1 Department of Cardiothoracic Surgery, Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiaotong University, 200127 Shanghai, China
2 Information Center, Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiaotong University, 200127 Shanghai, China
3 Shanghai Synyi Medical Technology Co., Ltd. 201203 Shanghai, China
†These authors contributed equally.
Academic Editor: Jerome L. Fleg
Abstract
Background: A machine learning model was developed to estimate the
in-hospital mortality risk after congenital heart disease (CHD) surgery in
pediatric patient. Methods: Patients with CHD who underwent surgery were
included in the study. A Extreme Gradient Boosting (XGBoost) model was
constructed based onsurgical risk stratification and preoperative variables to
predict the risk of in-hospital mortality. We compared the predictive value of
the XGBoost model with Risk Adjustment in Congenital Heart Surgery-1 (RACHS-1)
and Society of Thoracic Surgery-European Association for
Cardiothoracic Surgery (STS-EACTS) categories. Results: A total of 24,685 patients underwent
CHD surgery and 595 (2.4%) died in hospital.
The area under curve (AUC) of the STS-EACTS and RACHS-1 risk stratification
scores were 0.748 [95% Confidence Interval (CI): 0.707–0.789, p
Keywords
- congenital heart disease
- in-hospital mortality
- machine learning
- Extreme Gradient Boosting
Congenital heart disease (CHD) is the most common congenital malformations. The prevalence of CHD at birth is about 75–90/10,000 for live births and total pregnancies, with CHD occurring in approximately 1% of live births and 10% of aborted fetuses [1, 2]. In addition, CHD is the leading cause of mortality in children with birth defects [3] and affects 0.7% children born in China [4]. The risk of mortality in Chinese children with CHD has been increasing [5].
Surgery has been the cornerstone in the treatment of patients with CHD [6]. Without interventions, patients with CHD will experience significant mortality. In developed countries, surgery has greatly improved the outcome of patients with CHD and significantly reduced the mortality rate [7]. However, approximately 20% children who undergo surgery for pediatric CHD are readmitted within 30 days, and 4.2% patients who undergo surgery for CHD die [8, 9]. Early mortality after cardiac surgery in the neonatal period is approximately 10% [1].
Risk of death in CHD patients is associated with complexity of surgical procedures [10]. Accurate prediction of in-hospital death is important to facilitate clinical decisions-making for the performance of certain procedures and improve patient’s outcome [11]. Several major risk stratification categories are currently available for the prediction of mortality and morbidity in children undergoing surgery for CHD—Risk Adjustment in Congenital Heart Surgery-1 (RACHS-1) [12], Aristotles Basic Complexity, and Aristotles Comprehensive Complexity [13], Society of Thoracic Surgery-European Association for Cardiothoracic Surgery (STS-EACTS) Congenital Heart Surgery (STAT) Mortality Categories [14]. These risk adjustment categories have been developed based on projections of risk or complexity and heavily rely on expert experience and consensus [15]. These traditional tools focus on surgical procedure categories and do not include sufficient individual patient risk factors. Therefore, it may have lower predictive accuracy for individual patients. The prognosis should be determined by combined analysis of multiple features. Thus, it is of great clinical significance to build a prediction model that includes multiple important clinical features.
Some studies have shown performance of machine learning-assisted tools were better than standard scoring systems [16, 17]. Machine learning has the advantage of flexibility and scalability compared to traditional biostatistical methods [18]. It is well suited for complex multidimensional data and may uncover interactions that hard to be identified and illustrated through classic statistical analysis [19]. Extreme Gradient Boosting (XGBoost) is a machine learning algorithm. It is an implementation of Gradient Boosting that was originally started as a research project by Tianqi Chen as part of the Distributed (Deep) Machine Learning Community (DMLC) group at the University of Washington [20]. Currently being the fastest and the best open source boosting tree toolkit, XGBoost has made many optimizations, such as significant improvements in model training speed and accuracy. Kilic evaluated the predictive performance of XGBoost model for risk of death after cardiac surgery, and found that the XGBoost model was superior in predictive performance compared to Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) score [21]. Zeng et al. [22] showed that a XGBoost model has better prediction performance for predicting postoperative complications than other traditional risk adjustment models after paediatric cardiac surgery. However, research on the application of machine learning model for the prediction of mortality risk in children with CHD is lacking, especially in China.
The aim of the study was to establish and validate a XGBoost model for predicting the in-hospital mortality risk in pediatric CHD surgery, and to compare the predictive value of the XGBoost model with the RACHS-1 and STS-EACTS categories.
Patients aged 0–18 years who were diagnosed with CHD and underwent CHD surgery at Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiaotong University between January 1, 2006 and December 31, 2017 were included. For patients with multiple surgical records within a month, only the information of the last surgical record was extracted, and the previous surgical records were regarded as “operation history”. The exclusion criteria included general thoracic surgery (not involving cardiac surgery), patients with incomplete or missing in-hospital survival records, and surgical procedures that were performed in less than 3 patients. Our study was approved by the Ethical Committee of Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiaotong University. As our study only involved a retrospective review of previous clinical data, the requirement for informed consent was waived.
