1 Guangdong Cardiovascular Institute, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, 511436 Guangzhou, Guangdong, China
2 Guangdong Provincial Key Laboratory of Clinical Pharmacology, Guangdong Provincial People's Hospital, Guangdong Academy of Medical Sciences, 511436 Guangzhou, Guangdong, China
3 Department of Geriatrics, Guangdong Provincial People’s Hospital, Institute of Geriatrics, Guangdong Academy of Medical Sciences, 511436 Guangzhou, Guangdong, China
†These authors contributed equally.
Abstract
Background: The reported anticoagulation rate may be overestimated
among Chinese patients with atrial fibrillation (AF). Therefore, we aimed to
understand the current status and time trends of anticoagulation among older
people in the Chinese community. Methods: Data were obtained from the
physical examination program for the elderly (aged
Keywords
- atrial fibrillation
- anticoagulation
- older people
- China
Atrial fibrillation (AF) is the most common sustained arrhythmia with a global prevalence of approximately 2%–4% [1]. Prevalence is expected to increase even further owing to the increased longevity of the general population, ineffective control of risk factors, and improved diagnostic capabilities [2, 3]. AF can significantly increase the risk of stroke [4]. Compared to stroke without AF, AF-related stroke is more fatal and disabling [5]. Oral anticoagulants (OACs) are recommended to reduce the thromboembolic risk in AF patients with moderate to high stroke risks [6]. Previous studies suggested that more than 50% of AF patients with high risks of stroke were treated with OACs in developed countries [7, 8, 9], while in China, only 36.5% were reported to be treated with OACs [10].
However, since most of the available data are from medical institutions with high-quality health care, the current status of OACs in China may even be overestimated. At present, the medical level in China lags behind that of developed Western countries, and the distribution of medical resources is uneven. Owing to the large population and limited quality of medical resources, the task of diagnosing and treating common diseases in China mainly depends on primary community health institutions. Therefore, data from primary community health institutions may more accurately reflect the current anticoagulation status. To this end, we sought to increase the understanding of anticoagulation among older people with nonvalvular atrial fibrillation (NVAF) in Chinese communities by analyzing the physical examination data from primary community health institutions.
Data were obtained from the physical examination program for older people in Guangzhou, southern China. The project was funded by the local government and conducted at primary community health institutions annually. People over the age of 65 voluntarily participated. This project aimed to understand the health profile of older people and assist in the development of efficient public health strategies for geriatric chronic diseases. Information, such as sociodemographic characteristics, medical history, laboratory tests including blood routine, liver and kidney function, electrolytes, lipids, electrocardiogram (ECG), and chest radiograph, was collected from participants. The collection and aggregation of data are the responsibility of the local Center for Disease Control and Prevention (CDC).
With the authorization of the local government and CDC, this study obtained physical examination data from older people between 2017 and 2020 in the Yuexiu District of Guangzhou. Approved by the ethics committee of Guangdong Provincial People’s Hospital, this study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines. Since the information was retrospectively collected, the requirement for informed consent was waived. The permanent population of Yuexiu District is around 1.15 million, with 13% of the population aged 65 and above. There are 18 primary community health institutions in the area. During 2017–2020, a total of 31,829, 58,573, 55,483, and 54,845 older people underwent annual physical examinations in the Yuexiu District, respectively. General information (e.g., sex, age, body mass index (BMI)), AF-related medical history (e.g., hypertension, diabetes mellitus, coronary artery disease, heart failure, stroke, vascular disease), and use of OACs were collected for analysis.
Baseline characteristics were reported as proportions for categorical variables
and mean
Annual patient characteristics for each year between 2017 and 2020 are
summarized in Table 1. From 2017 to 2020, the estimated annual prevalence of
older people with NVAF in Guangzhou was 0.99%, 0.92%, 1.05%, and 1.14%,
respectively (Fig. 1). The proportion in males gradually increased, while the
proportion of older people over 75 years old gradually decreased (p
| Year | p-value | ||||
| 2017 (n = 316) | 2018 (n = 538) | 2019 (n = 585) | 2020 (n = 623) | ||
| Age ( |
192 (60.8) | 334 (62.1) | 326 (55.7) | 337 (54.1) | 0.021 |
| Female | 170 (53.8) | 265 (49.3) | 270 (46.2) | 274 (44.0) | 0.027 |
| Heart failure | 10 (3.2) | 31 (5.8) | 47 (8.0) | 27 (4.3) | 0.007 |
| Hypertension | 200 (63.3) | 356 (66.2) | 402 (68.7) | 431 (69.2) | 0.245 |
| Diabetes | 76 (24.1) | 125 (23.2) | 157 (26.8) | 149 (23.9) | 0.507 |
| Stroke/TIA | 36 (11.4) | 66 (12.3) | 89 (15.2) | 76 (12.2) | 0.276 |
| Coronary heart disease | 117 (37.0) | 208 (38.7) | 214 (36.6) | 201 (32.3) | 0.130 |
| Peripheral vascular disease | 7 (2.2) | 10 (1.9) | 8 (1.4) | 9 (1.4) | 0.749 |
| CHA2DS2-VASc score |
283 (89.6) | 488 (90.7) | 529 (90.4) | 550 (88.3) | 0.515 |
TIA, transient ischemic attack; NVAF, nonvalvular atrial fibrillation.
