1 Department of Psychology, University of Miami, Coral Gables, FL 33146, USA
2 Department of Medical Social Sciences, Northwestern University Feinberg School of Medicine, Chicago, IL 60611, USA
3 Department of Microbiology and Immunology, University of Miami School of Medicine, Miami, FL 33124, USA
4 Tumor Biology Program, Sylvester Comprehensive Cancer Center, Miami, FL 33136, USA
5 Cancer Control Program, Sylvester Comprehensive Cancer Center, Miami, FL 33136, USA
Academic Editor: Jordi Sastre-Serra
Abstract
Background: Overweight and obese (OW/OB) body mass index (BMI) is
associated with greater inflammation and poorer outcomes in breast cancer (BC).
Stress management interventions using cognitive behavioral therapy (CBT) and
relaxation training (RT) have reduced inflammation in BC patients but have not
been tested specifically in OW/OB patients undergoing primary treatment. We
developed brief CBT and RT-based group interventions and tested their effects (vs
time-matched Health Education [HE] control) on serum inflammatory cytokines
(IL-6, IL-1
Keywords
- breast cancer
- overweight
- obese
- inflammation
- stress management
- relaxation
- cognitive behavior therapy
Breast cancer (BC) is the most common cancer for women worldwide [1]. Notably,
obesity has been identified as a risk factor for BC and has been associated with
higher rates of obtaining a BC diagnosis and worse prognosis [2, 3]. The World
Health Organization (WHO) and the National Institute of Health (NIH) utilize body
mass index (BMI [kg/m
The relationship between obesity and BC has been attributed to chronic adipose
tissue inflammation which leads to a microenvironment favorable to cancer growth
[21, 22]. Accordingly, obesity has been consistently linked to greater
inflammation [23, 24, 25, 26, 27, 28]. High adiposity in OW/OB individuals is associated with
dysregulated metabolic pathways [23], including increased secretion of
pro-inflammatory cytokines [24, 25, 26, 27, 28, 29] and adipokines [27, 29]. This increased
inflammation related to adipose tissue dysfunction has been linked to increased
BC risk in OW/OB women [30]. Moreover, chronic inflammation and increases in
pro-inflammatory cytokines tumor necrosis factor alpha (TNF-
Despite adiposity being a theoretically modifiable factor related to
inflammation, a recent meta-analysis suggests that interventions targeting
adiposity (i.e., physical activity, caloric restriction, weight management) do
not significantly decrease inflammatory cytokines, including IL-6 and
TNF-
Stress management interventions (e.g., Cognitive-Behavioral Stress Management
[CBSM]) have reduced distress and inflammatory markers in BC patients undergoing
primary treatment [40, 41, 42]. CBSM is a 10-week group-based intervention that
combines relaxation training (RT) and cognitive behavioral therapy (CBT) [43].
Among women recruited in the weeks after surgery for non-metastatic BC, CBSM has
been shown to reduce depressive symptoms [42], anxiety and negative affect [41]
and inflammatory markers including leukocyte gene expression for IL-1
In the interest of comparing briefer forms of stress management intervention in
this population we created 5-week versions of group-based CBT and RT and compared
them with an attention-matched Health Education (HE) condition in women
undergoing primary treatment for BC. We found both CBT and RT conditions were
associated with decreases in psychological distress [46] and inflammatory markers
when compared to the HE group [47, 48]. However, these interventions have not been
tested specifically in OW/OB women with BC. Due to the potentially interacting
factors of stress and adiposity leading to increased inflammation in OW/OB women
[23, 24, 25, 26, 27, 28], these stress management interventions may be particularly beneficial in
this vulnerable population and may lead to improved health outcomes via a
reduction in inflammatory markers. Therefore, this study examined whether OW/OB
women initiating treatment for BC showed higher levels of pro-inflammatory
cytokines (IL-6, IL-1
Participants for the current analysis were women who enrolled in a prior randomized controlled trial testing two different 5-week group-based stress management interventions, CBT and RT, vs an attention-matched HE control, which took place from 2006–2014 (National Institutes of Health Clinical Trial NCT02103387). This study was approved by the Institutional Review Board at the University of Miami. Participants completed informed consent prior to completing study procedures.
Women aged 21–75 with non-metastatic BC who were between 2- and 10-weeks post-surgery were recruited from various cancer clinics in South Florida for this trial. Exclusion criteria were clinical interview-determined severe mental illness (i.e., untreated mania or psychosis) that would interfere with ability to participate in a group intervention format, initiation of adjuvant chemotherapy or radiation treatment prior to enrollment, a previous diagnosis of cancer, and lack of English fluency.
Enrolled participants completed a battery of psychosocial surveys and provided a blood sample at baseline (T1), prior to randomization to study condition. Women then participated in one of the three assigned group interventions (see 2.3). Immediately after the final group session, participants were given a follow-up questionnaire (T2; approximately 6 weeks post-T1) to test their perceived stress management skills. Six months post-randomization (T3), participants completed a third questionnaire to assess health behaviors and provided a second blood sample.
All three study conditions involved 5 consecutive, weekly 1.5 hours intervention sessions in groups of 3–7 participants. Group facilitators (total = 7) were doctoral students in clinical psychology who received training to conduct one or more of the three group interventions, and received weekly face-to-face supervision by one of the study investigators (MHA) in order to maintain the fidelity to each intervention protocol, minimize drift and prevent contamination across study conditions. In addition to weekly sessions, all participants were also given a workbook that included the information reviewed in each session. See Supplemental Material for further information regarding intervention content.
The CBT group condition was based on the cognitive-behavioral components of CBSM [43], which aims to teach adaptive coping within a cognitive-behavioral framework with emphasis on cancer-related stressors. Women in this condition were taught stress awareness, appraisal processes, cognitive restructuring, coping effectiveness, and interpersonal skills (i.e., assertiveness, anger management). Homework assignments were given for additional practice outside of group.
The RT group condition was based on the relaxation components of CBSM [43], which aimed to reduce stress and anxiety by teaching relaxation and mindfulness techniques including diaphragmatic breathing, progressive muscle relaxation, imagery, and mindful meditation. The rationale of these practices for stress management was also provided in the group format via psychoeducation. Participants were provided with audio recordings of each technique to practice at home.
