1 Institute of Clinical Medicine, College of Medicine, National Cheng Kung University, 70101 Tainan, Taiwan
2 Division of Cardiology, Department of Internal Medicine, Chi Mei Medical Center, 71004 Tainan, Taiwan
3 School of Medicine, College of Medicine, National Sun Yat-sen University, 80424 Kaohsiung, Taiwan
Abstract
Background: Angiotensin receptor neprilysin inhibitor (ARNI)
and sodium-glucose cotransporter 2 inhibitor (SGLT2i) are emerging medical
treatments for decompensated heart failure (HF) with reduced ejection fraction.
In clinical practice, the combination of ARNI and SGLT2i cannot be administered
owing to the poor hemodynamic status in patients with HF with reduced ejection
fraction (HFrEF). This study aimed to compare different strategies of HF
management for ARNI first or SGLT2i first in such a population. Methods:
From January 2016 to December 2021, 165 patients were diagnosed with HFrEF and
New York Heart Association functional class
Keywords
- heart failure with reduced ejection fraction
- angiotensin receptor neprilysin inhibitor
- sacubitril/valsartan
- sodium-glucose cotransporter 2 inhibitors
- decongestion
- early combination
The prevalence of heart failure (HF) in East Asian countries ranges from 1.3 to
6.7% and increases due to an aging society [1]. Angiotensin-converting enzyme
inhibitors (ACEIs)/angiotensin-receptor blockers (ARBs),
Accordingly, we conducted a retrospective study to compare the sequencing effects of ARNI and SGLT2i on the clinical outcomes over a 12-month follow-up period in patients with symptomatic HFrEF.
Between January 2016 and December 2021, the HF registry of Chi Mei Medical
Center enrolled 165 patients who had symptomatic HFrEF and New York Heart
Association (NYHA) functional class
Echocardiographic parameters, including left ventricular ejection fraction (LVEF), left atrial dimension (LAD), and left ventricular end-systolic and end-diastolic volume (LVESV and LVEDV), were measured using GE Vivid 9 (GE Healthcare Chicago, IL, USA), or Philips IE33, or Philips EPIQ 7 (Philips Healthcare, Amsterdam, Netherlands). LVEF, LAD, LVESV, and LVEDV were quantified using the M mode and corrected using the two-dimensional guided biplane Simpson’s method of disc measurements by using echocardiography. Echocardiographic examination was recommended every 3–6 months for patients with HFrEF thereafter in the absence of clinical events and the onset of HF.
Symptomatic HFrEF was defined as left ventricular ejection fraction
The study endpoints were hospitalization for HF, CV mortality, and all-cause mortality during one-year follow-up period.
Data were presented as the mean
In the ARNI-first group, the mean age was 60
| Variable | Group 1 | Group 2 | p value | ||
| ARNI first | SGLT2i first | ||||
| Number | 95 | 70 | |||
| The duration of adding another medication (Sacubitril/valsartan or SGLT2i) (Days) | 74 (49−100) | 112 (86−138) | 0.044 | ||
| Combination with one month | 57 (60.0) | 23 (32.9) | |||
| General demographics | |||||
| Age (years) | 60 |
60 |
0.992 | ||
| Male sex (%) | 71 (74.7) | 47 (67.1) | 0.300 | ||
| Hemodynamic condition | |||||
| SBP (mmHg) | 126.2 |
126.7 |
0.894 | ||
| 15 (15.8) | 9 (12.9) | 0.660 | |||
| HR (beat/min) | 88.5 |
89.0 |
0.860 | ||
| Etiology of HF | 0.700 | ||||
| Ischemic cardiomyopathy (%) | 90 (94.7) | 68 (97.1) | |||
| Non-ischemic cardiomyopathy (%) | 5 (5.3) | 2 (2.9) | |||
| Comorbidities | |||||
| Diabetes mellitus (%) | 82 (86.3) | 63 (90.0) | 0.630 | ||
| Hypertension (%) | 70 (73.7) | 48 (68.6) | 0.490 | ||
| Atrial fibrillation (%) | 9 (9.5) | 7 (10.0) | 0.910 | ||
| PAOD (%) | 0 (0) | 1 (1.4) | 0.424 | ||
| COPD (%) | 5 (5.3) | 3 (4.3) | 0.773 | ||
| CKD, stage |
13 (13.7) | 7 (10.0) | 0.630 | ||
| Valvular heart disease (%) | 20 (21.1) | 8 (11.4) | 0.142 | ||
| ICD (%) | 7 (7.4) | 3 (4.3) | 0.520 | ||
| CRT (%) | 5 (5.3) | 2 (2.9) | 0.700 | ||
