1 Department of Pharmacy, China Aerospace Science & Industry Corporation 731 Hospital, 100074 Beijing, China
2 Department of Medical, China Aerospace Science & Industry Corporation 731 Hospital, 100074 Beijing, China
3 Department of Cardiovascular Medicine, Beijing Hospital, National Center of Gerontology, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, 100730 Beijing, China
Abstract
Hypertrophic cardiomyopathy (HCM) is a common hereditary cardiomyopathy. Mavacamten, a first-in-class cardiac myosin inhibitor, is considered to be a specific drug for the treatment of HCM. This meta-analysis aimed to assess the efficacy and safety of mavacamten in patients with HCM.
PubMed, Cochrane Library, Embase and Clinical Trials.gov databases were searched from inception to February 6, 2024 for randomized controlled trials (RCTs) which compared the efficacy and safety between mavacamten and placebo in treating HCM.
Six RCTs involving 732 patients were included in this meta-analysis. This meta-analysis showed that mavacamten improved the New York Heart Association (NYHA) function class [risk ratios (RR): 2.21, 95% confidence interval (CI): 1.48 to 3.30, p = 0.00001], Clinical Summary Score of the Kansas City Cardiomyopathy Questionnaire (KCCQ-CSS) scores [mean difference (MD): 9.33, 95% CI: 7.09 to 11.57, p < 0.00001] and composite functional end point (RR: 1.86, 95% CI: 1.25 to 2.78, p = 0.002). Meanwhile, mavacamten decreased N-terminal pro-B-type natriuretic peptide (NT-proBNP) (MD: –492.28, 95% CI: –611.55 to –373.02, p < 0.00001), cardiac troponin I (cTnI) (MD: –14.58, 95% CI: –26.98 to –2.17, p = 0.02) and Valsalva left ventricular outflow tract (LVOT) gradient (MD: –57.96, 95% CI: –82.15 to –33.78, p < 0.00001). The results for the incidence of ≥1 total emergent adverse event (TEAE) and ≥1 serious adverse event (SAE) showed that there was no significant difference between both groups (RR: 1.9, 95% CI: 0.97 to 1.24, p = 0.16) (RR: 1.06, 95% CI: 0.46 to 2.44, p = 0.90).
Mavacamten has great efficacy for the treatment of HCM. Meanwhile, mavacamten did not increase the incidence of adverse events or serious adverse events.
Keywords
- hypertrophic cardiomyopathy
- mavacamten
- meta-analysis
- cardiac myosin inhibitor
Hypertrophic cardiomyopathy (HCM) is considered an autosomal dominant genetic disease caused by a sarcomere protein gene mutation, which is the most common hereditary cardiac condition featuring disorganized architecture of the myocardium and left ventricular hypertrophy [1, 2, 3]. The prevalence of HCM is 0.2% in the general population, and HCM is the primary cardiac cause of sudden cardiac death [4].
The pathogenic mechanism of HCM is highly complex, and is associated with
Traditional medication treatments of HCM are not disease-specific, HCM medical therapy depends on the patient’s clinical picture and remains limited to beta adrenergic blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, antiarrhythmics, diuretics and oral anticoagulants [5, 6].
Mavacamten (MYK-461), a selective and reversible cardiac myosin inhibitor, is a
novel
This study aimed to perform a meta-analysis to assess the efficacy and safety of mavacamten in treating HCM from available RCTs. By synthesizing the results of all published RCTs, the efficacy and safety of mavacamten in treating HCM can be more certain. This meta-analysis will also provide guidance and direction for future research on mavacamten and its role in HCM.
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) and Cochrane Handbook [9, 10]. We registered the review prospectively in Open Science Frameworks, https://osf.io/qryds/.
PubMed, Cochrane Library, Embase and Clinical Trials were searched from inception to February 6, 2024, without language restrictions. The detailed search strategy of all databases can be seen in Supplementary Text S1. Searched terms were “mavacamten”, “MYC-461”, “camzyos”, “hypertrophic cardiomyopathy”, “hypertrophic obstructive cardiomyopathy”, “familial hypertrophic cardiomyopathy”, “HCM”, “HOCM”. We searched all published papers related to mavacamten, including systematic reviews and meta-analysis.
We included human studies in this study if they met the following eligibility criteria: (1) the study was an RCTs; (2) patients in the included studies were diagnosed with HCM; (3) the intervention group received mavacamten and the control group received placebo; (4) the studies reported at least one of the outcomes of interest.
If the study was a review, case reports, non-RCTs, letter, abstracts and articles with insufficient data, it was excluded
All study search records were imported into the Rayyan software (Qatar Computer Research Institute, https://www.rayyan.ai/). Two authors (YMC and XTG) independently screened the papers and accessed all articles based on the title and abstract. When there was uncertainty about whether a study met the inclusion criteria, the same two authors read the full text to confirm the relevance. Disagreements were resolved by a third author (DPL) via discussion.
Two authors (LZ and XTG) independently extracted the data into a spreadsheet for
analysis. Any discrepancies were resolved by discussion. The following data were
extracted from eligible studies: first author’s last name, publication time,
research design, duration of intervention, patient baseline characteristics,
improvement in
Two authors (LZ and YMC) independently assessed the risk of bias of the included RCTs using the Cochrane Risk of Bias Tool (RoB2) [11]. Any discrepancies were resolved by mutual consensus or adjudicated by a third reviewer (DPL).
This meta-analysis was performed by Review Manager (RevMan) 5.3 (Nordic Cochrane Centre, Copenhagen, Denmark). Dichotomous outcomes were assessed by risk ratios (RR) while the mean difference (MD) was employed to express the continuous outcomes data, with 95% confidence intervals (CI). We used I2 to assess heterogeneity between included RCTs, with an I2 of greater than 50% indicating at least moderate heterogeneity. Based on the assumption of considerable clinical heterogeneity, the random-effects model was used for this meta-analysis.
A total of 533 studies were obtained from the above-mentioned database. Among them, 176 articles were deleted due to duplication and 321 studies were excluded based on titles and abstracts. At last, 6 studies met the inclusion criteria (Fig. 1).