The database was constructed by merging information from multiple data sources, including the laboratory information management system, hospital information system, intensive care unit database, clinical data repository, and the surgical record database of the cardiac surgery department in Shanghai Children’s Medical Center. We built a feature engineering pipeline to load and transform clinical data during and before CHD surgery for each individual. The collected data were divided into five categories as follows: (i) demographic data, such as sex, body mass index, and age; (ii) preoperative clinical factors, including diagnosis, numbers of defects, pulse oxygen saturation, a history of cardiac surgery (any prior cardiac surgeries), numbers of defects, non-cardiac malformations, and other risk factors; (iii) complexity of the CHD surgery according to RACHS-1 and STS-EACTS morbidity categories; (iv) cardiac Doppler ultrasound data; and (v) preoperative laboratory test results, including routine blood test findings, liver function test results, and coagulation index. Variables with more than 30% missing values were excluded.
The study endpoint was in-hospital mortality, defined as death due to any cause during hospitalization after surgery. The cause of death was defined as the disease, situation, or occurrence that causes a series of events, ultimately result in death [23]. And the cause of death in this study included cardiac, peri-operative, vascular and non-cardiovascular causes. Cardiac deaths included sudden death, documented ventricular arrhythmias, heart failure, infective endocarditis and myocardial infarction [23, 24]. Vascular death included haemorrhage, stroke, rupture of aneurysm, pulmonary embolism, and dissection [23, 24]. Non-cardiovascular death included malignancy, pneumonia, sepsis (excluding endocarditis), other infections, peritonitis, hip fracture, renal failure, suicide, and unknown [23, 24].
Mortality risk stratification was performed by classifying the procedures into clusters based on estimated mortality, following the statistical method proposed by a previous study [14]. First, we used a Bayesian random effect model to calculate the posterior probability distribution of the mortality rates of all procedures. Second, a homogeneity criterion was used to evaluate a partition scheme, which measured the within-category homogeneity of the mortality rates. The optimal partition solution to maximize the homogeneity criterion can be achieved using a dynamic programming algorithm. Finally, we successively performed the abovementioned calculations for 2–20 categories