| Laboratory data | |||||
| Creatinine (mg/dL) | 1.22 |
1.17 |
0.586 | ||
| eGFR (mL/min/1.73 m |
68.15 |
67.76 |
0.924 | ||
| NT-proBNP (pg/mL) | 3132 (2270−4289) | 3530 (1510−5452) | 0.997 | ||
| Medication | |||||
| Mean dose of ARNI (mg) | 199.5 |
147.5 |
0.005 | ||
| 60 (63.2) | 37 (52.9) | 0.203 | |||
| SGLT2i | 0.319 | ||||
| Empagliflozin (%) | 46 (48.4) | 36 (51.4) | |||
| Dapagliflozin (%) | 46 (48.4) | 34 (48.6) | |||
| Canagliflozin (%) | 3 (3.2) | 0 (0) | |||
| 88 (92.6) | 68 (97.1) | 0.304 | |||
| Ivabradine (%) | 57 (60.0) | 40 (57.1) | 0.750 | ||
| Spironolactone (%) | 82 (86.3) | 55 (78.6) | 0.212 | ||
| Data are expressed as mean Abbreviation: ARNI, angiotensin receptor neprilysin inhibitor; SGLT2i, sodium-glucose cotransporter 2 inhibitors; SBP, systolic blood pressure; HR, heart rate; HF, heart failure; PAOD, peripheral arterial occlusive disease; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease; ICD, implantable cardioverter-defibrillator; CRT, cardiac resynchronization therapy; eGFR, estimated glomerular filtration rate; NT-proBNP, N-terminal pro-B-type natriuretic peptide. | |||||
The baseline and follow-up left ventricular performances are listed in Table 2.
At the baseline phase, the mean LVEF, LAD, LVESV, LVEDV, E/A, mitral E/E’,
lateral E/E’, and RV S’ did not differ between the two groups. A numerically
higher prevalence of mitral regurgitation
| Variable | Group 1 | Group 2 | p value | |
| ARNI first | SGLT2i first | |||
| Number | 95 | 70 | ||
| Left ventricular performance (Baseline) | ||||
| Mean LVEF (%) | 34.37 |
35.73 |
0.481 | |
| Mean LAD (cm) | 4.4 |
4.3 |
0.534 | |
| Mean LVEDV (mL) | 190.05 |
180.66 |
0.376 | |
| Mean LVESV (mL) | 127.41 |
117.01 |
0.226 | |
| AR grade |
3 (3.2) | 1 (1.4) | 0.638 | |
| MR grade |
16 (16.8) | 5 (7.1) | 0.097 | |
| TR grade |
10 (10.5) | 3 (4.3) | 0.241 | |
| TRPG (mmHg) | 34.5 |
28.2 |
0.077 | |
| E/A | 1.61 |
1.79 |
0.473 | |
| Mitral E/E’ | 20.15 |
18.82 |
0.439 | |
| Lateral E/E’ | 13.65 |
12.91 |
0.530 | |
| RV S’ | 10.15 |
10.36 |
0.731 | |
| Left ventricular performance (Follow-up) | ||||
| Mean LVEF (%) | 47.91 |
50.89 |
0.618 | |
| Improving EF |
51 (63.7) | 41 (63.1) | 0.933 | |
| Mean LAD (cm) | 4.1 |
4.1 |
0.688 | |
| Mean LVEDV (mL) | 176.53 |
161.11 |
0.134 | |
| Mean LVESV (mL) | 97.36 |
89.50 |
0.406 | |
| AR grade |
4 (4.2) | 0 (0) | 0.138 | |
| MR grade |
7 (7.4) | 2 (2.9) | 0.304 | |
| TR grade |
3 (3.2) | 1 (1.4) | 0.638 | |
| TRPG (mmHg) | 27.44 |
23.41 |
0.412 | |
| E/A | 0.94 |
1.17 |
0.186 | |
| Mitral E/E’ | 14.73 |
14.13 |
0.702 | |
| Lateral E/E’ | 11.82 |
10.75 |
0.458 | |
| RV S’ | 11.27 |
11.38 |
0.868 | |
| The change of LVEF (%) | 10.90 (5.26 to 19.04) | 11.85 (5.46 to 16.19) | 0.358 | |
| Improving EF |
55 (71.4) | 44 (68.8) | 0.853 | |
| The change of LAD (cm) | –0.3 (–0.6 to –0.1) | –0.2 (–0.5 to 0.1) | 0.461 | |
| The change of LVEDV (mL) | –12.00 (–22.00 to 4.57) | –11.47 (–35.00 to 5.97) | 0.723 | |
| Decreasing LVEDV |
35 (45.5) | 28 (44.4) | 0.905 | |
| The change of LVESV (mL) | –25.20 (–46.48 to –1.89) | –25.90 (–35.50 to –10.95) | 0.943 | |
| Decreasing LVESV |
43 (55.8) | 42 (66.7) | 0.225 | |
| Data are expressed as mean Abbreviation: ARNI, angiotensin receptor neprilysin inhibitor; SGLT2i, sodium-glucose cotransporter 2 inhibitors; LVEF, left ventricular ejection fraction; LAD, left atrial dimension; LVEDV, left ventricular end-diastolic volume; LVESV, left ventricular end-systolic volume; AR, aortic regurgitation; MR, mitral regurgitation; TR, tricuspid regurgitation; TRPG, tricuspid regurgitation pressure gradient; RV, right ventricle. | ||||
The incidence of HF hospitalization, CV mortality, and all-cause mortality were higher in the ARNI-first group; however, they did not achieve a significant difference when the ARNI-first group was compared with the SGLT2i-first group (Table 3).
