1 Department of Cardiovascular Surgery, Chinese Academy of Medical Sciences and Peking Union Medical College Fuwai Hospital, 100037 Beijing, China
2 National Health Commission Key Laboratory of Cardiovascular Regenerative Medicine, Central China Fuwai Hospital of Zhengzhou University, 451400 Zhengzhou, Henan, China
Abstract
Current evidence suggests that multiple arterial grafting improves long-term survival following coronary artery bypass grafting (CABG). Sequential radial artery (RA) grafting is known to be a safe approach for maximizing arterial revascularization. This study aimed to compare RA conduit patency between sequential and individual grafting.
A total of 274 CABG patients who received at least one RA graft between January 2017 and June 2021 were included in our retrospective study. The occlusion of RA anastomoses was assessed by postoperative computed tomography angiography or coronary angiography at follow-up. Group comparisons for long-term outcomes were conducted using adjusted Cox regression models.
The median image follow-up time was 1.8 years. Among the 278 total RA grafts, 208 were individual and 70 were sequential. Multivariable Cox analysis found that sequential anastomoses were an independent risk factor for RA graft occlusion (adjusted hazard ratio = 2.45, 95% confidence interval (CI): 1.15–5.22; p = 0.020). However, the observed rate of occlusion was low (2.9%) when all the target vessels for a sequential graft had a quantitative flow ratio of ≤0.71.
Sequential RA grafting is associated with graft occlusion compared with individual grafting. For each RA graft, the selection of only one target vessel with significant functional stenosis may be preferable to achieve superior long-term patency.
Keywords
- coronary artery bypass
- radial artery graft
- sequential graft
Several studies have confirmed that utilization of two or more arterial grafts is associated with better long-term survival compared to conventional single-arterial coronary artery bypass grafting (CABG) based on the left internal thoracic artery (LITA) and saphenous vein graft (SVG) [1, 2, 3]. Given its relatively easy harvest and lower risk of deep sternal infection compared to bilateral internal thoracic artery (ITA) [4], the radial artery (RA) has emerged as the predominant choice for a second arterial graft in both the United States and Europe [5, 6]. To improve long-term cardiac outcomes, the most recent guidelines have increased their recommendation level for employing RA grafts to class I [7].
Frequent use of the right RA for angiography prior to CABG has raised concerns about intimal tears and impending graft failure [8]. Therefore, unilateral RA grafting is often used more frequently than bilateral RA. Sequential grafting of the RA is a safe method of choice and helps to maximize the number of constructed arterial grafts. A number of studies have investigated the long-term outcomes of CABG with sequential RA grafting. These reported superior 10-year survival compared with conventional LITA and SVG [1, 9]. The RA conduit is known to be sensitive to competitive flow from the native coronary artery, which may be a key factor in premature graft loss [10]. However, multiple distal anastomoses in sequential grafts can increase the risk of coronary steal and graft flow reversal [11]. Previous studies did not account for significant heterogeneity in the target vessels of RA grafts, and hence the efficacy of sequential RA grafting remains unclear.
We previously reported that the preoperative quantitative flow ratio (QFR) of target vessels at the site of RA anastomoses was a robust predictor of occlusion [12]. Indeed, QFR proved to be a more accurate indicator of RA graft occlusion than the degree of stenosis. There is currently a lack of published literature on the different risk factors for RA graft patency. Therefore, the aim of this study was to conduct a risk-adjusted comparison of long-term patency between individual and sequential RA grafting.
This retrospective study was approved by the Ethics Committee of Fuwai Hospital (No. 2021-1554), which also waived the need for written informed consent.
The cohort included consecutive patients who received CABG procedures at Fuwai Hospital from January 2017 to June 2021. Patient inclusion criteria were as follows: (1) received angiography at our center within 1 year before surgery; (2) at least one RA graft was used. Patient exclusion criteria were: (1) lack of imaging follow-up for graft patency beyond three months postoperatively; (2) poor quality of angiographic images hindering QFR measurement.
To evaluate the patency of sequential grafting, all RA grafts were first categorized into either individual or sequential groups. To compare the clinical outcomes between these two groups, patients with both individual and sequential grafts were excluded.