to determine the number of categories. The optimal category number was determined using of the Bayesian information criterion, a trade-off between homogeneity and partition complexity. All procedures were finally categorized into five relatively homogeneous categories. According to the pseudo-code algorithm description (see Appendix of the previous study) [14] we implemented handcrafted codes of the stratification computation pipeline using Python language (version 3.7.6, Python Software Foundation, Wilmington, DE, USA).
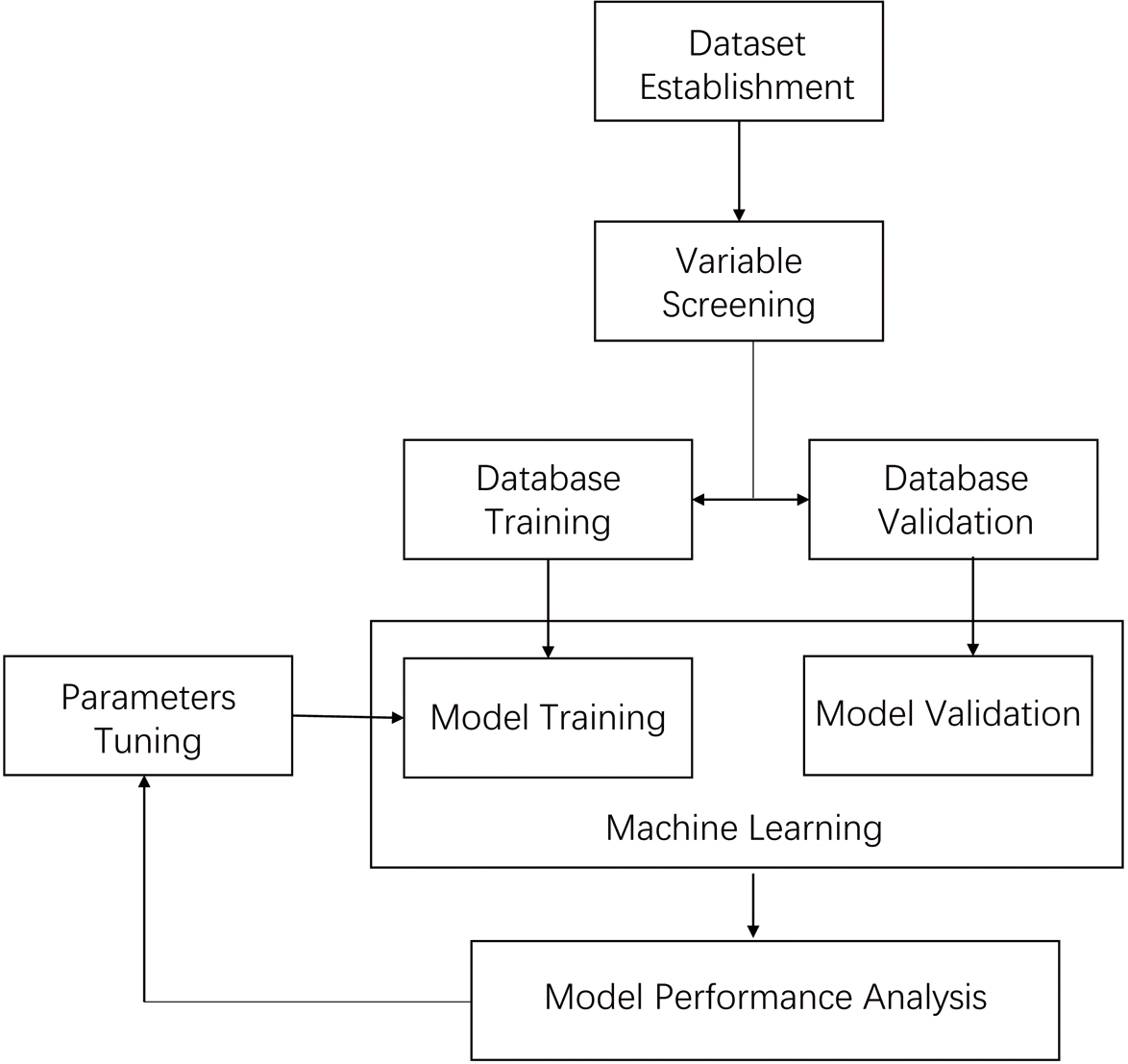
We used the XGBoost algorithm to build a in-hospital mortality predictive model for children with CHD. Dataset was devided into training set and testing set according to the 7.5:2.5 ratio. The training dataset was used for feature selection and model training, while the testing dataset was used for validation after model training. The importance of each feature was assessed using the recursive feature elimination (RFE) algorithm, and all features were sorted based on their level of importance. The RFE algorithm was used to recursively remove features and build a model on the remaining features. Among all possible combination of features, the model with the highest AUC was determined and the features included are eventually selected to build the XGBoost model. Furthermore, Grid Search was used to adjust the hyperparameters of model to reduce overfitting and improve the model accuracy. The stability of the model is tested by Bootstrap algorithm with random resampling of the samples, and 95% confidence interval (95% CI) was exported. Finally, we assessed the predictive power of the model using the area under the receiver operating characteristic curves (AUC), sensitivity, and specificity. Fig. 1 presents the whole process described above. The XGBoost was developed in Python language (version 3.7.6) with main packages scikit-learn (version 0.23.1) and XGBoost (version 1.1.1).
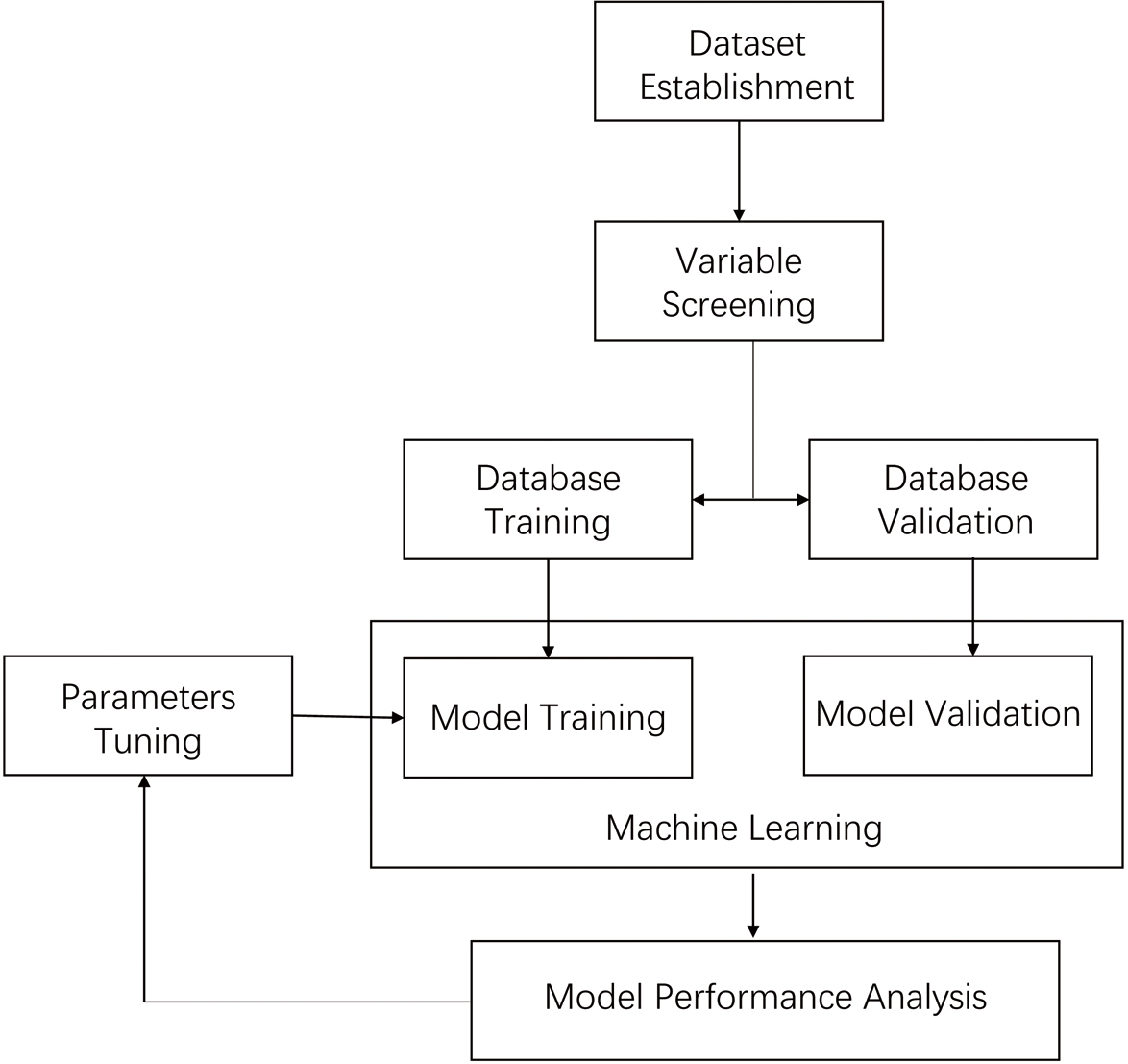 Fig. 1.
Fig. 1.Steps in the XGBoost model development.
Continuous variables are described as the median (range); all were non-normally
distributed. Categorical variables are described using frequency (%). To assess
the distributive balance between the training and validation sets, comparisons
between groups were performed using the Mann–Whitney U test, Fisher’s exact
test, and the chi-square test, as appropriate. The Area under receiver operating
characteristic (ROC) curve (AUC) with 95% confidence interval (CI) was
calculated to evaluate the predictive power. In addition, the optimal threshold
