1 Department of Cardiology, The Second Affiliated Hospital, Zhejiang University School of Medicine, Key Lab of Cardiovascular Disease of Zhejiang Province, 310009 Hangzhou, Zhejiang, China
Academic Editors: Brian Tomlinson and Fragasso Gabriele
Abstract
Background: Mitral regurgitation (MR) is one of the common
complications of heart failure (HF). The prevalence and characteristics of MR are
rarely investigated, especially in the Chinese population.
Objectives: The purpose of this study was to determine the
prevalence and characteristics of non-organic MR in HF patients and subgroups
defined by ejection fraction. Methods: A
single-center, hospital-based, and retrospective chart
review study included patients with heart failure admitted to the cardiovascular
department from January 2017 to April 2020. Demographic characteristics,
laboratory results, and echocardiogram results before discharge were analyzed in
different groups defined by left ventricular ejection fraction (EF) using
logistic regression and adjusted for confounders. Results: Finally, 2418 validated HF patients (age 67.2
Keywords
- functional mitral regurgitation
- heart failure
- prevalence
- associated factors
Heart failure (HF) remains a critical condition with a high global burden and poor prognosis [1, 2]. Mitral regurgitation (MR) following HF is distinguished by a structurally normal mitral valve and apparatus, which is frequently referred to as functional MR [3]. The prevalence of MR in HF patients ranges from 6.1% to 32.7% [4, 5]. It is associated with poor prognosis, high mortality rate, and worse life quality in HF patients [4, 5, 6, 7, 8, 9, 10].
Through the MitraClip system (Abbott Structural Heart), MR seemed to be a promising therapeutic target in patients with HF; however, two randomized clinical trials yielded opposite result on the major endpoint (hospitalization for heart failure or all-cause mortality) [11, 12]. The divergent inclusion criteria could have been attributed to the controversial results, and it raised many concerns [13]. Therefore, identifying the characteristics of MR is of growing importance.
The mechanisms underlying MR in heart failure include displacement of papillary muscles, tethering of chordae tendinae and leaflets, and annular dilation. Hence, MR is classified into the ventricle and the atrial types [3, 14]. Previous studies reported that sex, race, age, and dyslipidemia are associated with poor prognosis of MR [4, 6]. Population-based studies in HF, on the other hand, provided less clinical information concerning MR [1, 2, 15]. Hospital-based studies had reported the prevalence of MR in patients with HF, but these studies were limited to the specific types of HF and geographic regions; additionally, the clinical characteristics of MR in heart failure patients remained to be studied [4, 5, 6, 7, 8, 9, 10].
The purpose of this study was to determine the prevalence and characteristics of non-organic MR in HF patients and subgroups defined by ejection fraction. We identified the clinical characteristics of MR in a Chinese hospital based on these findings.
The Second Affiliated Hospital of Zhejiang University, Institutional Review Board approved this study and granted a waiver of informed consent. This study complied with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
It was a single-center, cross-sectional study based on the medical records in the electronic health record system. It included HF patients due to ischemic and non-ischemic etiology; the admission date was limited between January 2017 and April 2020. According to the ESC guideline, we selected and classified patients with heart failure based on symptoms description (dyspnoea, chest pain, palpitations, syncope, and edema) and test results [16].
(1) Heart failure with preserved ejection fraction (HFpEF):
LVEF
(2) Heart failure with mid-range ejection fraction (HFmrEF):
LVEF 41%–49%, symptoms
(3) Heart failure with reduced ejection fraction (HFrEF):
LVEF
We excluded organic valvular heart disease, apparent degenerative valve disease, congenital heart disease, hypertrophic cardiomyopathy, endocarditis, infiltrated cardiomyopathy, and pericardial disease. Patients without transthoracic echocardiography were also excluded. We classified regurgitation status using echocardiographic database records by the guideline [17]: patient with moderate or severe MR was defined as the MR group; patient with none or mild MR was defined as the non-MR group.
The clinical database was constructed based on the Electronic Medical Record System of the Second Affiliated Hospital of Zhejiang University. Generally, all admitted patients’ records (n = 27833) in the database were screened for detection. Probable HF hospitalizations (n = 4561) were eligible for inclusion. We excluded 773 patients who met the above-mentioned exclusion criteria, 900 patients who lacked echocardiogram data, 108 patients who lacked left atrium assessment data, and 162 patients who lacked NT-proBNP or BNP data. Finally, 2418 validated HF records from January 2017 to April 2020 were included. We did not use value imputation to fill in missing values. Two clinicians randomly selected twenty records for accuracy testing.