Median sternotomy was employed for all patients. In every procedure, the left ITA was in situ for grafting to the left anterior descending (LAD), while the RA served as an additional arterial conduit, either as the second or third graft. The sole basis for selection of the target vessel was preoperative angiography. Radial arteries were harvested using conventional open techniques with pedicle, then bathed in a solution composed of papaverine, diltiazem, and warm saline with heparinized autologous blood prior to grafting. All procedures were performed by highly experienced surgeons who adhered to standardized protocols. On-pump surgery was performed with cardiopulmonary bypass under cardioplegic arrest. Individual RA grafts had only one distal end-side anastomosis, whereas sequential RA grafts were anastomosed to two or more target vessels. The RA graft was connected proximally to the ascending aorta through a direct anastomosis.
Preoperative coronary angiography was conducted using a conventional percutaneous approach via either the femoral or radial artery. The degree of stenosis in target vessels of RA grafts was visually estimated by two experienced operators. QFR computation was performed using AngioPlus Core software (V3.0, Pulse Medical Imaging Technology, Shanghai Co., Ltd., Shanghai, China) by two experienced analysts (Supplementary Fig. 1). In cases where QFR could not be measured due to total occlusion of the target vessel, an assigned default value of 0.50 was given, as described in a previous study [13]. All patients were recommended to receive regular coronary computed tomography angiography (CCTA) or angiography follow-up at three months, one year, and three years postoperatively, as well as follow-up through outpatient consultation or telephone interviews. The percentage of patients who were followed up by imaging at each time point is shown in Supplementary Table 1.
The primary endpoint was the occlusion of RA grafts, as assessed by CCTA or
angiography at least three months after surgery. Occlusion of an RA graft was
defined as total occlusion in any segment between the proximal and distal
anastomoses of the graft. For sequential RA grafting, we aimed to position the
distal anastomoses at the optimal target site with favorable run-off and a
suitable degree of stenosis (
The secondary endpoint was major adverse cardiac or cerebrovascular events (MACCEs) in patients, defined as the composite outcome of all-cause mortality, myocardial infarction, stroke, or repeat revascularization.
Depending on their distribution, continuous variables were presented as the mean
A multivariable Cox proportional hazards model was used to evaluate the impact of the anastomoses method on graft outcomes. The proportional hazards assumption in the Cox model was assessed using Schoenfeld residuals. Variables were chosen based on previous literature and clinical plausibility. They included baseline characteristics and intraoperative conditions. The QFR of the target vessel was set at a threshold of 0.71 based on our previous findings [12]. For the primary outcome, subgroup and interaction-term analyses were used to investigate possible effect modifiers. These had been prespecified.
Statistical analyses were performed using R software, version 4.1.2 (R
Foundation for Statistical Computing, Vienna, Austria). p-values were
2-sided, and p-values
A total of 368 patients underwent preoperative angiography and CABG with at least one RA graft between January 2017 and June 2021 in our center. Five patients were excluded from the QFR measurement due to poor quality of angiographic images. Of the remaining 363 patients, 89 were excluded due to a lack of imaging follow-up after three months postoperatively. Consequently, the final analysis included 274 patients with a total of 278 RA grafts (Fig. 1). The majority of patients (98.5%) underwent one single RA grafting, either as an individual or sequential method. Only 3 patients underwent two separate RA grafts using the individual method, while one patient had both an individual graft and a sequential graft.