HE, the attention-matched control, covered educational information relevant to BC patients including symptom management, treatments and resources available, and tips for living a healthy life post-cancer diagnosis. The content of health education material was drawn from publically available sites sponsored by the American Cancer Society (ACS) and the National Cancer Institute (NCI) [49, 50] and presented in PowerPoint slides in the weekly sessions. No information on stress management was provided in this control condition. This condition was included to control for facilitator attention and the presence of a supportive group similar to what is available through supportive care services at many cancer centers [51].
Participants self-reported height in inches and weight in pounds at T1. Given
the post-hoc nature of the current analysis, the fact that the study took place
in community practices, and the time elapsed since the conduct of the trial, BMI
data at follow-up was not obtainable. Baseline BMI was calculated by dividing
weight by height squared and multiplying by the metric conversion factor of 703
[52]. Participants were then categorized per the Center for Disease Control and
Prevention as normal weight (18.5–24.9 m/kg
At T1 and T3, non-fasted blood samples (35 mL) were obtained between 4:00–6:30
PM. by a licensed phlebotomist and serum was subsequently separated by
centrifugation. Concentration of three pro-inflammatory cytokines, IL-1
The Measure of Current Status [53] was collected at T1 (baseline) and T2
(post-intervention) to measure perceived stress management skills (PSMS). We
calculated a composite score of items on this measure capturing confidence in two
CBT and two RT skills. This composite (
Physical activity was measured with a brief version of the 7-Day Physical Activity Recall Questionnaire [54], in which patients recalled the total number of minutes of moderate and vigorous physical activity (MVPA) completed over the past 7 days. This measure has been used to capture MVPA among cancer patients [55, 56]. We measured MVPA at T1 and T3. See Supplemental Material for the questionnaire.
Covariates for study outcomes included age, stage of disease (0-III), household income, and ethnicity (Hispanic, non-Hispanic White, other). These variables were collected at baseline through self-report, with stage and age being verified with subsequent medical record review. These covariates were based on previous literature suggesting that age and disease stage are related to inflammatory markers [57], and because they have been controlled for in our past studies relating inflammation to stress processes in breast cancer patients undergoing primary treatment [47, 58, 59]. We also collected self-report data at T1 and T3 on prescription medications [antidepressants, anxiolytics (drugs relieving anxiety), pain medications, sleep medications], and adjuvant treatments received (chemotherapy/radiation) in the period leading up to T3. We also collected self-reported data at T1 on presence of medical comorbidities, including diabetes, myocardial infarction, peripheral vascular disease, and connective tissue disease.
All analyses were conducted using the Statistical Package for the Social
Sciences (SPSS) Version 27 (IBM Corp. Armonk, NY, USA) [60]. Data were initially
screened for skewness and kurtosis. Values of IL-6, IL-1
First, to justify collapsing overweight and obese BMI groupings to the OW/OB category and collapsing the two active stress management conditions (CBT/RT), we conducted two three-group analysis of variance (ANOVA) tests: (1) between CBT, RT, and HE, and (2) between NW, OW, and OB weight groupings, each predicting both T1 and T3 cytokine levels.
After we justified collapsing these categories, preliminary analyses were conducted to determine whether intervention condition or BMI predicted inflammation or variables potentially related to inflammation at T1 and T3. We compared active (CBT/RT) vs control (HE) groups separately by BMI category for baseline cytokine levels, self-reported physical activity (MVPA) levels, income, age, days from surgery to baseline assessment, and group attendance using t-tests. Chi-square tests were also used to examine differences between study conditions by BMI category on categorical variables at T1 and T3 including ethnicity (T1 only), prescription medications (antidepressants, anxiolytics, pain medications, sleep medications), chemotherapy/radiation receipt, stage of disease, ER/PR status, type of surgery (mastectomy vs lumpectomy), and receipt of reconstructive surgery.
Third, we conducted a manipulation check to determine whether women receiving CBT/RT had improved stress management skills over the course of the intervention as compared to the HE control. To test whether intervention condition affected perceived stress management skills pre- to post-intervention, and whether this differed by BMI, we tested a two condition (CBT/RT vs HE) by two group (OW/OB vs NW) by two timepoint (T1, T2) repeated measures ANOVA (RMANOVA) on the PSMS composite score, controlling for previously stated covariates. RMANOVA uses listwise deletion for missing data.
To test our primary hypothesis that baseline BMI moderated the effect of
intervention condition (CBT/RT vs HE) on inflammatory cytokines pre- to 6-months
post-randomization, we tested a two condition (CBT/RT vs HE) by two group (OW/OB
vs NW) by two timepoint (T1, T3) RMANOVA on each inflammatory cytokine (IL-6,
IL-1
Finally, to investigate one potential mechanism by which the interventions may decrease inflammation, we assessed whether the relationship between condition (CBT/RT vs HE) and the change in self-reported weekly hours of MVPA from T1 to T3 was moderated by BMI. To assess this, we tested a two condition (CBT/RT vs HE) by two group (OW/OB vs NW) by two timepoint (T1, T3) RMANOVA on MVPA weekly hours. We then tested whether the moderating effect of BMI on intervention effects on cytokine changes held after controlling for contemporaneous changes in MVPA. The two-tailed alpha level for all analyses was set at 0.05.
