1 Department of Gynecology and Obstetrics, Kanuni Sultan Suleyman Training and Research Hospital, Health Sciences University, 34668 Istanbul, Turkey
2 Department of Gynecology and Obstetrics, Arnavutkoy State Hospital, 34275 Istanbul, Turkey
Abstract
Background: The aim of this study was to investigate patients having
pelvic organ prolapse (POP) stage 2 and greater who have undergone vaginal
hysterectomy concomitant with sacrospinous ligament fixation (VAH + SLF) or total
laparoscopic hysterectomy concomitant with sacrocolpopexy (TLH + SCP) in terms of
quality of life, sexual function, major or minor complications, and cure rates.
We also aimed to determine which procedure is superior according to the results
of the cases in which TLH + SCP and VAH + SLF were applied. Methods: A
retrospective cohort study was conducted at a tertiary center, including 137
patients who underwent vaginal or laparoscopic hysterectomy for symptomatic
uterine prolapse with a pelvic organ prolapse quantification system (POP-Q) score
Keywords
- laparoscopic sacrocolpopexy
- pelvic organ prolapse
- sacrospinous ligament fixation
- vaginal hysterectomy
- quality of life
Pelvic organ prolapse (POP) is a common condition that affects 40% of the female population and negatively affects the quality of life [1, 2]. The incidence of prolapse increases with age, with a peak frequency between 70 and 79 years of age [3]. In a recent review, the recurrence rate of POP was estimated to be 36%, and it was mentioned that levator muscle weakness, POP staging, and familial predisposition were the most common risk factors [4]. The cumulative incidence of vaginal cuff prolapse after a hysterectomy is 0.5% [5, 6]. Approximately half of women who have given birth experience laxity of their pelvic structures [7, 8, 9]. Nineteen percent of those women will require pelvic surgery during their lifetime [7, 8, 9]. Also, the risk for women having POP surgery throughout their lives is 12.6% [10].
POP surgeries constitute a significant proportion of all gynecologic surgeries. Although we do not know the exact causes of POP, the evidence supports that this condition is highly associated with previous pregnancy. Childbirth-related factors are an abnormally long latent phase or second stage, operative vaginal delivery (vacuum or forceps), grand multiparity, and fetal macrosomia. Frequently expressed symptoms of POP are fullness or pressure in the vagina, low back and groin pain, vaginal discomfort, and pelvic heaviness. Additional symptoms with POP can be seen, including vesical, bowel, and sexual-related problems [11]. Surgeons prefer various approaches for apical prolapse treatment based on the patient’s condition and concomitant pathologies. Those options include both abdominal and vaginal routes. Apical vaginal prolapse surgery consists of different approaches, including the vaginal route with sacrospinous ligament fixation (SLF) and the route of abdominal sacrocolpopexy (ASC).
ASC is the gold standard procedure for the treatment of apical vault prolapse, as described by Lane et al. [12] in 1962. In 1968, Richter et al. [13] contributed to the literature by performing SLF procedure utilizing a vaginal approach. Mahendran [14] described a minimally invasive option for vaginal prolapse treatment using laparoscopic sacrocolpopexy (LSC) in 1996. McCall culdoplasty, uterosacral ligament suspension, sacrospinous ligament suspension, and iliococcygeus suspension methods are vaginal route procedures that use the patient’s “native tissue” [15]. Conversely, synthetic mesh is used in ASC [16]. However, minimally invasive robotic sacrocolpopexy (SCP) options also exist [17]. Following a hysterectomy, we prefer LSC after laparoscopic hysterectomy and sacrospinous fixation after vaginal hysterectomy (VAH) to prevent vaginal cuff prolapse in patients with pelvic organ prolapse quantification system score of 2 (POP-Q 2) and greater POP. Although many procedures prevent cuff prolapse after a hysterectomy, should we prefer the laparoscopic or vaginal approach to prevent vaginal cuff prolapse after hysterectomy in cases with POP-Q 2 or higher pelvic organ prolapse (POP)? In cases with POP, should hysterectomy be performed according to the planned method of the sling, or should the sling procedure be preferred according to the method in which hysterectomy is performed? Here we aimed to find answers to these questions. Our clinical observations and experience showed better results in patients who underwent SCP after a hysterectomy. In this context, we wanted to support this hypothesis by performing our study.
