1 Department of Obstetrics and Gynecology, Liverpool Hospital, 2170 Sydney, NSW, Australia
2 Department of Radiology, Liverpool Hospital, 2170 Sydney, NSW, Australia
§Current address: Department of Obstetrics and Gynecology,
Abstract
Background: Placenta accreta spectrum (PAS) disorder refers to
pathologic adherence of the placenta and presents multiple perinatal challenges,
accounting for between 30–50% of emergency peripartum hysterectomies. Accurate
prenatal diagnosis allows multidisciplinary management and delivery at centres
with experience and has been shown to improve perinatal outcomes. This study aims
to analyse the results of implementing different strategies across the years on
the diagnosis and management of PAS in a tertiary Australian hospital (Liverpool
Hospital) including: the use of magnetic resonance imaging (MRI) and the benefits
of the use of iliac artery balloons and ureteric stents. Secondary objectives
include analysis of the risk factors and outcomes. Methods:
Retrospective case series of 34 pregnancies complicated by PAS disorders,
diagnosed between 2004 and 2020, and delivered at Liverpool Hospital. Descriptive
and analytic study (with a significance level of p
Keywords
- placenta accreta
- morbidly adherent placenta
- morbid adherent placenta
- placenta accreta spectrum
- adherent placenta
Placenta accreta spectrum (PAS) disorder refers to the range of pathologic adherence of the placenta, including placenta accreta, increta and percreta [1]. These occur with abnormal trophoblastic implantation through the decidua of the endometrium, myometrium or beyond the serosa of the uterus, respectively [2, 3]. The overall prevalence of placenta accreta disorders has been increasing, likely related to increased risk factors, especially the increased rate of caesarean deliveries [2]. PAS presents multiple perinatal challenges and serious surgical risks including catastrophic perinatal haemorrhage, accounting for between one-third and one-half of emergency peripartum hysterectomies [2, 4]. Accurate prenatal diagnosis of PAS disorders, allowing multidisciplinary management at centres with experience at the time of delivery, has been shown to improve maternal and fetal outcomes [1, 2, 3, 4].
The classical risk factors for PAS disorders are placenta previa associated with a previous caesarean section [2, 4]. In a systematic review, the rate of placenta accreta spectrum increased from 0.3% in women with one previous caesarean delivery to 6.74% for women with five or more caesarean deliveries [5]. In women diagnosed with placenta praevia and no prior caesarean deliveries the rate of PAS is around 3%. In the setting of a placenta praevia and one or more previous caesarean deliveries, the risk of placenta accreta spectrum is dramatically increased: reported as 3%, 11%, 40%, 61% and 67%, for the first, second, third, fourth and fifth or more caesarean respectively [6, 7, 8]. Surprisingly, the PACCRETA study from 176 hospitals in France (n = 249 cases) found that half of the cases did not have the classical combination of risk factors and only 17% of these were diagnosed antenatally [9].
Antenatal diagnosis of placenta accreta spectrum is important because outcomes are optimised when delivery occurs at a high-level maternal care facility before the onset of labor or bleeding [2, 3, 4, 6]. Current prenatal diagnosis is based on operator-dependent sonographic findings using two and three-dimensional (2D/3D) and colour Doppler imaging. These findings may be present as early as the first trimester, although most cases are diagnosed in the second and third trimesters [10, 11, 12, 13]. Throughout the literature the reported overall sensitivity of ultrasound imaging ranges widely from 50% to 90% [10], and expert panels have been publishing different consensus statements that aim to standardise the diagnosis of PAS [10].
Magnetic resonance imaging (MRI) has also been suggested as a helpful tool for PAS disorder diagnosis [11], however, it has still not clearly demonstrated a significant improvement in the pregnancy management and perinatal outcomes. Currently it is only recommended as an adjunct to ultrasound imaging by many international societies (especially for posteriorly located placentas and to evaluate parametrial involvement) [1, 2, 3]. Nonetheless, MRI has a high predictive accuracy in assessing both the depth and topography of placental implantation and our experience suggests that it may be an important additional imaging technique for the prenatal diagnosis in cases of PAS disorder when ultrasound is inconclusive [11, 14, 15].
Ideally, PAS management should involve a standardised approach with a multidisciplinary care team experienced in managing PAS disorders. American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) recommend that these patients receive at least level III (subspecialty) or higher care—including a 24-hour available medical team with appropriate experience in managing complex maternal and obstetric complications [2].
The overall aim of our study is to understand the impact of the implementation of new strategies over the years on the diagnosis and management of PAS at an Australian tertiary hospital (Liverpool Hospital, NSW). The primary objectives are to analyse the use of MRI in the prenatal diagnosis of PAS, to evaluate the impact of the use of iliac artery balloons in the total blood loss and operative time and the use of ureteric stents on urological complications.
Secondary objectives include: analysing the risk factors of patients with PAS disorders, describing the rate of intra- and post-operative complications and comparing the gestational age of the cases delivered emergently versus electively.
We hope that this study helps us to understand our strengths and limitations in antenatal diagnosis and current management of PAS disorders so that we can improve our clinical practice and the overall quality of care offered to patients.
A retrospective, descriptive and analytic, case series of suspected/diagnosed PAS disorders delivered at Liverpool Hospital between 2004 and 2020 (n = 34 pregnancies).
Liverpool Hospital is a tertiary hospital in Australia, and is the referral centre for all complex pregnancies and deliveries from the South West Sydney Local Health District (total of around 12,000 deliveries/year). Since 2004, a dedicated and experienced team has been responsible for the management of antenatally suspected PAS cases to improve perinatal outcomes. Ultrasound, ideally performed or reviewed by a Maternal Medicine Specialist, has been used for PAS prenatal diagnosis but since 2007, MRI started to be used as an additional diagnostic tool—especially for cases of posteriorly located placentas, parametrial involvement or inconclusive ultrasound. When PAS is suspected, the usual approach involves early referral and review by a multidisciplinary team to optimise pre-operative patient management. The relevant specialities would often include, Obstetrician/gynaecology services, anaesthesia, haematology, interventional radiology and urology. Delivery is planned based on the PAS extension, patient symptoms and family planning. Caesarean hysterectomy is the most commonly performed procedure but conservative approaches are also discussed individually if fertility preservation is desired.
Since 2011, the pre-operative insertion of iliac artery balloons (by interventional radiology—IR) has been used to reduce pelvic blood flow during complex PAS surgery. In earlier cases the balloon catheters were placed in the internal iliac arteries and later in the common iliac arteries. The balloon inflation starts while the uterine incision is closed and the inflation time is controlled by the IR team.
Routine pre-operative cystoscopy followed by insertion of ureteric stents by the urology team was also introduced in 2011 for the most complex PAS cases.
In this study, the proposed research variables included the risk factors for PAS, the ultrasound and MRI findings, the delivery details, intra-operative findings, post-operative complications and the histopathological results.
For data analysis, the initial database was completed in Microsoft® Excel (Microsoft Excel for Mac, version 16.61.1 (22052000), 2019, Redmond, WA, USA) with exclusion of cases with incomplete data. The data was converted to a numeric format and exported to SPSS software (Windows version 26.0, IBM Corp., Armonk, NY, USA) for statistical analyses.
Continuous variables were assessed for normality and a descriptive univariate
analysis was performed: frequencies for nominal variables, frequencies and media
for ordinal variables, mean and standard deviation (SD) for quantitative
variables. Independent Samples Mann–Whitney U-test and Kruskal-Wallis
test were used for comparative analysis. A significance level of p
The study was approved by the Research Ethics and Governance Information System (REGIS) with the identifier 2021/PID03717.
Between 2004 and 2020, there were 56,624 deliveries at Liverpool Hospital. During this period, 34 pregnant women were diagnosed antenatally with PAS disorders (incidence of 0.6/1000 deliveries).
Thirty-two patients had singleton pregnancies and two had twin pregnancies (Table 1).
| Characteristics | N | Mean (min–max) | Median | SD |
|---|---|---|---|---|
| Age (y) | 34 | 34.5 (25–46) | 34.5 | 5.73 |
| BMI (kg/m |
30 | 28.5 (19–55) | 26.2 | 8.68 |
| Parity | 33 | 2.6 (1–8) | 2 | 1.87 |
| Interval from last CS (y) | 27 | 3.9 (1–12) | 3 | 2.98 |
| N | % | |||
| Ethnicity | White | 27 | 84.4 | |
| Asian | 3 | 9.4 | ||
| Black/African/Caribbean | 2 | 6.3 | ||
| Obesity (BMI |
10 | 33.3 | ||
| Nr previous uterine surgeries | Caesareans | % | ||
| - 0 | 7 | 20.6 | ||
| - 1 | 11 | 32.4 | ||
| - 2 | 9 | 26.5 | ||
| - 3 | 4 | 11.8 | ||
| - 4 | 3 | 8.8 | ||
| D&C | 16 | 47.1 | ||
| Myomectomies | 1 | 2.9 | ||
| IVF | 1 | 2.9 | ||
| Placenta praevia | Anterior | 31 | 91.2 | |
| Posterior | 3 | 8.8 | ||
| APH | 17 | 50.0 | ||
| Twins | 2 | 5.8 | ||
BMI, body mass index; CS, caesarean section; D&C, dilatation & curettage; IVF, in vitro fertilization; APH, antepartum haemorrhage; N, total number of observations; SD, standard deviation.
In this cohort, 27 cases (79%) had previous caesarean sections (32.4% had 1, 26.5% had 2, 11.8% had 3 and 8.8% had 4 previous caesareans). From the 7 patients that had no previous history of caesarean section, 4 had a history of cervical dilatation and uterine curettage and 3 had no previous uterine surgeries (Table 1).
In relation to other risk factors, the morphology scan described a placenta previa in all cases, located anteriorly in most of the cases (91.2%). Only 1 case was documented as an in vitro fertilization (IVF) pregnancy (Table 1). Admission for antepartum haemorrhage (APH) was documented in 50% of the cases (Table 1).
Regarding delivery, twenty-three patients had an elective delivery and eleven had an emergency delivery due to APH or preterm labor (PTL).