The most recent medical record was used as the baseline for patients with multiple admission records. Clinical data were extracted on patients’ clinical status, comorbidities, medication, intervention, laboratory results, and echocardiogram results prior to discharge when patients were hemodynamically stable. The etiology of HF was classified as either ischemic or non-ischemic. Thyroid disease was defined as thyroid disease diagnosed by a physician.
A standard echocardiogram was performed at the hospital before discharge
following the American Society of Echocardiography guidelines [18]. MR was
measured semi-quantitatively using color Doppler to assess regurgitation fraction
(the regurgitant jet area/the left atrium area) in the two-and four-chamber views
at end-systole. The severity of MR was classified as mild (occupied
Laboratory results were defined as the initial assessment of hospital visits.
Items were listed below: brain natriuretic peptide (BNP), N-terminal pro-B type
natriuretic peptide (NT-proBNP), C-reactive protein (CRP), creatine (Cr),
hemoglobin (Hb), alanine aminotransferase (ALT), glycated hemoglobin (HbA1c),
free fatty acid (FFA),
Continuous variables in both the MR group and the non-MR group were tested for
the normal distribution (Kolmogorov–Smirnov one-sample test, all p
Overall, a total of 2418 patients were eligible for analysis (age 67.2
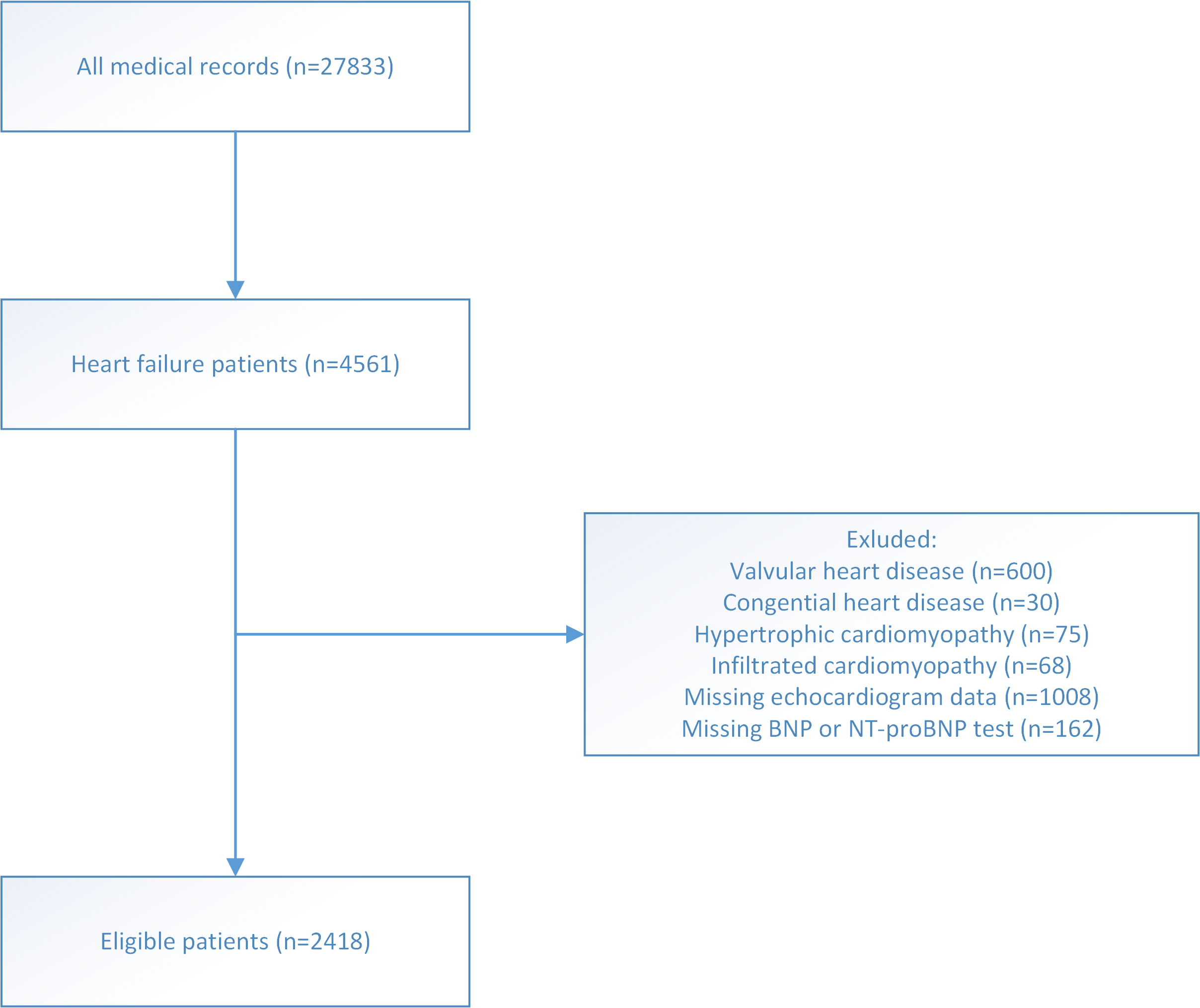 Fig. 1.