In this present study, we performed SLF and LSC surgery to prevent cuff prolapse in patients diagnosed with POP with a POP-Q score of 2 or higher, who were undergoing laparoscopic or VAH for various indications. We compared all the results of total laparoscopic hysterectomy concomitant with sacrocolpopexy (TLH + SCP) and vaginal hysterectomy concomitant with sacrospinous ligament fixation (VAH + SLF) and further investigated whether either of those procedures was superior to the other.
We conducted a retrospective cohort study which included 137 patients diagnosed with POP at stage 2 or greater according to POP-Q staging. The procedures of VAH + SLF or TLH + SCP occurred between January 2017 and May 2022 in the department of Istanbul Health Sciences University Kanuni Sultan Süleyman Training and Research Hospital. The study protocol was approved by the institution’s ethics committee (Approval number: KAEK 2022.05.118). This study was carried out according to the Helsinki Declaration.
The first group comprised 90 patients (VAH + SLF) who underwent VAH for POP and
SLF concomitantly to prevent cuff prolapse. The second group consisted of 47
patients who underwent SCP (TLH + SCP) for prevention of cuff prolapse in
patients who were scheduled for laparoscopic hysterectomy for uterine prolapse
and other additional pathologies. The electronic medical database of the hospital
was used to determine patients who underwent VAH + SLF or TLH + SCP concurrently
due to uterine descent. We reviewed all the patient information from the
hospital’s electronic medical database between June 2022 and September 2022.
Patients older than 40 with POP staging
Demographic data including age, parity, body mass index (BMI), smoking, menopausal status, presence of chronic disease, and obstetric history were obtained from the patients’ records. All patients received the same pre-operative and postoperative procedures during the study. A complete medical history was obtained from the patients prior to surgery including a detailed physical examination. The Turkish-translated version of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) and the Prolapse Quality of Life Questionnaire (P-QoL) questionnaires were routinely administered to the patients during both pre-operative and postoperative periods. Topical estrogen therapy was administered to patients pre-operatively for two weeks. Antibiotic prophylaxis was administered to all patients pre-operatively (1–2 g intravenous ceftriaxone). Additionally, we administered low molecular weight heparin prophylaxis to at-risk patients in the postoperative period.
Perioperative and postoperative complications were classified as minor and major. Minor complications included postoperative fever, vaginal cuff coagulum, vaginal cuff infection, urinary tract infection, mesh or suture erosion, and neural entrapment. Major complications were bladder injury, re-laparotomy due to bleeding, bowel injury, and intra-abdominal hematoma. The perioperative data, such as the surgical type (vaginal or laparoscopic), operating time, length of hospital stay, return to daily activities, and estimated blood loss, were recorded. We assessed the presence of recurrence, long-term complications, and POP-Q classifications in the patients. We evaluated the results of the P-QoL and PISQ-12 questionnaires which were requested to be completed by all patients. Patients routinely completed these questionnaires on the 30th postoperative day, at six months, and at one year. A visual analog scale (VAS) was performed after the 6th and 48th hours of the procedure to evaluate postoperative pain. A validated 100 mm VAS was used for measuring patients’ pain scores. We accepted that all cases included in the study improved objectively if the C point (cervix uteri or vaginal cuff) was –5 or below in the POP-Q test, which was determined by the gynecological examination performed one year after the surgery. The subjective cure was analyzed with P-QoL and PISQ-12 validated questionnaires.