66.7% of the cases had a documented management plan for delivery (conservative in 66.1% and caesarean-hysterectomy in 33.3%) after review by a multidisciplinary team (Table 2).
| Delivery | N | % | |
|---|---|---|---|
| Type of delivery | Elective | 23 | 67.6 |
| Emergency | 11 | 32.4 | |
| Planned surgery | Conservative | 16 | 66.7 |
| Hysterectomy | 8 | 33.3 | |
| Preventive measures | Iliac balloons | 20 | 55.5 |
| Ureteric stents | 16 | 44.4 | |
| Primary surgery performed | CS | 3 | 8.8 |
| CS HT with no trial of placental removal | 12 | 35.3 | |
| CS, trial of placental removal, followed by HT | 18 | 52.9 | |
| CS with placenta left in situ | 1 | 2.9 | |
| Additional procedures to control haemorrhage | Nil | 23 | 67.6 |
| Placental bed sutures (PBS) | 4 | 11.8 | |
| PBS + Bakri | 1 | 2.9 | |
| UAE (by IR) | 2 | 5.9 | |
| PBS + Bakri + UAE | 1 | 2.9 | |
| Abdominal packing | 3 | 8.8 | |
| Major complications | Nil | 23 | 67.6 |
| Bladder injury | 7 | 20.6 | |
| IVC thrombosis | 1 | 2.9 | |
| Haemoperitoneum | 2 | 5.9 | |
| Pelvic haematoma | 1 | 2.9 | |
| Mean (min–max) | Median | SD | |
| Operative time | 132 (37–265) | 126 | 47.9 |
| EBL | 2.8 (0.3–10.5) | 2.5 | 2.1 |
| Hb drop | 34 (14–84) | 28 | 18 |
| Nr RBC transfusions | 6 (0–24) | 4 | 6.5 |
CS, caesarean section; HT, hysterectomy; CS HT, caesarean hysterectomy; PBS, placental bed sutures; UAE, uterine artery embolization; IVC, inferior vena cava; EBL, estimated blood loss; Hb, hemoglobin; RBC, red blood cells; N, total number of observations.
Of this cohort, in 18 cases (52.9%), a trial of placental removal was performed but was followed by hysterectomy. In 12 cases (35.3%) the hysterectomy was performed straight after the delivery. 3 cases (8.8%) were managed with a caesarean section (no need for hysterectomy) and the histopathology showed focal accreta in 2 of them and no PAS in the other. In 1 case of placenta percreta, the placenta was left inside the uterus for fertility preservation: collagen with gentamycin were applied to the placenta and bilateral uterine artery embolisation was performed by interventional radiology. Long term antibiotics were given and a weekly review was performed by the operating team. The patient had a subsequent pregnancy 5 years later and lower segment caesarean section and bilateral tubal ligation were performed at that delivery without complications.
In our cohort, the insertion of iliac artery balloons was performed by interventional radiology in 55% of the cases (2 cases in the internal iliac and the others in the common iliac arteries) and ureteric stents were inserted before the main surgery in 44% of the cases. Additional procedures to control haemorrhage (placental bed sutures, Bakri balloon, uterine artery embolisation and abdominal packing) were required in 32.4% of the cases (Table 2).
The average operative time was 132 minutes (min = 37, max = 265) and the mean estimated blood loss (EBL) was 2.8 L (min = 0.3, max = 10.5). The mean hemoglobin drop was 34 g/L and the mean number of units of packed red blood cells given was 6 (min = 0, max = 24).
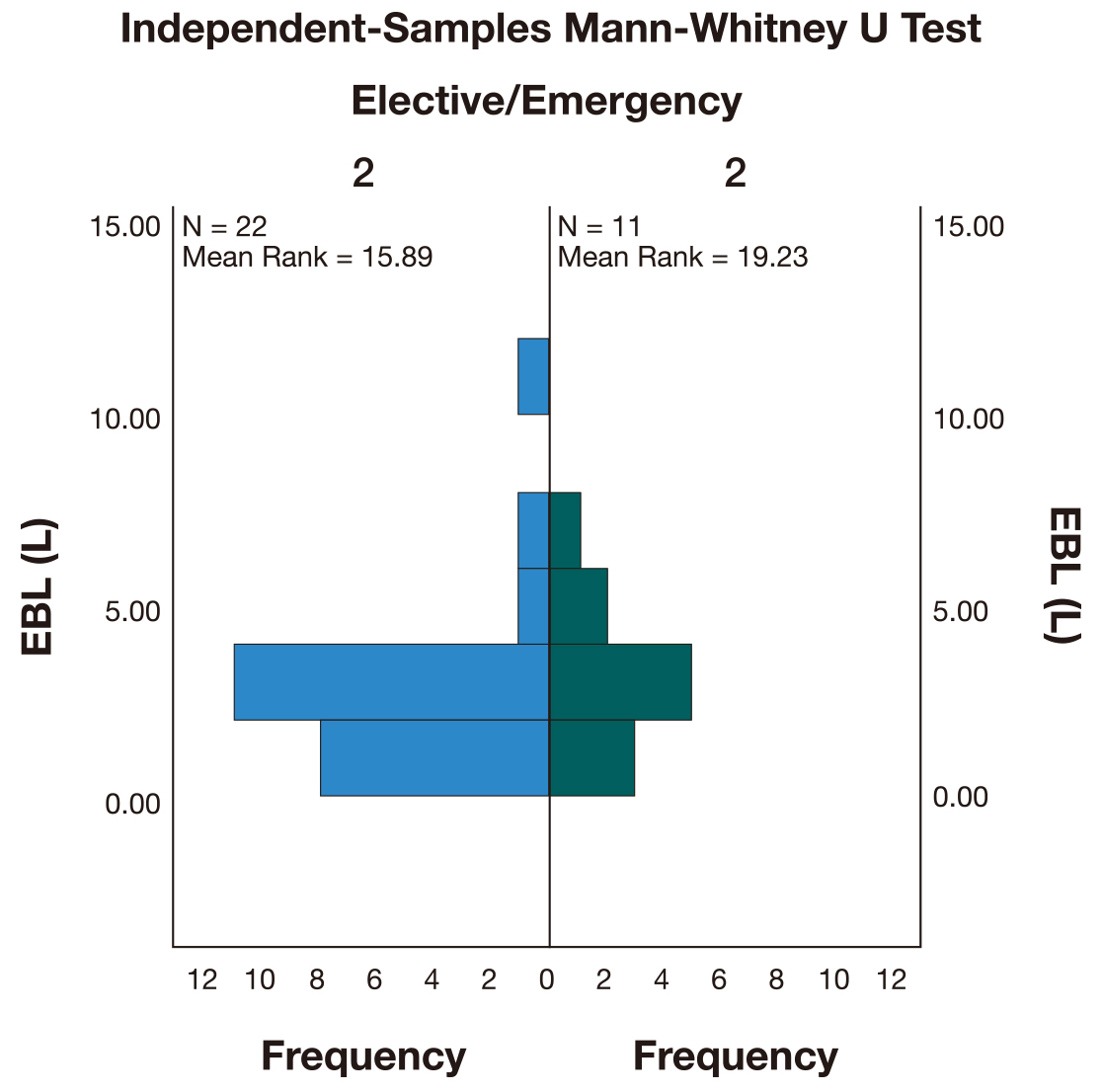
The EBL of the elective procedures (M = 2.5 L) was lower than for emergency procedures (M = 3 L). However, a Mann-Whitney U test (Fig. 1) indicated that this difference was not statistically significant (U = 145,500, p = 0.35).
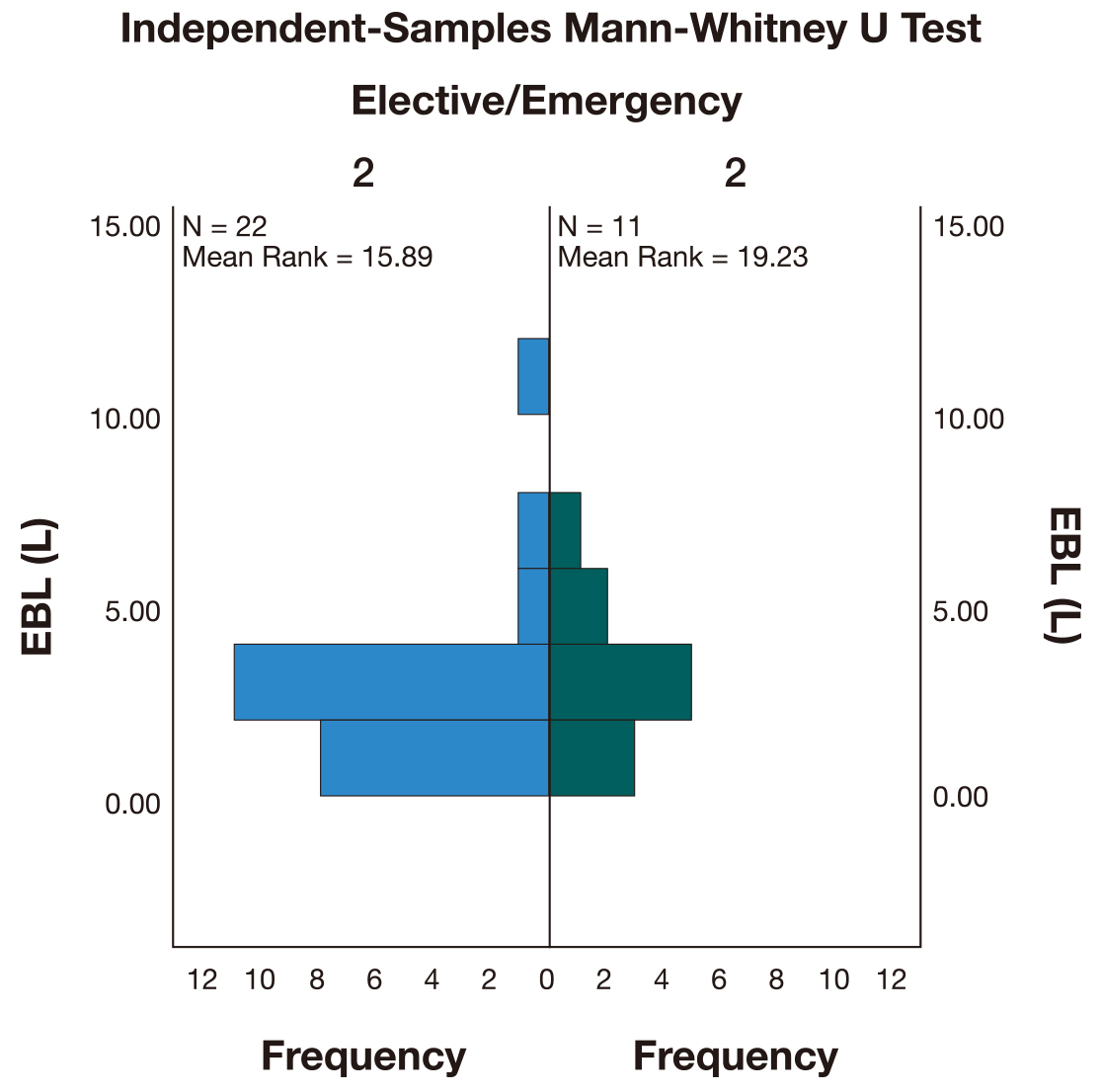 Fig. 1.