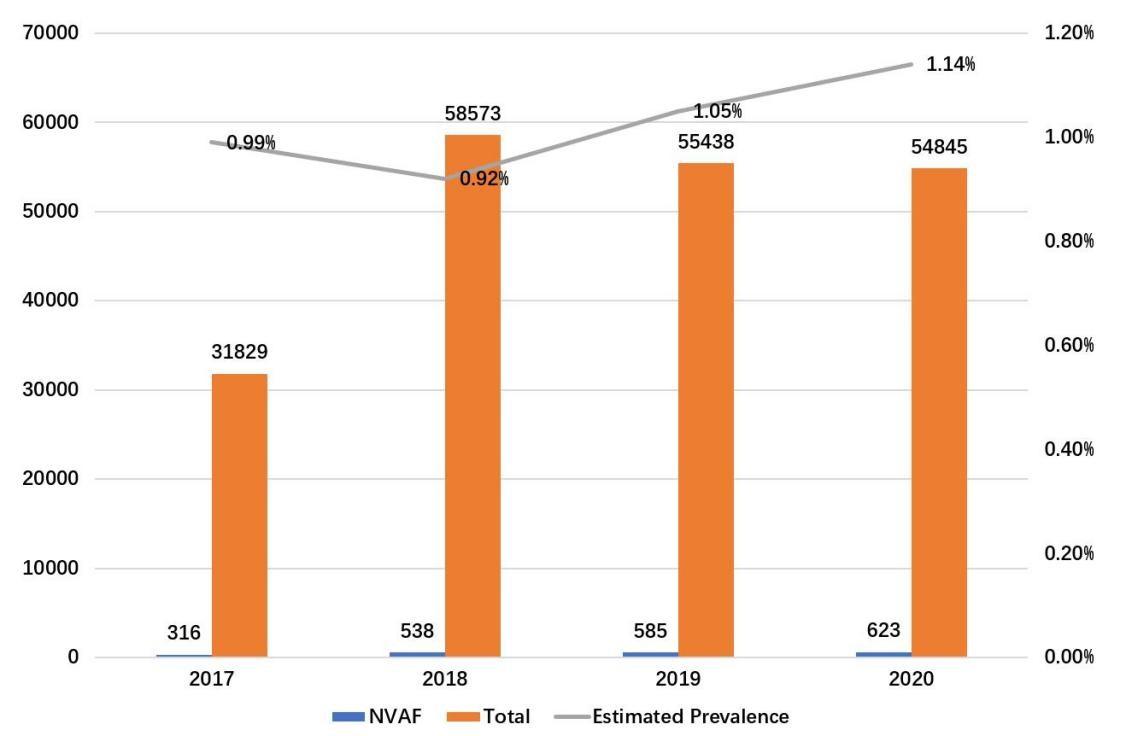 Fig. 1.
Fig. 1.The annual prevalence of NVAF. NVAF, nonvalvular atrial fibrillation.
Changes in anticoagulation use between 2017 and 2020 are summarized in Table 2.
Regardless of the patients’ CHA2DS2-VASc scores, the annual anticoagulation rates
among older people with NVAF were 3.16%, 3.16%, 5.64%, and 5.62%,
respectively. No significant difference was shown in the overall anticoagulation
rate. In patients with high stroke risk (CHA2DS2-VASc score
| Year | p-value | |||||
| 2017 (n = 316) | 2018 (n = 538) | 2019 (n = 585) | 2020 (n = 623) | |||
| Anticoagulation rate (%) | 3.16 (10/316) | 3.16 (17/538) | 5.64 (33/585) | 5.62 (35/623) | 0.074 | |
| Anticoagulation rate (%) in CHA2DS2-VASc |
2.83 (8/283) | 2.05 (10/488) | 5.29 (28/529) | 5.82 (32/550) | 0.007 | |
| OACs | 0.004 | |||||
| Warfarin | 8 | 15 | 21 | 14 | ||
| NOACs | 2 | 2 | 12 | 21 | ||
| Antiplatelet drugs | 25 (7.9) | 52 (9.7) | 70 (12.0) | 68 (10.9) | —— | |
OACs, oral anticoagulants; NOACs, non-vitamin K antagonist oral anticoagulants.