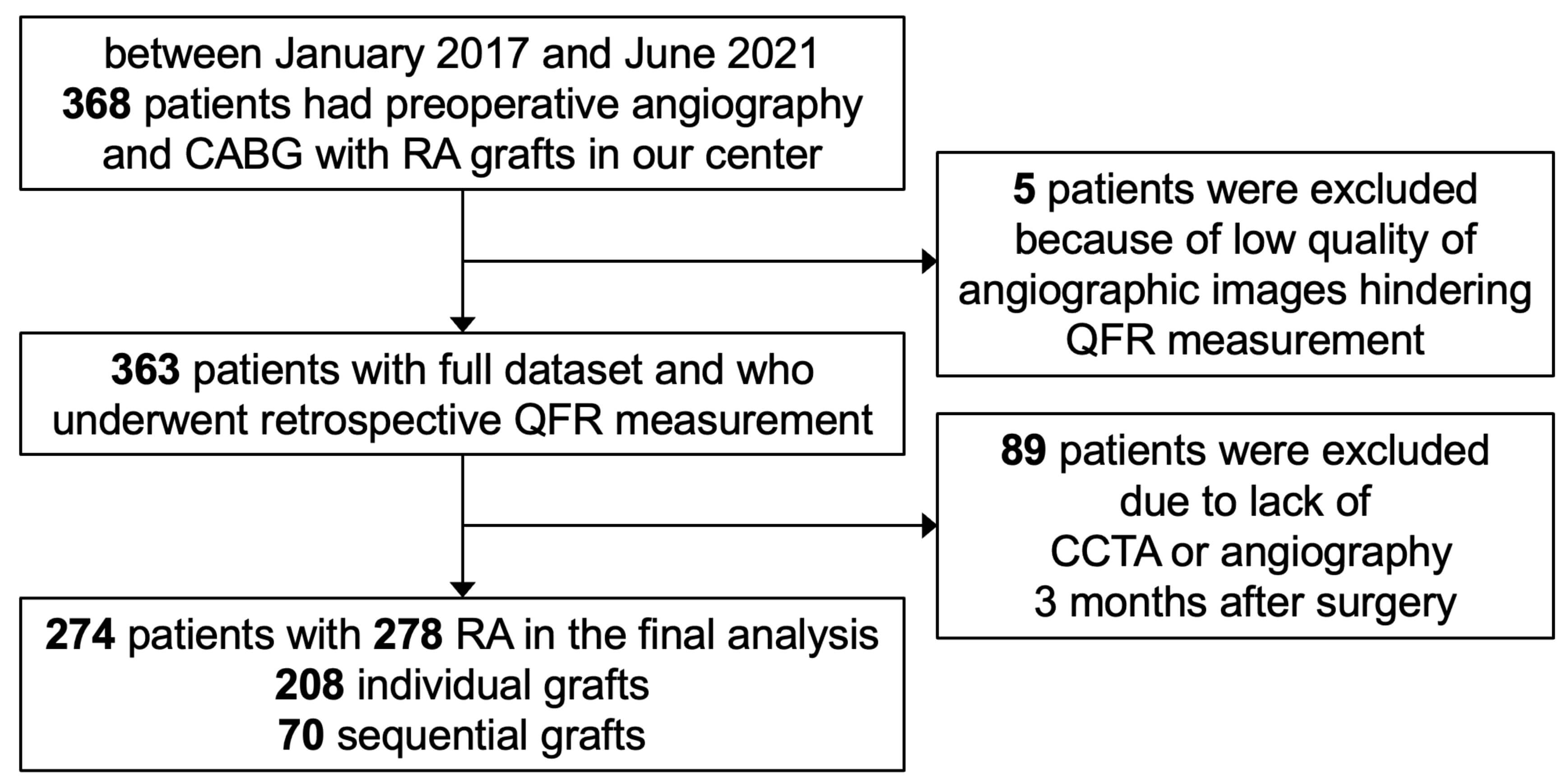 Fig. 1.
Fig. 1.
Study flow chart. CABG, coronary artery bypass grafting; RA, radial artery; QFR, quantitative flow ratio; CCTA, coronary computed tomography angiography.