Fig. 1.Flow chart of patients selection.
| HFpEF | HFmEF | HFrEF | p | ||
| (n = 1005) | (n = 373) | (n = 1040) | |||
| Clinical status | |||||
| Mitral regurgitation (n) | 168 (16.7%) | 106 (28.4%) | 517 (49.7%) | ||
| Age (y) | 70.3 (12.6) | 66.7 (13.7) | 64.3 (13.6) | ||
| Sex (male) | 616 (61.3%) | 274 (73.5%) | 755 (72.6%) | ||
| Body mass index (kg/m |
24.5 (3.68) | 24.1 (3.76) | 23.5 (3.82) | ||
| Hypertension (n) | 679 (67.6%) | 225 (60.3%) | 477 (45.9%) | ||
| Diabetes (n) | 275 (27.4%) | 98 (26.3%) | 283 (27.2%) | 0.919 | |
| Atrial fibrillation (n) | 363 (36.1%) | 151 (40.5%) | 323 (31.1%) | 0.002 | |
| Stroke (n) | 129 (12.8%) | 53 (14.2%) | 111 (10.7%) | 0.132 | |
| Chronic obstructive pulmonary disease (n) | 84 (8.36%) | 21 (5.63%) | 73 (7.02%) | 0.194 | |
| Thyroid disease (n) | 8 (0.80%) | 3 (0.80%) | 17 (1.63%) | 0.202 | |
| Chronic kidney disease (n) | 105 (10.4%) | 55 (14.7%) | 157 (15.1%) | 0.005 | |
| Heart failure cause | |||||
| Ischemic (n) | 674 (67.1%) | 211 (56.6%) | 468 (45.0%) | ||
| Non-Ischemic (n) | 331 (32.9%) | 162 (43.4%) | 572 (55%) | ||
| All values are presented as the means | |||||
Table 2 and Table 3 summarize the baseline characteristics of the MR and non-MR
groups. Patients in the MR group and the non-MR group were comparable in terms of
age and sex. Patients in the MR group had a lower body mass index (BMI), systolic
blood pressure (SBP), diastolic blood pressure (DBP). Patients in the MR group
had a lower rate of hypertension (MR 50.3% vs. non-MR 60.4%, p
| non-MR | MR | p | ||
| (n = 1627) | (n = 791) | |||
| Clinical status age (y) | 68.0 (59.0–76.0) | 69.0 (59.0–78.0) | 0.051 | |
| Sex (male) | 1120 (68.8%) | 525 (66.4%) | 0.240 | |
| Body mass index (kg/m |
24.2 (22.0–26.6) | 23.0 (20.8–25.5) | ||
| Systolic blood pressure (mmHg) | 118 (105–132) | 113 (101–127) | ||
| Diastolic blood pressure (mmHg) | 68.0 (60.0–76.0) | 67.0 (59.0–75.0) | 0.047 | |
| Heart rate (beat/min) | 72.0 (63.0–81.0) | 74.0 (65.0–83.0) | 0.011 | |
| Heart failure classification | ||||
| Preserved | 837 (51.4%) | 168 (21.2%) | ||
| Mid-range | 267 (16.4%) | 106 (13.4%) | ||
| reduced | 523 (32.1%) | 517 (65.4%) | ||
| Comorbidities | ||||
| Hypertension (n) | 983 (60.4%) | 398 (50.3%) | ||
| Coronary artery disease (n) | 997 (61.3%) | 356 (45.0%) | ||
| Diabetes (n) | 456 (28.0%) | 200 (25.3%) | 0.169 | |
| Atrial fibrillation (n) | 491 (30.2%) | 346 (43.7%) | ||
| Stroke (n) | 201 (12.4%) | 92 (11.6%) | 0.656 | |
| Chronic obstructive pulmonary disease (n) | 115 (7.07%) | 63 (7.96%) | 0.478 | |