According to current guidelines, OACs should be considered for NVAF patients with CHA2DS2-VASc scores = 1 (male) or = 2 (female) [6]. Factors associated with OAC use were determined by stepwise multiple logistic regression analysis. Males (OR, 0.556; 95% CI, 0.362–0.855; p = 0.008), ages over 75 (OR, 0.538; 95% CI, 0.351–0.825; p = 0.005), low education levels (OR, 0.576; 95% CI, 0.375–0.883; p = 0.011), and lacking the ability for self-care (OR, 0.226; 95% CI, 0.054–0.937; p = 0.041) were less likely to receive OAC therapy (Table 3).
| No anticoagulation (n = 1967) | Anticoagulation (n = 95) | p-value | OR (95% CI) | |
| Male | 1040 (52.9) | 43 (45.3) | 0.008 | 0.556 (0.362–0.855) |
| Married | 1567 (79.7) | 85 (89.5) | 0.217 | —— |
| Age ( |
1150 (58.5) | 39 (41.1) | 0.005 | 0.538 (0.351–0.825) |
| BMI | 24.2 |
23.8 |
0.052 | —— |
| CHA2DS2-VASc |
1772 (90.1) | 78 (82.1) | 0.237 | —— |
| Alcohol | 1785 (90.8) | 82 (86.3) | 0.190 | —— |
| Smoking | 261 (13.3) | 11 (11.6) | 0.468 | —— |
| Exercise | 1293 (65.7) | 64 (67.4) | 0.326 | —— |
| Education (under high school) | 1276 (64.9) | 50 (52.6) | 0.011 | 0.576 (0.375–0.883) |
| Without medical insurance | 48 (2.4) | 3 (3.2) | 0.616 | —— |
| Lacking self-care ability | 208 (10.6) | 2 (2.1) | 0.041 | 0.226 (0.054–0.937) |
BMI, body mass index; OACs, oral anticoagulants; OR, odds ratio.
The present study is the first to examine trends in NVAF prevalence and OAC
therapy for older people in China using data obtained from primary community
health institutions. We found that the prevalence of NVAF in Guangzhou was around
1%, which was lower than previously reported [1]. According to the results of a
previous epidemiological study in Guangzhou, the prevalence of AF in people over
60 was over 1.65%, while the prevalence in people aged 80 years and above was
5.0% [11]. Since there is a higher risk of significant mitral calcification or
degenerative valve disease in older populations, it may limit the population from
being diagnosed with NVAF [12]. Although the use rate of OACs among patients with
high-risk NVAF (CHA2DS2-VASc score
Several studies suggested that the anticoagulation rate in the Chinese community was only 2.2%–7.8% from 2010 to 2016 [15, 16, 17], which was much lower than reported in the US and Europe [18]. The present study found that the anticoagulation rate in the community was only 5.8%, according to data from Guangzhou during 2017–2020. Since there was no obvious improvement in the low anticoagulation rate during this period, the status of OAC use in the Chinese community remains a concern. According to the results of a previous survey, which we conducted in the community of Guangzhou, multiple factors may contribute to the insufficient anticoagulation treatment observed in the community. First, standardized training in AF management is lacking among physicians in the community. Second, there is no NOAC and coagulation monitoring equipment in primary community health institutions. Additionally, concerns over bleeding impair the willingness of physicians and patients to use OACs. Finally, antiplatelet agents have been inappropriately used in China to prevent stroke among patients with AF [19]. In the present study, 8–11% of patients were still prescribed antiplatelet agents for stroke prevention. However, the use of antiplatelet agents is neither safe nor effective for preventing stroke in patients with AF [20].
In China, a large number of patients in the community with AF remain exposed to
the risk of stroke because of a lack of anticoagulants. Therefore, it is
necessary to establish an appropriate mode of anticoagulant management for
patients in the community with AF. Multiple effective modes of anticoagulant
management have been explored in the community, similar to those in the US and
Europe [21, 22, 23, 24]. Among them, National programs promoted by the UK and Canada seem
to be effective modes that can increase the anticoagulation rate and improve
quality of life [25, 26]. Notably, stepwise multiple logistic regression analysis
suggested that being male, advanced in age (
There were several limitations in this study. First of all, since the data were collected from Guangzhou, an economic center in China, the results are not fully representative of the whole country, especially in less-developed regions. Therefore, it may lack generalizability outside of China. Second, this study only analyzed the current status and time trends of oral anticoagulation use in older people, those aged over 65 years old. Finally, this study was not able to analyze the duration of anticoagulation use and changes in OAC selection for each patient because of limitations in the data.
In conclusion, the low anticoagulation rate in older people with NVAF in the
Chinese community has not significantly improved in recent years, with only
5.82% of patients with high stroke risk (CHA2DS2-VASc score
The data that support the findings of this study are available from Health Bureau and CDC of Yuexiu District but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Health Bureau and CDC of Yuexiu District. If necessary, please contact Junrong Jiang (571023647@qq.com).
YW, JJ and JH have contributed equally to this work. YX and SW conceived the study and drafted the manuscript. YW, JJ and JH collected data, drafted and revised the manuscript. HL, HD, XZ and XF analyzed data, interpreted results and revised the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
The study was approved by the ethics committee of Guangdong Provincial People’s Hospital (KY-H-2021-036-01) and was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines. The data was obtained with the authorization of Health Bureau and CDC of Yuexiu District. Humans are not directly involved and only data is used in this study. The requirement for informed consent from patients whose information was retrospectively collected was waived with the consent of the ethics committee of Guangdong Provincial People’s Hospital.
Not applicable.
This work was supported by the Science and Technology Programs of Guangdong Province (No.2019B020230004), National Natural Science Foundation of China (No.81870254) and the ZHONGNANSHAN MEDICAL FOUNDATION OF GUANGDONG PROVINCE (grant number NO.202151).
The authors declare no conflict of interest.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