The baseline demographic, clinical, and operative profiles of patients who
underwent individual or sequential grafts are shown in Table 1. The average age
of patients at the time of surgery was 53.8
| Individual (n = 208) | Sequential (n = 70) | p-value | |
| Male | 197 (94.7%) | 62 (88.6%) | 0.137 |
| Age, years | 53.4 |
55.3 |
0.147 |
| BMI, kg/m2 | 26.2 |
26.3 |
0.843 |
| EF |
11 (5.3%) | 3 (4.3%) | 0.987 |
| Smoking | 141 (67.8%) | 43 (61.4%) | 0.408 |
| Diabetes | 77 (37.0%) | 27 (38.6%) | 0.929 |
| Hypertension | 120 (57.7%) | 46 (65.7%) | 0.297 |
| Hypercholesterolemia | 170 (81.7%) | 57 (81.4%) | |
| PVD | 8 (3.8%) | 6 (8.6%) | 0.212 |
| Prior PCI | 43 (20.7%) | 13 (18.6%) | 0.836 |
| Prior MI | 60 (28.8%) | 23 (32.9%) | 0.629 |
| 3-vessel disease | 129 (62.0%) | 36 (51.4%) | 0.156 |
| Left main disease | 12 (5.8%) | 3 (4.3%) | 0.865 |
| Distal target diameter, mm | 1.92 |
1.89 |
0.699 |
| Distal target to left coronary system* | 122 (58.7%) | 60 (85.7%) | |
| On-pump | 107 (51.4%) | 12 (17.1%) | |
| Imaging follow-up, years | 2.0 [1.2, 3.3] | 1.4 [1.0, 2.2] | 0.008 |
| QFR of distal anastomoses | 0.58 [0.50, 0.74] | 0.54 [0.50, 0.73] | 0.905 |
| QFR |
66 (31.7%) | 24 (34.3) | 0.805 |
| DS of distal anastomoses, % | 90.0 [80.0, 95.0] | 90.0 [80.0, 99.0] | 0.488 |
QFR, quantitative flow ratio; DS, degree of stenosis; BMI, body mass index; EF, ejection fraction; PVD, peripheral vascular disease; PCI, percutaneous coronary intervention; MI, myocardial infarction.
*The left coronary system includes diagonal, ramus intermedius, obtuse marginal and posterior branches of left ventricle from circumflex.
The RA grafts included 70 sequential (61 double, 9 triple) and 208 individual
configurations. Compared to the individual RA group, the sequential group had a
lower proportion of on-pump CABG (17.1% vs. 51.4%, p
| Coronary target | Individual (n = 208) | Sequential (n = 70) | |
| Single coronary system | |||
| Diagonal or ramus intermedius | 47 (22.6%) | 4 (5.7%) | |
| Circumflex | 76 (36.5%) | 9 (12.9%) | |
| RCA | 85 (40.9%) | 5 (7.1%) | |
| Multiple coronary systems | |||