| Thyroid disease (n) | 11 (0.68%) | 17 (2.15%) | 0.003 | |
| Chronic kidney disease (n) | 190 (11.7%) | 127 (16.1%) | 0.003 | |
| Echocardiogram | ||||
| Ejection fraction (%) | 50.8 (36.0–61.3) | 33.0 (25.0–46.0) | ||
| Interventricular septum thickness in diastolic phase (cm) | 1.00 (0.90–1.09) | 0.95 (0.85–1.05) | ||
| Left atrium dimension (cm) | 4.05 (3.62–4.54) | 4.68 (4.24–5.08) | ||
| Left ventricular end-diastolic volume (mL) | 130 (102–171) | 162 (126–212) | ||
| Left ventricular internal diameter in diastolic phase (cm) | 5.17 (4.60–5.87) | 6.08 (5.30–6.72) | ||
| Left ventricular posterior wall thickness in diastolic phase (cm) | 0.99 (0.91–1.08) | 0.95 (0.85–1.05) | ||
| Tricuspid reugrgitation | 241 (14.8%) | 370 (46.8%) | ||
| All values are presented as the means | ||||
| non-MR | MR | p | ||
| (n = 1627) | (n = 791) | |||
| Laboratory result | ||||
| BNP (pg/mL) | 206 (64.6–524) | 574 (268–1346) | ||
| NT-proBNP (pg/mL) | 1458 (488–3828) | 3478 (1522–7178) | ||
| CRP (mg/L) | 5.00 (5.00–11.6) | 5.70 (5.00–14.0) | 0.002 | |
| Cr (umol/L) | 77.0 (64.0–98.0) | 83.0 (68.0–110) | ||
| Hb (g/L) | 131 (118–145) | 129 (115–142) | 0.006 | |
| ALT (u/L) | 30.0 (23.0–40.2) | 31.0 (24.0–44.0) | 0.001 | |
| HbA1c (%) | 6.20 (5.80–6.90) | 6.20 (5.80–6.80) | 0.410 | |
| FFA (umol/L) | 451 (315–631) | 528 (356–726) | ||
| BHB (mmol/L) | 0.06 (0.04–0.10) | 0.08 (0.05–0.19) | ||
| Glu (mmol/L) | 6.30 (5.24–8.06) | 6.31 (5.16–7.86) | 0.239 | |
| TG (mmol/L) | 1.16 (0.88–1.64) | 1.02 (0.77–1.37) | ||
| HDL (mmol/L) | 1.12 (0.96–1.32) | 1.13 (0.92–1.32) | 0.364 | |
| LDL (mmol/L) | 1.85 (1.39–2.42) | 1.88 (1.37–2.38) | 0.784 | |
| Medication | ||||
| ACEI | 680 (41.8%) | 391 (49.4%) | ||
| ARB | 581 (35.7%) | 234 (29.6%) | 0.003 | |
| ARNi | 138 (8.48%) | 136 (17.2%) | ||
| 1273 (78.2%) | 678 (85.7%) | |||
| Spironolactone | 974 (59.9%) | 675 (85.3%) | ||
| Diuretic | 1079 (66.3%) | 714 (90.3%) | ||
| Digoxin | 296 (18.2%) | 316 (39.9%) | ||
| Amiodarone | 207 (12.7%) | 164 (20.7%) | ||
| Anti-platelet | 204 (12.5%) | 48 (6.07%) | ||
| Statin | 1361 (83.7%) | 567 (71.7%) | ||
| Insulin | 273 (16.8%) | 127 (16.1%) | 0.696 | |
| Metformin | 143 (8.79%) | 56 (7.08%) | 0.175 | |
| Trimetazidine | 515 (31.7%) | 313 (39.6%) | ||
| Intervention | ||||
| ICD | 30 (1.84%) | 53 (6.70%) | ||
| CRT | 25 (1.54%) | 33 (4.17%) | ||
| PCI | 375 (23.0%) | 113 (14.3%) | ||
| Ablation | 90 (5.53%) | 49 (6.19%) | 0.573 | |
| All values are presented as the means | ||||
Univariable analysis data was displayed in Supplementary Table 1.