The mesh used in LSC surgery was the Betamix brand. We applied LSC to the patients who underwent total laparoscopic hysterectomy (TLH) to prevent vaginal prolapse. Considering the possibility of affecting the results of sling operations, only cases with a VAH and sacrospinous fixation, laparoscopic hysterectomy, and LSC were included in the study. Those who had other additional operations were excluded from the study. In LSC, the 30-degree telescope was entered at the umbilicus through a 10 mm trocar after the pneumoperitoneum was created. Three 5 mm trocars were entered, two from the bilateral lower left sides and one from the suprapubic region. We used the Koh Cup™ and a RUMI-2 uterine manipulator colpotomizer (Rumi II, UMH650, Cooper Surgical, Trumbull, CT, USA) to elevate the vaginal cuff after TLH. We deperitonized the pubocervical fascia anteriorly and rectovaginal fascia posteriorly. We fixed the sigmoid colon and rectum to the left side of the abdominal wall with a number one silk suture. The peritoneum was cut with a harmonic device (HP300 Ethicon, Johnson & Johnson Medical NV, Waterloo, Belgium), starting from the promontory and proceeding from the right of the rectum through the deepest part of the cul-de-sac and vaginal vault. We fixed Betamix mesh to the vaginal cuff with Type 1 monofilament size 0 propylene suture; the other end of the mesh was fixed with a size 0 propylene suture to the sacral promontory by hanging the vagina in a way that would not create too much tension in the appropriate anatomical position. The peritoneum, including the vaginal vault, was repaired with a size 0 polyflame absorbable suture. Additionally, we performed other surgical procedures as necessary in the same session.
We unilaterally performed SLF on the right side following a VAH. We incised the posterior wall of the vagina, including the mucosa and the vaginal wall, from the midline to the apex of the cuff, from a distance of 20 mm to the vaginal entrance. We removed the vaginal wall from the rectovaginal fascia with sharp and blunt dissection. We entered the pararectal area from the right side of the vagina with sharp and blunt dissection, passing the rectovaginal fascia. We analyzed the os ischiatic and sacrum plates anatomically. Using the Breisky retractor, we placed one on the right side of the rectum and one on the base to view the sacrospinous ligament. We crossed twice, taking the total thickness from the sacrospinous ligament with 0 Prolene sutures. We passed both sutures at the apex of the vaginal dome posteriorly through the rectovaginal fascia from both sides. We primarily repaired the rectovaginal fascia and then sutured the posterior vaginal wall with a 2/0 vicryl suture. We knotted the Prolene sutures through the posterior wall of the vaginal cuff and fixed the new vaginal apex up to the sacrospinous ligament level.
In selected cases, pelvic floor physiotherapy, Kegel exercises, and pessary placement treatments were applied for conservative treatment. However, these surgical procedures were applied to those who passed the surgical threshold and could not comply with the treatment and recommendations.
The reasons for vaginal hysterectomy in cases diagnosed with POP-Q 2 and above pelvic organ prolapse are as follows; Cases of refusal of organ preserving surgery, treatment-resistant abnormal uterine bleeding, simple type endometrial hyperplasia without atypia, adenomyosis, persistent postmenopausal bleeding, progression of uterine prolapse despite conservative treatment, presence of a premalignant cervical lesion. The reasons for performing a laparoscopic hysterectomy in cases with POP-Q 2 and above pelvic organ prolapse are myoma uteri, treatment-resistant menometrorrhagia, presence of benign pelvic mass, simple type endometrial hyperplasia without atypia. We preferred the fixation of the sacrospinous ligament in vaginal hysterectomy since it is the procedure that has been performed the most and for the longest time in the world since 1958, and it is close to improving the anatomy [18, 19]. Our application of laparoscopic sacrocolpopexy after laparoscopic hysterectomy is accepted as the gold standard for apical prolapse after hysterectomy with a success rate of approximately 91.3% [20].
Reference study number 18 was used in the calculation. The G-Power Version 3.1.9.4 program (Kiel University, Kiel, Germany) calculated the sample size as at least 68 people.