was chosen by maximizing the Youden Index. The sensitivity and specificity of the
predictive model were obtained based on the threshold. All statistical tests were
two sided, and p-value of
A total of 24,685 patients underwent surgery for CHD were included (Table 1). The mean age of the patients was 316 (1–6568) days, and 14,215 (57.59%) patients were male. A total of 591 (2.4%) in-hospital deaths occurred. Other patient characteristics are summarized in Table 1.
| Parameter | Training set n = 18552 | Testing set n = 6133 | Total n = 24685 | |||||||
| Death n = 442 | Non-death n = 18110 | Total n = 18552 | p-value | Death n = 149 | Non-death n = 5984 | Total n = 6133 | p-value | |||
| Age (days)* | Median (range) | 168 (2,6459) | 323 (1,6568) | 317 (1,6568) | 153 (1,4716) | 319 (2,6410) | 313 (1,6410) | 316 (1,6568) | ||
| 329 (74.4%) | 9681 (53.5%) | 10010 (54.0%) | 112 (75.2%) | 3205 (53.6%) | 3317 (54.2%) | 13327 (54.0%) | ||||
| 365 days to 1095 days | 51 (11.5%) | 4600 (25.4%) | 4651 (25.1%) | 19 (12.8%) | 1493 (25.0%) | 1512 (24.7%) | 6163 (25.0%) | |||
| 62 (14.0%) | 3812 (21.1%) | 3874 (20.9%) | 18 (12.1%) | 1276 (21.45) | 1294 (21.1%) | 5168 (21.0%) | ||||
| Sex* | Male | 278 (62.9%) | 10342 (57.11%) | 10620 (57.24%) | 0.015 | 81 (54.36%) | 3514 (58.72%) | 3595 (58.62%) | 0.286 | 14215 (57.59%) |
| Female | 164 (37.1%) | 7768 (42.89%) | 7932 (42.76%) | 68 (45.64%) | 2470 (41.28%) | 2538 (41.38%) | 10470 (42.41%) | |||
| BMI* | 82 (20.55%) | 3077 (19.26%) | 3159 (19.29%) | 0.494 | 34 (25.19%) | 1066 (20.14%) | 1100 (20.26%) | 0.122 | 4259 (19.53%) | |
| P5–P95 percentile | 252 (63.16%) | 10539 (65.97%) | 10791 (65.9%) | 75 (55.56%) | 3395 (64.13%) | 3470 (63.92%) | 14261 (65.41%) | |||
| 65 (16.29%) | 2360 (14.77%) | 2425 (14.81%) | 26 (19.26%) | 833 (15.73%) | 859 (15.82%) | 3284 (15.06%) | ||||
| A history of cardiac surgery | 0 | 311 (70.4%) | 16323 (90.1%) | 16634 (89.7%) | 103 (69.1%) | 5364 (89.6%) | 5467 (89.1%) | 22101 (89.5%) | ||
| 1 | 122 (27.6%) | 1663 (9.2%) | 1785 (9.6%) | 44 (29.5%) | 583 (9.7%) | 627 (10.2%) | 2412 (9.8%) | |||
| 9 (2.0%) | 124 (0.7%) | 133 (0.7%) | 2 (1.3%) | 37 (0.6%) | 39 (0.6%) | 172 (0.7%) | ||||
| Preoperative ICU admission | 0 | 429 (97.1%) | 17530 (96.8%) | 17959 (96.8%) | 0.758 | 141 (94.6%) | 5755 (96.2%) | 5896 (96.1%) | 0.335 | 23855 (96.6%) |
| 1 | 13 (2.9%) | 580 (3.2%) | 593 (3.2%) | 8 (5.4%) | 229 (3.8%) | 237 (3.9%) | 830 (3.4%) | |||
| ABO blood type | A | 125 (29.9%) | 5534 (30.87%) | 5659 (30.85%) | 0.919 | 44 (31.21%) | 1840 (30.97%) | 1884 (30.98%) | 0.988 | 7543 (30.88%) |
| B | 119 (28.47%) | 4942 (27.57%) | 5061 (27.59%) | 38 (26.95%) | 1654 (27.84%) | 1692 (27.82%) | 6753 (27.65%) | |||