Stepwise multivariable logistic regression using likelihood ratio method was
utilized to identify the associated factors of MR. The result showed that EF (OR
0.966, 95% confidence interval (CI) [0.957, 0.974], p
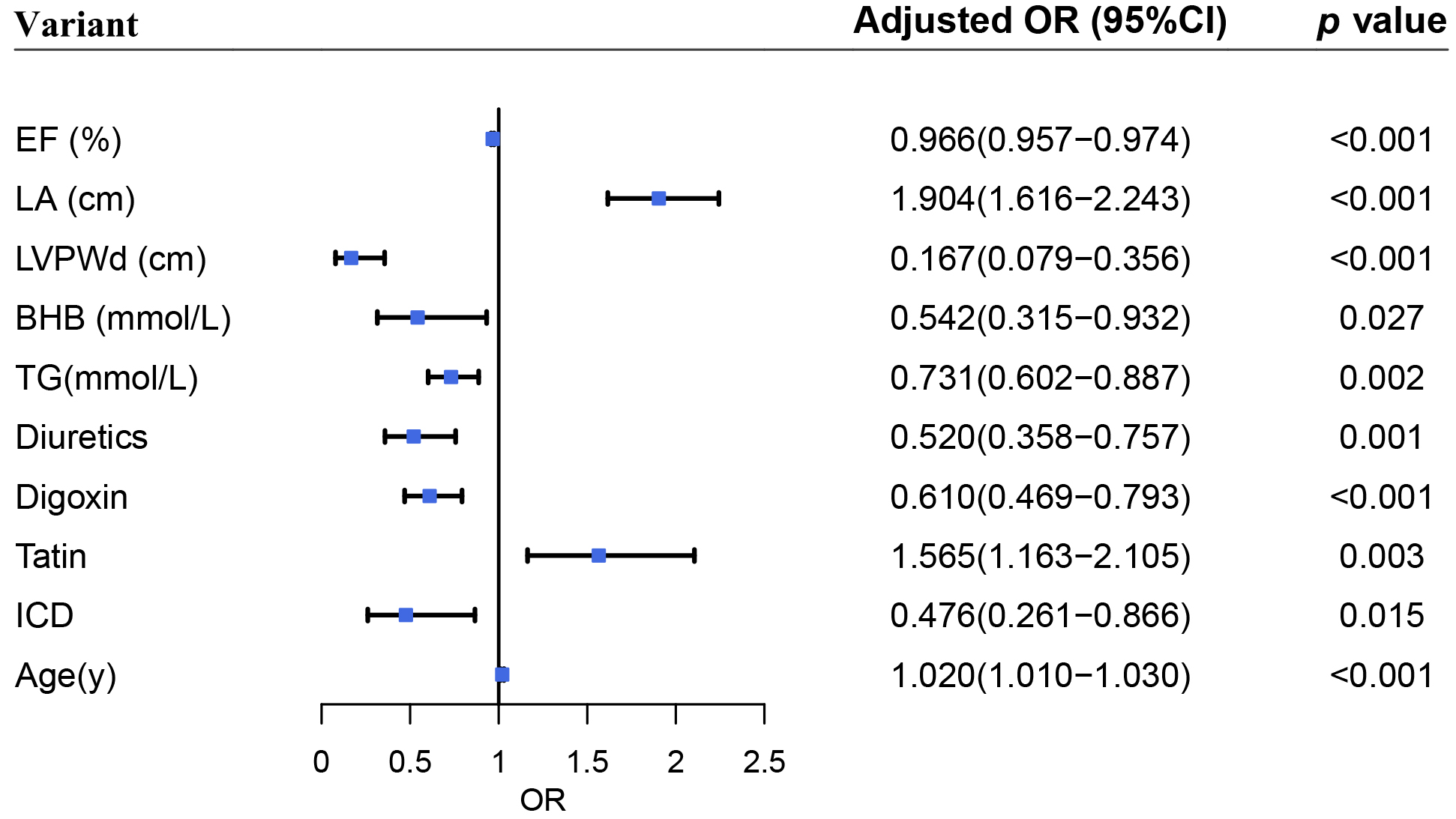 Fig. 2.