The formula used for the calculation was: Sample size n = [DEFF (DISEIN EFFECT)
N: Population size (for finite population correction [FPC] factor);
p: Frequency of hypothesized outcome factor in the population;
d: Confidence limits as % of 100 (absolute
The analyses were performed using SPSS 24.0 (IBM Corp., Armonk, NY, USA). We
applied the independent t-test, Fisher’s exact test, and the Chi-square
test for categorical variables. Sample t-test was applied within the
groups, especially to evaluate the survey results. The level of significance was
set at a p-value
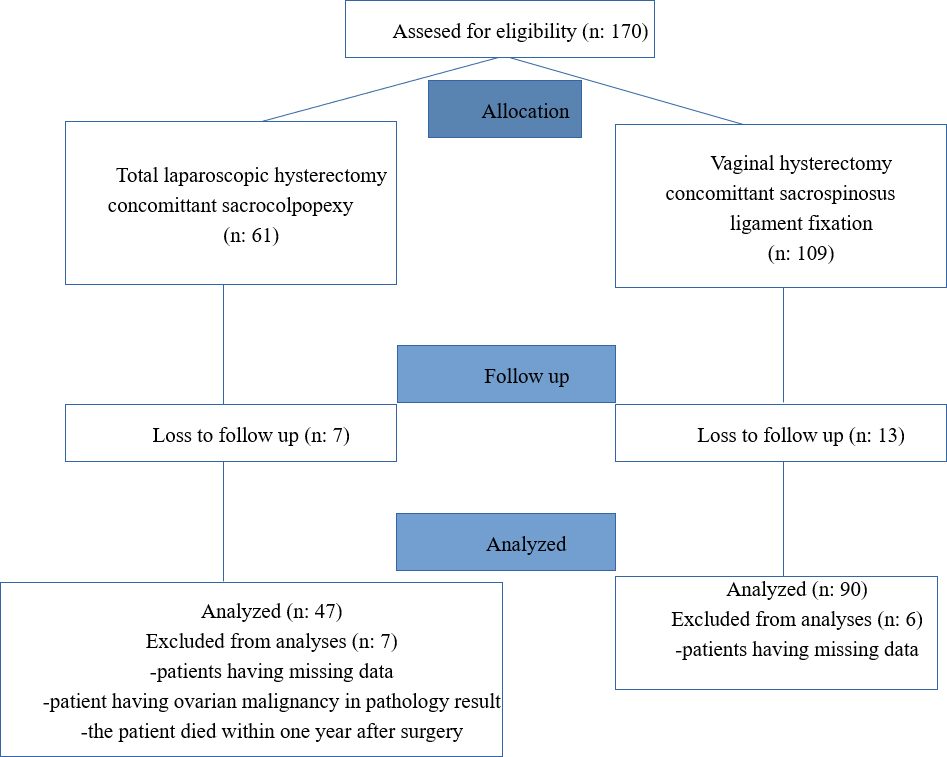
In our study, a total of 137 patients were included who had undergone TLH + SCP (n = 90) or VAH + SLF (n = 47) for benign indications (Fig. 1). There was no statistically significant difference among groups in terms of demographic and clinical characteristics (age, BMI, parity, smoking, menopausal status, and type of birth) except for chronic diseases (p = 0.004) (Tables 1,2).
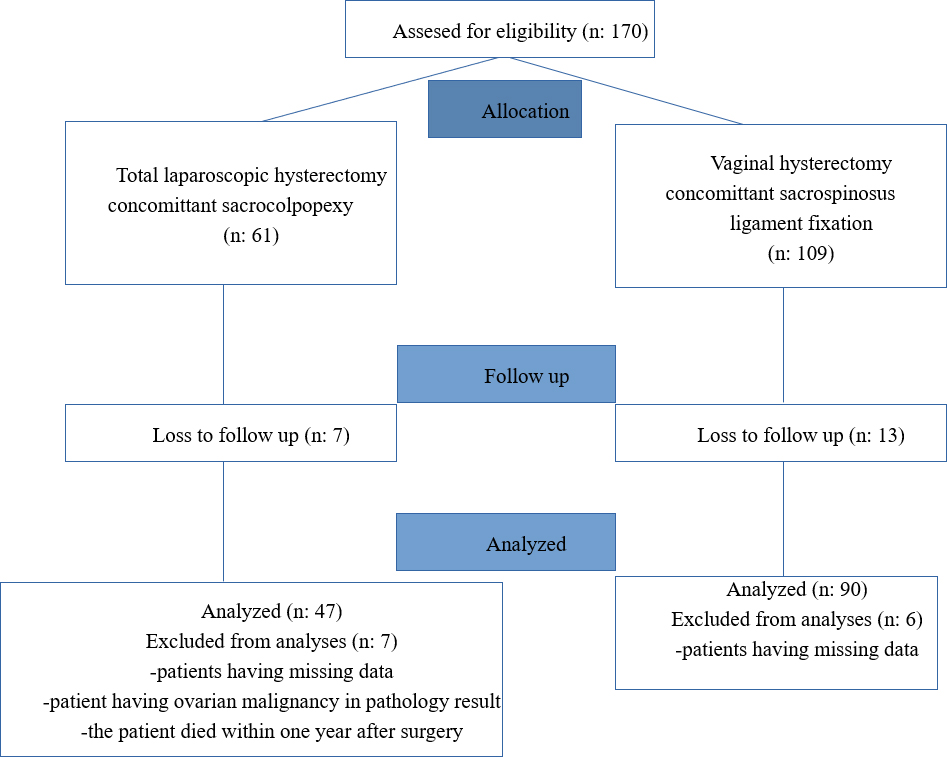 Fig. 1.