| O | 95 (22.73%) | 4210 (23.49%) | 4305 (23.47%) | 34 (24.11%) | 1366 (22.99%) | 1400 (23.02%) | 5705 (23.36%) | |||
| AB | 79 (18.9%) | 3238 (18.07%) | 3317 (18.08%) | 25 (17.73%) | 1081 (18.2%) | 1106 (18.18%) | 4423 (18.11%) | |||
| RH blood type | - | 3 (0.72%) | 77 (0.43%) | 80 (0.44%) | 0.431 | 0 (0%) | 26 (0.44%) | 26 (0.43%) | 106 (0.43%) | |
| + | 413 (99.28%) | 17866 (99.57%) | 18279 (99.56%) | 140 (100%) | 5904 (99.56%) | 6044 (99.57%) | 24323 (99.57%) | |||
| Premature | No | 437 (98.87%) | 17960 (99.17%) | 18397 (99.16%) | 0.423 | 145 (97.32%) | 5927 (99.05%) | 6072 (99.01%) | 0.06 | 24469 (99.12%) |
| Yes | 5 (1.13%) | 150 (0.83%) | 155 (0.84%) | 4 (2.68%) | 57 (0.95%) | 61 (0.99%) | 216 (0.88%) | |||
| Non-cardiac malformation | No | 440 (99.55%) | 18088 (99.88%) | 18528 (99.87%) | 0.111 | 149 (100%) | 5982 (99.97%) | 6131 (99.97%) | 24659 (99.89%) | |
| Yes | 2 (0.45%) | 22 (0.12%) | 24 (0.13%) | 0 (0%) | 2 (0.03%) | 2 (0.03%) | 26 (0.11%) | |||
| Chromosome abnormality or syndrome | No | 438 (99.1%) | 17920 (99.0%) | 18358 (99.0%) | 146 (98.0%) | 5920 (98.9%) | 6066 (98.9%) | 0.222 | 24424 (98.9%) | |
| Yes | 4 (0.9%) | 190 (1.0%) | 194 (1.0%) | 3 (2.0%) | 64 (1.1%) | 67 (1.1%) | 261 (1.1%) | |||
| Allergy* | No | 436 (98.64%) | 17522 (96.75%) | 17958 (96.8%) | 0.026 | 145 (97.32%) | 5783 (96.64%) | 5928 (96.66%) | 0.819 | 23886 (96.76%) |
| Yes | 6 (1.36%) | 588 (3.25%) | 594 (3.2%) | 4 (2.68%) | 201 (3.36%) | 205 (3.34%) | 799 (3.24%) | |||
| Special treatment before surgery* | No | 400 (90.5%) | 17800 (98.29%) | 18200 (98.1%) | 136 (91.28%) | 5876 (98.2%) | 6012 (98.03%) | 24212 (98.08%) | ||
| Yes | 42 (9.5%) | 310 (1.71%) | 352 (1.9%) | 13 (8.72%) | 108 (1.8%) | 121 (1.97%) | 473 (1.92%) | |||
| Preoperative HCT* | Low | 19 (5.4%) | 873 (5.84%) | 892 (5.83%) | 9 (6.87%) | 327 (6.56%) | 336 (6.57%) | 0.069 | 1228 (6.02%) | |
| Normal | 285 (80.97%) | 13580 (90.92%) | 13865 (90.69%) | 112 (85.5%) | 4470 (89.7%) | 4582 (89.6%) | 18447 (90.41%) | |||
| High | 48 (13.64%) | 484 (3.24%) | 532 (3.48%) | 10 (7.63%) | 186 (3.73%) | 196 (3.83%) | 728 (3.57%) | |||
| STS-EACTS categories* | 1 | 111 (25.3%) | 10359 (57.4%) | 10470 (56.6%) | 27 (18.2%) | 3405 (57.0%) | 3432 (56.1%) | 13902 (56.5%) | ||
| 2 | 120 (27.4%) | 5074 (28.1%) | 5194 (28.1%) | 44 (29.7%) | 1708 (28.6%) | 1752 (28.6%) | 6946 (28.2%) | |||
| 3 | 117 (26.7%) | 1407 (7.8%) | 1524 (8.2%) | 40 (27.0%) | 443 (7.4%) | 483 (7.9%) | 2007 (8.2%) | |||
| 4 | 80 (18.3%) | 1198 (6.6%) | 1278 (6.9%) | 33 (22.3%) | 409 (6.8%) | 442 (7.2%) | 1720 (7.0%) | |||
