Baldi | Native | Constipation, digestive troubles, intestinal pains | 06 | Stems | Decoction, infusion, maceration | 0.0270 | ||
| Diplotaxis pitardiana Maire | El-kerkaz | Native | Skin disease, eczema, cough | 33 | Aerial parts | Poultice infusion | 0.1486 | ||
| Raphanus raphanistrum subsp. sativus (L.) Domin | Fjel | Native | Diabetes, abdominal pains | 03 | Roots, aerial parts | Raw | 0.0135 | ||
| Cactaceae | Opuntia ficus-indica (L.) Mill. | Hendiya | Introduced (Mexico) | Diarrhea, skin diseases, stomach ache, kidney disorders | 21 | Aerial parts, fruits, leaves | Decoction, infusion, powder | 0.0946 | 0.0946 |
| Camelliaceae | Camellia sinensis (L.) Kuntze | Atay | Introduced (China) | Digestive problems, intestinal pains | 03 | Leaves | Decoction | 0.0135 | 0.0090 |
| Cannabaceae | Cannabis sativa L. | Lkif | Introduced (Central Asia, Pakistan) | Anxiety, sedative, stomach ache, narcotic | 02 | Leaves, flowers | Powder, inhalation | 0.0090 | 0.0090 |
| Capparaceae | Capparis spinosa L. | Kebbar | Native | Appetite stimulant, diabetes, aphrodisiac | 25 | Seeds | Decoction, infusion | 0.1126 | 0.1126 |
| Caryophyllaceae | Corrigiola telephiifolia Pourr. | Sarghina | Native | Lung problems, cosmetic, stomach ache, digestive disorders, diarrhea | 10 | Root | Decoction | 0.0450 | 0.0615 |
| Herniaria glabra L. | Harras Hjar | Native | Urinary and kidney diseases | 28 | Leaves | Decoction | 0.1261 | ||
| Saponaria officinalis L. | Tighcht | Introduced (Europe) | Skin diseases, eczema, parasitic skin, wound healing | 3 | Leaves | Poultice | 0.0135 | ||
| Cucurbitaceae | Citrullus colocynthis (L.) Schrad. | Hdej | Native | Laxative, purgative, cancer, bronchitis, anti-inflammatory. | 44 | Root, seeds | Decoction, fumigation, maceration | 0.1982 | 0.0477 |
| Citrullus lanatus (Thunb.) Matsum. | |||||||||
| Naka | Dalaa | Introduced (Africa) | Constipation, digestive problems | 02 | Whole plant | Raw | 0.0090 | ||
| Cucumis sativus L. | Khyar | Introduced (Asia) | Renal diseases, abdominal pain, diabetes | 02 | Root | Raw | 0.0090 | ||
| Cucurbita pepo L. | Garaa Hamra | Introduced (Mexico) | Laxative, renal disorders | 2 | Fruit | Decoction, maceration | 0.0090 | ||
| Cucurbita moschata Duchesne | Slawi | Introduced (Mexico, Guatemala) | Cosmetic, skincare, | 3 | Leaves, fruit | Poultice | 0.0135 | ||
| Cupressaceae | Cupressus sempervirens L. | srou | Introduced (Europe, Iran) | Wound healing, cosmetic | 01 | Leaves | Poultice | 0.0045 | 0.0736 |
| Platycladus orientalis (L.) Franco | Araar | Introduced (Asia) | Abdominal pain, respiratory diseases, bronchitis, cold, influenza | 11 | Leaves | Infusion, fumigation | 0.0495 | ||
| Tetraclinis articulata (Vahl) Mast. | Araar | Native | Digestive pains, anti-infection, diarrhea | 02 | Leaves | Decoction | 0.0090 | ||
| Cyperaceae | Cyperus maculatus Boeckeler | Tara | Introduced (Africa) | Cosmetic, skin diseases, eczema | 02 | Leaves | Poultice | 0.0090 | 0.0090 |
| Ephedraceae | Ephedra nebrodensis Tineo | Abo | Native | Haircare, diabetes | 03 | Leaves | Decoction, maceration | 0.0135 | 0.0135 |
| Euphorbiaceae | Euphorbia tirucalli L. | Heliliba | Introduced (Ethiopia, South Africa, India) | Uro-genital infections | 05 | Leaves | Poultice | 0.0225 | 0.0736 |
| Mercurialis annua L. | Horriga EL Malssa | Native | Wound healing, skin infections, abdominal pain | 40 | Leaves | Decoction, poultice | 0.1802 | ||
| Ricinus communis L. | Kharwaa | Introduced (Africa) | Cosmetic, diabetes, skin problems, abdominal pains | 04 | Leaves, seeds | Oil, poultice, decoction | 0.0180 | ||
| Fabaceae | Ceratonia siliqua L. | Kharob | Native | Diarrhea, intestinal worms, skin diseases | 39 | Leaves, seeds | Decoction, raw, infusion. | 0.1757 | 0.0794 |
| Glycine max (L.) Merr. | Soja | Introduced (Russia, China) | Laxative, digestive disorders, cosmetic, skin diseases | 02 | Seeds | Decoction, oil | 0.0090 | ||
| Glycyrrhiza glabra L. | Aarq Soss | Introduced (Europe, Asia) | Cough, renal problems, constipation, digestive problems, weakness, fatigue | 04 | Roots, stem | Powder, infusion, oil | 0.0180 | ||
| Lupinus angustifolius L. | Rjel Djaja | Native | Diabetes, intestinal pains | 05 | Leaves, stem | Powder, decoction | 0.0225 | ||
| Retama raetam (Forssk.) Webb | |||||||||
| Berthel. | Retam | Native | Diabetes, renal diseases, cancer | 39 | Leaves, stem | Decoction, maceration | 0.1757 | ||
| Trigonella foenum-graecum L. | Halba | Introduced (Iraq, Pakistan) | Appetite stimulant, digestive problems, anemia, weakness | 42 | Seeds | Powder, decoction | 0.1892 | ||
| Vicia faba L. | Fol | Introduced (Asia) | Renal diseases, bronchitis, weakness, digestive problems | 06 | Seeds, leaves | Powder, maceration, raw | 0.0270 | ||
| Vicia lens (L.) Coss. | |||||||||
| Germ. | Adass | Native | Jaundice, weakness, fatigue, anemia, digestive problems | 04 | Seeds | Decoction, powder | 0.0180 | ||