In total, 739 women were assessed for eligibility, of which 194 met eligibility
criteria and signed consent. Of these, 184 completed baseline procedures and were
randomized. For the present analysis, we looked at the subsample of participants
who self-reported weight and height data at baseline (N = 153; 83.2%). Women who
declined to provide height and weight data did not differ from those who did on
baseline levels of IL-6 (t(175) = –0.68, p = 0.498),
IL-1
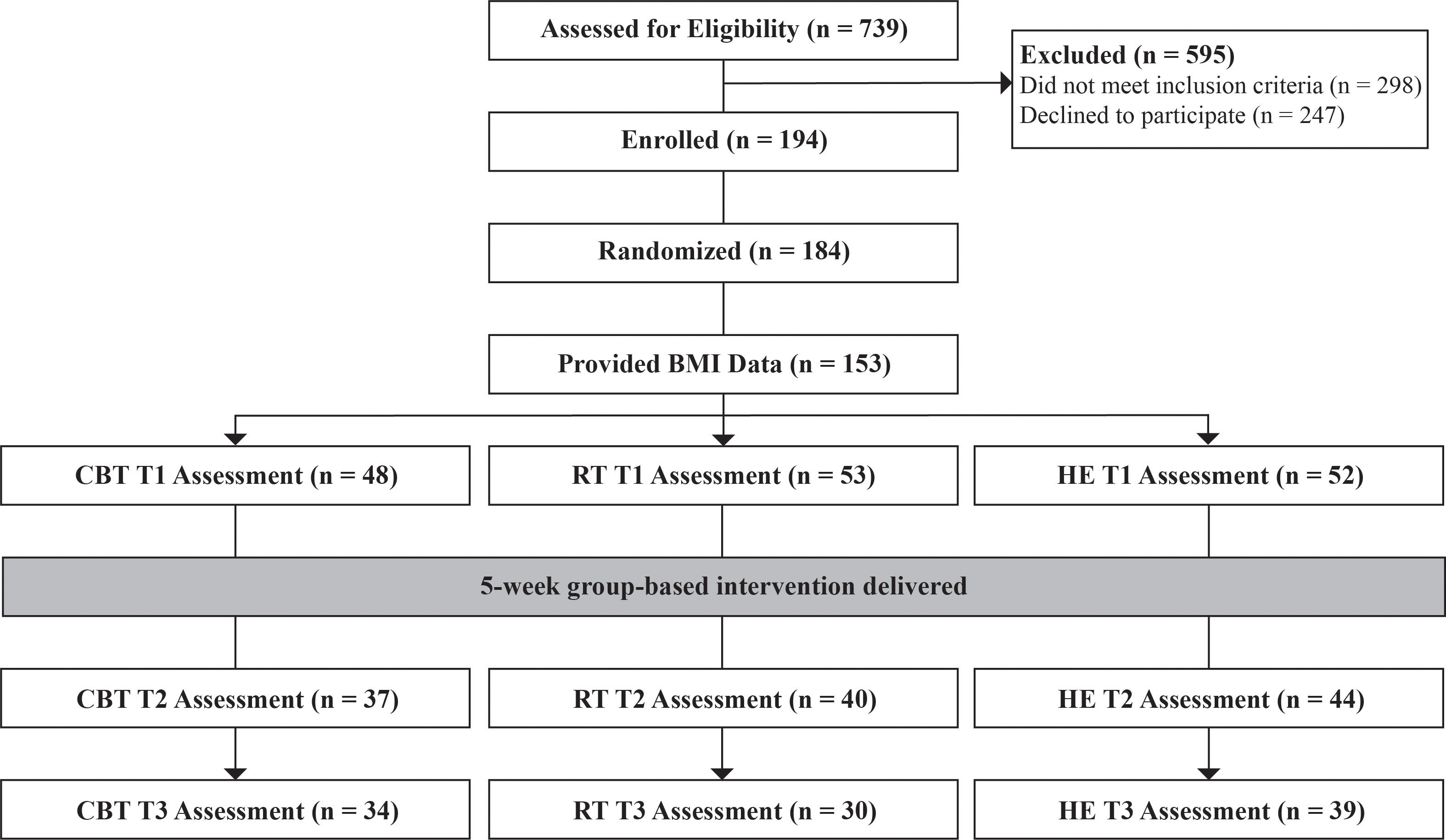 Fig. 1.
Fig. 1.CONSORT flow diagram. CBT, Cognitive Behavioral Therapy; RT, Relaxation Training; HE, Health Education. Of the 153 women who provided BMI data, baseline cytokine data were available for 149 women.
The sample (N = 153) was predominately middle-aged (M = 55.07, SD = 10.02), White (43.3%) and Hispanic (42.0%), with stage 1 (55.6%) disease. The majority (55.6%) fell within the OW/OB BMI (OW = 27.5%, OB = 28.1%), and 44.4% fell within the NW range. See Table 1 for full demographics and study variables by BMI classification and Table 2 for demographics and study variables by intervention condition.
| Normal weight vs Overweight/obese | ||||||
| Baseline (T1) | NW | OW/OB | Statistic | Diff | ||
| (N = 66) | (N = 83) | |||||
| IL-6 (ln) | 0.33 (1.34) | 1.24 (1.40) | t(146) = –4.03 | p | ||
| IL-6 (ng/mL) | 3.79 (8.73) | 15.29 (69.55) | - | - | ||
| IL-1 |
–0.60 (1.90) | 0.26 (1.90) | t(147) = –2.76 | p = 0.007** | ||
| IL-1 |
3.58 (10.68) | 7.90 (22.77) | - | - | ||
| TNF- |
0.41 (0.10) | 0.43 (1.12) | t(147) = –0.13 | p = 0.893 | ||
| TNF- |
2.34 (2.33) | 3.84 (13.05) | - | - | ||
| Anti-dep. | 5 (7.3%) | 11 (13.6%) | p = 0.221 | |||
| Anxiolytic | 10 (14.7%) | 14 (17.3%) | p = 0.694 | |||
| Pain med | 12 (17.6%) | 14 (17.3%) | p = 0 .954 | |||
| Sleep med | 12 (17.6%) | 12 (14.6%) | p = 0.616 | |||
| MVPA (hours) | 1.30 (1.94) | 0.76 (1.64) | t(132) = 1.75 | p = 0.082 | ||
| Age | 53.85 (10.6) | 54.71 (10.3) | t(108) = –0.42 | p = 0.676 | ||
| Income | 110.5 (69.7) | 118.65 (79.2) | t(108) = –0.56 | p = 0.573 | ||
| Stage | p = 0.183 | |||||
| Stage 0 | 13 (19.1%) | 13 (15.3%) | ||||
| Stage 1 | 41 (60.3%) | 44 (51.8%) | ||||
| Stage 2 | 10 (14.7%) | 25 (29.4%) | ||||
| Stage 3 | 4 (5.9%) | 3 (3.5%) | ||||
| ER+ Status | 55 (84.6%) | 71 (87.7%) | p = 0.596 | |||
| PR+ Status | 48 (73.8%) | 62 (79.5%) | p = 0.425 | |||
| Mastectomy | 34 (50.0%) | 43 (50.6%) | p = 0.942 | |||
| Time f/ surg. | 37.3 (25.2) | 35.7 (20.2) | t(151) = 0.44 | p = 0.661 | ||
| Ethnicity | p = 0.021* | |||||
| NHW | 37 (60.7%) | 28 (35.4%) | ||||
| Hispanic | 21 (34.4%) | 43 (54.4%) | ||||
| Other | 3 (4.9%) | 8 (10.1%) | ||||
| Follow-up (T3) | NW | OW/OB | Statistic | Diff | ||
| (N = 49) | (N = 54) | |||||
| IL-6 (ln) | 0.75 (1.44) | 1.35 (1.25) | t(99) = –2.25 | p = 0.027* | ||
| IL-6 (ng/mL) | 7.49 (19.48) | 10.27 (21.51) | - | - | ||
| IL-1 |