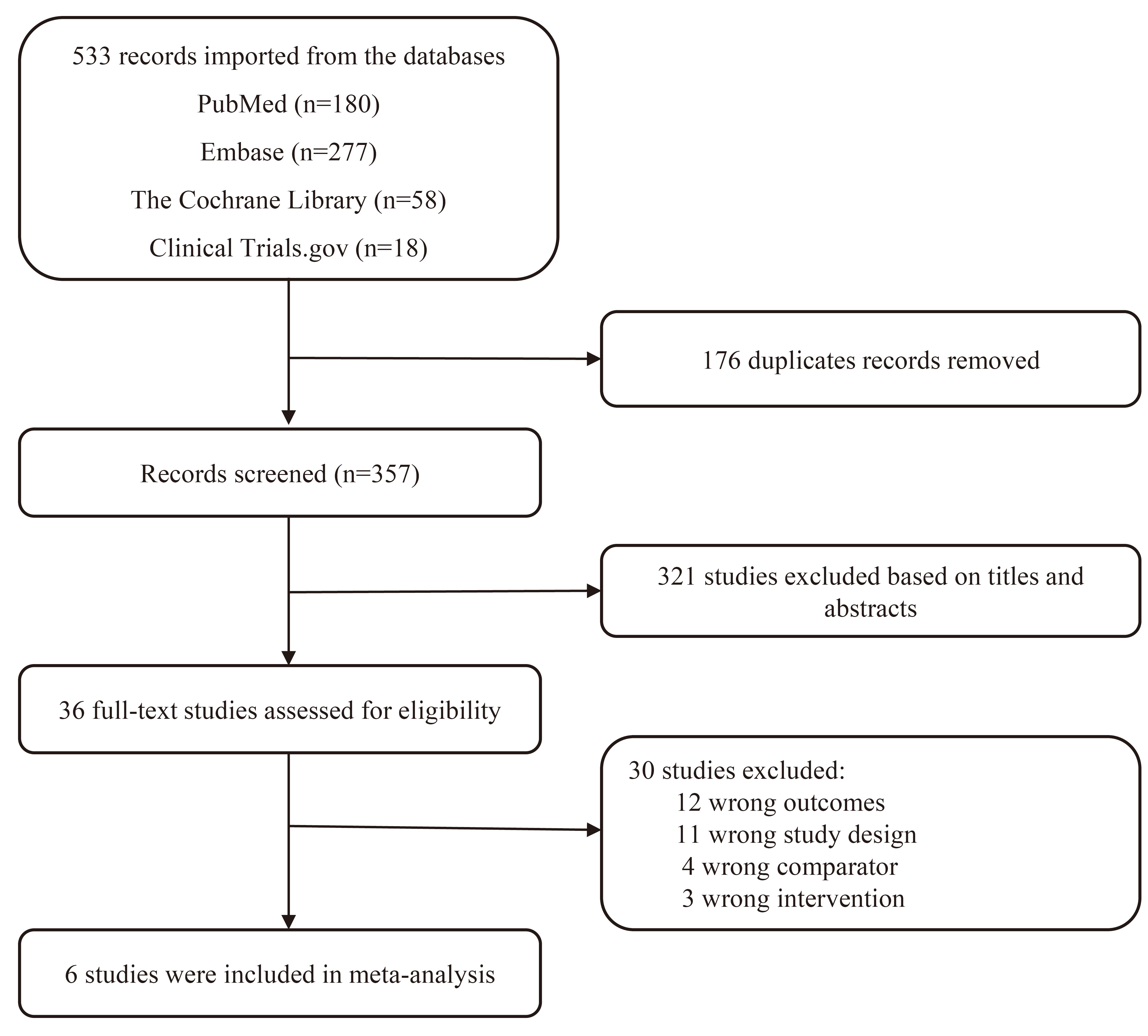 Fig. 1.
Fig. 1.
Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) flowchart of the study screen.
The 6 included RCTs [12, 13, 14, 15, 16, 17] were comprised of 732 patients with HCM, of whom 388 received mavacamten and 344 received placebo. Five of the RCTs [13, 14, 15, 16, 17] were performed in obstructive HCM and one RCT [12] was performed in non-obstructive HCM. The mean age of patients was above 40 years old in these included RCTs. In this meta-analysis, most baseline characteristics were similar in either group. Table 1 (Ref. [12, 13, 14, 15, 16, 17]) presented more characteristics of the included RCTs.
| Study | Research design | Patients type | Interventions | No. | Average age (y) | Dose of medication | Duration of treatment (weeks) |
| Ho et al. 2020 [12] | a multicenter, double-blind, placebo-controlled, dose-ranging phase II study | non-obstructive hypertrophic cardiomyopathy | mavacamten | 40 | 54.0 |
200 or 500 ng/mL once a day | 16 |
| placebo | 19 | 53.8 |
placebo | ||||
| Saberi et al. 2021 [13] | a randomized, double-blind, placebo-controlled, phase III trial | obstructive hypertrophic cardiomyopathy | mavacamten | 17 | 60.3 | 2.5, 5, 10, or 15 mg once a day | 30 |
| placebo | 18 | placebo | |||||
| Olivotto et al. 2020 [14] | a randomized, double-blind, placebo-controlled, phase III trial | obstructive hypertrophic cardiomyopathy | mavacamten | 123 | 58.5 |
2.5, 5, 10, or 15 mg once a day | 30 |
| placebo | 128 | 58.5 |
placebo | ||||
| Spertus et al. 2021 [15] | a randomized, double-blind, placebo-controlled, phase III trial | obstructive hypertrophic cardiomyopathy | mavacamten | 98 | 57.8 |
15 mg/d | 30 |
| placebo | 96 | 58.2 |
placebo | ||||
| Desai et al. 2022 [16] | a multicenter, randomized, double-blind, placebo controlled, phase III trial | severe obstructive hypertrophic cardiomyopathy | mavacamten | 56 | 59.8 |
2.5, 5, 10, or 15 mg once a day | 16 |
| placebo | 56 | 60.9 |
placebo | ||||
| Tian et al. 2023 [17] | randomized, double-blind, placebo-controlled, phase III trial | obstructive hypertrophic cardiomyopathy | mavacamten | 54 | 52.4 |
1, 2.5, 5, 10, or 15 mg once a day | 30 |
| placebo | 27 | 51.0 |
placebo |
Table 2 (Ref. [12, 13, 14, 15, 16, 17]) showed the risk of bias of the RCTs in this meta-analysis. 1 included study [12] was judged at probably low risk of bias. Overall, the quality of the included RCTs in this meta-analysis was high and illustrated a low risk of bias.