| Geraniaceae | Pelargonium graveolens L’Hér. | Aatarcha | Introduced (South Africa, Zimbabwe) | Anxiety, digestive problems | 38 | Leaves | Infusion, decoction | 0.1712 | 0.1712 |
| Iridaceae | Crocus sativus L. | Zaafrane | Introduced (Greece) | Intestinal parasites, skin diseases, anemia | 03 | Roots, flowers | Infusion | 0.0135 | 0.0135 |
| Juncaceae | Juncus acutus L. | Smar | Native | Renal stones, skin infections, abdominal pains | 04 | Leaves | Decoction | 0.0180 | 0.0113 |
| Juncus maritimus Lam | Smar | Introduced (Europe, Central Asia) | Cold, influenza, anxiety | 01 | Leaves | Decoction, infusion | 0.0045 | ||
| Lamiaceae | Ajuga iva (L.) Schreb. | Chandgora | Native | Diabetes, hypertension, digestive problems, respiratory disorders | 42 | Leaves | Decoction | 0.1892 | 0.1692 |
| Lavandula angustifolia subsp. angustifolia | Khzama | Introduced (Europe) | Bronchitis, respiratory problems, influenza, colds, repellent, cosmetic | 45 | Aerial parts | Decoction, infusion, oil | 0.2072 | ||
| Lavandula bipinnata (Roth) Kuntze | Kohila | Introduced (Bangladesh, India) | Digestives and respiratory problems, delivery difficulties | 35 | Aerial parts | decoction | 0.1577 | ||
| Lavandula stoechas L. | Halhal | Native | Digestive problems, diabetes | 04 | Leaves | Infusion, decoction | 0.0180 | ||
| Marrubium deserti (de Noé) Coss. | Jaada | Native | Respiratory problems, cosmetic, skin diseases | 03 | Aerial parts, roots | Poultice, decoction | 0.0135 | ||
| Marrubium vulgare L. | Marriout | Native | Haircare, jaundice, anemia, fatigue, weakness, diabetes, hypertension | 126 | Aerial parts | Decoction | 0.5676 | ||
| Mentha × piperita L. | Naanaa Aabdi | Introduced (Artificial hybrid) | Abdominal pain, heartburn, bloating, laxative | 03 | Aerial parts | Infusion, maceration, raw | 0.01351 | ||
| Mentha pulegium L. | Flayyo | Native | Bronchitis, cough, bad breath, chest pain, intestinal pains | 35 | Aerial parts | Decoction | 0.1577 | ||
| Mentha suaveolens Ehrh. | Timija | Native | Digestive disorders, abdominal pains, respiratory difficulties | 08 | Aerial parts | Decoction, Infusion | 0.0360 | ||
| Ocimum basilicum L. | Lahbeq | Introduced (Asia) | Respiratory diseases, bronchitis, sinusitis, hemorrhoids | 25 | Leaves | Decoction, infusion | 0.1126 | ||
| Origanum majorana L. | Mardadoch | Introduced (Turkey, Cyprus) | Caner, digestive disorders, abdominal pains, diabetes, skin diseases | 07 | Leaves | Decoction, poultice | 0.0315 | ||
| Saccocalyx satureioides Coss. | |||||||||
| Durieu | Zaitra | Native | Respiratory problems, diabetes, hypertension | 20 | Leaves, aerial parts | Decoction, poultice | 0.0901 | ||
| Salvia officinalis L. | Salmia | Introduced (Europe) | Intestinal antiseptic, diabetes, digestives problems | 54 | Leaves, aerial parts | Decoction, infusion | 0.2432 | ||
| Salvia rosmarinus Spenn. | Azir | Native | Intestinal parasites, intestinal pains, diarrhea, anxiety, wound healing | 105 | Leaves, aerial parts | Decoction, infusion, poultice | 0.4730 | ||
| Salvia verbenaca L. | Khwiwita | Native | Skin infections, wound healing | 17 | Aerial parts | Decoction, poultice | 0.0767 | ||
| Thymus serpyllum L. | Zaatar | Introduced (Europe to Siberia) | Bronchitis, allergy, skin diseases, intestinal pains, intestinal worms | 72 | Leaves, aerial parts | Decoction, poultice | 0.3243 | ||
| Lauraceae | Persea americana Mill. | Avocat | Introduced (Guatemala, Honduras, Mexico, Nicaragua) | Aphrodisiac, anemia, jaundice, weakness, fatigue, respiratory problems | 01 | Fruits | Raw | 0.0045 | 0.0045 |
| Liliaceae | Allium cepa L. | Basla | Introduced (Central Asia) | Infections, cough, asthma, digestive troubles | 25 | Bulb, rhizome | Raw, powder | 0.1126 | 0.1014 |
| Allium sativum L. | Toma | Introduced (Iran, Kazakhstan, Uzbekistan) | Antiseptic, intestinal parasites, cold, influenza | 20 | Bulb, rhizome | Raw, powder | 0.0901 | ||
| Linaceae | linum usitatissimum L. | Zariaat Elkattan | Introduced (Turkey, Iran) | Urinary problems, cough, skin infections, eczema | 04 | Seeds | Powder, infusion, decoction | 0.0180 | 0.0180 |
| Lythraceae | lawsonia inermis L. | Lhana | Introduced (Africa, Arabian Peninsula, Pakistan, India) | Haircare, skin diseases, eczema, vomiting | 10 | leaves | Decoction, poultice | 0.0450 | 0.0450 |
| Malvaceae | Althaea officinalis L. | Bakola/Khobiza | Native | Digestive problems, abdominal pains, diarrhea | 14 | Leaves | Decoction, infusion | 0.0631 | 0.06306 |
| Moraceae | Ficus carica L. | Kerma | Introduced (E. Medit. Asia, Afghanistan) | Laxative, digestive problems, diabetes, constipation | 13 | Fruits, leaves | Raw, decoction, infusion | 0.0586 | 0.0586 |
| Myristicaceae | Myristica fragrans Houtt. | Goza | Introduced (Banda Islands) | Skin diseases, digestive problems, abdominal pains, constipation, tooth care, painful gum | 02 | Nutmeg bark, leaves, | Decoction, infusion, raw | 0.0090 | 0.0090 |