Fig. 1.Flow chart of patients who underwent prolapse surgery with concomitant vaginal or laparoscopic hysterectomy.
| TLH + SCP (n = 47) | VAH + SLF (n = 90) | p-value* | |||
|---|---|---|---|---|---|
| mean | Standard deviation | mean | Standard deviation | ||
| Age | 53.47 | 10.54 | 61.89 | 10.26 | 0.946 |
| Parity | 3.98 | 2.28 | 4.14 | 2.43 | 0.431 |
| BMI | 24.38 | 2.08 | 25.2 | 2.48 | 0.168 |
*p
| TLH + SCP | VAH + SLF | p value | ||||
|---|---|---|---|---|---|---|
| n = 47 | % | n = 90 | % | |||
| Smoking | Yes | 6 | 12.8 | 14 | 15.6 | 0.661 |
| No | 41 | 87.2 | 76 | 84.4 | ||
| Menopause status | Yes | 36 | 76.6 | 78 | 86.7 | 0.134 |
| No | 11 | 23.4 | 12 | 13.3 | ||
| Chronic disease | No | 25 | 53.2 | 37 | 41.1 | 0.004* |
| Hypertension | 11 | 23.4 | 21 | 23.3 | ||
| Diabetes mellitus | 5 | 10.5 | 6 | 6.7 | ||
| Multiple chronic diseases | 6 | 12.9 | 26 | 28.9 | ||
| Type of labor | Vaginal | 40 | 85.1 | 78 | 86.7 | 0.621 |
| C/S | 5 | 24.9 | 12 | 13.3 | ||
| POP-Q C point preoperative | 2.77 | 0.729 | 2.99 | 0.679 | 0.057 | |
*p
Perioperative and postoperative variables were presented for both groups (Table 3). The study showed a statistically significant difference between both groups
regarding the length of surgery. The operation time was significantly shorter in
the VAH + SLF group compared to the TLH + SCP group (TLH + SCP 108.3
| TLH + SCP (n = 47) | VAH + SLF (n = 90) | p value | |||
|---|---|---|---|---|---|
| mean | Standard deviation | mean | Standard deviation | ||
| Operating time (minutes) | 108.3 | 17.85 | 94.17 | 11.99 | 0.037* |
| Estimated Blood loss (milliliters) | 96.60 | 57.76 | 139.50 | 69.02 | 0.038* |
| Preoperative Hemoglobin mg/dL | 12.92 | 1.27 | 12.98 | 1.21 | 0.665 |
| Postoperative Hemoglobin mg/dL | 11.36 | 1.25 | 10.02 | 1.38 | 0.254 |
| Hospital stay (days) | 3.26 | 1.66 | 2.42 | 0.76 | 0.057 |
| Return to Daily Activity (days) | 27.89 | 1.92 | 22.64 | 2.17 | 0.997 |
| Postoperative 6th-hour VAS value | 6.83 | 0.99 | 5.16 | 0.63 | 0.001* |
| Postoperative 48th-hour VAS value | 2.19 | 0.39 | 1.86 | 0.53 | 0.239 |
| POP-Q C point postoperative | –6.20 | 1.08 | –6.09 | 1.06 | 0.607 |
*p
| TLH+ SCP (n = 47) | VAH + SLF (n = 90) | p value | ||||
|---|---|---|---|---|---|---|
| mean | Standard deviation | mean | Standard deviation | |||
| P-QoL score | Preoperative | 3.17 | 0.64 | 3.14 | 0.65 | 0.807 |
| Postoperative 30th-day | 0.60 | 0.65 | 0.68 | 0.70 | 0.547 | |
| Postoperative 6th-month | 0.68 | 0.70 | 0.59 | 0.65 | 0.533 | |
| Postoperative 12th-month | 0.66 | 0.61 | 0.87 | 0.66 | 0.144 | |
| PISQ-12 score | Preoperative | 26.64 | 2.50 | 26.57 | 2.48 | 0.932 |
| Postoperative 30th-day | 6.94 | 2.15 | 6.89 | 2.14 | 0.919 | |
| Postoperative 6th-month | 7.25 | 2.15 | 7.25 | 2.15 | 0.068 | |
| Postoperative 12th-month | 9.74 | 4.07 | 10.89 | 2.52 | 0.0001* | |
*p
Table 5 presents intraoperative and postoperative complications. Although complication rates differed in both groups, major complication rates were lower in the TLH + SCP group (p = 0.015). In the VAH + SLF group, one patient needed a blood transfusion due to postoperative cuff hematoma, and one patient experienced bladder injury. In the TLH + SCP group, one patient experienced bowel injury intraoperatively without needing a colostomy. Additionally, one patient had bleeding from the lower segment of the uterine artery that needed re-laparotomy and massive blood transfusion. Lastly, one patient needed a blood transfusion due to cuff hematoma.