| Diagnal/Ramus + Circumflex | - | 47 (67.1%) | |
| Circumflex + RCA | - | 5 (7.1%) | |
Circumflex system includes obtuse marginal and posterior branches of left ventricle from circumflex; RCA, right coronary artery system (includes right main, acute marginal, posterior descending, and posterior branches of left ventricle from right coronary); RA, radial artery.
No perioperative deaths occurred in the study cohort. The median duration of
imaging follow-up was 1.8 years (IQR [1.1, 2.9]), during which the overall
unadjusted RA graft patency reached 82.0%. Kaplan-Meier analysis revealed that
cumulative patency rates at 1, 2, and 3 years were 91.5%, 83.6%, and 79.3%,
respectively (Fig. 2A). The incidence rate for graft occlusion was 79 events per
1000 patient-years in the individual group, versus 136 events per 1000
patient-years in the sequential group (Table 3). Although log-rank analysis
showed no statistically significant difference between the two groups (p
= 0.099; Fig. 2B), sequential grafting was identified as an independent risk
factor for graft occlusion in multivariable analysis (adjusted hazard ratio (aHR)
= 2.45; 95% CI: 1.15–5.22; p = 0.020) (Table 4). QFR
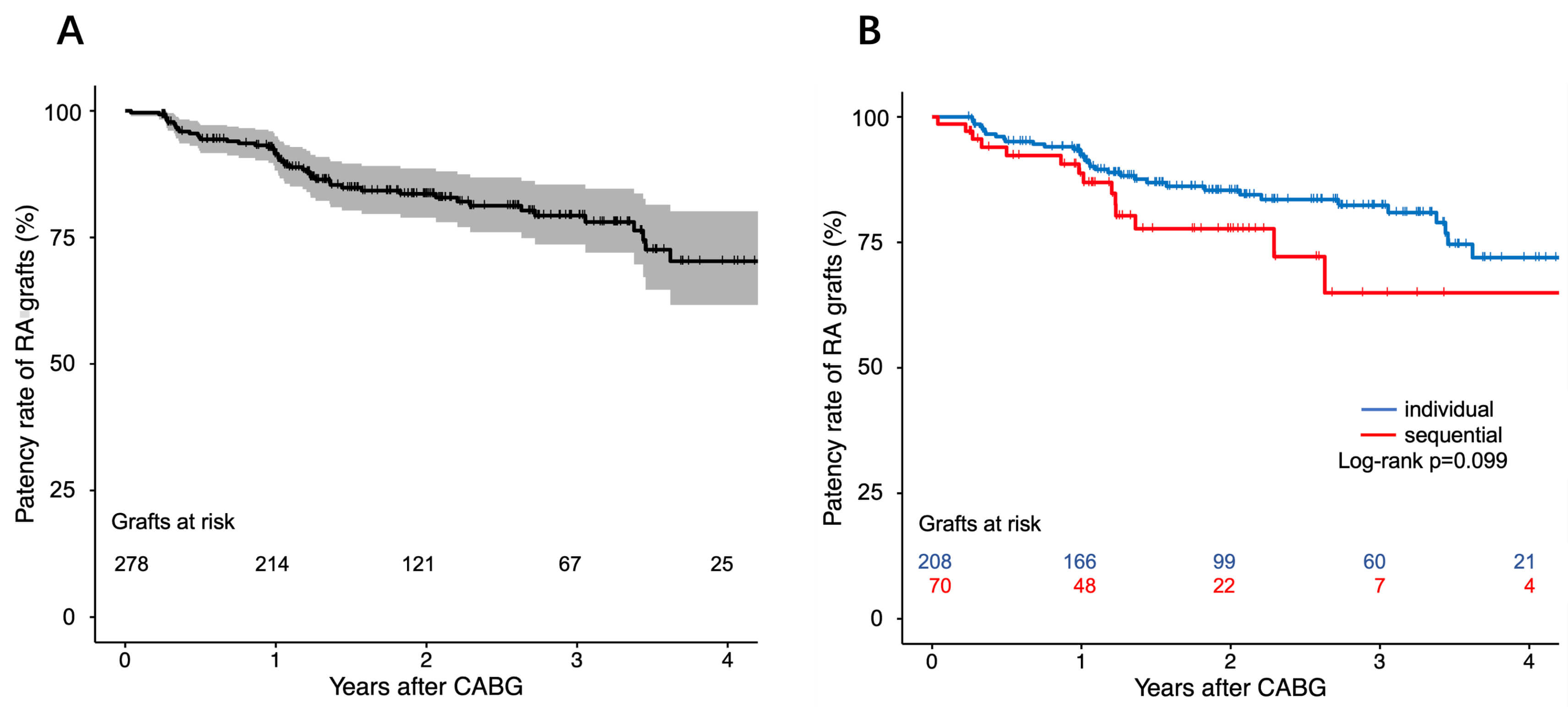 Fig. 2.
Fig. 2.
Kaplan-Meier curve of RA grafts patency. (A) Kaplan-Meier curve of total RA grafts patency. (B) Comparison of cumulative RA grafts patency between individual and sequential groups. RA, radial artery; CABG, coronary artery bypass grafting.
| Outcomes | Individual (n = 208) | Sequential (n = 70) | Treatment effect* | |||||
| No. of events | E/kPY | No. of events | E/kPY | HR (95% CI) | p-value | aHR (95% CI) | p-value | |
| Graft occlusion | 35 (16.8%) | 79 | 15 (21.4%) | 136 | 1.67 (0.90–3.08) | 0.103 | 2.45 (1.15–5.22) | 0.020 |
| MACCEs# | 10/204 (4.9%) | 24 | 1/69 (1.4%) | 9 | 0.39 (0.05–3.02) | 0.364 | 0.14 (0.01–1.63) | 0.117 |
*Results are from a multivariable Cox regression model, with the individual group used as the reference group.
#The analysis of MACCEs excluded 1 patient who received both individual and sequential RA grafts.