| Myrtaceae | Eucalyptus globulus Labill. | Kalitus | Introduced (Australia) | Diabetes, respiratory diseases, asthma, bad breath, digestive problems, influenza | 61 | Leaves | Decoction, inhalation | 0.2748 | 0.1599 |
| Syzygium aromaticum (L.) Merr. | |||||||||
| L.M.Perry | Qrenfal | Introduced (Maluku) | Tooth care, painful gum, intestinal pains, digestive problems | 10 | Fruits | Decoction, infusion, raw | 0.0450 | ||
| Nitrariaceae | Peganum harmala L. | Harmal | Native | Jaundice, anemia, weakness, digestive problems, cold, nervous problems, magic | 13 | Seeds, whole plant, root | Decoction, infusion, fumigation | 0.0586 | 0.0585 |
| Oleaceae | Olea europaea L. | Zeitoun | Native | Cosmetic, mouth hygiene, digestive problems, skin diseases, cold, influenza | 38 | Fruits, leaves | Oil, decoction, infusion, | 0.1712 | 0.1711 |
| Papaveraceae | Papaver rhoeas L. | Belaaman | Native | Sedative, bronchitis, insomnia, respiratory disorders, intestinal pains | 58 | Leaves, seeds | Decoction, infusion | 0.2613 | 0.2613 |
| Pedaliaceae | Sesamum indicum L. | Jaljlane | Introduced (Bangladesh, India) | Stress, bad breath, bronchitis, sinusitis, chest pain, sedative | 02 | seeds | Decoction, infusion, powder | 0.0090 | 0.0090 |
| Pinaceae | Pinus halepensis Mill. | Tayda | Native | Digestive problems, cold, respiratory diseases | 07 | Leaves, roots | Poultice, decoction, powder | 0.0315 | 0.0315 |
| Plantaginaceae | Plantago major L. | Msasa | Native | Cancer, skin diseases | 08 | Leaves, whole plant | Poultice, powder | 0.0360 | 0.0360 |
| Poaceae | Cynodon dactylon (L.) Pers. | Njem | Native | Renal disease, diuretic | 05 | Stem, roots | Decoction, powder | 0.0225 | 0.0210 |
| Hordeum vulgare L. | Chaair | Introduced (Palestine) | Digestive problems, jaundice, anemia, weakness | 06 | Aerial parts, Seeds | Powder, maceration | 0.0270 | ||
| Panicum miliaceum L. | Illan | Introduced (India) | Skin diseases, digestive problems | 03 | Seeds | Powder, infusion | 0.0135 | ||
| Phragmites australis (Cav.) Trin. ex Steud. | Qsab | Native | Skin diseases, cosmetic | 03 | Root, stem | Decoction, poultice | 0.0135 | ||
| Triticum sp | Qamh | Introduced (Central Asia, India, Ethiopia) | Anemia, jaundice, digestive problems | 01 | Seeds | Powder | 0.0045 | ||
| Zea mays L. | Dra | Introduced (Mexico, Guatemala) | Anemia, weakness, digestive problems | 10 | Seeds | Raw, powder | 0.0450 | ||
| Polygonaceae | Rumex acetosa L. | Homayda | Native | Influenza, bronchitis, chest pain, bad breath, abdominal pains | 05 | Leaves, whole plant, roots | Powder, maceration, decoction | 0.0225 | 0.0225 |
| Portulacaceae | Portulaca oleracea L. | Rejla | Native | Anemia, weakness, jaundice, diabetes | 08 | Leaves, whole plants, | Decoction, infusion | 0.0360 | 0.0360 |
| Punicaceae | Punica granatum L. | Romman | Introduced (Turkey to Pakistan) | Digestive problems, stomach ache, stomach ulcer, skincare | 10 | Fruit barks | Decoction, maceration | 0.0450 | 0.0450 |
| Ranunculaceae | Ranunculus arvensis L. | Ouden Halouf | Native | Chest pain, painful breath, insomnia | 03 | Leaves | Decoction | 0.0135 | 0.0135 |
| Rhamnaceae | Ziziphus oenopolia (L.) Mill. | Nbeg | Introduced (China, Tropical Asia) | Diabetes, respiratory disorders, hair care | 11 | Flowers, leaves, roots | Decoction, infusion, raw | 0.0495 | 0.0495 |
| Rosaceae | Prunus amygdalus Batsch | Louz | Introduced (Transcaucasus) | Skin problems, headaches | 01 | Fruits | Raw, oil, decoction | 0.0045 | 0.0203 |
| Rosa x centifolia L. | Lward | Introduced ((Artificial hybrid) | Laxative, intestinal pains, skin care, hair care | 08 | Flowers | Decoction, maceration, oil | 0.0360 | ||
| Rubiaceae | Rubia tinctorum L. | Fowa | Introduced (Europe, Himalaya, Vietnam) | Digestive problems, constipation | 25 | Roots | Decoction | 0.1126 | 0.1126 |
| Rutaceae | Citrus × aurantium L. | Limon | Introduced (Artificial hybrid) | Anemia, weakness, fatigue | 05 | Fruits | Juice | 0.0225 | 0.0450 |
| Citrus × limon (L.) Osbeck | Lhamad Baldi | Introduced (Artificial hybrid) | Diarrhea, digestive problems, oral hygiene, cold, bronchitis | 05 | Fruits | Juice | 0.0225 | ||
| Ruta montana (L.) L. | Fijel, ourmi | Native | Skin diseases, vitiligo, sterility, vermifuge | 20 | Leaves | Decoction | 0.0901 | ||
| Salicaceae | Populus nigra L. | Safssaf | Native | Digestive problems, respiratory disorders, skin diseases | 01 | Leaves | Decoction, powder, | 0.0045 | 0.0045 |
| Sapotaceae | Sideroxylon spinosum L. | Argane | Native | Hear care, skin infection, diabetes, aphrodisiac, eczema | 02 | Fruits, seeds, | Poultice, decoction, infusion | 0.0090 | 0.0090 |
| Schisandraceae | Illicium verum Hook.f. | Najma sinia | Introduced (China, Vietnam) | Digestive and respiratory problems, constipation, laxative, asthma | 09 | Leaves, fruits | Infusion | 0.0405 | 0.0405 |
| Solanaceae | Capsicum frutescens L. | Flfla Hamra | Introduced (Bolivia, Brazil) | Digestive problems, intestinal parasites, abdominal pains, tonifying, appetite stimulant, anemia, diabetes | 01 | Fruits | Raw, decoction, chewing | 0.0045 | 0.0188 |