| Study | Bias arising from the randomization process | Bias due to deviations from the intended intervention | Bias due to missing outcome data | Bias in measurement of the outcome | Bias in selection of the reported results | Other risk of bias | Overall judgement |
| Ho et al. 2020 [12] | Low | Probably Low | Low | Low | Probably Low | Probably Low | Probably Low |
| Saberi et al. 2021 [13] | Low | Low | Low | Low | Probably Low | Low | Low |
| Olivotto et al. 2020 [14] | Low | Low | Low | Low | Probably Low | Low | Low |
| Spertus et al. 2021 [15] | Low | Low | Low | Low | Probably Low | Low | Low |
| Desai et al. 2022 [16] | Low | Low | Low | Low | Probably Low | Low | Low |
| Tian et al. 2023 [17] | Low | Low | Low | Low | Probably Low | Low | Low |
RCTs, randomized clinical trials.
4 RCTs [12, 14, 16, 17] reported the improvement of
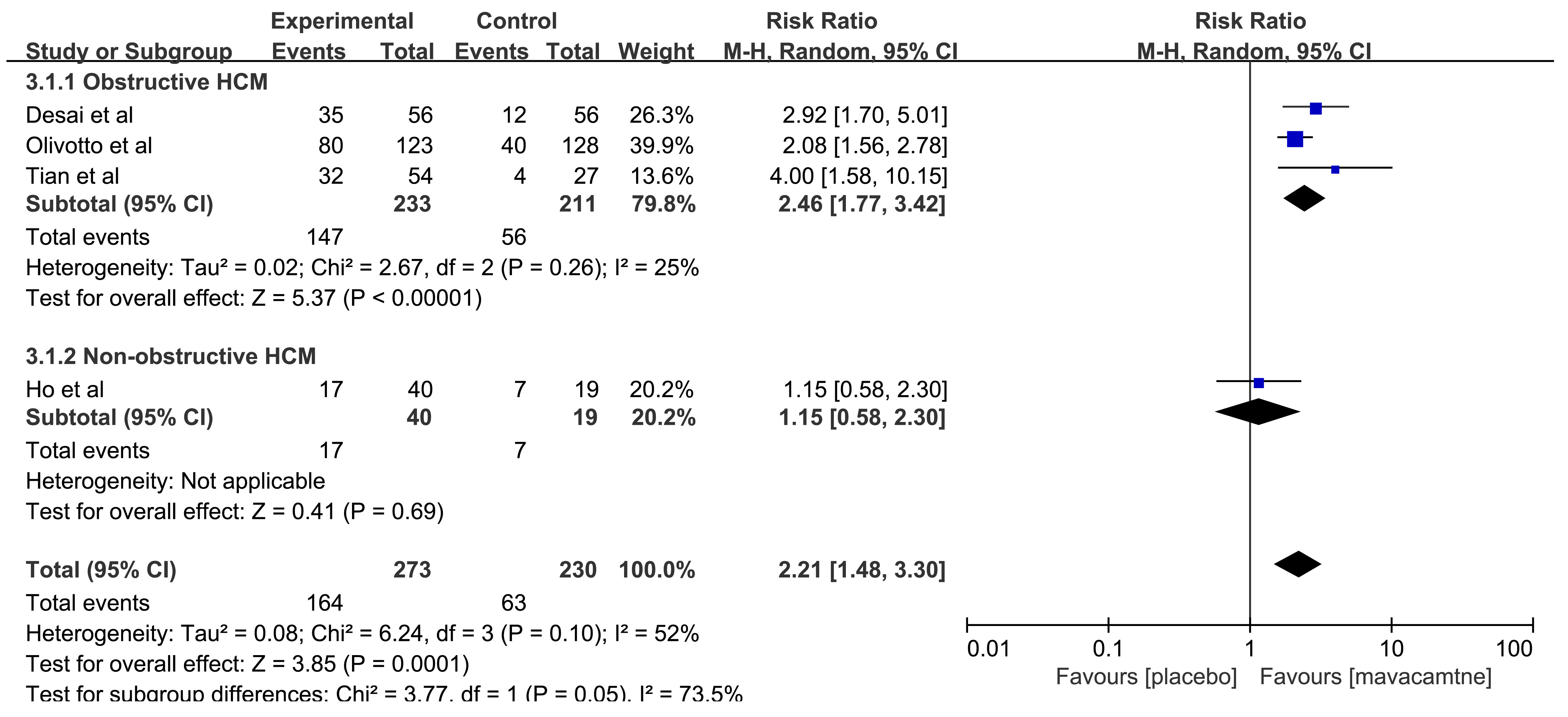 Fig. 2.
Fig. 2.