0.04 (2.14) | 0.43 (2.16) | t(101) = –0.92 | p = 0.360 | ||
| IL-1 |
7.55 (19.12) | 11.45 (36.36) | - | - | ||
| TNF- |
0.38 (1.62) | 0.43 (1.50) | t(101) = –0.14 | p = 0.893 | ||
| TNF- |
3.57 (4.03) | 3.45 (4.10) | - | - | ||
| Anti-dep. | 5 (8.9%) | 4 (6.7%) | p = 0.649 | |||
| Anxiolytic | 12 (21.4%) | 6 (9.8%) | p = 0.083 | |||
| Pain med | 10 (17.9%) | 3 (5.0%) | p = 0.028* | |||
| Sleep med | 11 (20.0%) | 9 (15.0%) | p = 0.480 | |||
| Radiation | 9 (16.1%) | 11 (18.3%) | p = 0.746 | |||
| Chemo | 5 (8.9%) | 4 (6.7%) | p = 0.651 | |||
| Reconstr. | 14 (24.6%) | 22 (36.1%) | p = 0.175 | |||
| MVPA (hours) | 0.67 (0.73) | 0.57 (0.73) | t(103) = 0.63 | p = 0.533 | ||
| Attendance | 4.29 (1.17) | 3.86 (1.49) | t(120) = 1.74 | p = 0.085 | ||
| Sample size based on participants with cytokine data. CBT, Cognitive Behavioral
Therapy; RT, Relaxation Training; HE, Health Education; Anti-dep., antidepressant;
MVPA, weekly moderate/vigorous physical activity; med, medicine; NHW,
non-Hispanic White; chemo, chemotherapy; time f/ surg., days from surgery until
T1; reconst, reconstructive surgery. Income measured in thousands.
| ||||||
| Normal weight (CBT/RT vs HE) (N = 66) | Overweight/obese (CBT/RT Vvs HE) (N = 83) | |||||||||
| Baseline (T1) | CBT/RT | HE | Statistic | Diff. | CBT/RT | HE | Statistic | Diff. | ||
| (N = 42) | (N = 24) | (N = 56) | (N = 27) | |||||||
| IL-6 (ln) | 0.29 (1.25) | 0.39 (1.50) | t(64) = –0.26 | p = 0.792 | 1.34 (1.36) | 0.97 (1.47) | t(80) = 1.20 | p = 0.250 | ||
| IL-6 (ng/mL) | 2.75 (4.12) | 5.62 (13.40) | - | - | 18.32 (83.0) | 8.77 (21.65) | - | - | ||
| IL-1 |
–0.33 (1.78) | 1.08 (2.04) | t(64) = 1.56 | p = 0.124 | 0.51 (1.78) | –0.25 (2.07) | t(81) = 1.73 | p = 0.108 | ||
| IL-1 |
3.00 (5.59) | 4.58 (16.27) | - | - | 8.53 (25.00) | 6.60 (17.71) | - | - | ||
| TNF- |
0.57 (1.04) | 0.12 (0.86) | t(64) = 1.79 | p = 0.078 |
0.33 (1.10) | 0.64 (1.14) | t(81) = –1.21 | p = 0.231 | ||
| TNF- |
2.75 (2.59) | 1.63 (1.59) | - | - | 4.00 (15.68) | 3.51 (4.08) | - | - | ||
| Anti-dep. | 5 (11.6%) | 0 (0%) | p = 0.150 | 9 (16.3%) | 2 (7.7%) | p = 0.489 | ||||
| Anxiolytic | 6 (14.0%) | 4 (16.0%) | p = 0.818 | 11 (20%) | 3 (11.1%) | p = 0.369 | ||||
| Pain med | 9 (20.9%) | 3 (12.0%) | p = 0.352 | 9 (16.3%) | 5 (12.0%) | p = 0.750 | ||||
| Sleep med | 7 (16.3%) | 5 (20%) | p = 0.700 | 9 (16.3%) | 3 (11.1%) | p = 0.527 | ||||
| MVPA (hours) | 1.40 (1.82) | 1.13 (2.14) | t(58) = 0.53 | p = 0.597 | 0.73 (1.63) | 0.81 (1.69) | t(72) = –0.21 | p = 0.831 | ||
| Age | 52.88 (10.6) | 55.52 (10.5) | t(66) = –0.99 | p = 0.326 | 56.66 (10.0) | 54.74 (8.3) | t(83) = 0.87 | p = 0.390 | ||
| Income | 94.84 (50.8) | 137.43 (88.7) | t(66) = –2.53 | p = 0.014* | 99.22 (69.9) | 110.34 (74.4) | t(83) = –0.67 | p = 0.505 | ||
| Stage | p = 0.349 | p = 0.647 | ||||||||
| Stage 0 | 11 (25.6%) | 2 (8.0%) | 7 (12.1%) | 6 (22.2%) | ||||||