| Hyoscyamus albus L. | Sikran | Native | Tooth care, painful gum | 11 | Seeds | Decoction, infusion | 0.0495 | ||
| Mandragora autumnalis Bertol. | Bayd Ghol | Native | Narcotic, sedative, cancer, respiratory problems | 07 | Aerial parts, seeds | Maceration, decoction | 0.0315 | ||
| Nicotiana glauca Graham | Taba | Introduced (Bolivia, Brazil) | Sedative, digestive problems, intestinal parasites, | 04 | Leaves | powder | 0.0180 | ||
| Solanum lycopersicum var. esculentum (Mill.) Voss | Maticha | Introduced (Peru) | Skincare, cosmetic | 01 | Fruits | Maceration | 0.0045 | ||
| Solanum nigrum L. | Ain dib | Native | Sedative, antiseptic, antispasmodic, intestinal pains | 01 | Leaves | decoction | 0.0045 | ||
| Thymelaeaceae | Thymelaea hirsuta (L.) Endl. | Almatnane | Native | Bad breath, tooth care, diabetes, constipation | 02 | Leaves, seeds | Decoction, infusion | 0.0090 | 0.0090 |
| Urticaceae | Urtica dioica L. | Horriga Harcha | Native | Renal problems, urinary system disorders, diabetes, skincare | 51 | Leaves, aerial parts | Maceration, infusion, poultice | 0.2297 | 0.2297 |
| Vitaceae | Vitis vinifera L. | Laanab | Introduced (Europe, Asia) | Jaundice, anemia, weakness, headache | 01 | Leaves, fruits | Decoction, maceration | 0.0045 | 0.0045 |
| Verbenaceae | Aloysia citrodora Paláu | Lwiza | Introduced (Bolivia, Argentina) | Sedative, digestive problems, intestinal pains, anxiety | 46 | leaves | Decoction, infusion | 0.2027 | 0.1171 |
| Vitex agnus-castus L. | Sadrat Maryam | Native | Digestive problems, skincare | 06 | Leaves | Poultice, decoction | 0.0270 | ||
| Zingiberaceae | Curcuma longa L. | Lark sfar | Introduced (E. Medit. to Iran) | Anemia, jaundice, weakness, fatigue | 02 | Stem, roots | Powder | 0.0090 | 0.0105 |
| Elettaria cardamomum (L.) Maton | Bsibissa | Introduced (India) | Digestive problems, sterility | 02 | Seeds | Decoction, powder | 0.0090 | ||
| Zingiber officinale Roscoe | Sekkin jbir | Introduced (India, China) | Respiratory diseases, influenza, cough, diabetes | 03 | Seeds | Powder, decoction | 0.0135 |
 Fig. 1.
Fig. 1.Species frequency of major plant families used in the Safi Province (Morocco).
In terms of plant status, the local population of Safi employs at least 78 native taxa (54%) and 66 introduced taxa (46%) as medicine. The exotic plants reported here were originally introduced as food and food spices (28 taxa, 42%), ornamental (4 taxa, 6%), or cosmetic (3 taxa, 5%). One plant (Trigonella foenum-graecum) was likely introduced specifically as medicines. The probable reason for the introduction of 45% of exotic plants remains unknown (Table 3). The inefficiency of native species may lead people to experiment and adopt introduced species in local traditional pharmacopeia [64]. Most of the introduced plants are native to Asia (52%), Europe (18%), America (15%), and Africa (15%).
| Probable reason for introduction (% of total exotic plants) | Taxa |
|---|---|
| Food (31%) | Opuntia ficus-indica, Camellia sinensis, Citrullus lanatus, Cucumis sativus, Cucurbita pepo, Cucurbita moschata, Glycine max, Persea americana, Allium cepa, Allium sativum, Ficus carica, Hordeum vulgare, Triticum sp, Zea mays , Punica granatum, Prunus amygdalus, Capsicum frutescens, Solanum lycopersicum var. esculentum, Urtica dioica, Vitis vinifera, Aloysia citrodora . |
| Food spices (11%) | Carum carvi, Pimpinella anisum, Crocus sativus, linum usitatissimum, Sesamum indicum, Elettaria cardamomum, Zingiber officinale. |
| Ornamental (6%) | Aloe succotrina, Ocimum basilicum, Rosa x centifolia, Carpobrotus edulis. |
| Cosmetic (5%) | Glycyrrhiza glabra, Lawsonia inermis, Syzygium aromaticum. |
| Medicinal (2%) | Trigonella foenum-graecum. |
The data compiled during the field studies were analyzed by calculating the use-value (UV) which determines the relative importance of species having more use reports indicated by local informants. During this investigation, 2257 uses were reported. The highest use values were observed by the following species: Marrubium vulgare (UV = 0.57), Salvia rosmarinus (UV = 0.47), Thymus serpyllum (UV = 0.32), Dysphania ambrosioides (UV = 0.29), Eucalyptus globulus (UV = 0.27), Papaver rhoeas (UV = 0.26), Salvia officinalis (UV = 0.24), Urtica dioica (UV = 0.23), Echinops glaberrimus (UV = 0.22), Lavandula angustifolia subsp. angustifolia and Aloysia citrodora (UV = 0.20) (Fig. 2). Species with the highest UV values may have powerful curative properties that can be useful to manage and alleviate a variety of ailments categories. Previous studies from different regions of Morocco have reported the same sort of finding [27, 29, 31]. These species are also prominent in traditional medicine practices in the Mediterranean region [6, 65].
 Fig. 2.
Fig. 2.Use values of the most used medicinal plants in the Safi Province (Morocco).