Forest plot for improvement
3 RCTs [12, 16, 17] reported the effect of mavacamten on NT-proBNP. Two RCTs
[16, 17] compared the changes in NT-proBNP from the baseline
(
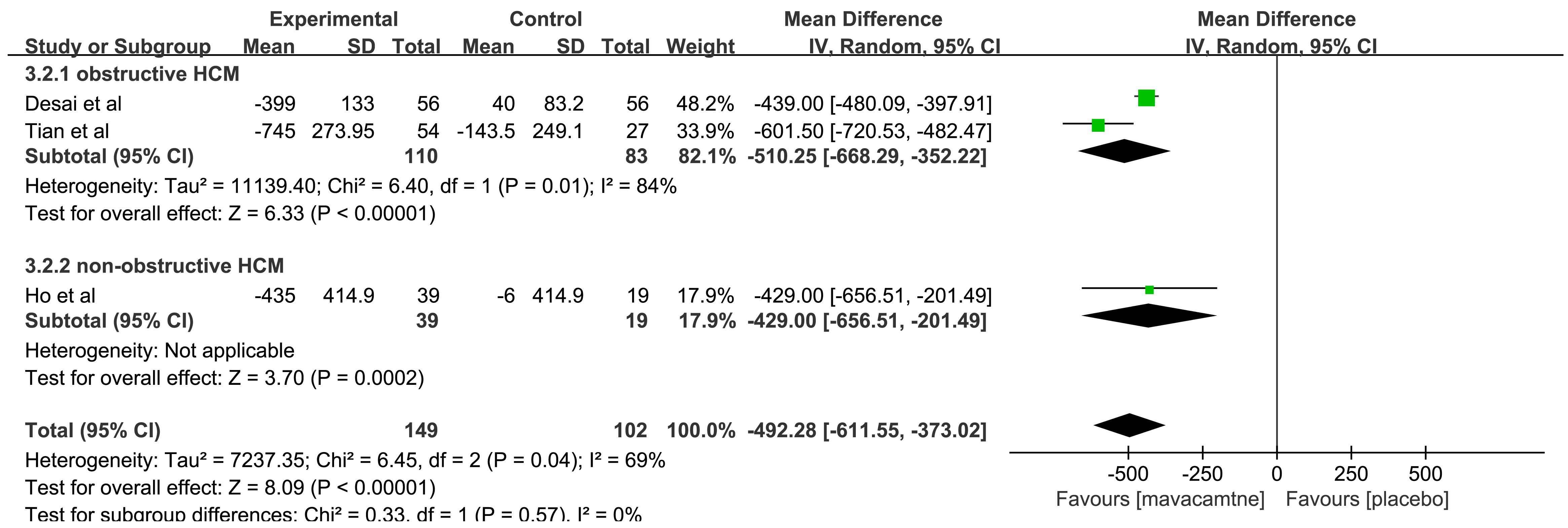 Fig. 3.
Fig. 3.
Forest plot for change in N-terminal pro-B-type natriuretic
peptide (
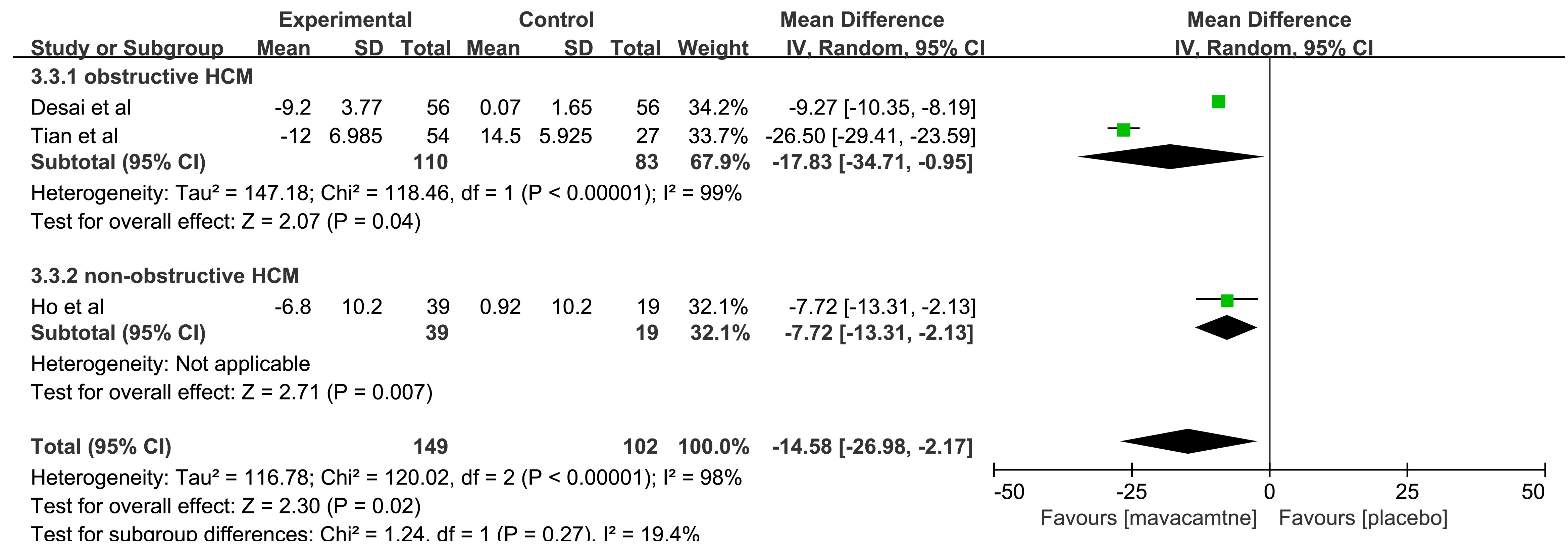 Fig. 4.
Fig. 4.
Forest plot for change from baseline in cardiac troponin I
(
The aggregated results [12, 14, 16] showed that mavacamten can significantly improve the composite functional end points (RR: 1.86, 95% CI: 1.25 to 2.78, p = 0.002, Fig. 5). The subgroup results showed no significant difference in the composite functional end points among the non-obstructive HCM (RR: 1.07, 95% CI: 0.38 to 3.03, p = 0.90). However, in obstructive HCM, mavacamten improved the composite functional end points higher than that in placebo (RR: 2.05, 95% CI: 1.33 to 3.16, p = 0.001).