| TLH + SCP | VAH + SLF | p value | ||||
|---|---|---|---|---|---|---|
| n = 47 | % | n = 90 | % | |||
| Relapse within one year postoperatively | 0 | 0 | 2 | 2.22 | 0.038* | |
| Minor complications | No | 42 | 89.36 | 85 | 94.44 | 0.360 |
| Post-operative fever | 3 | 6.38 | 0 | 0 | ||
| Cuff Hematoma | 0 | 0 | 2 | 2.22 | ||
| Vault infection | 0 | 0 | 1 | 1.11 | ||
| Urinary tract infection | 0 | 0 | 1 | 1.11 | ||
| Mesh or suture erosion | 1 | 2.13 | 0 | 0 | ||
| Ileus | 1 | 2.13 | 0 | 0 | ||
| Neural trap | 0 | 0 | 1 | 1.11 | ||
| Major complications | No | 44 | 93.62 | 88 | 97.78 | 0.015* |
| Bladder injury | 0 | 0 | 1 | 1.11 | ||
| Relaparotomy due to bleeding | 1 | 2.13 | 0 | 0 | ||
| Bowel injury | 1 | 2.13 | 0 | 0 | ||
| Hemorrhage/Hematoma (blood transfusion) | 1 | 2.13 | 1 | 1.11 | ||
*p
Both groups showed the same success rates, where all patients had stage one or
less prolapse (point C is
In our study, we did not detect de novo urgency or any other type of urinary incontinence after the operations we performed in the one-year follow-up of the patients.
We performed multivariable analyzes of age, menopausal status, chronic disease,
mode of delivery, and parity, among the dependent variables of the cases included
in the study. Our study found that the effects of these dependent variables were
statistically significant in the choice of surgical procedure in patients with
POP-Q 2 and below, with pelvic organ prolapse (Table 6, p = 0.002).
Among these dependent variables, we found that the most crucial parameter for
this effect was the age of the subjects (Table 7, p
| Value | F | Hypothesis df | Error df | p value | Partial Eta Squared | ||
|---|---|---|---|---|---|---|---|
| Groups | Pillai’s Trace | 0.135 | 4.097 | 5 | 131 | 0.002 | 0.135 |
| Wilks’ Lambda | 0.865 | 4.097 | 5 | 131 | 0.002* | 0.135 | |
| Hotelling’s Trace | 0.156 | 4.097 | 5 | 131 | 0.002 | 0.135 | |
| Roy’s Largest Root | 0.156 | 4.097 | 5 | 131 | 0.002 | 0.135 | |
*p-value
| Source | Dependent Variable | Type III Sum of Squares | df | Mean Square | F | p value | Partial Eta Squared |
|---|---|---|---|---|---|---|---|
| Groups | Age | 2189.409 | 1 | 2189.409 | 20.414 | 0.0001* | 0.131 |
| Parity | 0.848 | 1 | 0.848 | 0.149 | 0.700 | 0.001 | |
| Chronic diseases | 0.451 | 1 | 0.451 | 1.816 | 0.180 | 0.013 | |
| Type of labor | 0.008 | 1 | 0.008 | 0.062 | 0.804 | 0.0001 | |
| Menopause status | 0.313 | 1 | 0.313 | 2.246 | 0.136 | 0.016 |
*p-value
The SCP operation has been considered a gold standard treatment option for patients with POP due to its lower relapse rate than other surgical options. However, the vaginal route can be considered by physicians due to natural orifice usage and positional advantage for advanced POP. In the literature, there is not enough evidence about the most suitable surgical technique for patients with POP-Q 2 and above to avoid vaginal cuff prolapse after a hysterectomy. Although it is widely believed that SCP is curatively superior, in our opinion, the optimal surgical technique is still to be decided. In addition, although it is an enigma which operation will be performed in which case, it is understood that the age of the cases, one of the dependent variables in our study, is effective in the choice of surgical procedure. In this context, we found no study with similar results in the literature affecting surgical choice.