It is also important to note that for the abovementioned medicinal plants, many other folk uses have been reported in different regions of Morocco. Furthermore, literature-based proof revealed that these species have proven a wide variety of biological and pharmacological activities (Table 4, Ref. [14, 17, 19, 20, 21, 23, 24, 26, 28, 30, 31, 34, 35, 36, 38, 39, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116]), which may confirm the different popular applications of extracts obtained from these plants in traditional medicine.
| Other folk uses in Morocco | Evidence-based pharmacological properties | |
| Marrubium vulgare | Diabetes, hypertension, hair care, fever, jaundice, diarrhea, intestinal pains, cough, colds, respiratory problems, ear pains, menstrual pains [14, 20, 21, 26, 31, 36, 39, 116] | Antioxidant acitivities [65], hepatoprotective effect [66], antidiabetic effect [67, 68, 69], antihypertensive activities [70, 71], hypolipidemic effect [70], gastroprotective effect [72], antibacterial effect [73]. No reports on toxicity. |
| Salvia rosmarinus | Allergy, diabetes, hypertension, intestinal parasites, rheumatism, kidney diseases, sedative, wounds healing [19, 20, 23, 28, 35, 116] | Antidiabetic effect [74], anti-inflammatory, antinociceptive activities [75], antioxidant effect [76]. No reports on toxicity. |
| Thymus serpyllum | Stimulant, aid to menstruation, digestive stimulant, against headache, cardiac stimulant [14, 19] | Antioxidant activities [77], antimicrobial effect [78], antitumor and cytotoxic activities [79]. No reports on toxicity. |
| Dysphania ambrosioides | Hypertension, cold, antitussive, emmenagogue, diabetes, menstrual pains, asthma, analgesic, headache, respiratory infections, fever, oral infections, anxiety [17, 20, 21, 35, 114]. | Antibacterial effect [80], anticancer effect [81], antidiabetic activity [82], antidiarrheal effect [83], anti-inflammatory and anti-nociceptive activities [84], antioxidant activity [85], anti-ulcer effect [86], immunomodulatory effect [87]. Decoctions and infusions of this plant may have a genotoxic effect [88]. |
| Eucalyptus globulus | Diabetes [20], renal colic [34], influenza [28, 35], stomach pain [31], typhoid [19]. | Antidiabetic activities [89, 90], anti-inflammatory effect [91], cytotoxic activities [92], hypotensive action [93]. No reports on toxicity |
| Papaver rhoeas | Diabetes, cosmetic, sedative, sterility, menstrual pains, cough, bronchitis, insomnia, analgesic, allergy Kidney stones, kidney inflammation [17, 19, 21, 34, 38, 114]. | Cytotoxic and antiproliferative activities [94], antiulcerogenic effect [95], antimicrobial effect [96]. May be toxic [97]. |
| Salvia officinalis | Diabetes, hemostatic, respiratory problems, hypertension, intestinal antiseptic, kidney stones, diuretic, renal colic [17, 19, 21, 30, 34, 35, 38, 114]. | Gastroprotective action [98], antioxidant effect [99], anti-diabetic effects [100], antinociceptive and anti-inflammatory activities [101], hepatoprotective action [102], hypolipidemic effect [103]. No reports on toxicity |
| Urtica dioica | Diabetes, hypertension, renal diseases, digestive problems, rheumatism, diarrhea, allergy [21, 24, 34, 35, 114]. | Diuretic [104], hypotensive [105], antidiabetic [106], anti-inflammatory [107], immunomodulatory [108], analgesic [109], hepatorenal protective [110]. No reports on toxicity |
| Echinops glaberrimus | diuretic, hypoglycemiant, stomachic, liver disorders, post-partum care [17, 19], kidney stones [34]. | Anti-inflammatory [111], renal inflammation [112], antibacterial [113]. No reports on toxicity |
| Aloysia citrodora | Digestive problems, hypertension, diabetes, headache, colds [31, 114], diuretic [34, 35]. | Cytotoxic and antibacterial [114], sedative and cardiovascular effects [115]. No reports on toxicity |
FUV indicates the most biologically significant plant family. In the present research, the use-values of families were calculated and are presented in Table 2. The highest FUV was reported for the families Papaveraceae (FUV = 0.26), Urticaceae (FUV = 0.23), Geraniaceae (FUV = 0.17), Oleaceae (FUV = 0.17), Lamiaceae (FUV = 0.17), Myrtaceae (FUV = 0.16), Amaranthaceae (FUV = 0.15), Aristolochiaceae (FUV = 0.15), Asphodelaceae (FUV = 0.14), Verbenaceae (FUV = 0.12), Capparaceae and Rubiaceae (FUV = 0.11) (Fig. 3). Our study indicates that the most important families (Papaveraceae, Urticaceae, Geraniaceae) are monotypic and are represented by only one species in the study area. High values of FUV might be because the plant species are cited by a large number of people in the study area. While the Lamiaceae family was represented by the highest number of plant species (16 taxa).