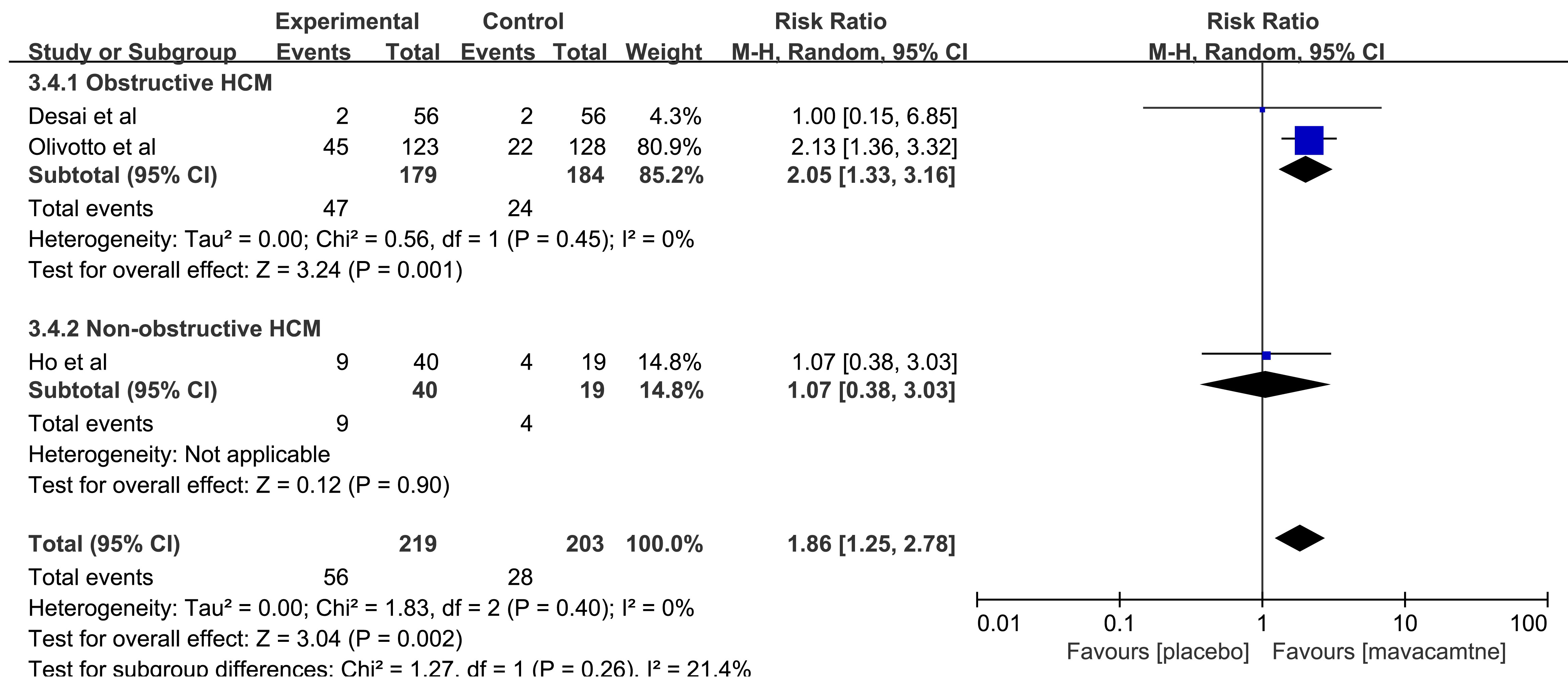 Fig. 5.
Fig. 5.
Forest plot for composite functional end point, including two subgroups: obstructive hypertrophic cardiomyopathy (HCM) and non-obstructive HCM. M-H, Mantel Haenszel method.
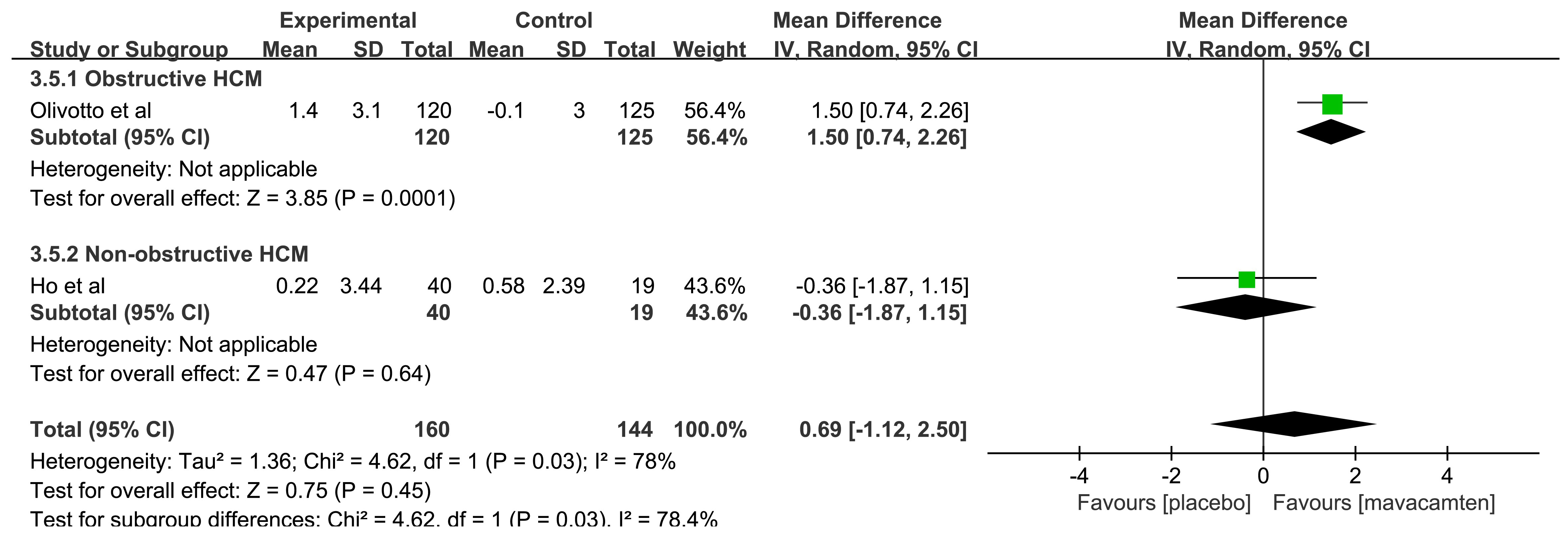 Fig. 6.
Fig. 6.
Forest plot for peak oxygen uptake (pVO2), including two subgroups: obstructive hypertrophic cardiomyopathy (HCM) and non-obstructive HCM. IV, inverse variance method.