Fig. 1.Independent-Samples Mann-Whitney U test comparing the total estimated blood loss (EBL) between elective and emergency procedures.
The incidence of major complications was 32.4%, with urological injury being the most common complication (Table 2).
Post-operatively, a re-look laparotomy for ongoing bleeding was required in 6 cases (Table 3).
| Post-op | N | % | ||
|---|---|---|---|---|
| Admission to ICU | 17 | 50% | ||
| Re-operation | 6 | 17.6% | ||
| Readmission after discharge | 2 | 5.8% | ||
| N | Mean (min–max) | Median | SD | |
| Duration ICU stay (d) | 17 | 2 (1–4) | 2 | 0.8 |
| Duration hospital stay (d) | 34 | 8 (3–17) | 7 | 3.2 |
ICU, intensive care unit; N, total number of observations; SD, standard deviation.
There were 2 readmissions after discharge (Table 3): one of the cases was a woman who had a hysterectomy for placenta percreta complicated by bladder injury and discharged herself against medical advice. She represented a day later with abdominal pain and fever and was treated conservatively with intravenous antibiotics, with good progress. The other case was a readmission for a pelvic hematoma post hysterectomy with bladder injury, also treated conservatively.
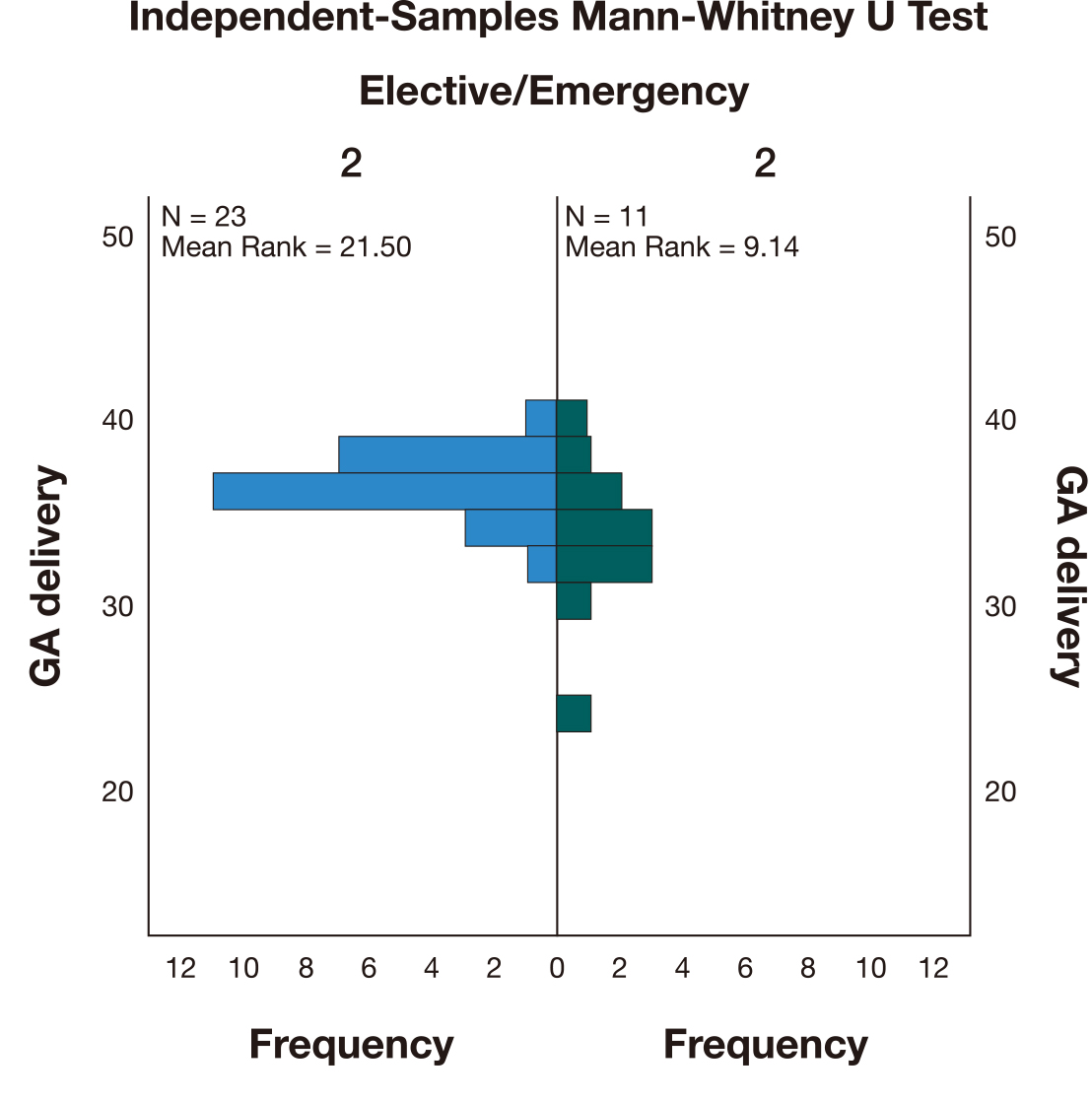
The average gestational age of delivery was 36 weeks. The GA of the elective
procedures (M = 36) was higher than for emergency procedures (M = 33). A
Mann-Whitney U test (Fig. 2) indicated that this difference was statistically
significant (U = 34,500, p
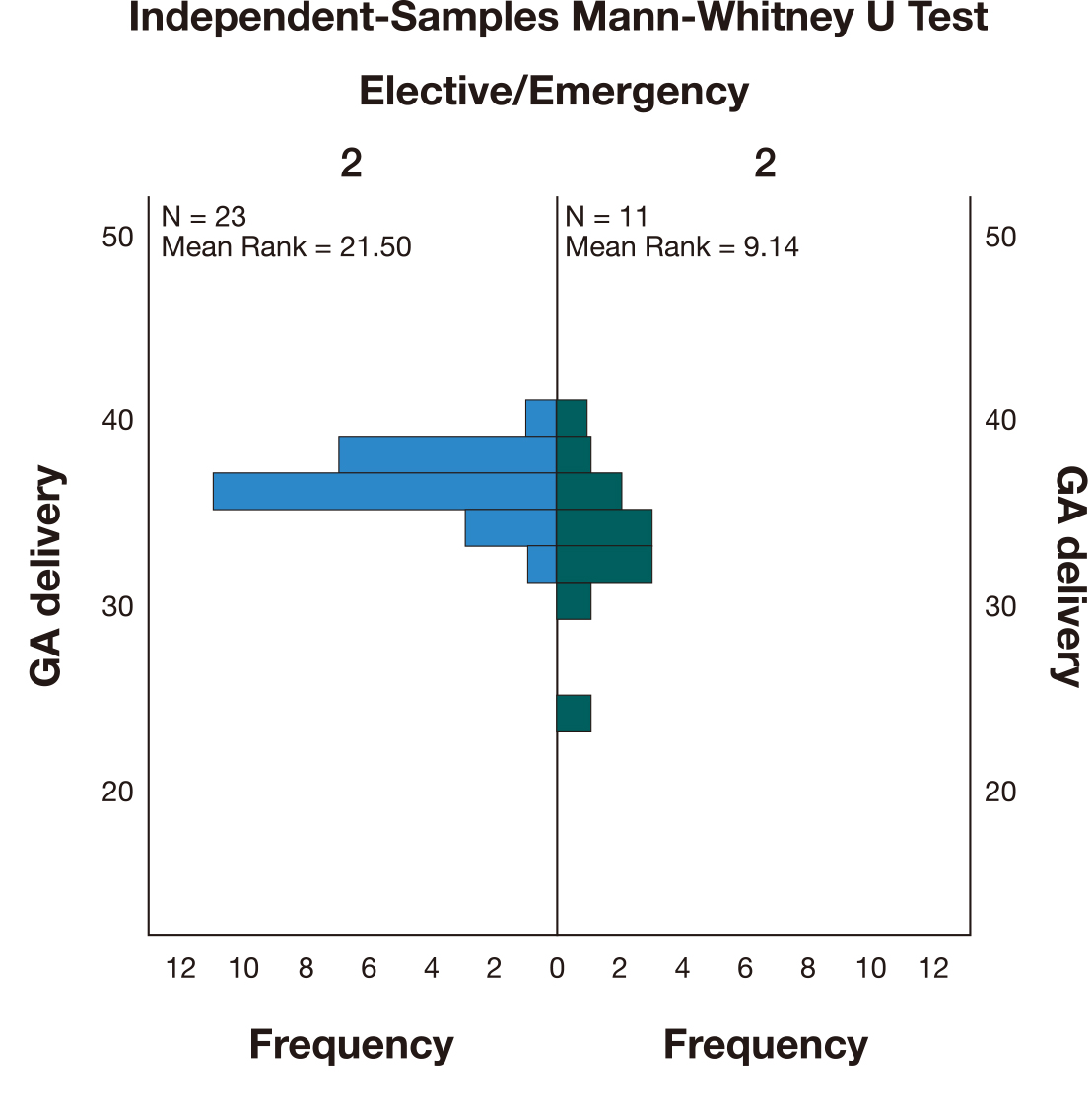 Fig. 2.