This study did not show a statistically significant difference in demographic parameters between the two groups, except for chronic diseases. In the literature, no statistical difference has been shown regarding chronic diseases. The fact that the mean age of the VAH + SLF group is higher than that of the TLH + SCP group supports that the probability of experiencing a chronic disease may increase as age progresses.
Despite longer operative times in the TLH + SCP group, which is consistent with the literature [22, 23], lesser operative blood loss was seen in the laparoscopic group compared with the vaginal approach. The reason for this time difference was the long pre-intervention preparations and the need to work with various surgical instruments in the laparoscopic approach. While the same ligament is held with a clamp to be cut and tied in the vaginal approach, many technical steps, such as the assistant surgeon using the telescope to see the same ligament laparoscopically, showing the ligament at the appropriate angle, asking the nurse for the appropriate instrument for traction, and inserting it through the trocar, all increase the length of the operation. While most patients easily tolerate the position required for VAH, some patients do not tolerate the position in cases such as increased intra-abdominal pressure utilized in the laparoscopic approach, and the patient’s ventilation is improved by using reverse Trendelenburg. Although studies in the literature detected no difference in blood loss during vaginal or laparoscopic approach [22, 23, 24, 25], we found a statistically significant difference among both cohorts favoring the TLH + SCP group. We believe that bleeding was less in the TLH + SCP group since vessel sealing in laparoscopic operations are performed more slowly. Compared with open techniques, the bleeding area can be better visualized, and the excess bleeding can be detected and resolved with early intervention. This can be more difficult when performing vaginal surgery.
Unlike other studies, we compared the VAS scores of the patients postoperative at 6 and 48 hours. The postoperative 6-hour VAS values were higher in the group that underwent TLH + SCP. We believe this difference was higher in the TLH + SCP group for reasons such as laparoscopic entry to the abdomen from at least four different locations, the opening of the planes of the retroperitoneum during laparoscopic hysterectomy, and mesh fixation.
A recent meta-analysis including 4120 cases (five randomized controlled, eight retrospective, and two prospective studies) comparing the effectiveness of vaginal SLF and SCP demonstrated that the recurrence rate was significantly higher in the SLF group [23]. Compatible with this data, various studies have shown that SLF and SCP have similar recurrence rates [26, 27]. Although there are conflicting results in the literature, in our study, 2 cases in the VAH + SLF group developed vaginal vault prolapse (2.2%). In this context, the low incidence of SCP made us think that the strength of the mesh material used in practice ensures better support to the apex than the sutures used at SLF. This results in the vaginal cuff being stabilized at a higher level, which provides lower recurrence rates. Another meta-analysis comparing vaginal or abdominal support in women having uterine prolapse who underwent concomitant hysterectomy showed similar postoperative point C results, supporting this evidence [28].