In the included RCTs reporting KCCQ-CSS score, all patients involved were
obstructive HCM. The combined data [14, 15, 16, 17] for change from baseline in KCCQ-CSS
score showed a significant improvement with mavacamten (MD: 9.33, 95% CI: 7.09
to 11.57, p
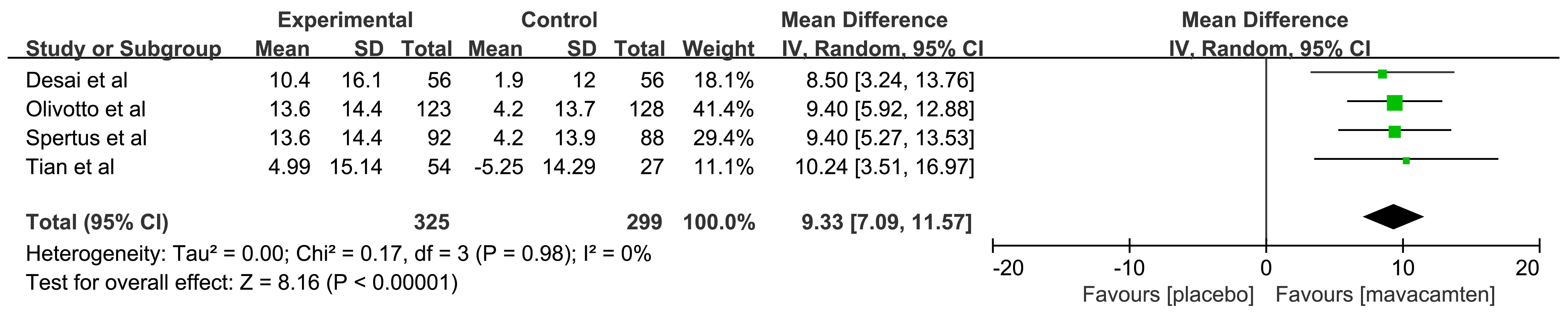 Fig. 7.
Fig. 7.
Forest plot for Clinical Summary Score of the Kansas City Cardiomyopathy Questionnaire (KCCQ-CSS). IV, inverse variance method.
In the included RCTs reporting the change in LVOT gradient induced by Valsalva
from baseline, all patients involved had obstructive HCM. With respect to the
change in LVOT gradient induced by Valsalva from baseline [16, 17], a significant
relationship was illustrated when mavacamten was compared with placebo (MD:
–57.96, 95% CI: –82.15 to –33.78, p
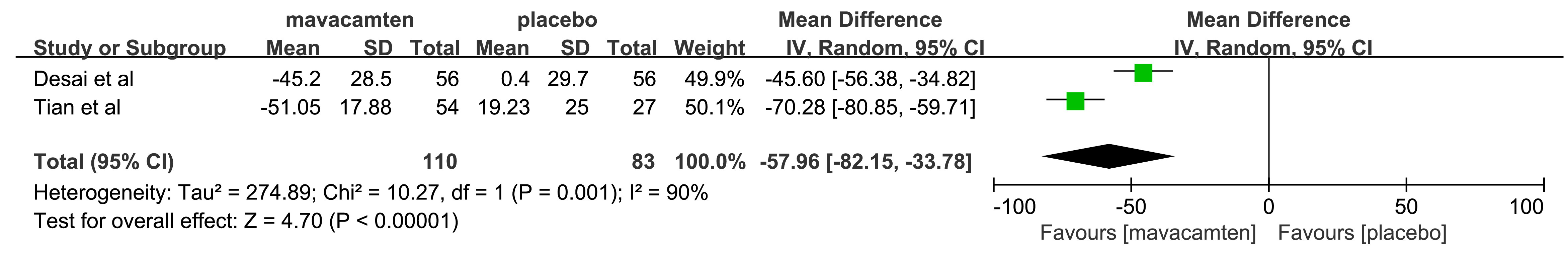 Fig. 8.
Fig. 8.
Forest plot for Valsalva left ventricular outflow tract (LVOT) gradient. IV, inverse variance method.
4 RCTs [12, 14, 16, 17] reported the data of patients with
The pooled results showed that there was no significant difference with the
rates of
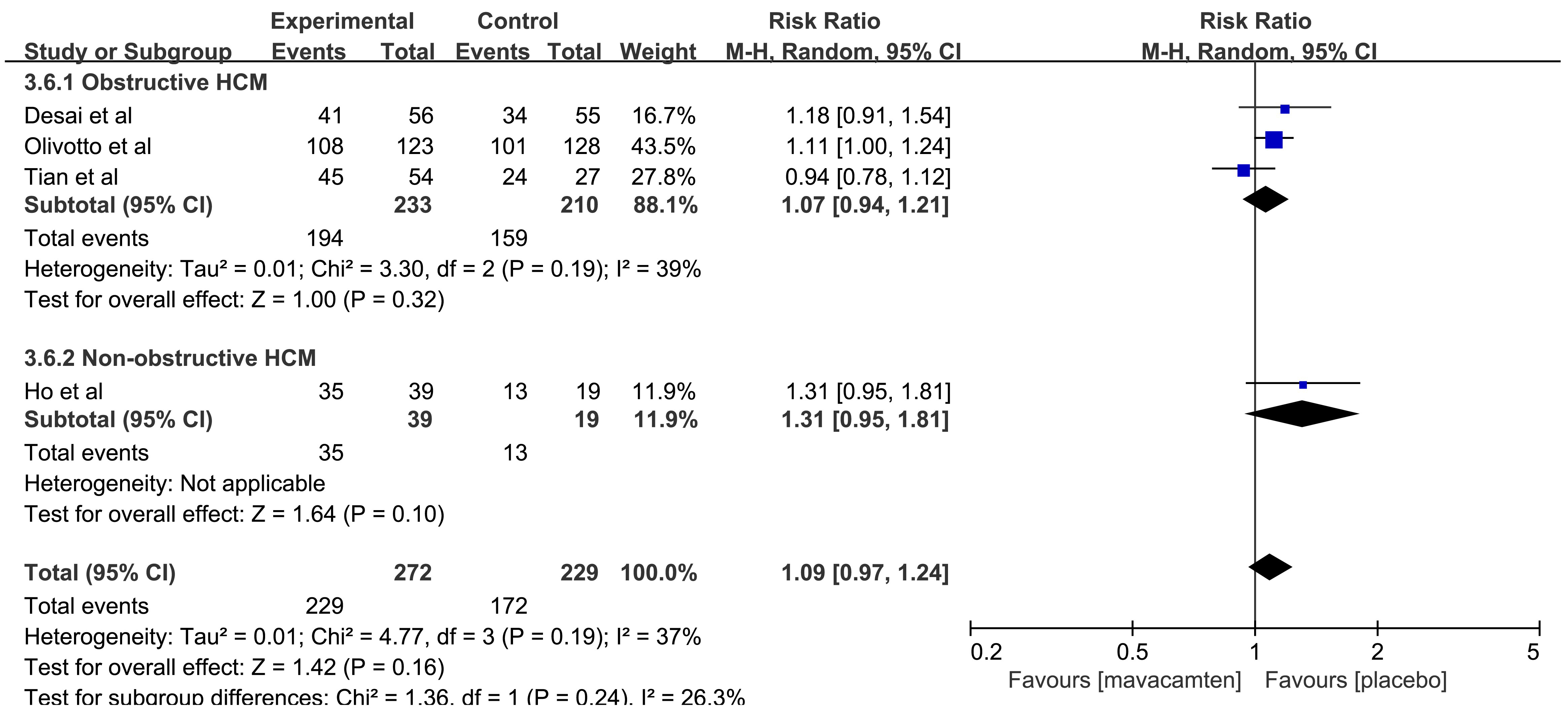 Fig. 9.