Fig. 2.Independent-Samples Mann-Whitney U test comparing the gestational age (GA) at delivery between elective and emergency deliveries.
The mean birthweight was 2398 g and 69.4% of the cases required admission to the neonatal intensive care unit (22 cases due primarily to prematurity and 3 cases with respiratory distress syndrome). There was a neonatal death in a case delivered at 24 weeks (Table 4).
| Newborn | Mean (min–max) | Median | SD |
|---|---|---|---|
| GA delivery (weeks) | 34.8 (24–40) | 36 | 2.9 |
| BW (g) | 2398 (672–3605) | 2378 | 648 |
| N | % | ||
| Admission NICU | 25 | 69.4 | |
| Diagnosis | 72.2 | ||
| Prematurity | 22 | 84.6 | |
| RDS | 3 | 11.5 | |
| NND | 1 | 2.9 | |
GA, gestational age; BW, birthweight; NICU, neonatal intensive care unit; RDS, respiratory distress syndrome; NND, neonatal death; SD, standard deviation.
The ultrasound findings were available for 30 of the 34 cases and were highly suspicious of the diagnosis in 63.3%, inconclusive in 16.7% and normal/no signs of PAS in 20%. MRI was used in 14 cases (when ultrasound was inconclusive or placenta posterior and difficult to see in detail with ultrasound). MRI was only inconclusive in 1 of the cases (Table 5).
| PAS diagnosis | N | % | |
|---|---|---|---|
| US | 30 | 83.3% | |
| No US signs of PAS | 6 | 20.0% | |
| High suspicion | 19 | 63.3% | |
| Inconclusive | 5 | 16.7% | |
| MRI | 14 | 38.9% | |
| High suspicion | 13 | 92.9% | |
| Inconclusive | 1 | 7.1% | |
| Macroscopic (intra-op) | |||
| No PAS | 2 | 5.9% | |
| Accreta | 23 | 67.6% | |
| Increta | 2 | 5.9% | |
| Percreta | 7 | 20.6% | |
| HP | 33 | 97.0% | |
| No PAS | 3 | 9.1% | |
| Accreta | 16 | 48.5% | |
| Increta | 10 | 30.3% | |
| Percreta | 4 | 12.1% | |
PAS, placenta accreta spectrum; US, ultrasound; MRI, magnetic ressonance imaging; HP, histopathology; N, total number.
Intra-operatively, the macroscopic findings were suspicious of PAS in 32 cases (Table 5).
The histopathological (HP) examination confirmed PAS diagnosis in 30 cases (90.9%). From the other 4 cases, 1 had no histopathological result as the placenta was left in situ and in the other 3 cases the diagnosis wasn’t confirmed on histopathology.
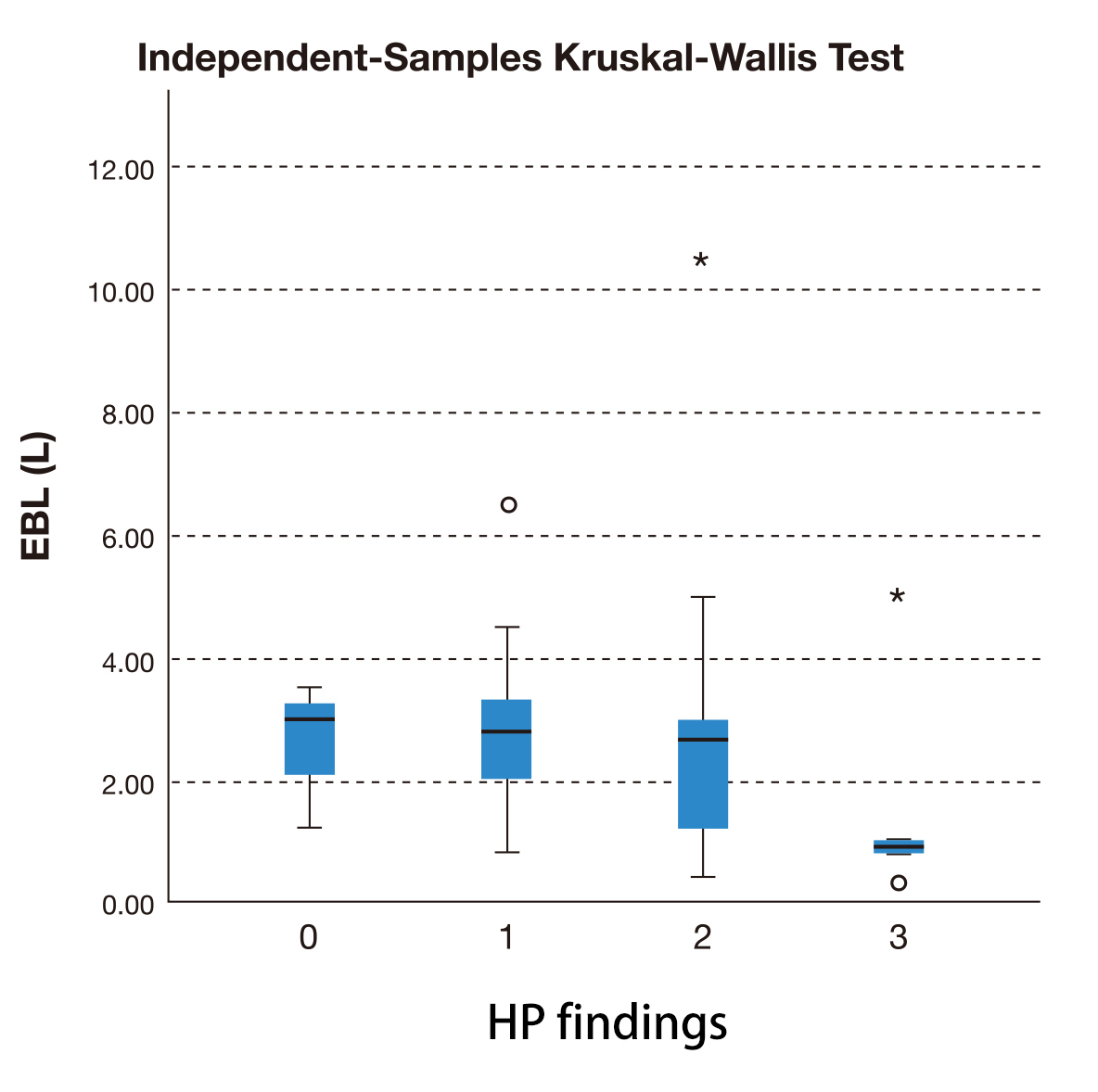
The difference in blood loss of the cases where PAS wasn’t confirmed on histopathology (M = 3 L) and the different grades of PAS—placenta accreta (M = 2.8 L), increta (M = 2.7 L) and percreta (M = 2.5 L)—was not statistically significant (p = 0.27) as represented in Fig. 3.
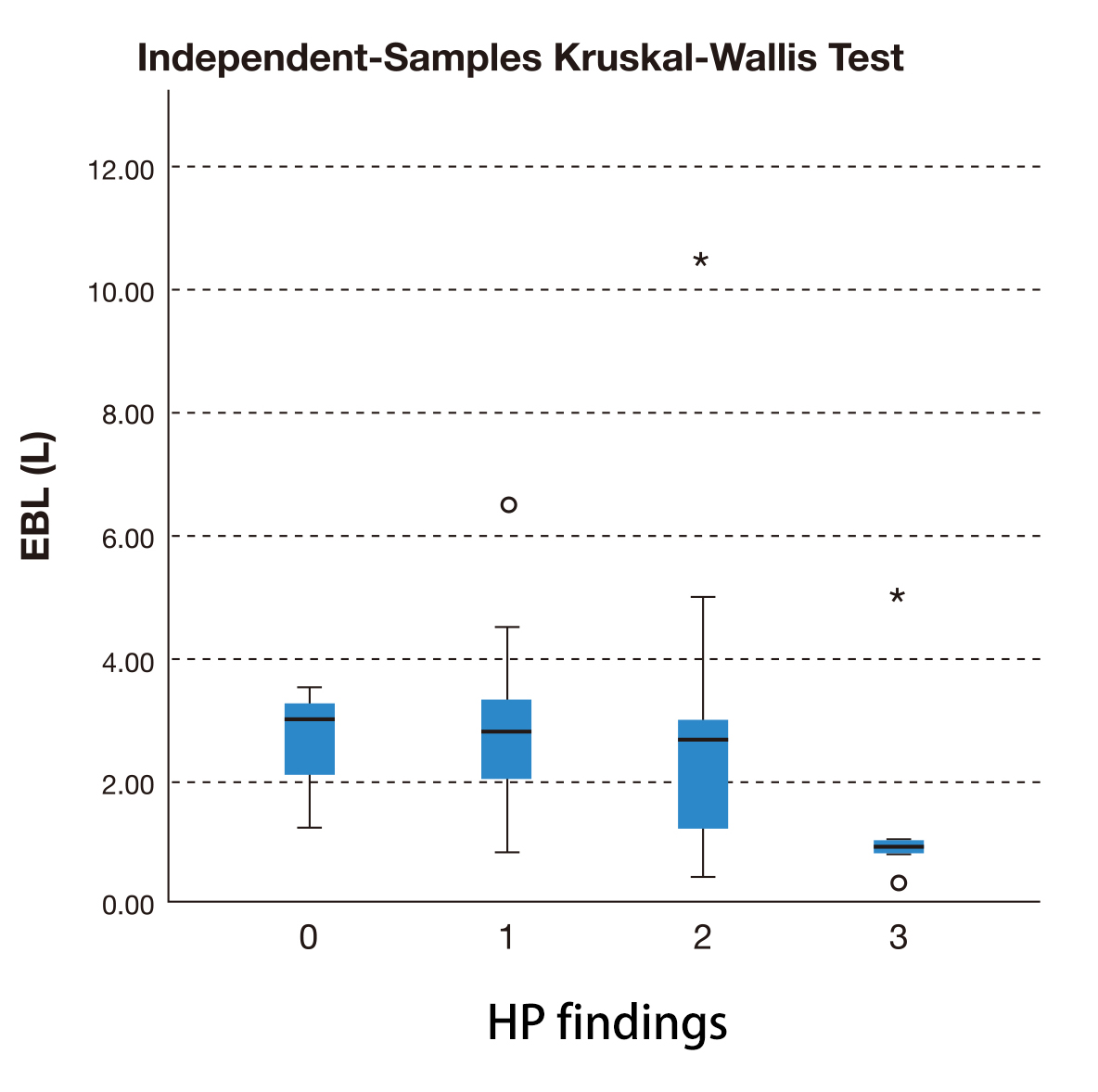 Fig. 3.