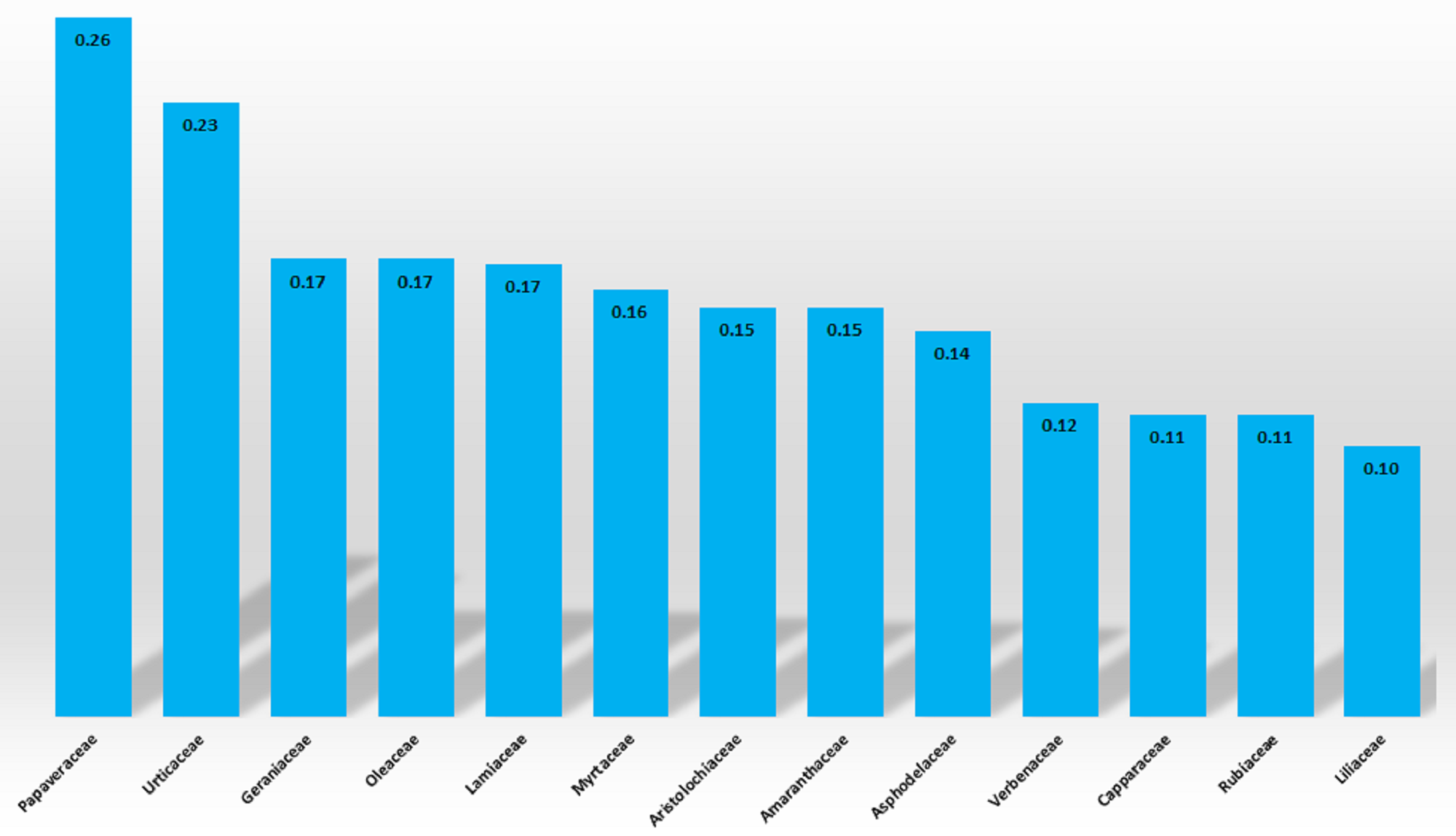 Fig. 3.
Fig. 3.Family use values of medicinal plants used in the Safi Province (Morocco).
In the current investigation, we report the use of different plants’ parts for medical purposes by the local population (Figs. 4,5). Leaves are the part most used (48%), followed by stems (16%), flowers and inflorescence (12%), underground parts (the roots) (11%), and the whole plant (7%). The leaves are easily accessible, which can explain their high use in the medicinal recipe’s preparation. The potential leaves’ curative effectiveness may be due to the higher concentration of bioactive compounds. This finding agrees with most medicinal plant studies in Morocco [29, 23, 24, 28, 31] and neighboring countries [2, 47, 117, 118, 119].
 Fig. 4.
Fig. 4.Used parts of medicinal plants.
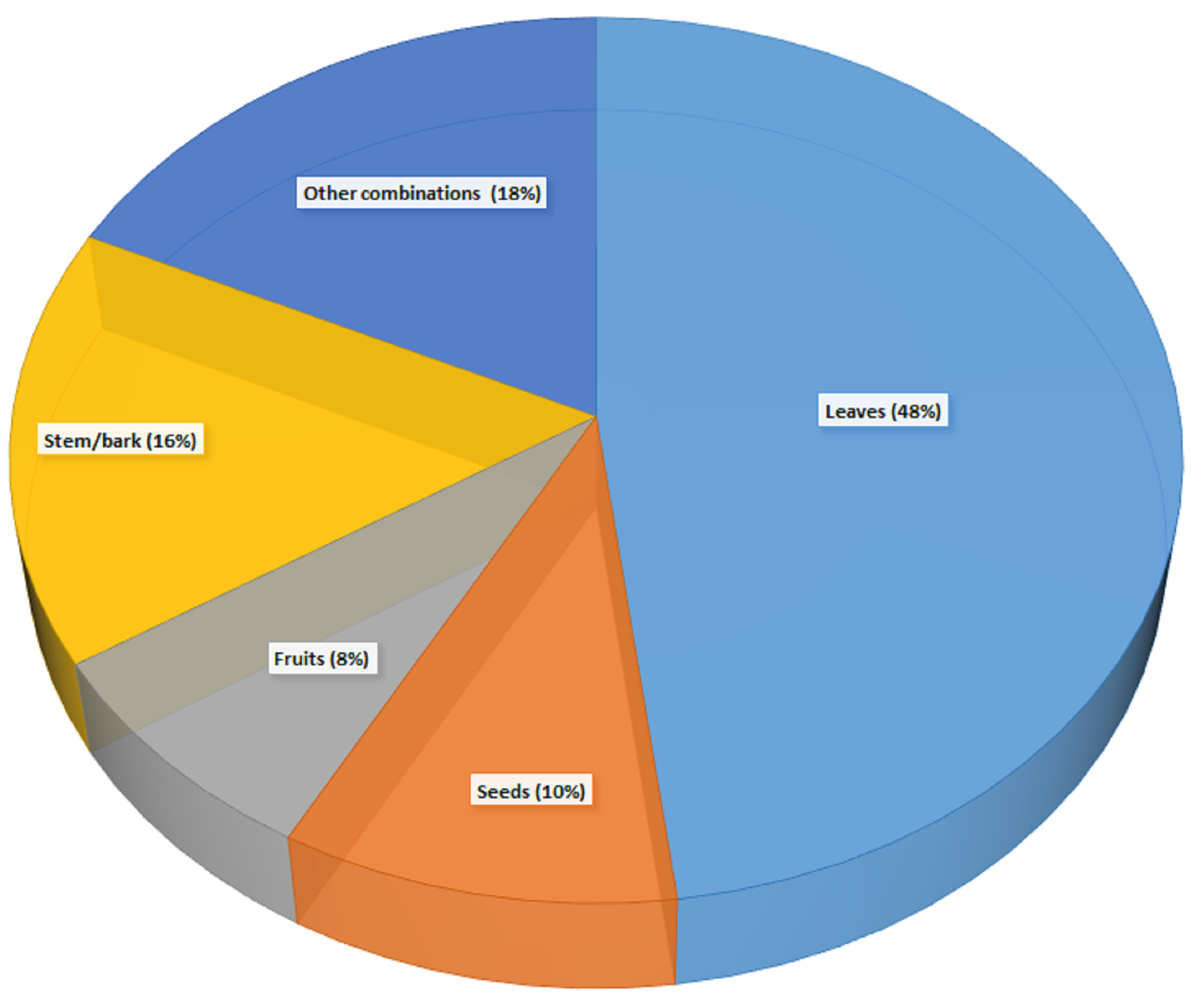 Fig. 5.