Thirty-five percent of cases were sexually active. Sexual activity rates did not change during the first year. We attributed this to the advanced age of the patients. In addition, we realized that even though the sagging tissues of patients with POP were corrected in the postoperative period, their sexual activity habits continued. These results also explain the results of surveys used to measure sexual function. Although similar cure rates, sexual activity, and quality of life scores were noted between both cohorts, we found deterioration in the PISQ-12 and P-QoL scores after the 30th day, 6th month, and 12th month postoperatively. Moreover, despite lower PISQ-12 and P-QoL scores on the 30th day postoperatively, the 6th month and 1st-year survey scores improved gradually but were still lower than pre-operative scores. The low PISQ-12 and P-QoL scores on the 30th day are predictable due to the healing process following surgery. However, low survey scores in the sixth month and first year differ from the expected ones. The controversy of our results with the literature is related to the fact that we included more older patients having higher rates of chronic diseases. Accordingly, chronic diseases may affect patients’ quality of life and sexual activities as an independent factor which might open a new debate on this topic. We found statistical significance only on the postoperative 1st year PISQ-12 scores among both cohorts in favor of VAH + SLF. The possible reason for this might be the use of mesh at the SCP procedure, which gives rise to dyspareunia. Fayyad et al. [29] state that there is a 10% chance that women may develop new-onset dyspareunia after LSC. Patients should be informed about this situation prior to surgery.
We classified both groups’ pre-operative and postoperative complications as minor and major. Despite not being statistically significant, when the subheadings under the minor complications were evaluated, one significant complication was seen in each group, which is consistent with the literature [17, 22]. In the TLH + SCP group, one patient experienced mesh exposure, while in the VAH + SLF group, neural trap complications occurred. Conversely, some studies reported higher rates of postoperative fever in the SLF group which is contrary to our results. We found higher postoperative fever rates in the laparoscopic approach, but it was not statistically significant. We also subtitled the major complications, for which we found a statistically significant difference between the SCP and SLF groups. Previous studies have demonstrated similar complication rates between SCP and SLF [22, 23]. However, the small sample size involved in the analysis of our study makes further controlled studies necessary.
As evidenced in the literature, especially in postmenopausal women, the blood flow of the region increases with the effect of estrogen, making the atrophic tissues more lively [30]. Thus, it becomes easier to distinguish tissue planes, making dissection more possible. As mentioned in some studies in the literature, the quality of life increases after surgery [30]. In this context, we can say that postoperative recovery is faster based on our clinical experience.
Although the procedures applied in our study were performed by surgeons who had completed the learning curve, the difference in surgical skills of those who operated suggests that this may affect surgical success. While the data we obtained is reliable, it is less targeted than data collected in a prospective study. In addition, the number of cases included in the study is limited. Although this study is valuable for comparing two different approaches for pelvic support after a hysterectomy, the retrospective nature of our study is a limitation. There is a need for further studies to determine the ideal approach for pelvic support because of the lack of studies on this topic. Also, the shorter (12-month) observation period for patients regarding subjective and objective outcomes is a limitation. Lastly, the average age of our population sample is higher compared to other studies, making it difficult to decide whether the overall satisfaction deteriorated due to surgery or chronic diseases. However, the strengths of our study include an experienced surgical team with the same operators performing the surgeries, a homogenous study population including patients having only POP, using Turkish validated questionnaires for subjective outcomes, pre- and post-operative POP-Q point C scores for objective outcomes, and a large sample size.
It seems impossible to determine the ideal suspension operation due to too many variables. Based on this study, while SCP may be an option to keep the vaginal cuff in an anatomically appropriate position, SLF may be the best solution given mesh erosion, cost-effectiveness, operative time, re-laparotomy, and gastrointestinal and bladder complications. As can be understood from all these results, we should always suspend the cuff to avoid vaginal cuff prolapse in cases with POP-Q 2 and above POP.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
ÖÜ conceptualized and designed the study; ÖÜ, OK conducted statistical analysis and wrote the article; ÖÜ, OK contributed to the interpretation of results; ÖÜ, OK provided final approval and had the manuscript ready for publication. Both authors contributed to editorial changes in the manuscript. Both authors read and approved the final manuscript. Both authors have participated sufficiently in the work to take public responsibility for appropriate portions of the content and agreed to be accountable for all aspects of the work in ensuring that questions related to its accuracy or integrity.
The ethical committee of Istanbul Kanuni Sultan Süleyman Training and Research Hospital accepted this study, which was carried out in compliance with the Declaration of Helsinki as revised in 2013 (Application No. KAEK 2022.05.118). Due to the study’s retrospective character, the need for patient consent for both participation and publishing was waived. All patients provided written, fully informed consent before surgery.
Thanks to all the peer reviewers for their opinions and suggestions. Thanks to Ejear English editing service for the premium English editing.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.