Fig. 3.Independent-Samples Kruskal-Wallis test to compare estimated
blood loss (EBL) between placenta not accreta (0), accreta (1), increta (2) and
percreta (3) (confirmed on histopathological examination).
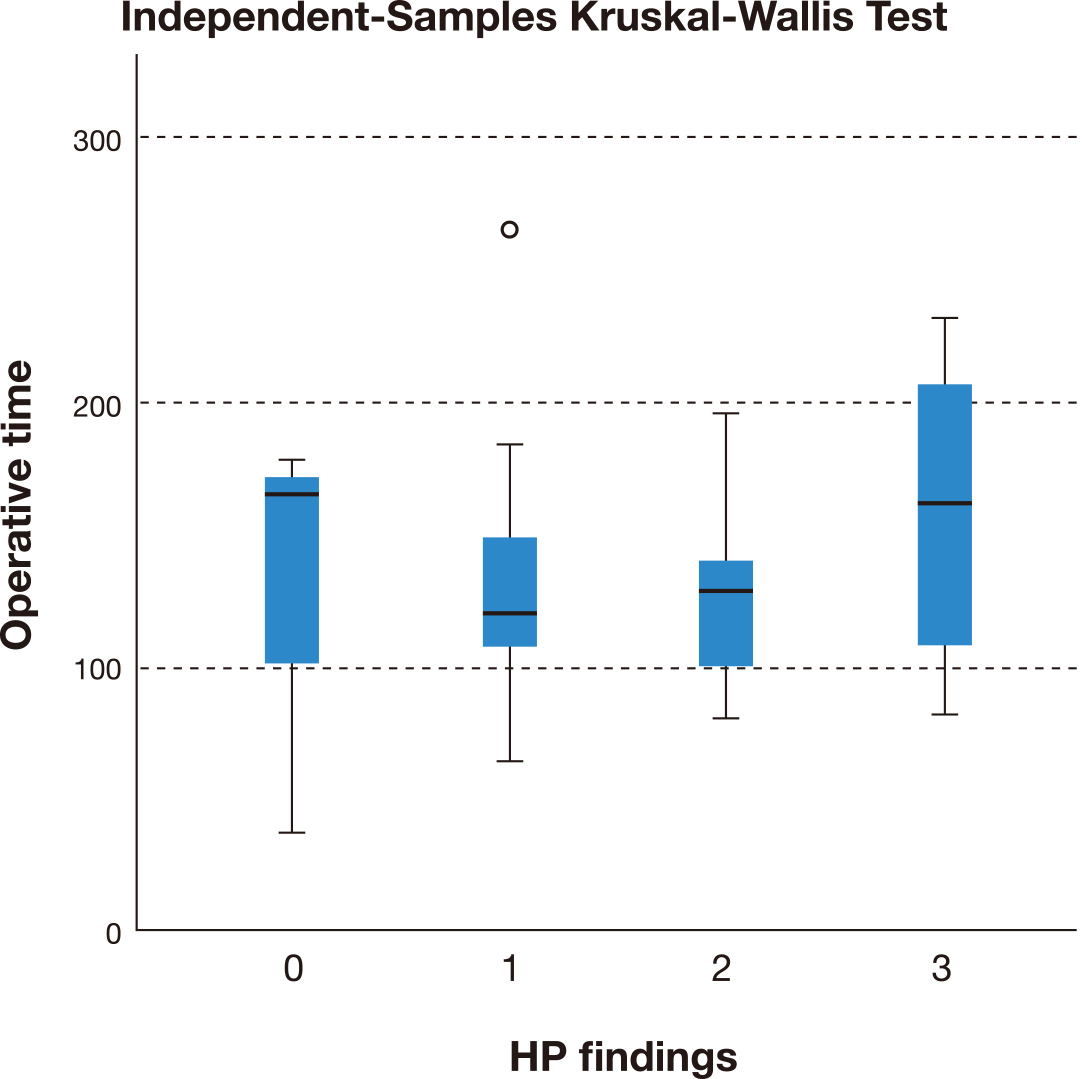
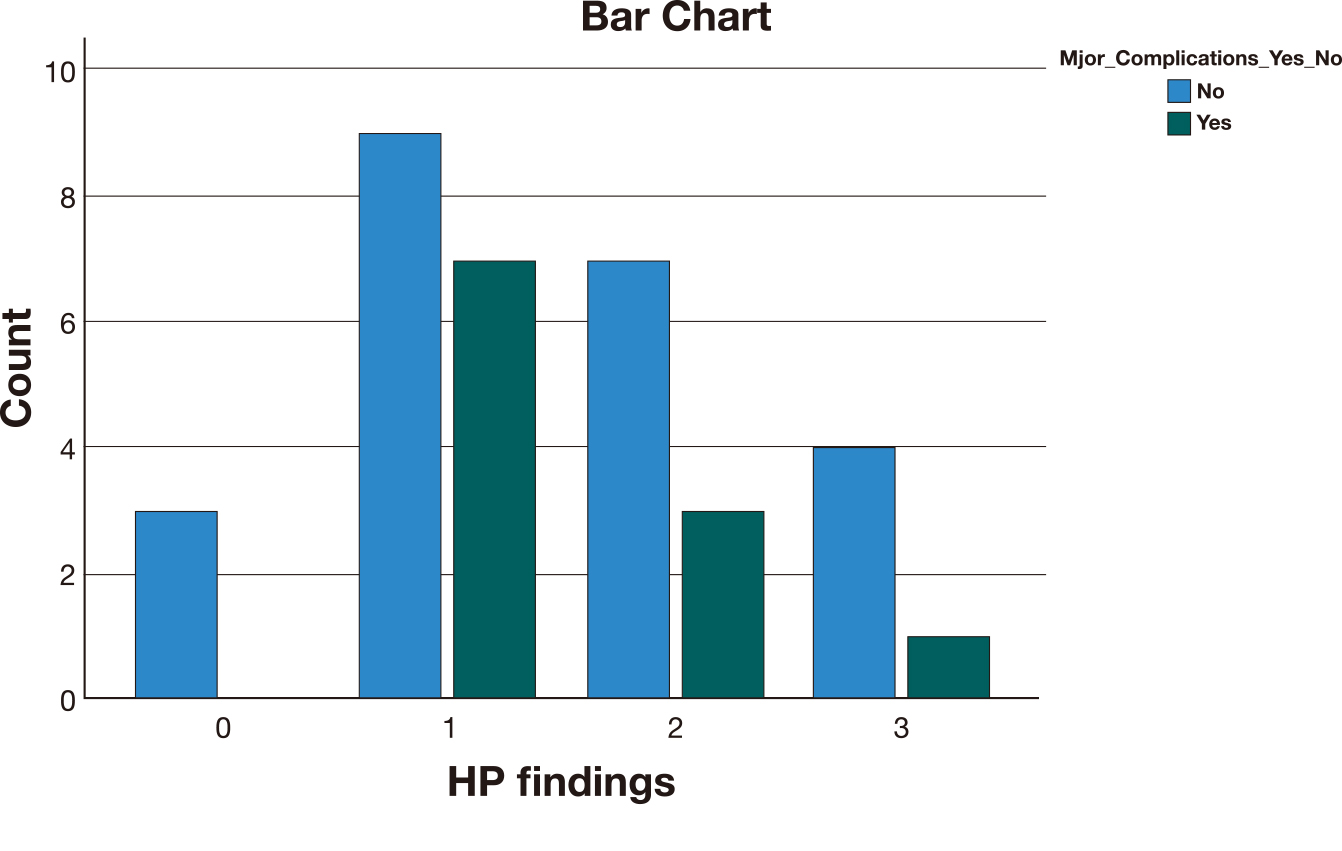
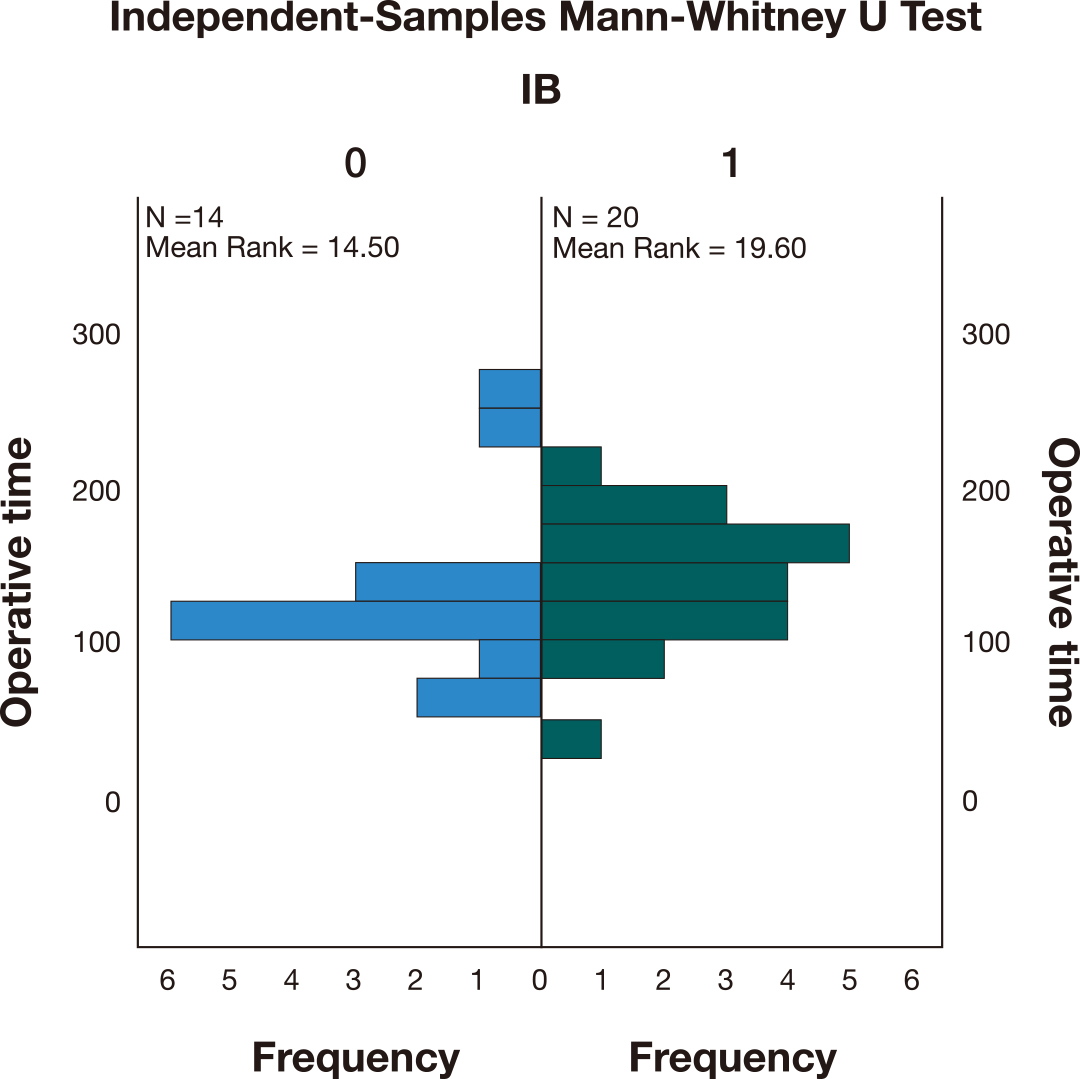
The operative time (Fig. 4) among the different groups of PAS/no PAS and the major complications rate (Fig. 5) were also not statistically different (p = 0.43 and p = 0.78 respectively).