| Stage 1 | 24 (55.8%) | 17 (68.0%) | 32 (55.2%) | 12 (44.4%) | ||||||
| Stage 2 | 6 (14.0%) | 4 (16.0%) | 17 (29.3%) | 8 (29.6%) | ||||||
| Stage 3 | 2 (4.7%) | 2 (8.0%) | 2 (3.4%) | 1 (3.7%) | ||||||
| ER+ Status | 35 (85.0%) | 20 (80.0%) | p = 0.415 | 51 (91.1%) | 20 (80%) | p = 0.271 | ||||
| PR+ Status | 30 (75.0%) | 18 (71.0%) | p = 0.749 | 43 (78.2%) | 19 (82.6%) | p = 0.659 | ||||
| Mastectomy | 22 (51.2%) | 12 (48.0%) | p = 0.801 | 30 (51.7%) | 13 (48.1%) | p = 0.759 | ||||
| Time f/ surg. | 39.2 (29.6) | 34.0 (15.0) | t(66) = 0.81 | p = 0.419 | 36.0 (21.5) | 35.1 (17.5) | t(83) = 0.18 | p = 0.857 | ||
| Ethnicity | p = 0.334 | p = 0.958 | ||||||||
| NHW | 21 (56.8%) | 16 (66.7%) | 19 (35.8%) | 9 (34.6%) | ||||||
| Hispanic | 15 (40.5%) | 6 (25.5%) | 29 (54.7%) | 14 (53.8%) | ||||||
| Other | 1 (2.7%) | 2 (8.3%) | 5 (9.4%) | 3 (11.5%) | ||||||
| Follow-up (T3) | CBT/RT | HE | Statistic | Diff. | CBT/RT | HE | Statistic | Diff. | ||
| (N = 31) | (N = 18) | (N = 33) | (N = 21) | |||||||
| IL-6 (ln) | 0.92 (1.57) | 0.45 (1.18) | t(46) = 1.09 | p = 0.280 | 1.47 (1.15) | 1.14 (1.39) | t(51) = 0.94 | p = 0.353 | ||
| IL-6 (ng/mL) | 10.32 (24.2) | 2.77 (2.91) | - | - | 10.65 (21.5) | 9.64 (22.11) | - | - | ||
| IL-1 |
0.19 (2.28) | –0.21 (1.93) | t(47) = 0.62 | p = 0.555 | 0.60 (1.93) | 0.15 (2.50) | t(52) = 0.75 | p = 0.459 | ||
| IL-1 |
10.11 (23.5) | 3.15 (4.82) | - | - | 6.46 (9.70) | 19.28 (56.98) | - | - | ||
| TNF- |
0.40 (1.74) | 0.36 (1.44) | t(47) = 0.08 | p = 0.935 | 0.34 (1.34) | 0.56 (1.75) | t(52) = –0.51 | p = 0.611 | ||
| TNF- |
3.88 (4.37) | 3.05 (3.42) | - | - | 2.71 (2.72) | 4.62 (5.52) | - | - | ||
| Anti-dep. | 4 (11.1%) | 1 (4.8%) | p = 0.397 | 2 (5.1%) | 2 (9.0%) | p = 0.567 | ||||
| Anxiolytic | 7 (19.4%) | 5 (23.8%) | p = 0.737 | 5 (12.8%) | 1 (4.5%) | p = 0.297 | ||||
| Pain med | 4 (11.1%) | 6 (28.6%) | p = 0.105 | 2 (5.1%) | 1 (4.5%) | p = 0.902 | ||||
| Sleep med | 8 (22.2%) | 3 (14.3%) | p = 0.405 | 5 (12.8%) | 4 (18.2%) | p = 0.599 | ||||
| Radiation | 6 (16.7%) | 3 (14.3%) | p = 0.812 | 8 (20.5%) | 3 (13.6%) | p = 0.502 | ||||
| Chemo | 5 (13.9%) | 0 (0%) | p = 0.074 |
3 (7.7%) | 1 (4.5%) | p = 0.634 | ||||
| Reconstr. | 10 (27.8%) | 4 (19.0%) | p = 0.460 | 15 (38.5%) | 7 (31.8%) | p = 0.604 | ||||
| MVPA (hours) | 0.60 (0.73) | 0.76 (0.74) | t(49) = –0.78 | p = 0.442 | 0.54 (0.77) | 0.65 (0.68) | t(52) = –0.56 | p = 0.578 | ||
| Attendance | 4.22 (1.27) | 4.47 (0.915) | t(49) = –0.68 | p = 0.503 | 3.72 (1.57) | 4.19 (1.25) | t(69) = –1.22 | p = 0.226 | ||
| Sample size based on participants with cytokine data. CBT, Cognitive Behavioral
Therapy; RT, Relaxation Training; HE, Health Education; Anti-dep., antidepressant;
MVPA, weekly hours of moderate/vigorous physical activity; med, medicine; NHW,
non-Hispanic White; chemo, chemotherapy; time f/ surg., days from surgery until
T1; reconst, reconstructive surgery. Income measured in thousands.