Fig. 2.Forest plot on associated factors of functional mitral regurgitation.
For patients with HFpEF, four factors associated with MR incuding EF (OR 0.954
(0.928–0.981), p = 0.001), LVPWd (OR
0.274 (0.081–0.932), p = 0.038), LA dimension (OR 2.049 (1.631–2.576),
p
| Model 1 | Model 2 | ||||
| Adjusted OR (95% CI) | p | Adjusted OR (95% CI) | p | ||
| HFpEF | |||||
| EF (%) | 0.955 (0.927–0.983) | 0.002 | 0.954 (0.928–0.981) | 0.001 | |
| LA dimension (cm) | 1.923 (1.527–2.423) | 2.049 (1.631–2.576) | |||
| LVPWd (cm) | 0.260 (0.073–0.928) | 0.038 | 0.274 (0.081–0.932) | 0.038 | |
| Diuretic | 0.453 (0.284–0.723) | 0.001 | 0.549 (0.348–0.867) | 0.100 | |
| Statin | 1.736 (1.063–2.836) | 0.028 | 1.368 (0.805–2.322) | 0.246 | |
| Age | 1.022 (1.005–1.040) | 0.013 | 1.024 (1.007–1.041) | 0.007 | |
| HFmrEF | |||||
| LA dimension (cm) | 1.904 (1.355–2.675) | 2.009 (1.427–2.829) | |||
| TG (mmol/L) | 0.562 (0.365–0.865) | 0.009 | 0.552 (0.359–0.849) | 0.007 | |
| Digoxin | 0.315 (0.183–0.540) | 2.836 (1.624–4.951) | |||
| HFrEF | |||||
| EF (%) | 0.969 (0.949–0.991) | 0.005 | 0.969 (0.949–0.990) | 0.004 | |
| LA dimension (cm) | 2.222 (1.776–2.779) | 2.289 (1.821–2.878) | |||
| LVPWd (cm) | 0.145 (0.060–0.352) | 0.161 (0.067–0.387) | |||
| TG (mmol/L) | 0.744 (0.594–0.933) | 0.010 | 0.746 (0.595–0.936) | 0.011 | |
| Diuretic | 0.518 (0.309–0.869) | 0.013 | 0.559 (0.334–0.934) | 0.026 | |
| Statin | 1.443 (1.033–2.015) | 0.031 | 1.312 (0.917–1.878) | 0.138 | |
| ICD | 0.483 (0.272–0.857) | 0.013 | 1.898 (1.074–3.354) | 0.027 | |
| Age | 1.017 (1.006–1.029) | 0.003 | 1.016 (1.004–1.027) | 0.009 | |
| Model 1 multivariable logistic regression model; Model 2 adjusted for sex, CAD and DM. FMR, functional mitral regurgitation; OR, odds ratio; CI, confidence interval; EF, ejection fraction; LA, left atrium; LVPWd, left ventricular posterior wall thickness in diastolic phase; TG, triglycerides; ICD, implantable cardioverter defibrillator. | |||||
For patients with HFmrEF, three factors associated with MR including LA
dimension (OR 2.009 (1.427–2.829), p
For patients with HFrEF, seven factors associated with MR: EF (OR 0.969
(0.949–0.990), p = 0.004), LVPWd (OR
0.161 (0.067–0.387), p
The prevalence and characteristics of MR in HF patients (including HFpEF) were determined in this study using data from a Chinese hospital. To begin, a significant proportion of HF patients in our study had MR, particularly the HFrEF patients. Due to the high prevalence of HF in China, a significant proportion of MR patients have a poor prognosis and may benefit from mitral valve repair, as clinical trials continue [20, 21]. Second, MR is associated with deteriorated cardiac function, including atrial and ventricle abnormalities. It is worth noting that the LA dimension appeared to be critical in the progression of HF and MR. Third, older age was associated with increased MR. Finally, it appeared as though TG, diuretics, digoxin, and ICD were associated with decreased MR.