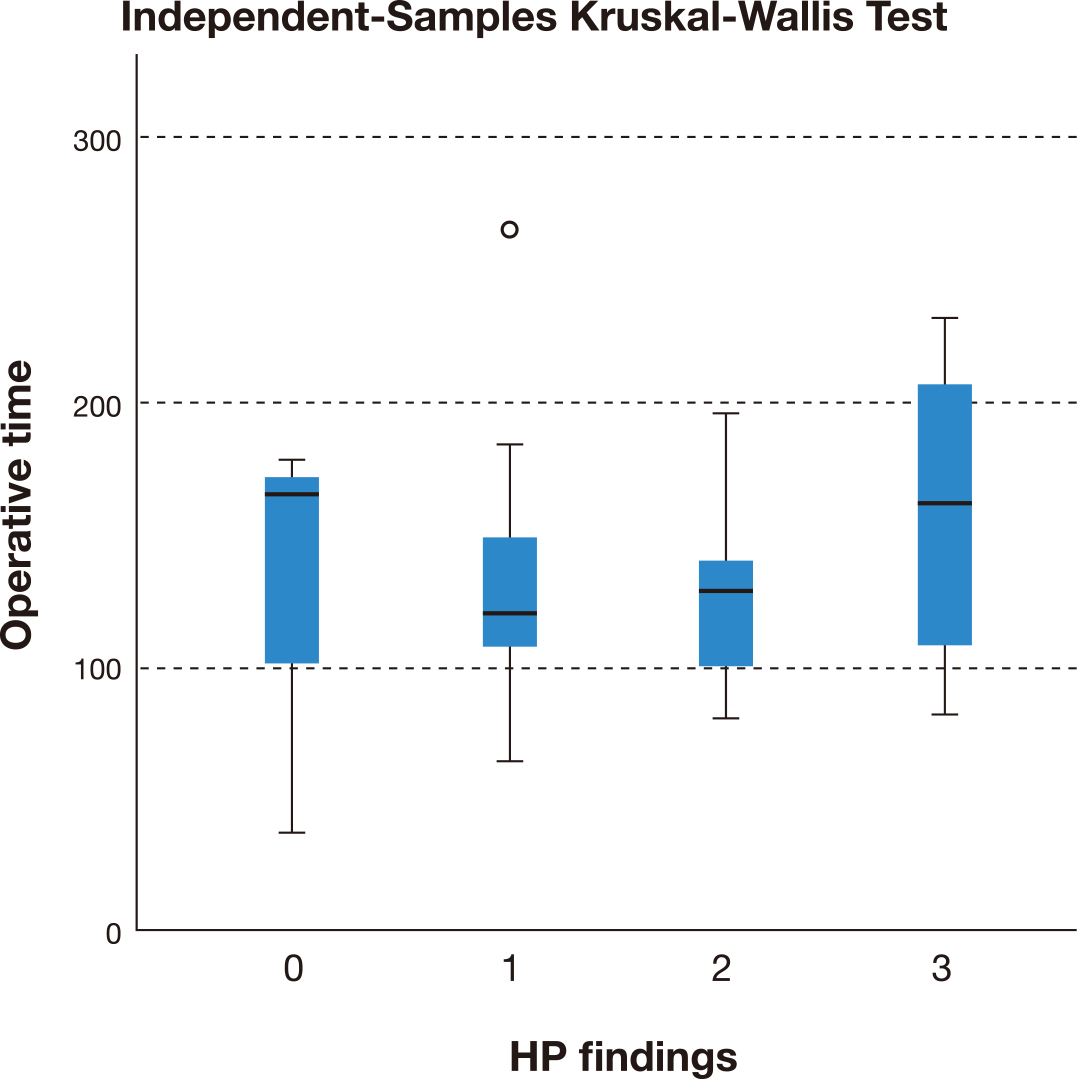 Fig. 4.
Fig. 4.Independent-Samples Kruskal-Wallis Test comparing the operative
time between placenta not accreta (0), accreta (1), increta (2) and percreta (3)
(confirmed on histopathological examination).
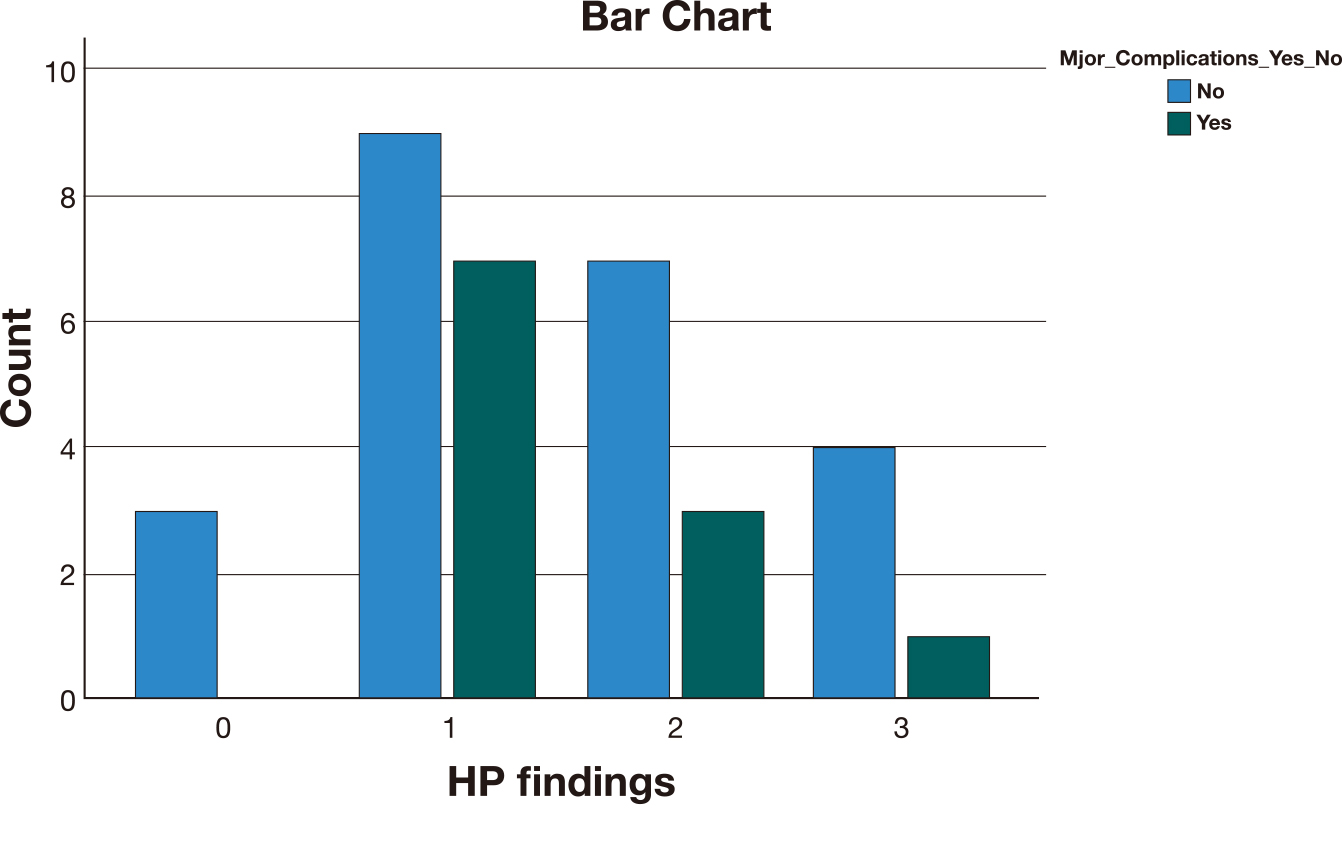 Fig. 5.
Fig. 5.Major complications frequency among the different histopathological groups (0 = no accreta, 1 = accreta, 2 = increta, 3 = percreta).