E/kPY, Events per 1000 Patient-Years; aHR, adjusted hazard ratio; 95% CI, 95% confidence interval; MACCEs, major adverse cardiac or cerebrovascular events; HR, hazard ratio.
| Variable | HR (univariate) | p-value | aHR (multivariate) | p-value |
| Sequential graft | 1.67 (0.90–3.08) | 0.103 | 2.45 (1.15–5.22) | 0.020 |
| QFR |
9.66 (4.82–19.34) | 10.55 (4.72–23.56) | ||
| Age |
0.45 (0.19–1.06) | 0.066 | 0.58 (0.23–1.44) | 0.239 |
| Female | 0.70 (0.17–2.91) | 0.627 | 1.05 (0.24–4.61) | 0.951 |
| BMI | 1.05 (0.95–1.15) | 0.350 | 0.97 (0.85–1.10) | 0.630 |
| EF |
0.81 (0.20–3.35) | 0.773 | - | - |
| Diabetes | 1.23 (0.70–2.16) | 0.467 | - | - |
| Hypertension | 1.12 (0.63–1.99) | 0.692 | - | - |
| Hypercholesterolemia | 0.92 (0.44–1.89) | 0.815 | - | - |
| PVD | 1.16 (0.28–4.80) | 0.837 | - | - |
| Prior MI | 0.50 (0.23–1.10) | 0.085 | 0.40 (0.18–0.87) | 0.021 |
| Smoking | 1.20 (0.65–2.24) | 0.559 | - | - |
| On-pump surgery | 0.94 (0.51–1.73) | 0.838 | 0.94 (0.47–1.90) | 0.877 |
| Target on left system | 1.00 (0.56–1.79) | 0.797 | 1.51 (0.66–3.34) | 0.309 |
HR, hazard ratio; aHR, adjusted hazard ratio; QFR, quantitative flow ratio; BMI, body mass index; EF, ejection fraction; PVD, peripheral vascular disease; MI, myocardial infarction.
After a median follow-up period of 1.8 years (IQR [0.9, 3.0]), the overall incidence of MACCEs was just 4.0%. All patients survived without experiencing a myocardial infarction. Eight patients suffered a stroke, and 3 patients underwent percutaneous coronary intervention. The Kaplan-Meier curve for patient outcomes is shown in Supplementary Fig. 4. After the exclusion of one patient who received both individual and sequential RA grafts, the incidence of MACCEs was not significantly different between the individual (4.9%) and sequential (1.4%) groups (aHR = 0.14, 95% CI: 0.01–1.63, p = 0.117) (Supplementary Table 2).
The sequential grafts were classified into four categories based on the QFR of
distal and middle anastomoses, with a cut-off value of 0.71. The graft occlusion
in each group is shown in Fig. 3. When the QFR of both the distal and middle
anastomoses was