Fig. 5.Used aerial parts of medicinal plants.
The preparation of recipes from medicinal plants is represented by many methods, such as infusion, decoction, inhalation, and powder. Fig. 6 summarizes the methods of preparation found in this study. The decoction was the most widely used method in the study area for herbal preparation, with a percentage contribution of 42%, followed by infusion, powder, and poultice, which were used in 20%, 18%, and 17% of the preparations, respectively. The remaining 3% was used as inhalation, or “bkhour” (Fig. 6). The higher frequency of decoction use might be related to the simple preparation method. Similarly, the same sort of conclusions has been observed in previous studies [29, 31, 47, 117, 118, 119].
 Fig. 6.
Fig. 6.Mode of the utilization of medicinal plants.
Fidelity level determines the relative plant’s healing potential. High FL values indicate that a plant is mainly used to treat a single therapeutic category and low FL values show that plants are used for a wide range of diseases. FL is artificially high for plants with few use reports, thus species with less than five use reports were excluded from the discussion. Only 10 plants show high fidelity values to certain diseases category. We report M. vulgare, S. rosmarinus Spenn., T. serpyllum, D. ambrosioides, E. globulus, P. rhoeas, S. officinalis, U. dioica, E. glaberrimus, and A. citriodora as the most important species (Table 4). Concerning gastrointestinal disorders, S. rosmarinus, T. serpyllum, A. citriodora, and S. officinalis have the highest FL values (89%, 77%, 53%, and 50%, respectively). E. globulus is popular in the traditional treatment of respiratory disease (FL = 61%) and M. vulgare for cancer treatment (FL = 44%) (Table 5). Plants with recurrent uses are more likely to be pharmacologically active [120]. Validation of this ethnomedicinal knowledge through in-depth phytochemical and pharmacological studies could be innovative in novel drug research and development approaches.
| Taxa | Frequent disease category | Fidelity level (FL) % | Relative popular level (RPL) % | Ranking order priority (ROP) % |
|---|---|---|---|---|
| Marrubium vulgare | Respiratory diseases | 47% | 100% | 47% |
| Cancer | 44% | 100% | 44% | |
| Salvia rosmarinus | Gastrointestinal disorders | 89% | 83% | 74% |
| Thymus serpyllum | Gastrointestinal disorders | 77% | 57% | 44% |
| Respiratory diseases | 30% | 57% | 17% | |
| Dysphania ambrosioides | Respiratory diseases | 49% | 52% | 25% |
| Eucalyptus globulus | Respiratory diseases | 61% | 48% | 29% |
| Papaver rhoeas | Respiratory diseases | 40% | 46% | 18% |
| Dermatological diseases | 28% | 46% | 13% | |
| Salvia officinalis | Gastrointestinal disorders | 50% | 43% | 21% |
| Urtica dioica | Respiratory diseases | 20% | 40% | 8% |
| Gastrointestinal disorders | 18% | 40% | 7% | |
| Dermatological diseases | 14% | 40% | 6% | |
| Echinops glaberrimus | Gastrointestinal disorders | 21% | 38% | 8% |
| Aloysia citrodora | Gastrointestinal disorders | 53% | 36% | 19% |
The distribution of species knowledge concerning the richness of the resources referenced in the examined use category was determined using Rank Order Priority (ROP). As our study showed, the highest ROP values were observed for S. rosmarinus (ROP = 74%), M. vulgare (ROP = 47%), and T. serpyllum (ROP = 44%), indicating that these species are the most well known in the Safi region. While, U. dioica (ROP = 8%), and E. glaberrimus (ROP = 8%) had a lower priority and were considered unpopular among medicinal plants used by the local population.
The ICF measures the agreement between informants and plants used for each disease. Based on the plants’ use reports, we classified the reported ailments into five disease categories (Table 6). Gastrointestinal disorders, respiratory diseases, and anemia have the highest ICF values (85%, 82%, and 66%, respectively), suggesting that these ailments were prevalent in the study area.
| Ailments category | Nur | Nut | ICF% |
| Respiratory diseases | 391 | 61 | 85% |
| Dermatological diseases | 169 | 52 | 70% |
| Gastrointestinal disorders | 670 | 83 | 88% |
| Cancer | 124 | 25 | 80% |
| Anemia | 75 | 26 | 66% |
| ICF, Informant Consensus Factor; Nur, number of use reports for a particular ailment category; Nut, number of taxa used for an ailment category by all informants. | |||
The prevalence of gastrointestinal disorders may be due to more common and easily identifiable clinical signs. Among other factors, poor hygienic conditions such as consumption of contaminated food or low drinking water quality may exacerbate digestive troubles in the study area. In the case of respiratory diseases, air quality is a significant risk factor in the development and exacerbation of the disease. Long-term exposure to high levels of pollution, particularly in childhood, raises the risk of developing respiratory disorders [121]. Because the region is home to a large and highly polluting chemical and para-chemical industry, the high ICF recorded for this disease category may explain, at least in part, the high ICF. Anemia received the third-highest ICF value (66%). The majority of cases of anemia are caused by malnutrition or a lack of proper nutrition, which results in iron and other micronutrient deficiencies. In the 2014 Moroccan census, the Safi area had a poverty rate of 10–15% [122]. This fact can explain, at least in part, the prevalence of anemia in this region. Several studies conducted in other areas in Morocco [22, 29, 53, 123], Algeria [47, 54, 124], Pakistan [125], and the Mediterranean region [6] show a similar high prevalence of ICF value for digestive and respiratory diseases.
The present study was conducted in five different coastal localities: Ayyer, El
Beddouza, Had Hrara, Khat Azakan, and Safi City in the Safi Province (Morocco)
(Fig. 7). The study area is administratively part of the Marrakech-Safi Region.