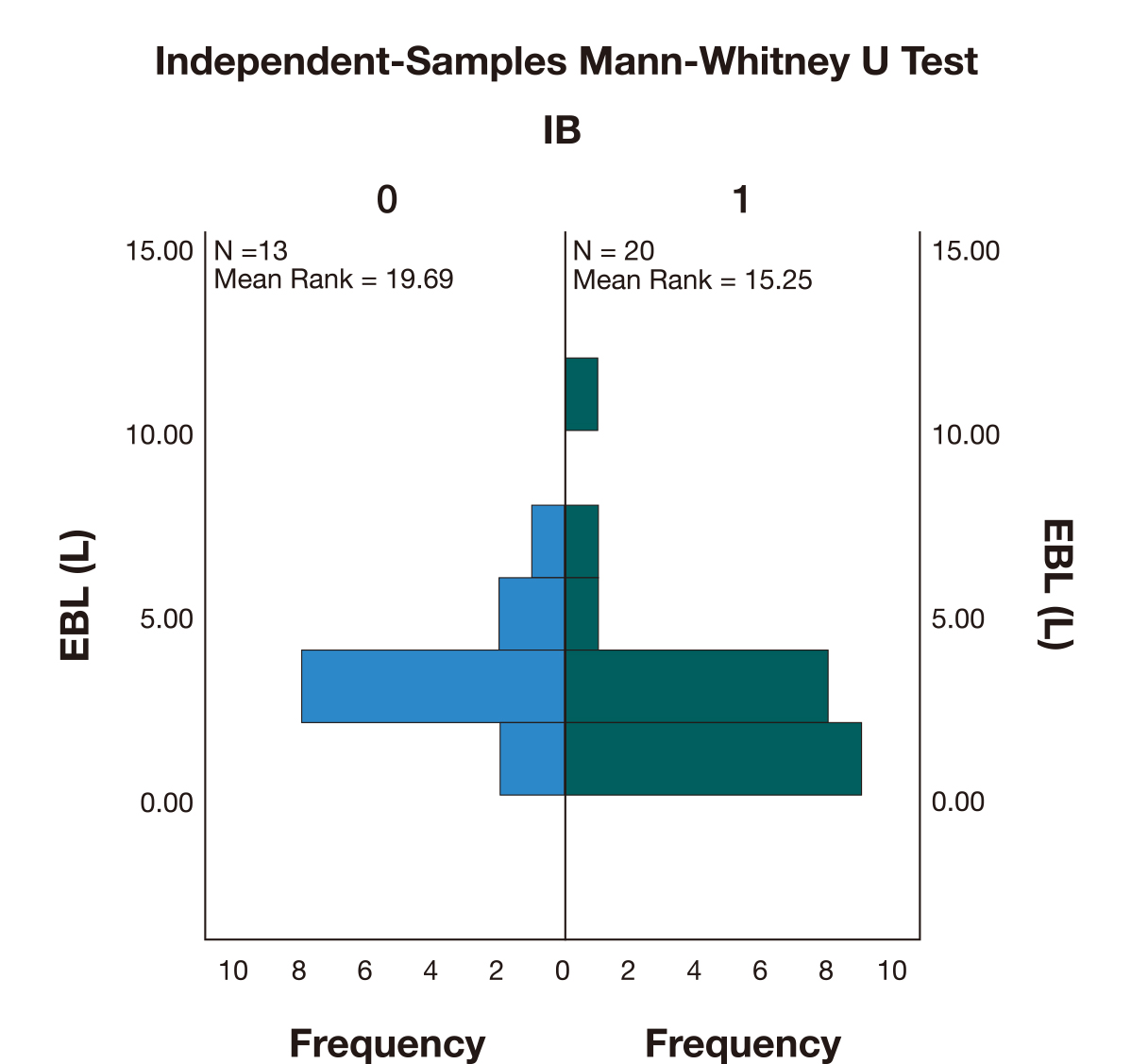
The use of iliac artery balloons (IB) was associated with lower blood loss (M = 2.5 L) when compared with the cases where IB weren’t used (M = 2.8 L). However, a Mann-Whitney U test (Fig. 6) indicated that this difference was not statistically significant (U = 95,000, p = 0.21).
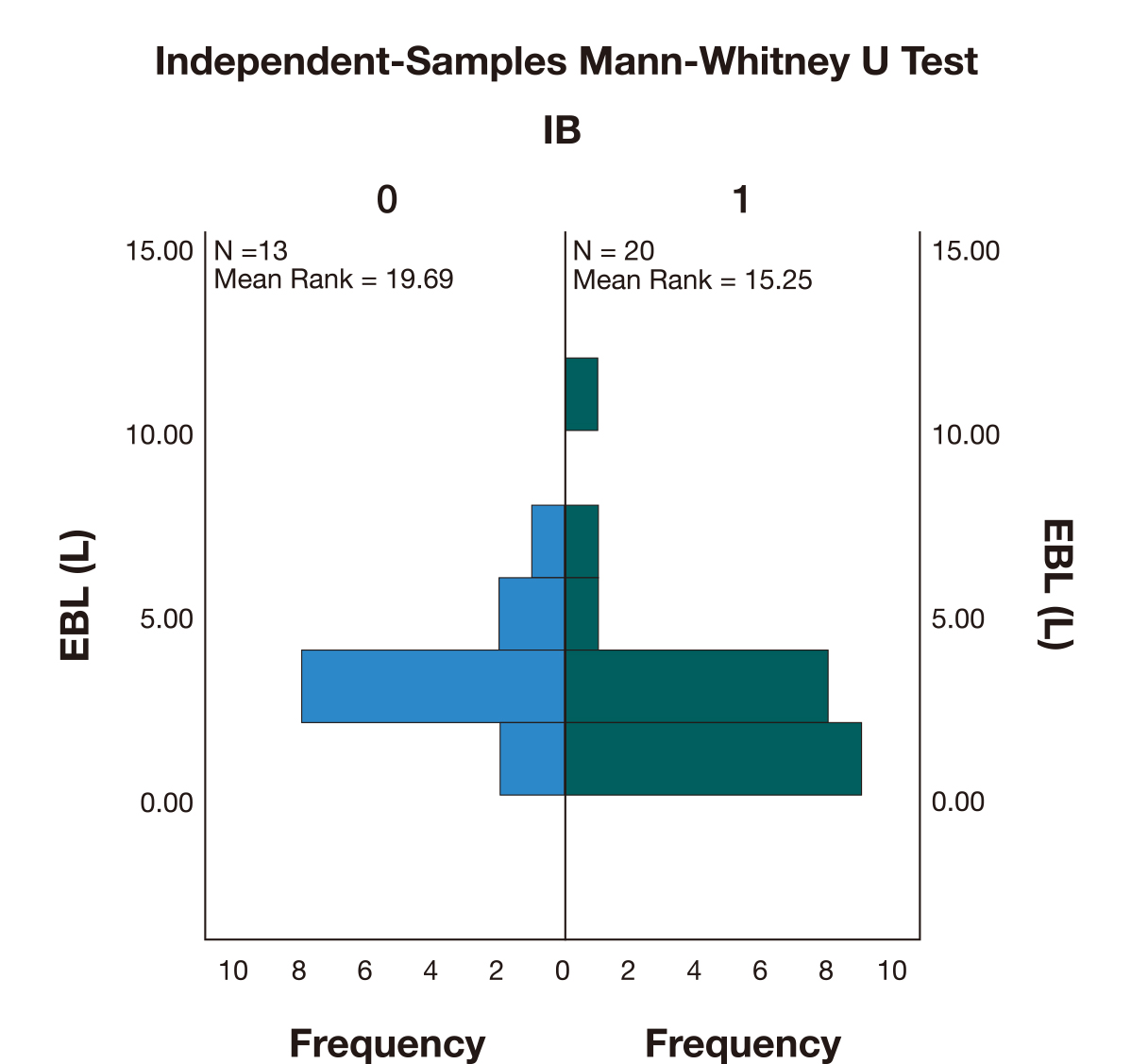 Fig. 6.
Fig. 6.Independent-Samples Mann-Whitney U Test comparing the estimated blood loss (EBL) between the cases where iliac artery occlusion was performed (1) versus the cases where iliac balloons (IB) were not used (0).
The operative time in the cases where IB were used (M = 138) was higher compared to the cases where IB weren’t used (M = 116). A Mann-Whitney U test (Fig. 7) indicated that this difference was not statistically significant (U = 182,000, p = 0.15).
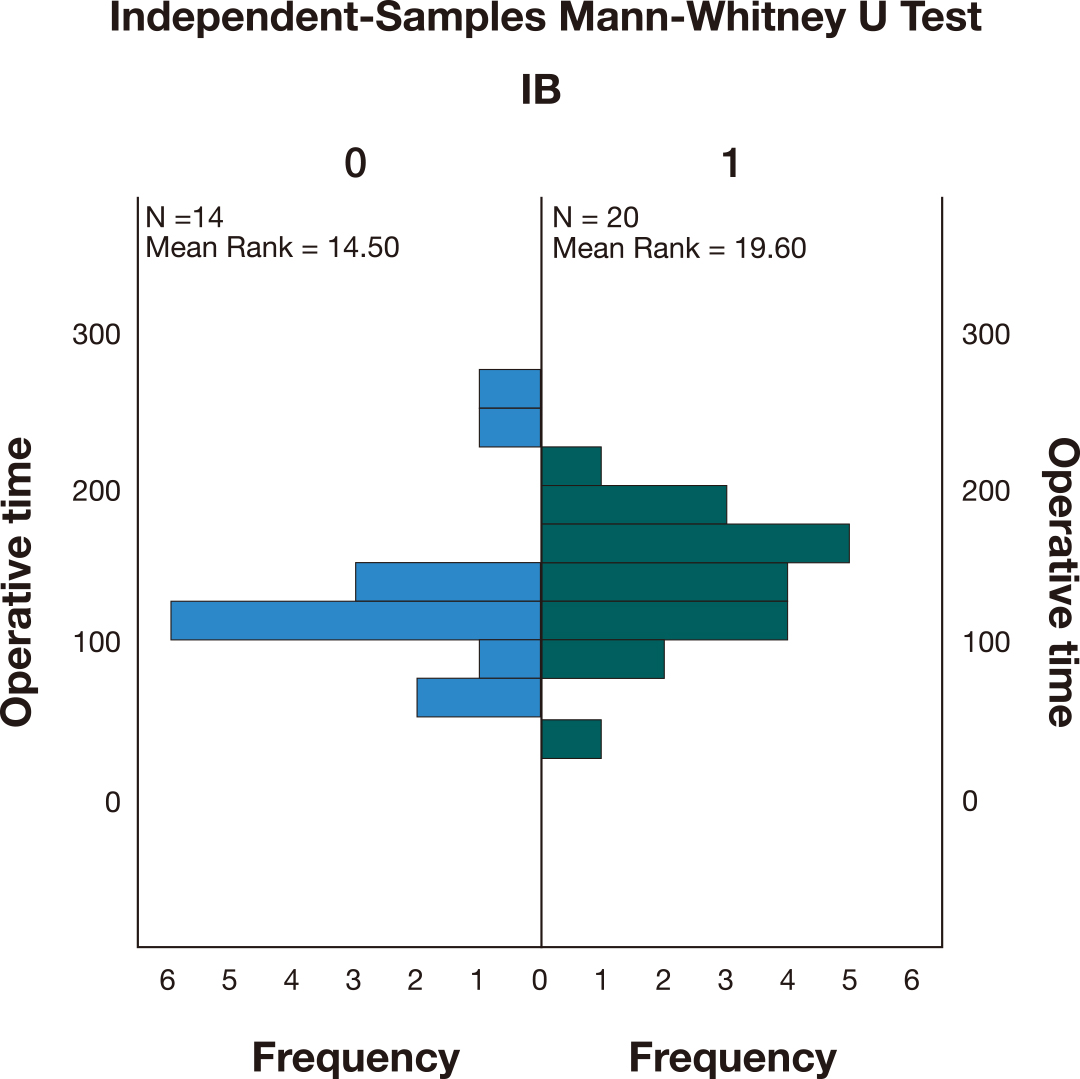 Fig. 7.