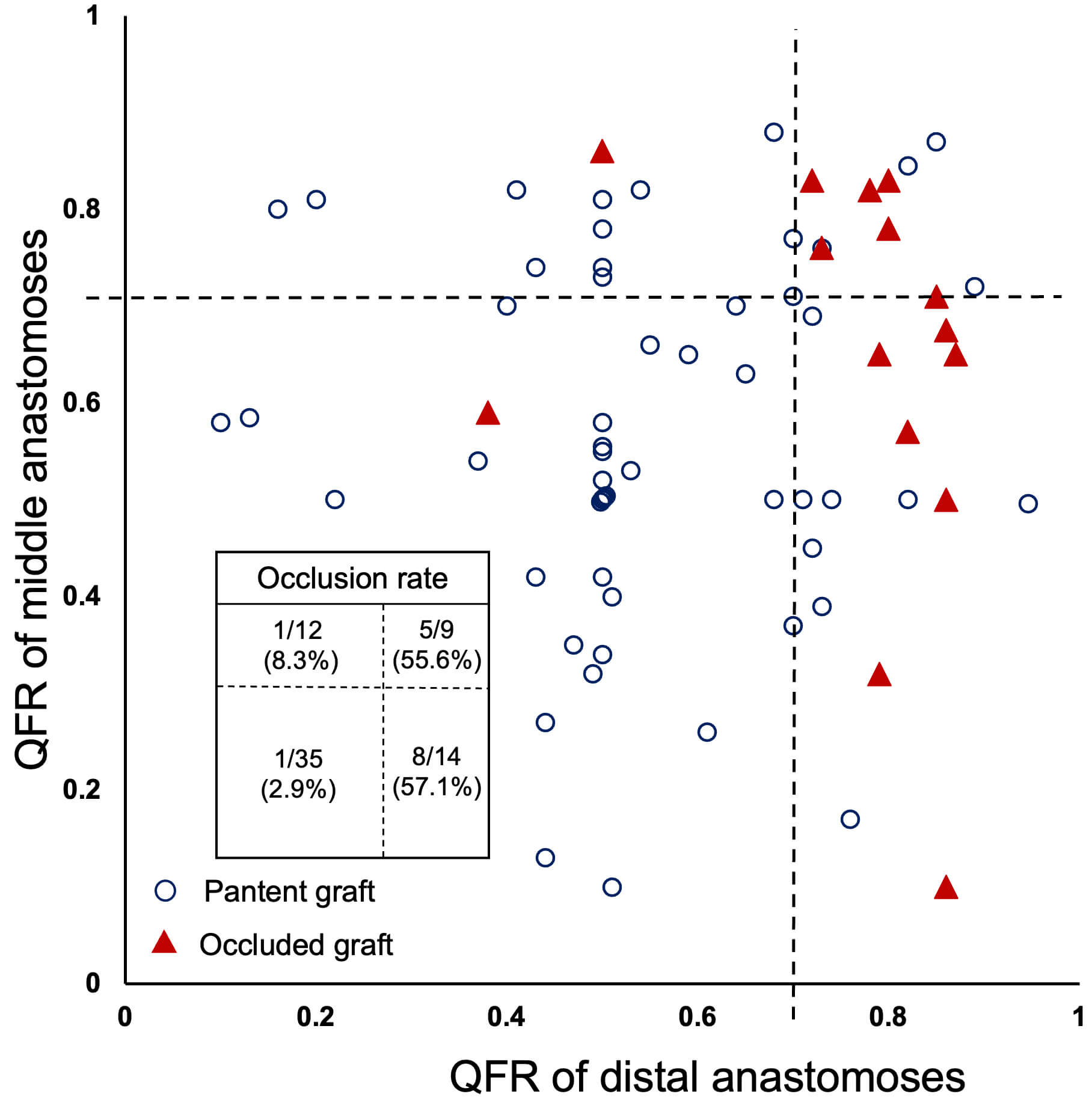 Fig. 3.
Fig. 3.
The QFR of target vessels in sequential grafts and graft patency. Each point represents an RA graft. The x-axis shows the QFR of the distal anastomoses of sequential grafts, while the y-axis shows the QFR of the middle anastomoses (average used when multiple). QFR, quantitative flow ratio; RA, radial artery.
This single-center retrospective cohort study investigated the long-term patency
of RA bypass grafts to identify risk factors associated with graft occlusion. The
sequential method of anastomoses was found to be a significant predictive factor
for RA graft occlusion, as well as target vessels with a QFR
Following revival of the RA conduit in the 1990s [14], its utilization in CABG has been supported by solid evidence demonstrating its clinical benefits. The RADIAL project found that patients with RA grafts as the second conduit in addition to the left ITA had significantly reduced incidence of MACCEs at both 5- and 10-year follow-up compared to SVG [2, 3]. The RA also showed advantages over the right ITA, with better long-term patency and fewer sternal-related complications [15]. Consequently, utilization of the RA was recommended in the guidelines and is frequently utilized in clinical practice as the primary choice for second arterial graft material [7, 16].
Sequential RA grafting helps to achieve complete revascularization and maximize the number of arterial grafts. However, there have been only a few studies on the patency of sequential RA grafting. Schwann et al. [9] assessed the angiographic results of sequential RA grafting in 122 patients with a median follow-up of 1.8 years, finding an overall patency of 71%. Furthermore, no significant difference in patency was observed between sequential and individual RA grafts. However, the conclusion reached by these authors is open to question, first because the angiographic follow-up was symptom-driven, and second because the sample size of nonsequential grafts in their study was limited. There are also ongoing concerns about the long-term patency of sequential RA grafts due to the coronary steal phenomenon.