| 5 | 10 (2.3%) | 20 (0.1%) | 30 (0.2%) | 4 (2.7%) | 6 (0.1%) | 10 (0.2%) | 40 (0.2%) | |||
| RACHS-1 categories | 1 | 65 (14.7%) | 3148 (17.4%) | 3213 (17.3%) | 19 (12.8%) | 966 (16.1) | 985 (16.1%) | 4198 (17.0%) | ||
| 2 | 161 (36.4%) | 11341 (62.6%) | 11502 (62.0%) | 45 (30.2%) | 3830 (64.0%) | 3875 (63.2%) | 15377 (62.3%) | |||
| 3 | 152 (34.4%) | 3124 (17.3%) | 3276 (17.7%) | 69 (46.3%) | 1032 (17.2%) | 1101 (18.0%) | 4377 (17.7%) | |||
| 4 | 50 (11.3%) | 446 (2.5%) | 496 (2.7%) | 12 (8.1) | 135 (2.3%) | 147 (2.4%) | 643 (2.6%) | |||
| 5 | 8 (1.8%) | 46 (0.3%) | 54 (0.3%) | 3 (2.0%) | 20 (0.3%) | 23 (0.4%) | 77 (0.3%) | |||
| 6 | 6 (1.4%) | 5 (0.0%) | 11 (0.1%) | 1 (0.7%) | 1 (0.0%) | 2 (0.0%) | 13 (0.1%) | |||
| Risk stratification | 1 | 28 (6.33%) | 10605 (58.56%) | 10633 (57.31%) | 14 (9.4%) | 3459 (57.8%) | 3473 (56.63%) | 14106 (57.14%) | ||
| 2 | 87 (19.68%) | 4399 (24.29%) | 4486 (24.18%) | 33 (22.15%) | 1477 (24.68%) | 1510 (24.62%) | 5996 (24.29%) | |||
| 3 | 145 (32.81%) | 2228 (12.3%) | 2373 (12.79%) | 45 (30.2%) | 717 (11.98%) | 762 (12.42%) | 3135 (12.7%) | |||
| 4 | 82 (18.55%) | 529 (2.92%) | 611 (3.29%) | 27 (18.12%) | 199 (3.33%) | 226 (3.68%) | 837 (3.39%) | |||
| 5 | 100 (22.62%) | 349 (1.93%) | 449 (2.42%) | 30 (20.13%) | 132 (2.21%) | 162 (2.64%) | 611 (2.48%) | |||
| Pulse oxygen saturation* | 235 (72.76%) | 3368 (24.77%) | 3603 (25.89%) | 80 (68.38%) | 1179 (26.09%) | 1259 (27.16%) | 0.001 | 4862 (26.2%) | ||
| 88 (27.24%) | 10228 (75.23%) | 10316 (74.11%) | 37 (31.62%) | 3340 (73.91%) | 3377 (72.84%) | 13693 (73.8%) | ||||
| Diameter of aortic sinus* | 72 (25.9%) | 3225 (20.83%) | 3297 (20.92%) | 0.008 | 22 (26.19%) | 1018 (19.9%) | 1040 (20%) | 0.353 | 4337 (20.69%) | |
| Normal | 72 (25.9%) | 5299 (34.23%) | 5371 (34.08%) | 27 (32.14%) | 1732 (33.85%) | 1759 (33.83%) | 7130 (34.02%) | |||
| 134 (48.2%) | 6958 (44.94%) | 7092 (45%) | 35 (41.67%) | 2366 (46.25%) | 2401 (46.17%) | 9493 (45.29%) | ||||
| AAO* | Median (range) | 1.1 (0.2, 4.11) | 1.2 (0.4, 14.1) | 1.2 (0.2, 14.1) | 1.15 (0.5, 6.69) | 1.2 (0.4, 6.62) | 1.2 (0.4, 6.69) | 0.635 | 1.2 (0.2, 14.1) | |
| DAO* | Median (range) | 1.2 (0.6, 4.28) | 1.3 (0.38, 11.1) | 1.3 (0.38, 11.1) | 0.005 | 1.2 (0.6, 3.45) | 1.27 (0.5, 5.03) | 1.23 (0.5, 5.03) | 0.058 | 1.28 (0.38, 11.1) |
| MPA (mm)* | Median (range) | 1.72 (0.34, 6.19) | 1.6 (0.2, 20) | 1.6 (0.2, 20) | 0.022 | 1.7 (0.6, 17) | 1.6 (0.3, 41.6) | 1.6 (0.3, 41.6) | 0.588 | 1.6 (0.2, 41.6) |
| MV (m/s)* | Median (range) | 1 (0.3, 3.3) | 1.2 (0.36, 3.81) | 1.2 (0.3, 3.81) | 1 (0.4, 2.68) | 1.2 (0.4, 12) | 1.2 (0.4, 12) | 1.2 (0.3, 12) | ||