| ||||||||||
We first compared cytokine values at baseline between intervention conditions
(CBT, RT, HE) and between BMI groups (NW, OW, OB) using ANOVA. At baseline, there
was a significant difference between intervention conditions in IL-1
As hypothesized there was a significant overall difference in baseline IL-6
(F(2,145) = 8.45, p
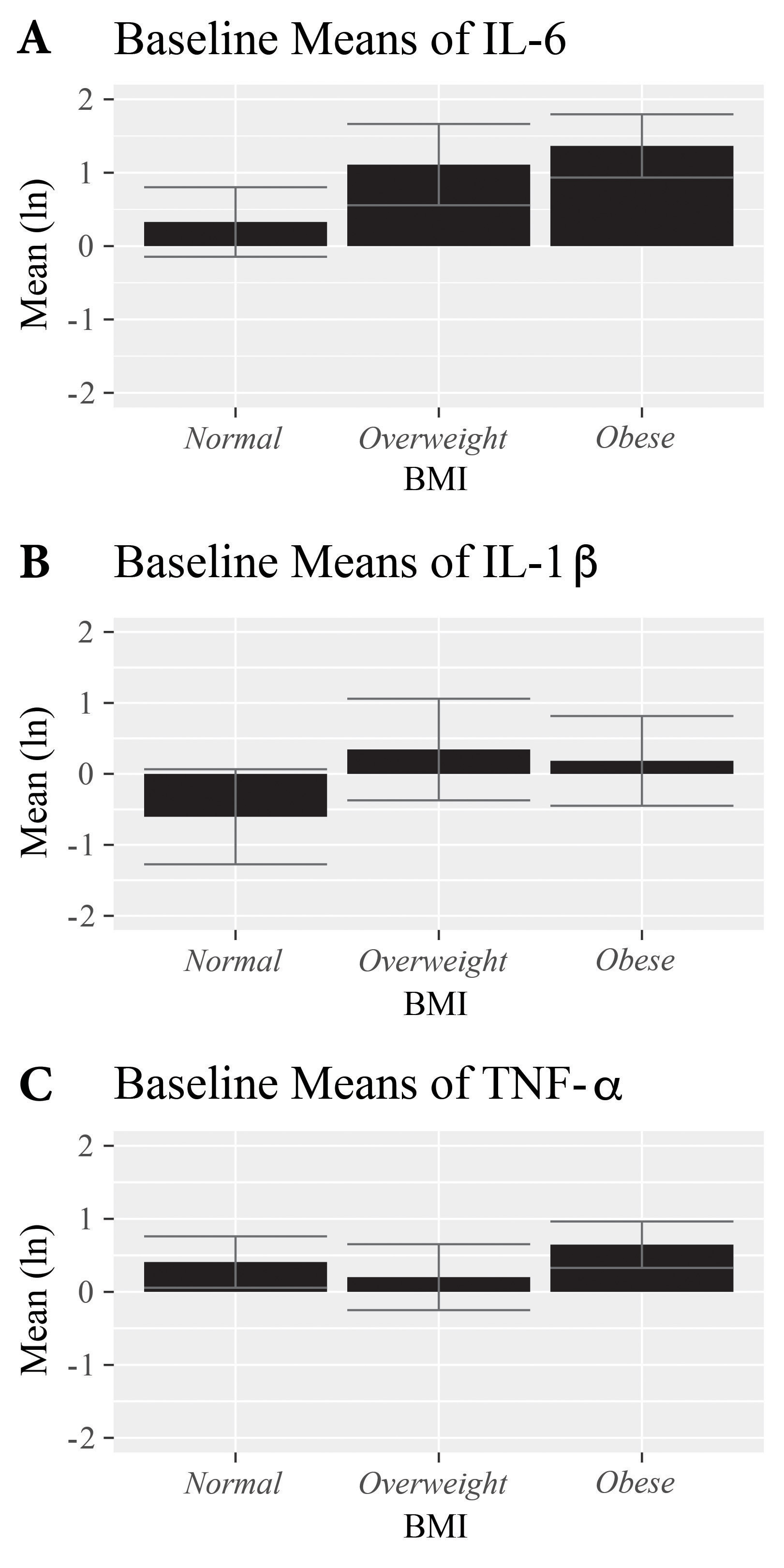 Fig. 2.
Fig. 2.Mean baseline cytokine
values by BMI category in breast cancer patients 2–10 weeks post-surgery and
prior to initiating adjuvant chemotherapy or radiation. Cytokine levels are
log-transformed to achieve normality. Error bars represent 95% confidence
intervals. There was a significant overall difference in baseline IL-6 (F(2,145)
= 8.45, p
Only one participant (CBT/RT; OW/OB) had received radiation within the 3 weeks
prior to T3, and only one participant (HE; OW/OB) received chemotherapy within
the 3 weeks prior to T3. Neither receipt of chemotherapy (F(1,105) = 0.028,
p = 0.868) nor radiation (F(1,105) = 0.754, p = 0.387)
significantly predicted the change in IL-6. Similar results were observed for
predicting change in IL-1
Most participants (61.4%) completed at least 4 out of 5 intervention sessions. There was no significant difference in session attendance between BMI categories (p = 0.085), with NW women attending an average of 4.29 out of 5 sessions as compared to OW/OB women attending an average 3.86 out of 5 sessions. A two condition (CBT/RT vs HE) by two group (OW/OB vs NW) by two timepoint (T1, T2) RMANOVA predicting the PSMS composite score was run as a manipulation check. There was a significant time by condition interaction (F(1,102) = 9.52, p = 0.003), such that women in the active CBT/RT conditions had greater increases in perceived stress management skills over time compared to women in the HE control condition. The three-way interaction was not significant (F(1,102) = 3.16, p = 0.078). Thus, assignment to either of the stress management interventions produced greater improvements in perceived stress management skills as compared to the HE condition irrespective of BMI group.
A two condition (CBT/RT vs HE) by two group (OW/OB vs NW) by two timepoint (T1, T3) RMANOVA predicting IL-6 was run. There was no main effect of time in predicting IL-6 (F(1,86) = 0.44, p = 0.410), but there was a main effect of BMI (F(1,86) = 9.66, p = 0.003), with OW/OB women having greater IL-6 levels across timepoints and conditions. There was a significant three-way time by BMI by condition interaction (F(1,86) = 5.00, p = 0.028), indicating moderation. Given the significant three-way interaction, we conducted subgroup analyses by BMI. There was no significant time by condition interaction among NW women, F(1,37) = 0.19, p = 0.664), but there was a time by condition interaction among OW/OB women (F(1,45) = 4.24, p = 0.045), such that only OW/OB women experienced decreased IL-6 over time when receiving CBT/RT vs HE, as shown by the the mean change score in IL-6 by study condition (CBT/RT vs HE) among OW/OB women (Fig. 3). Supplementary Fig. 1 shows IL-6 change scores by intervention in OW and OB women separately for descriptive purposes. In each case assignment to CBT/RT was associated with a decrease or no increase in IL-6 vs a rise in IL-6 in HE.