Clinical and demographic characteristics were taken into account in the present
study, and specifically the functional characteristics of target vessels. We
observed a significant association between the sequential grafting method and the
occlusion of RA grafts following CABG surgery. Several pathophysiological factors
may be responsible for the superior patency observed with single conduits. First,
sequential grafts may be more susceptible to blood flow reversal compared to
individual grafts. In the context of RA to non-LAD bypass, Nakajima et
al. [17] reported that 86.3% of competitive flow occurred at the distal end of
sequential grafts. Graft occlusion in our cohort was lowest when the QFR of both
the middle and distal anastomoses was
Our results may provide an explanation for the unsuitability of extensive constructions involving more than two arterial conduits using sequential RA grafting. In a meta-analysis of 10,287 patients, Gaudino et al. [19] found that the use of a third individual arterial graft was associated with a 24% relative survival benefit. In contrast, Schwann et al. [20] did not observe a statistically significant advantage in 15-year survival in patients with three-artery grafts compared to those with two-artery grafts. The latter study consisted almost entirely of patients who received a left ITA and supplemental sequential RA grafts (bilateral, sequential, or both) rather than bilateral ITA. The construction of an extensive artery bypass based on sequential RA may be less effective clinically compared to the use of bilateral ITA and an individual RA. The higher attrition rate of sequential RA grafts observed in our study may be due to one of these underlying factors.
We also found that prior myocardial infarction was a protective factor for RA graft patency. This observation concurs with the results of subgroup analysis in the RADIAL project, which favored RA over SVG [2]. We speculate that patients who had collateral flow were prone to limited previous infarct size, and also had enhanced native competitive flow, thereby leading to decreased patency of RA grafts after CABG [21].
These findings underscore the potential clinical utility of QFR in guiding arterial graft planning during CABG. Preoperative QFR assessment may help identify target vessels with high competitive flow risk, particularly in sequential grafting, and thus assist in selecting optimal anastomosis sites to reduce the likelihood of graft occlusion. Incorporating QFR into routine surgical planning may enhance long-term graft patency and improve patient outcomes, although prospective validation is warranted.
This study has several limitations. First, its retrospective design may have included unmeasured confounding factors. Baseline differences, such as less use of cardiopulmonary bypass in the individual group, may also have introduced some bias in patency comparisons, as the choice of on-pump or off-pump grafting was based on coronary anatomy and surgical judgment. However, all procedures were performed by highly experienced surgeons who adhered to standardized protocols. Additionally, sequential anastomosis remained as an independent risk factor for occlusion after the incorporation of variables into the multivariate model. Second, some patient selection bias for RA grafting may have occurred. However, our imaging follow-up was planned and not symptom-driven, and up to 75.4% of patients successfully completed postoperative imaging follow-up. Follow-up of incomplete and non-uniform imaging may introduce bias, despite the use of time-to-event analyses that account for censoring. Third, the limited sample size and relatively short follow-up gave rise to a low incidence of MACCEs, particularly in the sequential group, making it difficult to assess the impact of RA occlusion on clinical outcomes.
Compared to individual RA bypass grafting, sequential RA was associated with inferior graft patency after CABG. Multiple target options exist for sequential grafts, and inappropriate selection may result in increased competition of blood flow and subsequent failure of the RA graft.
CABG, coronary artery bypass grafting; RA, radial artery; ITA, internal thoracic artery; SVG, saphenous vein graft; QFR, quantitative flow ratio; CCTA, coronary computed tomography angiography; MACCEs, major adverse cardiac or cerebrovascular events; IQR, interquartile range; LAD, left anterior descending; 95% CI, 95% confidence interval; aHR, adjusted hazard ratio.
The data underlying this article cannot be shared publicly due to the policy of data sharing of our centre. The data will be shared on reasonable request to the corresponding author.
SZ, ZH, and ZZ contributed to the conception and design of the study. SZ and CW performed the data analysis. SZ drafted the manuscript. ZH, YZ, and ZZ provided critical revisions to the manuscript. All authors contributed to the conception and editorial changes in the manuscript. All authors participated in the editing process and approved the final version of the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was carried out in accordance with the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Fuwai Hospital (No. 2021-1554). Due to the retrospective nature of the study, written informed consent was waived.
We gratefully acknowledge the assistance and instruction from professor Zhihui Hou and Lei Song of the Department of Radiology and the Department of Cardiology, Fuwai Hospital.
This study was supported by grants from National High Level Hospital Clinical Research Funding (2024-GSP-TJ-01), Beijing Natural Science Foundation - Fengtai Innovation Joint Fund (L251022), and the high-level hospital clinical research of Fuwai Hospital, Chinese Academy of Medical Sciences (2023-GSP-RC-14,2023-GSP-QN-27).
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/RCM39689.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.