Fig. 9.
Forest plot of patients with
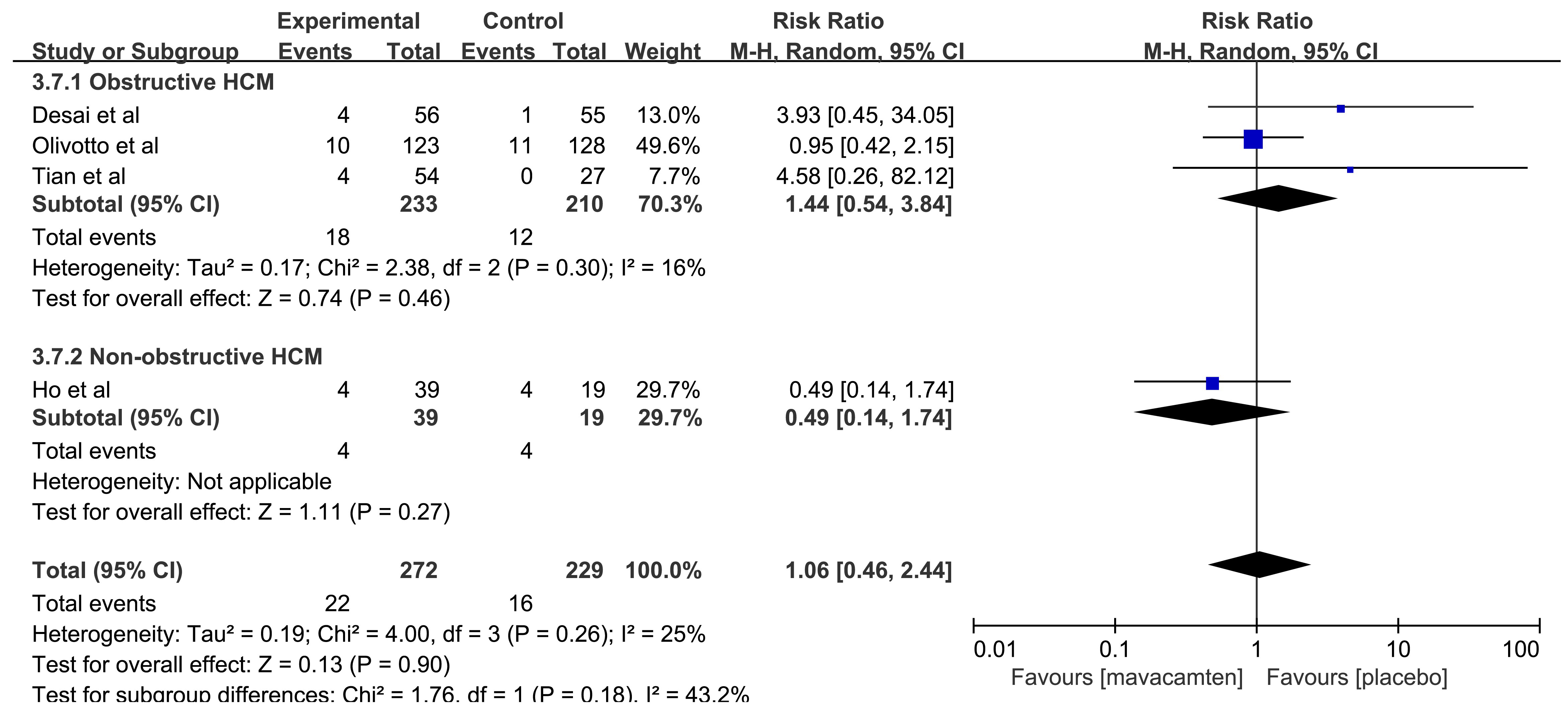 Fig. 10.
Fig. 10.
Forest plot of patients with
Several symptoms of TEAEs and SAEs were analyzed in this study, including palpitations, atrial fibrillation, dizziness, chest pain, infection, renal failure and so on. The detailed results are shown in Table 3.
| Type | Symptom | No. of studies (n) | Mavacamten group, n/n | Placebo group, n/n | Heterogeneity | RR | 95% CI | p |
| TEAEs | Palpitations | 2 | 8/95 | 5/74 | I2 = 0% | 0.97 | 0.34–2.82 | 0.97 |
| Atrial fibrillation | 2 | 5/95 | 1/74 | I2 = 0% | 2.23 | 0.38–13.13 | 0.38 | |
| Syncope | 2 | 3/67 | 1/75 | I2 = 0% | 3.39 | 0.53–21.65 | 0.20 | |
| Fatigue | 1 | 5/39 | 3/19 | NA | 1.81 | 0.22–3.05 | 0.76 | |
| Dizziness | 1 | 7/39 | 1/19 | NA | 3.41 | 0.45–25.77 | 0.23 | |
| Chest pain | 1 | 2/56 | 3/55 | NA | 0.65 | 0.11–3.77 | 0.64 | |
| SAEs | Atrial fibrillation | 4 | 8/272 | 5/229 | I2 = 0% | 1.06 | 0.34–3.33 | 0.92 |
| Infection | 2 | 2/179 | 2/183 | I2 = 0% | 0.97 | 0.14–6.56 | 0.98 | |
| Renal failure | 1 | 1/39 | 0/19 | NA | 1.50 | 0.06–35.19 | 0.80 |
RR, risk ratios; CI, confidence interval; TEAEs, total emergent adverse events; SAEs, serious adverse events; RCTs, randomized controlled trials; NA, not applicable.