| TV2 (m/s)* | Median (range) | 0.8 (0.4, 2.47) | 0.8 (0.2, 33) | 0.8 (0.2, 33) | 0.025 | 0.8 (0.4, 1.7) | 0.8 (0.3, 10.7) | 0.8 (0.3, 10.7) | 0.487 | 0.8 (0.2, 33) |
| Left atrial dimension* | 79 (27.82%) | 1907 (12.24%) | 1986 (12.52%) | 25 (27.78%) | 621 (12.06%) | 646 (12.33%) | 2632 (12.47%) | |||
| Normal | 79 (27.82%) | 3330 (21.37%) | 3409 (21.49%) | 26 (28.89%) | 1146 (22.25%) | 1172 (22.37%) | 4581 (21.71%) | |||
| 126 (44.37%) | 10343 (66.39%) | 10469 (65.99%) | 39 (43.33%) | 3383 (65.69%) | 3422 (65.31%) | 13891 (65.82%) | ||||
| LVDD* | 209 (56.64%) | 5535 (33.42%) | 5744 (33.92%) | 65 (50.39%) | 1791 (32.81%) | 1856 (33.21%) | 7600 (33.75%) | |||
| Normal | 81 (21.95%) | 3337 (20.15%) | 3418 (20.19%) | 28 (21.71%) | 1095 (20.06%) | 1123 (20.1%) | 4541 (20.16%) | |||
| 79 (21.41%) | 7691 (46.43%) | 7770 (45.89%) | 36 (27.91%) | 2573 (47.13%) | 2609 (46.69%) | 10379 (46.09%) | ||||
| LVEF* | 176 (48.22%) | 8881 (53.7%) | 9057 (53.58%) | 0.022 | 67 (52.34%) | 3050 (55.93%) | 3117 (55.85%) | 0.009 | 12174 (54.15%) | |
| Normal | 108 (29.59%) | 4846 (29.3%) | 4954 (29.31%) | 27 (21.09%) | 1495 (27.42%) | 1522 (27.27%) | 6476 (28.8%) | |||
| 81 (22.19%) | 2811 (17%) | 2892 (17.11%) | 34 (26.56%) | 908 (16.65%) | 942 (16.88%) | 3834 (17.05%) | ||||
| LVFS* | 191 (52.33%) | 8697 (52.59%) | 8888 (52.58%) | 0.096 | 68 (53.13%) | 2993 (54.89%) | 3061 (54.85%) | 0.01 | 11949 (53.14%) | |
| Normal | 102 (27.95%) | 5209 (31.5%) | 5311 (31.42%) | 28 (21.88%) | 1600 (29.34%) | 1628 (29.17%) | 6939 (30.86%) | |||
| 72 (19.73%) | 2632 (15.91%) | 2704 (16%) | 32 (25%) | 860 (15.77%) | 892 (15.98%) | 3596 (15.99%) | ||||
| LVPWD | 121 (33.06%) | 4734 (28.61%) | 4855 (28.7%) | 0.146 | 36 (28.13%) | 1590 (29.15%) | 1626 (29.12%) | 0.605 | 6481 (28.81%) | |
| Normal | 101 (27.6%) | 4635 (28.01%) | 4736 (28%) | 39 (30.47%) | 1448 (26.54%) | 1487 (26.63%) | 6223 (27.66%) | |||
| 144 (39.34%) | 7179 (43.38%) | 7323 (43.3%) | 53 (41.41%) | 2417 (44.31%) | 2470 (44.24%) | 9793 (43.53%) | ||||
| Large artery shunt* | None | 220 (58.51%) | 14125 (85.46%) | 14345 (84.86%) | 72 (54.96%) | 4669 (85.8%) | 4741 (85.07%) | 19086 (84.91%) | ||
| Left to right | 108 (28.72%) | 1728 (10.45%) | 1836 (10.86%) | 37 (28.24%) | 564 (10.36%) | 601 (10.78%) | 2437 (10.84%) | |||
| Right to left | 12 (3.19%) | 53 (0.32%) | 65 (0.38%) | 2 (1.53%) | 21 (0.39%) | 23 (0.41%) | 88 (0.39%) | |||
| Two-way | 36 (9.57%) | 623 (3.77%) | 659 (3.9%) | 20 (15.27%) | 188 (3.45%) | 208 (3.73%) | 867 (3.86%) | |||
| Atrial shunt* | None | 77 (19.74%) | 6169 (36.95%) | 6246 (36.55%) | 29 (21.64%) | 2018 (36.6%) | 2047 (36.25%) | 8293 (36.48%) | ||