| Variable | Group 1 | Group 2 | p value |
|---|---|---|---|
| ARNI first | SGLT2i first | ||
| Number | 95 | 70 | |
| HF hospitalization (%) | 21 (22.1) | 11 (15.7) | 0.327 |
| CV mortality (%) | 3 (3.2) | 1 (1.4) | 0.638 |
| All-cause mortality (%) | 7 (7.4) | 3 (4.3) | 0.520 |
| Data are expressed as mean Abbreviation: ARNI, angiotensin receptor neprilysin inhibitor; SGLT2i, sodium-glucose cotransporter 2 inhibitors; HF, heart failure; CV, cardiovascular. | |||
Follow-up serum creatinine levels and estimated glomerular filtration rate (eGFR) did not differ between the two groups (Table 4). The decrease in eGFR was not significantly higher in the SGLT2i-first group. A non-significant trend of lower NT-proBNP levels was noted in the SGLT2i-first group (ARNI-first vs. SGLT2i-first; 1383 [319–2507] pg/mL vs. 570 [206–1314] pg/mL; p = 0.055). A significantly higher discontinuation rate of diuretic agents was noted in the SGLT2i-first group (ARNI-first vs. SGLT2i-first; 6.8% vs. 17.5%; p = 0.039).
| Variable | Group 1 | Group 2 | p value | ||
|---|---|---|---|---|---|
| ARNI first | SGLT2i first | ||||
| Number | 95 | 70 | |||
| Creatinine (mg/dL) | 1.22 |
1.25 |
0.748 | ||
| eGFR (mL/min/1.73 m |
66.42 |
64.10 |
0.604 | ||
| The change of eGFR | –1.63 |
–3.47 |
0.551 | ||
| NT-proBNP (pg/mL) | 1383 (319−2507) | 570 (206−1314) | 0.055 | ||
| Discontinue diuretic (%) | 6 (6.8) | 11 (17.5) | 0.039 | ||
| Data are expressed as mean Abbreviation: NT-proBNP, N-terminal pro-B-type natriuretic peptide; ARNI, angiotensin receptor neprilysin inhibitor; SGLT2i, sodium-glucose cotransporter 2 inhibitors; eGFR, estimated glomerular filtration rate. | |||||
Fig. 1A showed non-significant trend of improving EF
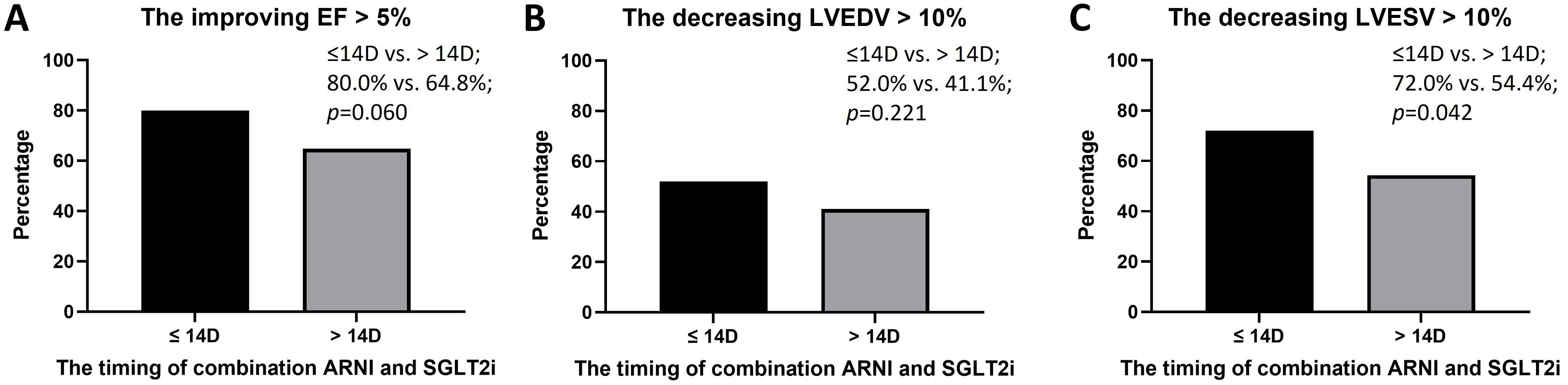 Fig. 1.