6 RCTs [12, 13, 14, 15, 16, 17] allocating 732 patients diagnosed with HCM were included in this
meta-analysis. Among them, 673 patients were diagnosed with obstructive HCM, and
59 patients were diagnosed with non-obstructive HCM. The results of this study
provide evidence for the efficacy and safety of mavacamten for treating HCM. The
main finding as follows: (1) overall, mavacamten can achieve higher rates of
During our search in the above-mentioned databases, we found several
meta-analyses [8, 18, 19] have reported the effect and safety of mavacamten in the
treatment of HCM. The results of our study are consistent with the conclusions
stated in these 3 studies that mavacamten can effectively improve
Before the emergence of mavacamten, the treatment of HCM could only be achieved through non-specific drugs and surgery to improve symptoms and prevent sudden death. But, these therapies did not show any benefits in clinical trials [20]. The emergence of mavacamten has reversed this passive situation. Mavacamten can target and affect myosin, leading to a decrease in ATPase activity [21]. While improving the symptoms and signs of HCM, it can also prevent further disease progression, reduce ventricular wall tension, improve cardiac structure, and reduce heart damage [12, 14]. Mavacamten is a major advancement in HCM precision therapy, opening a new era of HCM treatment.
Due to the limitations of conventional drug therapy for HCM patients, the
emergence of a targeted drug named mavacamten is undoubtedly a ray of hope in the
darkness for HCM patients. However, as a cardiac myosin inhibitor, mavacamten
directly interferes with the contractile function of myocardial cells and
disturbs the processes involving energy production, storage, and utilization
within the myocardial cells. It also disrupts the uptake, release, and reuptake
of calcium ions within the myocardial cells, thereby affecting the
excitation-contraction coupling of the myocardium. This ultimately leads to a
decrease in myocardial contractility and relaxation of the heart muscle. While it
is effective in treating HCM, it can also result in a reduction in left
ventricular ejection fraction (LVEF). It is worth noting that the specific
pathological mechanism leading to a reduction in LVEF caused by mavacamten is
currently not fully understood. Although the mechanism of mavacamten has been
described, the specific cellular and molecular-level pathological changes have
not been completely elucidated. Fortunately, several RCT [12, 14, 16, 17] findings
have indicated that the LVEF reduction caused by mavacamten is reversible, and
the incidence rate is low. Out of the 6 RCTs included in this study, 3 RCTs
reported the effect of mavacamten on LVEF. Ho et al. [12] found that 5
cases of patients experienced a decrease in LVEF to below 45% after taking
mavacamten, but the LVEF recovered to above 50% after discontinuation of the
drug. Olivotto et al. [14] found that a total of 9 patients experienced
a decrease in LVEF after taking mavacamten. Among them, 5 patients had their LVEF
recovered to baseline levels after discontinuing mavacamten treatment, 3 patients
had their LVEF restored during the drug washout period at the end of the trial,
but 1 patient with concomitant atrial fibrillation opted for atrial fibrillation
ablation due to severe LVEF reduction and still had incomplete LVEF recovery at
the end of the trial. The research findings by Desai et al. [16] showed
that the resting LVEF remained stable throughout the entire treatment process,
with only 2 patients experiencing a decrease in LVEF after taking mavacamten.
These 2 patients resumed treatment without further adverse effects and remain in
the long-term extension study. Tian et al. [17] found that no patient
had an LVEF less than 50% or developed heart failure. The above results suggest
that mavacamten is generally well-tolerated, and in the few cases where there was
a decrease in LVEF, most patients were able to recover to normal levels after
discontinuing the medication. But the instructions for mavacamten (CAMZYOS) state
two precautions: (1) Initiation of CAMZYOS in patients with LVEF
The Food and Drug Administration (FDA) has approved mavacamten for the treatment of HCM, which can further expand the sample size of clinical studies and obtain more reliable data based on current clinical studies. Meanwhile, different from the race and living environment limitations of foreign clinical research samples, RCTs of mavacamten should be conducted on a large scale in the Asian region. Additionally, there are several aspects that need to be further explored regarding the research of mavacamten: (1) conduct clinical trial research with the main indicator of “hard endpoint”, such as reducing death, atrial fibrillation, and heart failure; (2) conduct clinical research on the correlation between mavacamten and the occurrence of arrhythmia; (3) conduct research on contraindications of mavacamten; (4) conduct research on interactions between mavacamten and other therapeutic drugs; (5) although there is no difference in the incidence of TEAE and SAEs between the mavacamten group and the placebo group in this study, the longest follow-up time of the included RCTs was only 30 weeks, and long-term monitoring is still needed in the future, which requires real-world observation and follow-up after marketing.
Compared with other meta-analyses [8, 18, 19], we have expanded the sample size and obtained results that are more informative, but our study still has several limitations. First, only 6 RCTs met our inclusion criteria as mavacamten is a new drug in the market. As a result, these findings may underestimate the efficacy and overestimate the safety of mavacamten. More RCTs with a large number of patients are needed to obtain a definite conclusion. Second, not all included RCTs reported the outcome indicators for evaluation, which further restricted the sample size for certain outcomes. Third, the longest follow-up time of the included RCTs was only 30 weeks, hence the value in predicting clinical effects is limited, and we have to rely on post-marketing safety surveillance systems for adverse events (AEs). Long term research data is needed to confirm the safety and efficacy of mavacamten. Nonetheless, our findings still provide preliminary evidence supporting favorable outcomes of mavacamten in treating HCM.
This meta-analysis found that mavacamten could improve the NYHA function class, KCCQ-CSS scores and composite functional end point. Meanwhile, mavacamten can decrease the NT-proBNP, cTnI and Valsalva LVOT gradient. This meta-analysis did not find any increased risk of AEs or SAEs following treatment with mavacamten. Further research should focus on a long-term follow up study to evaluate the efficacy and safety of mavacamten for the treatment of HCM.
The data presented in the study were included in the article or in its supplementary material.
LZ and DPL designed the research study. LZ and DPL performed the research. XTG and YMC screened studies. LZ and XTG extracted and analyzed the data. LZ and YMC performed the quality assessment of the included studies. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
Not applicable.
Not applicable.
This research received no external funding.
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.rcm2510375.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.