Our cross-sectional study found a high prevalence of MR in HF patients (32.71%)
and an increasing ratio in HFrEF patients (49.70%). Similar findings have been
reported. A previous study showed 44.5% MR in acute HF patients (EF
A significant finding was that MR was associated with a deteriorated cardiac
function (EF), a thinner wall thickness (LVPWd), and a larger LA chamber (LA
dimension), as determined by the etiology. Previous studies have demonstrated
that a proportion of AF patients exhibit atrial MR (most commonly in HFpEF
patients) characterized by LA and mitral annular enlargement [23, 24]. In the
meanwhile, conventional MR was characterized by LV enlargement and papillary
muscle dysfunction. We classified HF patients by ejection fraction to investigate
the clinical characteristics of MR in different HF subtypes. LA dimension
appeared to be associated with MR in patients with HFpEF (OR 2.049
(1.631–2.576), p
While LA dimension was found to be significantly associated with MR, there was a
significant interaction between LA dimension and AF. AF, HF, and MR appeared to
construct a vicious circle, which could be broken to delay the progression of HF.
On the one hand, worsened MR seemed to aggravate the burden of left atrium,
resulting in the enlargement and dysfunction of LA, which eventually developed
into AF [27]. On the other hand, recent studies indicated that atrial MR seemed
to be a novel subtype characterized by significant dilatation of mitral annulus
and LA [23, 28, 29]. A randomized clinical trial published in 2018 enrolled 363
patients with HF (EF
Demographic differences in MR, including sex, age, and race, were reported. Elderly patients were more likely to associate with progressive HF and worsen MR [11, 12]. The white and the female were more likely to have moderate to severe MR [8]. We found that BHB (OR 0.542, 95% CI [0.315–0.932], p = 0.002) and TG (OR 0.731, 95% CI [0.602–0.887], p = 0.002) might associate with MR. BHB, a ketone body, served as an energy supply for the heart, especially during heart failure [32]. Several clinical trials tested the external supplement of BHB and received positive results, which seemed to strengthen the cardiac function and possibly ameliorate MR condition [33, 34]. We found that a lower level of TG was associated with MR. However, a previous study pointed out that a high serum level of TG is associated with the later development of heart failure [35]. BHB and TG might serve as potential markers of MR though these applications should be investigated in further studies.
The use of diuretics and digoxin included in the guideline-directed medical
therapy of HF was associated with less MR [16, 36]. Clinical trials failed to
demonstrate the benefit of statins in patients with HF [37]; furthermore, our
research found that the use of statins associated with more MR, which indicated
that statins might be deleterious for patients with MR. However, subgroup
analysis seemed not to support this hypothesis. The implantation of ICD seemed to
be associated with MR. Previous studies have demonstrated that CRT reduces the
volume of mitral regurgitation. ICD was recommended for patients with
asymptomatic LV systolic dysfunction (LVEF
This was a chart review study, and the authors are aware of the limitations. Firstly, this was a retrospective study conducted in a single center. To minimize biases, we adopted standardized data extraction; multivariable logistic regression was adopted in order to adjust for well-known confounders. We further classified HF into three groups due to the significantly different etiology between them and adjusted for known confounders. Secondly, it was a chart review study; echocardiogram diagnosis and parameters were acquired from medical records at diagnosis instead of post-analysis from echocardiogram image. As such, our results should be interpreted with caution. Notably, the echocardiologists in our center applied parameters including effective regurgitation orifice area and regurgitation volume when diagnosing severe regurgitation; however, these parameters were not available in the medical records. Thirdly, there were missing values in the original data set; we excluded the records when missing values existed instead of replacing them.
Our research showed that in a large Chinese hospital, MR had a high prevalence in patients with HF. Worsen cardiac structure (LA dimension and LVPWd) and function (EF), age, and medical treatment strategy played important roles in MR. Among them, LA dimension is of great importance in subtypes of HF. These findings described the characteristics and etiology of MR in the clinical context.
Conceived and designed the experiment—CZ, CJ and MX. Data curation—CJ , YS, XL, YY and CZ. Writing, review and editing—CZ, CJ and MX. All authors have read and agreed to the published version of the manuscript.
The Second Affiliated Hospital of Zhejiang University, Institutional Review Board approved this study (register number 2017-007).
Not applicable.
This study was supported by Provincial and Ministry Joint Major Projects of National Health Commission of China (WKJ-ZJ-1703 to Meixiang Xiang) and The Key Research and Development Program of Zhejiang Province (2020C03118 to Meixiang Xiang).
The authors declare no conflict of interest.
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.31083/j.rcm2307235.
References
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.