Fig. 7.Independent-Samples Mann-Whitney U Test comparing the operative time between the cases where iliac artery occlusion was performed (1) versus the cases where iliac balloons (IB) were not used (0).
The overall incidence of PAS in our unit was 0.6/1000 from 2004 to 2020, which appears lower when compared to the available literature [12].
In our cohort, the ultrasound findings were highly suspicious of the diagnosis
of PAS in 63.3%, inconclusive in 16.7% and normal/no signs of PAS in 20%. Some
of the current available literature describes a sensitivity ranging from 50 to
90% for the diagnosis of PAS using ultrasonography [10, 15]. Silveira et
al. [16] recently published an analysis of 70 cases of PAS diagnosed on
hysterectomy specimens over the last 14 years in Western Sydney Local Health
District to determine the antenatal detection rate and differences in management
and outcomes between PAS suspected and not suspected antenatally. The reported
prenatal detection rate was 54% (lower than ours) [16]. D’Antonio et
al. [11] reported, however, very high sensitivity and specificity (
Overall, the histopathological examination confirmed PAS diagnosis in 90.9% (no histopathological results for the case with the placenta was left in situ but the macroscopic appearance intra-operatively was that of placenta percreta). In 3 cases, the diagnosis wasn’t confirmed on histopathology. One of the cases had 1 previous CS, the ultrasound findings were suspicious of placenta accreta and the MRI findings were compatible with a focal accreta. The intra-operative findings were also suggestive of PAS and a hysterectomy was required to control the bleeding after a trial of removal of the placenta, but the abnormal placental implantation wasn’t confirmed on the histopathological examination. A second case had no previous caesarean sections, only one dilatation and curettage. The ultrasound findings suggested a possible accreta, the MRI findings were similar, however, the intra-operative macroscopic appearance and the histopathological examination did not confirm PAS, with a routine caesarean section being performed in this case. In the third case where PAS wasn’t confirmed on HP, the patient had 3 previous caesarean sections and both ultrasound and macroscopic findings were suggestive of accreta. A planned hysterectomy was performed as the woman didn’t want to preserve fertility.
The use of iliac artery balloons (in earlier cases placed in the internal iliac arteries and later in the common iliac arteries, as the latter will additionally block the supply to the placenta from the external iliac arteries) [17, 18, 19, 20, 21] was associated with a reduction in blood loss, although not statistically significant. This may have been related to the fact that the cases who had iliac balloons placed were the most complex and were expected to be associated with high blood loss. According to the SMFM guidelines, the role of iliac artery occlusion (internal and common arteries) is still controversial as it has been reported to decrease blood loss in some studies but showed no difference in others [2]. It also has been postulated that PAS is associated with neovascularisation and abnormal blood supply therefore occluding pelvic vessels may exacerbate bleeding from the collateral circulation, thus limiting the benefit of this procedure [17, 18, 19, 20, 21, 22, 23, 24, 25, 26]. International Federation of Obstetrics and Gynecology (FIGO) does not recommend its routine use due to a lack of strong supporting evidence of their benefit [1]. Furthermore, interventional radiology-related complication rates as high as 15% have been quoted, including iliac artery thrombosis or rupture and ischaemic nerve injury [3, 4], however, in our cohort there were no complications associated with this procedure.
The value of preoperative ureteric stent placement to prevent ureteric injury has also been controversial [25, 27]. In our cohort, there was no ureteric injuries but the sample is too small to draw any conclusions. Nevertheless, the surgeons in our team found that ureteric stents were helpful to identify the ureters during the surgery and so are useful for complex cases to avoid ureteric injury.
Unexpectedly in our cohort, the degree of PAS was not correlated with higher risk of bleeding and complications. This may have been related to the small size of the sample or to the fact that in the more severe cases, a hysterectomy was planned from the outset and preventive measures (iliac balloons, ureteric stents and cell salvage) were used systematically. Of the 4 cases where placenta percreta was confirmed on histopathological examination, 3 had a planned hysterectomy without trial of placenta removal and iliac balloons, ureteric stents and cell salvage were used as preventive measures to decrease blood loss and complications. One of the cases required bladder repair after hysterectomy due to bladder involvement.
In relation to risk factors, although the PACCRETA study [9] from 176 hospitals in France (n = 249 cases) found that half of the cases did not have the classical combination of risk factors, in our cohort 79% of the patients had previous caesarean sections and only 3 patients had no history of uterine surgeries. All patients had a placenta praevia on morphology scan. The traditional risk factors were present in the majority of our patients.
The mean gestational age at delivery for the cases delivered emergently was 32 weeks and mostly due to APH and PTL. For planned deliveries the mean GA was 36 weeks. The blood loss was higher for the cases delivered emergently but the difference was not statistically significant. The perinatal outcomes, including admission to neonatal intensive care unit (NICU), were directly related to prematurity. This suggests that the ideal gestational age for delivery should balance the risk of prematurity with the risk of maternal complications that might follow emergent deliveries. Presently, current international guidelines recommend 34 to 36 weeks as the ideal timing to balance these risks [1, 2, 3, 4].
The maternal morbidity from our study including major complications (32.7%) and reoperation rates (17.6%) is similar to other published papers. Eller described an overall maternal morbidity of 59% [19] and Bartels et al. [28] described postoperative complications ranging from 35% to 46% in women with PAS managed in a large tertiary center with multidisciplinary involvement.
As a retrospective study with a small sample size the nature of the study design is open to inclusion bias and error. Our incidence of PAS was only 0.6:1000 cases, lower than the literature. Internationally, PAS prevalence has been increasing along with the caesarean section rate in most of the Organisation for Economic Cooperation and Development (OECD) countries. And according to the “Mothers and babies report” from 2020, the Australia’s caesarean rate has increased from 24.5% in 2004 to 32.1% in 2020 and these numbers are similar to countries such as the United Kingdom, Switzerland, Italy, Ireland, Hungary and Poland, although higher than the OECD average (28% in 2019). Based on these statistics, the number of caesarean sections doesn’t explain our difference in PAS prevalence. Furthermore, previous Australian studies on PAS have quoted an incidence of 0.92:1000 to 24.8:1000 [16]. Reasons for our lower rates may include the fact that only the prenatally suspected cases were included, some of the cases of mild accreta are not recognised as such during delivery and are managed as a postpartum haemorrhage due to atony, and so the placenta is not sent for histopathological (HP) examination, or that some of them may be only focal and so the HP routine placental cuts may miss small focal areas.
Due to our small sample size we were unable to assess some parameters for their statistical significance, or perform statistical analyses to correct for confounders. We were also not able to collect the cases of PAS that were not suspected clinically or diagnosed prenatally, which would be very important for some of the conclusions.
In conclusion, the implementation of new strategies for the diagnosis and management of PAS disorders, including the use of MRI for cases where ultrasound is inconclusive and delivery planning by an experienced surgical team in collaboration with other specialities (interventional radiology, urology, haematology, blood bank and intensive care unit (ICU)) has been shown to be of the utmost importance for the management of PAS disorders [1, 2, 3, 4, 5, 6, 29, 30].
In our study, although limited by the small sample size, the use of iliac balloons reduced the blood loss and operative time (although the difference was not statistically significant) and ureteric stents were used in the most complex cases where the surgeons found them to be useful in helping identify the ureters and avoid ureteric injury.
In 2019, we started using a PAS assessment tool (based on FIGO and SMFM guidelines) to improve the prenatal diagnosis of PAS and we also implemented a policy for ultrasound evaluation of uterine scars during pregnancy, including scar identification and location relative to the internal cervical os from the first trimester. Hopefully we will be able to evaluate the impact of these tools on the prenatal diagnosis of this condition in future with higher numbers. Nonetheless, the clinical risk assessment may be the most important factor to assess the risk of these disorders, as some authors suggest [2].
We hope that our study can help us to improve our clinical practice and the quality of care offered to patients that may present in future with PAS disorders.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
RC—Principal Investigator (responsible for the project design, acquisition of data, analysis and interpretation of data, drafting the manuscript); AP—Associate Investigator (contribution for data collection and obtaining ethics approval); AA—Associate Investigator (contribution to revision of the manuscript); NB—Associate Investigator (contribution to data acquisition process); JS—Associate Investigator (contribution to data acquisition process); FR—Coordinating Principal Investigator (contribution to conception and design of the study, revision of the manuscript and final approval of the version to be published). All authors read and approved the final manuscript.
The study was approved by the Research Ethics and Governance Information System (REGIS) with the identifier 2021/PID03717. A waiver of consent was justified in this study as all data was de-identified and there was no risks to the participants - apporved by REGIS.
We would like to express our very great appreciation to Professor Jose Carlos Caldas for his help with the statistical analysis.
This research received no external funding.
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.