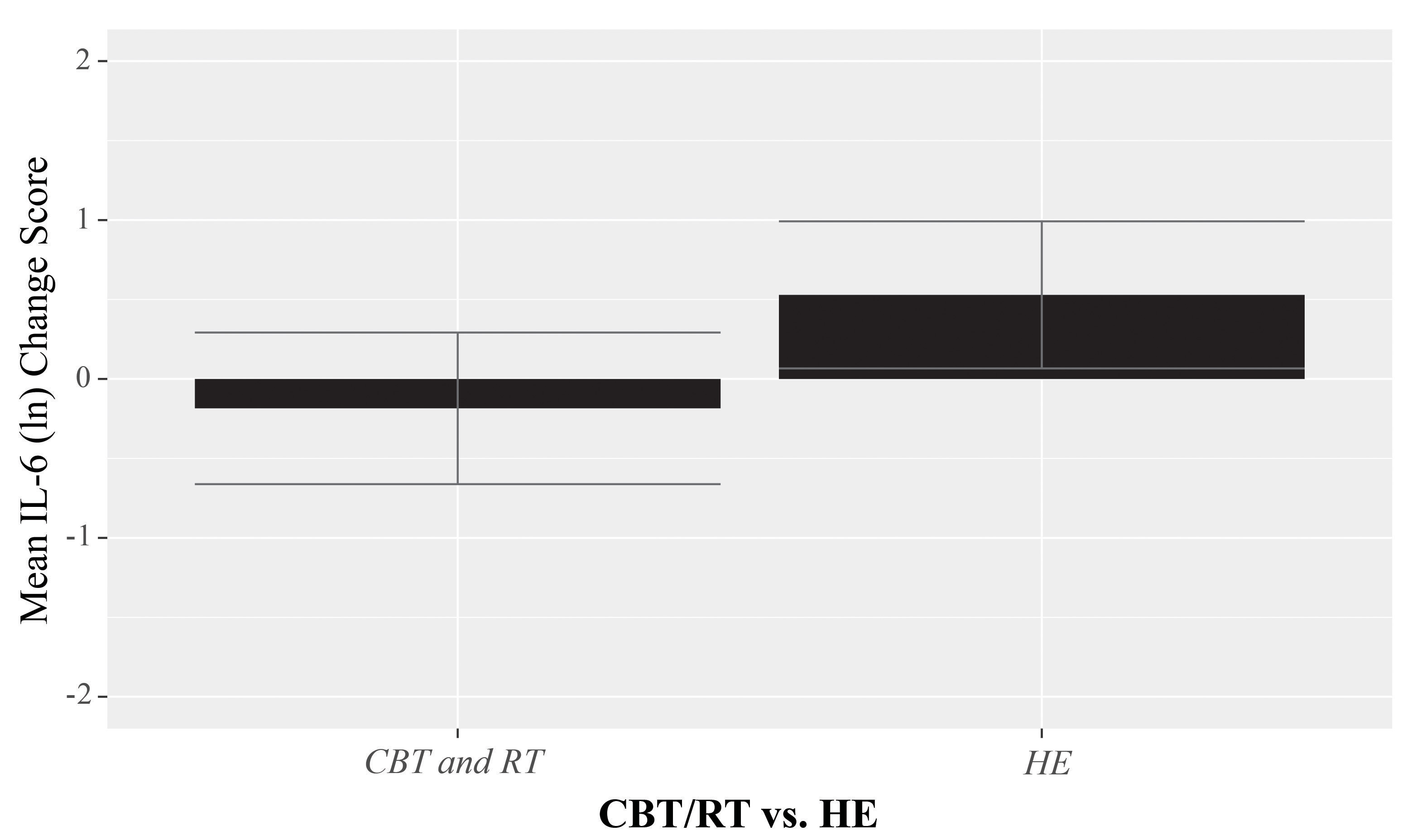 Fig. 3.
Fig. 3.Change in IL-6 pre- to 6-months post-intervention by study condition (CBT/RT vs HE) among overweight and obese women with breast cancer combined. Cytokine levels are log-transformed to achieve normality. Error bars represent 95% confidence intervals. RMANOVA indicated that overweight/obese women receiving CBT/RT had significantly decreased IL-6 levels over time vs those who received HE (F(1,45) = 4.24, p = 0.045).
An additional two condition (CBT/RT vs HE) by two group (OW/OB vs NW) by two
timepoint (T1, T3) RMANOVA predicting IL-1
Finally, a two condition (CBT/RT vs HE) by two group (OW/OB vs NW) by two
timepoint (T1, T3) RMANOVA predicting TNF-
There were no significant baseline differences between BMI categories on the self-reported level of MVPA (t(132) = 1.75, p = 0.082), with OW/OB women having a mean of 0.75 hours of MVPA while NW women had a mean of 1.30 hours in the past week. At follow-up, there was also no difference between groups (t(103) = 0.63, p = 0.533), with OW/OB women having a mean of 0.57 hours of MVPA while NW women had a mean of 0.67 hours in the past week (Table 1).
In a two condition (CBT/RT vs HE) by two group (OW/OB vs NW) by two timepoint (T1, T3) RMANOVA predicting MVPA controlling for previously stated covariates, there was no main effect of time (F(1,83) = 0.39, p = 0.533) or of BMI (F(1,83) = 1.90, p = 0.172). There was no significant three-way time by BMI by condition interaction (F(1,83) = 0.01, p = 0.920) Finally, we reran the analyses of intervention effects on IL-6 and found that the significant three-way interaction predicting IL-6 change was retained when we controlled for contemporaneous changes in MVPA (F(1,70) = 4.05, p = 0.048). Together, this evidence suggests that changes in MVPA did not explain the effects of treatment arm on contemporaneous changes in IL-6 over time.
The present analyses found that both OW and OB women with newly diagnosed BC had
significantly greater levels of circulating inflammatory cytokines IL-6 and
IL-1
We did not find any evidence of a relationship between 5-week stress management,
BMI, and the change in inflammatory IL-1
A manipulation check demonstrated that women who received the active stress management conditions reported significantly increased perceived stress management skills vs those in the HE control condition, which verified that our active conditions were effectively training participants. Notably, this effect did not differ by BMI. Thus, although both OW/OB and NW women receiving stress management interventions reported significantly greater confidence in their ability to manage stress, unique processes occurred within OW/OB women resulting in decreased IL-6 levels over the study period. It is likely that OW/OB women, who presented with significantly higher IL-6 at baseline, were more able to benefit physiologically from a stress management intervention due to the co-occurring, and potentially interacting, effects of acute stress [38], chronic stress [39], and adiposity [24, 25, 26, 27, 28, 29] on neuroendocrine regulation and inflammation. Providing coping and relaxation techniques may have been more impactful in this particularly vulnerable population.