Fig. 1.The improving ejection fraction, decreasing left ventricular
end-diastolic volume, and decreasing left ventricular end-systolic volume when
early combination (
In clinical practice, the sequence of new emerging medications remains a
difficult decision for physicians, especially in patients with HFrEF and poor
hemodynamic conditions. Most patients with HFrEF also present with cardiorenal
syndrome and may not receive all four pillar-directed medical therapies at the
same time. According to the guidelines of the European Society of Cardiology, the
triad of an ACEIs/ARNI, a
In patients with HFrEF, several factors may affect renal function, including cardiac pump failure related to lower blood supply and increased congestion, chronic activation of the adrenergic system and renin-angiotensin-aldosterone system (RAAS), and direct and indirect effects of anti-HF medication [11, 12]. Approximately 30% of the patients with HF also have chronic kidney disease, and worsening renal function occurs in approximately 25% of the cases, with a deleterious effect on outcomes [13]. Additionally, renal function may also be affected by age, and comorbidities, including atherosclerosis, diabetes mellitus, hypertension, and renal dysfunction, are associated with poor outcomes [14]. Acute worsening renal function after starting RAAS inhibitors occurs in approximately 13% of the patients with HF, more so in the older hypertensive patients, following exposure to iodinated contrast, during acute illness, heart failure exacerbation, hypotension, and dehydration [15, 16, 17]. According to recent studies on SGLT2i for HF, a lower risk of kidney failure and slower progression of renal function were observed when the SGLT2i group was compared with the control group [18, 19]. In our study, no patients needed emerge hemodialysis and experienced renal death. The progression of renal function did not differ between ARNI and SGLT2i-first strategy groups. Therefore, sequential combination of ARNI and SGLT2i may be feasible for the patients with symptomatic HFrEF.
Among the patients with HFrEF, a low proportion of patients received the target
dose (or received at least 50% of the target dose), partly due to hypotension
[20]. In the PIONEER-HF study, ARNI could safely be initiated in patients with
SBP
In a retrospective study of diabetic patients with HFrEF, those with the initiation of sacubitril/valsartan presented a more prominent improvement in LV performance than those with the initiation of SGLT2i, and the combination of ARNI and SGT2i showed significant improvement in cardiac function and prognosis in this population [24]. Another real-world study also found that treatment with a combination of SGLT2i and ARNI was associated with a lower risk of composite HF hospitalization or all-cause mortality and was well tolerated [25]. The subgroups with SGLT2i presented better results than those without SGLT2i [26]. A meta-analysis concluded that SGLT2i and ARNI demonstrated similar effects (indirect comparison hazard ratio 0.93, 95% confidence interval 0.82–1.06, p-value = 0.28), while the combination of SGLT2i and ARNI resulted in a better cardiovascular protective effect [25]. In our study, the sequence of ARNI and SGLT2i did not affect reverse LV remodeling and renal function progression and did not present with acute kidney injury. The SGLT2i-first strategy may provide better decongestion. Early combination may provide better LV remodeling effect.
This study had several limitations. First, it was a retrospective, nonrandomized study with limited size, and we could not rule out selective bias. Second, the timing of adding another medication based on the judgement of physicians and a shorter interval was noted in the ARNI-first group. Third, echocardiographic examination was performed every 3–6 months for patients with HFrEF if no new events. However, we still provide important information for clinical practice regarding the sequence of ARNI and SGLT2i implementation in patients with symptomatic HFrEF.
In patients with symptomatic HFrEF, SGLT2i-first strategy may provide a higher
possibility of discontinuing diuretic agents than the ARNI-first strategy.
Changes in LV performance, progression of renal function, and clinical outcomes
did not differ between the two groups. Early combination (
The study data are available from the corresponding author upon reasonable request.
W-CL did data curation, formal analysis, investigation, and methodology. Z-CC critically reviewed the study proposal. W-TC, C-SH, C-TL, P-SH, S-CH, C-HL, C-YC, and Z-CC participated in the interpretation of data. W-CL wrote original draft. J-YS participated in writing and technical editing of final manuscript and also contributed conception as well as the design of the work. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
This retrospective study conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved for human research by the Institutional Review Committee of the Chi Mei Medical Center (Number: 11104-008).
The authors thank Chi Mei research team for data collection for this study.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