It is located in the Western Central Plain of Morocco and lies about
32
 Fig. 7.
Fig. 7.Localization of the study area.
In the 2014 Moroccan census, the Safi area had a population of about 691.983 people [122]. Amazigh and Arab descent constitute the majority of the local population.
Between March 2019 and March 2020, ethnobotanical surveys were conducted to compile knowledge of plants used in the area. A total of 222 informants of various ages were chosen at random for interviews. The International Society of Ethnobiology (ISE) code of ethics (https://www.ethnobiology.net/ethics.php) was strictly followed, and the purpose of the study was explained to the participants before conducting the interviews, and verbal informed consent was obtained from them.
Semi-structured interviews were used to collect ethnobotanical data [126], and the stratified sample (5 stratums) sampling technique was used [29]. The questionnaires have two sections. The first one included personal information from participants, such as age, gender, educational level, location, access to modern medicine, use of conventional medicine, preference for traditional or modern medicine, and how they learned about traditional medicine. The second one included open questions to gather information about medicinal plants, such as vernacular names (dialectal, Arabic, Tamazight, or literary).
The collected information also includes emic disease classification categories (as recorded in interviews) and an etic disease classification category into pathological groups, followed by the WHO’s international disease classification (International Classification of Primary Care (ICPC)) [127].
The above questionnaires complied with the guidelines for conducting and reporting ethnopharmacological field studies and an ethnopharmacological survey [126, 128].
During fieldwork, identification was mainly based on the local names of plants. For taxonomic confirmation, we used standard botanical references for Moroccan flora:
Food, aromatic, condiment, medicinal, and toxic plants in Morocco [129].
Statistics and comments on the current inventory of vascular flora in Morocco [130].
Elements for a red book of the vascular flora of Morocco [131].
We also used the online database https://powo.science.kew.org, the African plant database (http://www.ville-ge.ch/musin/bd/cjb/africa/recherche.php), and the International Plant Name Index (IPNI) (http://www.ipni.org/) for checking the scientific names and synonyms of plants. Voucher specimens of each identified plant have been deposited in the herbarium of our laboratory (Environment and Health Research Team, Polydisciplinary Faculty of Safi).
In the last few decades, the scientific precision of ethnobotanical research has increased substantially. One significant part of ethnobotany is the quantitative evaluation of indigenous knowledge of plants to produce meaningful yet intangible data. In ethnobotany, quantitative indices provide the data, enabling hypothesis testing, statistical verification, and comparative analysis [132]. Ethnobotanical information was examined in this study using Use Value (UV), Family Use Value (FUV), Fidelity Level (FL), Relative Popularity Level (RPL), Ranking Order Priority (ROP), and Informant Consensus Factor (ICF).
The UV, first described by Prance et al. [133], represents the relative importance of a species reported locally by taking into account the number of usage reports given by people in the research region. This quantitative index has been frequently used in ethnobotany to determine the species that are most important to specific people. The formula described below was used to calculate it:
To describe the most important plant families in the study area, Family Use Value (FUV) was calculated from the use-values of the species using the following formula [134].
Where UV is the use-values of the species belonging to the family, and N is the total number of species within each family.
Fidelity levels identify the main use of each plant and calculate the use report’s relative importance for each category of use. The FL was calculated using the following formula based on Friedman et al. [135].
Where Np: is the number of use reports for a use category and N is the total number of informants citing the species for the treatment of any use.
RPL is the ratio between the number of ailments treated by a particular plant species and the total number of informants for any disease [129, 130].
ROP is a correction factor derived from FL by multiplying RPL and FL values as explained earlier [131, 132].
FL is the Fidelity Level and RPL is the Relative Popularity Level.
Informant Consensus Factor highlights plants of particular cultural relevance and assesses the agreement among informants on the plant species used against a disease category as originally proposed by Trotter and Logan [136] and simplified by Heinrich et al. [137]. To use this tool, illnesses were classified [127]. ICF is based on the correlation between an informant’s knowledge and is calculated using the following formula:
Nur is the total number of the use reports in each use category and Nut is the total number of species used in that category.
ICF values lie between “0.00 and 1.00”. A value near 1 indicates that there is a homogeneity of information among informants, while low ICF values indicate that informants do not agree on which plant to use.
An in-depth literature search concerning the most cited plants’ biological activities reported in this study was made using the following confident electronic databases: PubMed, Science Direct, Google Scholar, Scopus, and Web of Science. We have used the following keywords: ”ethnobotanical uses”, ”hypertension”, ”diabetes”, ”renal disease”, “biological activity” in association with the plant’s scientific name.
Traditional knowledge about medicinal plants has received increasing academic attention. Our study mainly contributed to highlighting, on the one hand, the place of traditional herbal medicine in the study area and, on the other hand, the diversity of plants used in the preparation of medicinal remedies. Thus, it constitutes the first scientific study aimed at listing and documenting traditional therapeutic knowledge in this semi-arid region of Morocco. The results obtained justify the importance of the use of medicinal plants along the coastline of the Safi region. In addition, this study allowed us to assess the know-how and the importance of traditional practices used by the population of the study area. This natural (specific floristic richness) and human (accumulation of experiences) potential are likely to bring added value by developing the activities of women’s cooperatives and herbalists. Thus, offering a source of income, in particular, in semi-urban areas and rural areas. This traditional heritage is essentially passed down orally from generation to generation. The collection and analysis of ethnobotanical data would make it possible for the conservation of the biocultural heritage of this region by creating a database of medicinal plants used and their therapeutic uses. However, the use of medicinal plants for treatment is not always without risk. The indigenous knowledge regarding the toxicity of plants is modest. The misuse of some plants could be fatal. To raise awareness among the local population, an inventory of poisonous plants and their study is essential.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The design of the study was carried out by ALe, HA, AD, and BL. NL and ALa were the main data collectors and analyzers. The manuscript was prepared and edited by Ale, AB, AK. MAS, TB, CH, JML and JTC revised the manuscript. Lastly, the final manuscript was read and confirmed by all authors.
Not applicable.
The authors gratefully acknowledge the local people of Safi Province for sharing their traditional knowledge.
This research received no external funding.
The authors declare no conflict of interest. JTC is serving as one of the Guest editors of this journal. We declare that JTC had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to GD.