Our analyses were unable to identify the mechanism by which these interventions affected biomarkers within OW/OB women. Given that physical activity is related to inflammatory markers [65] and BMI (i.e., increases in physical activity may reduce BMI), and prior evidence that stress management interventions in other trials may increase engagement in physical activity during BC treatment [66], we tested whether there was an increase in MVPA among OW/OB women participating in stress management groups. However, there was no significant intervention condition by BMI by time interaction effect on MVPA over the study period. Overall, MVPA decreased over the study period across all conditions and BMI categories, likely due to physical limitations associated with adjuvant treatment, and was not a likely explanation for the effects of stress management intervention on cytokine changes. Since there were no differences in adjuvant treatments or other medications received among conditions, we can rule out these as contributing to our results.
Future research should continue to investigate potential mechanisms of change that may explain the relationship between BMI, stress management, and inflammation in BC patients. For example, it is possible stress management may decrease negative self-view and internalized weight stigma among OW/OB women, thereby decreasing stress and inflammation. There is literature suggesting that OW/OB individuals experience significant weight stigma and discrimination in the United States [67, 68, 69]. Some OW/OB individuals internalize this weight stigma, thus devaluing themselves based on their weight [70]. Stress management interventions may influence internalized weight stigma by targeting and reappraising cognitions and can provide adaptive coping mechanisms for the related distress. These skills may also allow them to better cope with external weight stigma they face, which have been shown occur frequently in healthcare settings [69], as these women navigate frequent medical appointments for their BC treatment.
In addition, it is possible women who received stress management replaced maladaptive coping techniques with adaptive coping skills. For example, women in stress management conditions may engage in cognitive restructuring (in CBT condition) or mindfulness meditation (in RT condition) when distressed as opposed to emotional eating, a common stress response that may lead to further distress [71] and which may contribute to the development and maintenance of obesity [72]. There is evidence that both behavioral [73] and mindfulness-based psychological interventions [74] decrease emotional eating behaviors. Therefore, it is plausible that in our sample, OW/OB women in the stress management conditions decreased maladaptive emotional eating and increased adaptive coping responses, thereby increasing psychological well-being, and decreasing circulating inflammatory cytokines. Future research should investigate the role of emotional eating in the relationship between BMI, stress management, and inflammation, as well as the role of other eating styles (i.e., mindless vs mindful eating [75], intuitive eating [76], restrictive eating [77]), to add further nuance to these findings.
There are several limitations of the current study to note. First, BMI was calculated through self-report by participants, which may be subject to error. However, there is data demonstrating that self-report and objective weights are generally well-correlated [78, 79]. In addition, 30 women who participated in the original trial (16.3%) declined to provide height and weight data and were thus excluded from the current analysis, which may add selection bias to our findings. Further, BMI as a measure of weight status has limitations and may lack specificity in estimating body fat. Due to the nature of the post-hoc analyses, we did not have a longitudinal measure of BMI or weight at follow-up, and therefore cannot know if the change in inflammatory cytokines in the OW/OB women receiving stress management is related to a decrease in weight over the study period. In addition, we did not have a standardized measure of diet or eating styles pre- to post-intervention, which would have added greater nuance to our findings. However, intervention effects on IL-6 held when controlling for contemporaneous changes in physical activity, providing some evidence that our results were not due to changes in energy balance over the study period.
The current analysis is also limited in that adipokines were not collected in addition to cytokines. The relationship between obesity and BC is thought to be likely related to both inflammation, measured here by inflammatory cytokines, as well as deregulation of adipokine secretion [80]. Adiponectin is the most numerous adipokine, has anti-inflammatory properties, and may decrease tumor proliferation, but is significantly decreased in OW/OB women [80, 81, 82, 83]. In addition, we did not collect data on the expression of genes that are associated with inflammation and health outcomes in BC, including ErbB2 [84]. Future research should determine whether stress management impacts adiponectin in OW/OB women, and whether specific gene expression may play a role in the relationship between stress and inflammation in OW/OB women with BC.
Despite these limitations, the current study has several strengths. We analyzed immunological, psychological, and behavioral data from a diverse cohort of women (42% Hispanic) with newly diagnosed BC who had participated in a prior RCT. This study adds to the current literature by examining how brief stress management interventions comprising CBSM (CBT- and RT-based) may impact inflammatory biomarkers among BC patients with different BMI levels. This work has important implications for further understanding the biobehavioral mechanisms by which OW/OB women with BC experience worse health outcomes [85, 86], and to work towards developing targeted interventions to improve outcomes among this high-risk population.
OW and OB women with newly diagnosed BC had significantly greater levels of IL-6
and IL-1
ACS, American Cancer Society; ANOVA, Analysis of variance; BC, Breast cancer;
BMI, Body mass index; CBSM, Cognitive-Behavioral Stress Management; CBT,
Cognitive behavioral therapy; CDC, Center for Disease Control and Prevention;
DFS, Disease-free survival; ELISA, Enzyme-linked immunosorbent assay; ER/PR,
Estrogen receptor/Progesterone receptor; HE, Health education; IL-1
MR, MA and BB conceptualized the current study. AD performed the research. MR analyzed the data. MA, BB, AD, CT, and DF provided guidance on analyses and interpretation. MR, ESC, and MA wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
This trial was approved by the Institutional Review Board at the University of Miami and is registered as National Institutes of Health Clinical Trial NCT02103387. The procedures used in this study adhere to the tenets of the Declaration of Helsinki. All women participating in the study completed informed consent procedures.
Not applicable.
This work was supported by the National Cancer Institute (2R01CA064710-10A1).
Michael Antoni reports that he is a paid consultant for Blue Note Therapeutics and Atlantis Healthcare, two digital health companies, is the inventor of CBSM (UMIP-483), and receives royalties for published CBSM treatment manuals. Chloe Taub is also a paid consultant for Blue Note Therapeutics. None of the other authors have conflicts of interest to report. DF is serving as the editorial board member of this journal. We declare that DF had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to GP.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.fbl2705148.