| Left to right | 114 (29.23%) | 7450 (44.62%) | 7564 (44.27%) | 42 (31.34%) | 2408 (43.68%) | 2450 (43.39%) | 10014 (44.05%) | |||
| Right to left | 48 (12.31%) | 617 (3.7%) | 665 (3.89%) | 10 (7.46%) | 235 (4.26%) | 245 (4.34%) | 910 (4%) | |||
| Two-way | 151 (38.72%) | 2461 (14.74%) | 2612 (15.29%) | 53 (39.55%) | 852 (15.45%) | 905 (16.03%) | 3517 (15.47%) | |||
| Ventricular shunt* | None | 106 (27.39%) | 4582 (27.45%) | 4688 (27.45%) | 34 (25.95%) | 1472 (26.73%) | 1506 (26.71%) | 6194 (27.27%) | ||
| Left to right | 17 (4.39%) | 6000 (35.95%) | 6017 (35.23%) | 4 (3.05%) | 1996 (36.24%) | 2000 (35.47%) | 8017 (35.29%) | |||
| Right to left | 5 (1.29%) | 33 (0.2%) | 38 (0.22%) | 0 (0%) | 9 (0.16%) | 9 (0.16%) | 47 (0.21%) | |||
| Two-way | 259 (66.93%) | 6077 (36.41%) | 6336 (37.1%) | 93 (70.99%) | 2030 (36.86%) | 2123 (37.66%) | 8459 (37.24%) | |||
| AI* | Negative | 307 (75.8%) | 13794 (81.81%) | 14101 (81.66%) | 0.002 | 98 (71.01%) | 4517 (81.2%) | 4615 (80.95%) | 0.003 | 18716 (81.49%) |
| Slight | 66 (16.3%) | 2110 (12.51%) | 2176 (12.6%) | 28 (20.29%) | 698 (12.55%) | 726 (12.73%) | 2902 (12.63%) | |||
| Mild | 28 (6.91%) | 831 (4.93%) | 859 (4.97%) | 11 (7.97%) | 311 (5.59%) | 322 (5.65%) | 1181 (5.14%) | |||
| Mild to moderate | 2 (0.49%) | 66 (0.39%) | 68 (0.39%) | 1 (0.72%) | 16 (0.29%) | 17 (0.3%) | 85 (0.37%) | |||
| Moderate | 2 (0.49%) | 31 (0.18%) | 33 (0.19%) | 0 (0%) | 16 (0.29%) | 16 (0.28%) | 49 (0.21%) | |||
| Moderate to severe | 0 (0%) | 14 (0.08%) | 14 (0.08%) | 0 (0%) | 2 (0.04%) | 2 (0.04%) | 16 (0.07%) | |||
| Severe | 0 (0%) | 16 (0.09%) | 16 (0.09%) | 0 (0%) | 3 (0.05%) | 3 (0.05%) | 19 (0.08%) | |||
| MR* | Negative | 129 (36.13%) | 4475 (27.41%) | 4604 (27.6%) | 0.001 | 32 (26.23%) | 1492 (27.71%) | 1524 (27.68%) | 0.297 | 6128 (27.62%) |
| Slight | 151 (42.3%) | 7495 (45.91%) | 7646 (45.83%) | 53 (43.44%) | 2456 (45.62%) | 2509 (45.57%) | 10155 (45.77%) | |||
| Mild | 52 (14.57%) | 3168 (19.41%) | 3220 (19.3%) | 22 (18.03%) | 1031 (19.15%) | 1053 (19.12%) | 4273 (19.26%) | |||
| Mild to moderate | 14 (3.92%) | 651 (3.99%) | 665 (3.99%) | 3 (2.46%) | 233 (4.33%) | 236 (4.29%) | 901 (4.06%) | |||
| Moderate | 7 (1.96%) | 389 (2.38%) | 396 (2.37%) | 5 (4.1%) | 123 (2.28%) | 128 (2.32%) | 524 (2.36%) | |||
| Moderate to severe | 1 (0.28%) | 82 (0.5%) | 83 (0.5%) | 4 (3.28%) | 27 (0.5%) | 31 (0.56%) | 114 (0.51%) | |||
| Severe | 3 (0.84%) | 65 (0.4%) | 68 (0.41%) | 3 (2.46%) | 22 (0.41%) | 25 (0.45%) | 93 (0.42%) | |||
| PI* | Negative | 95 (32.09%) | 2423 (15.11%) | 2518 (15.42%) | 27 (25%) | 811 (15.38%) | 838 (15.57%) | 0.668 | 3356 (15.45%) | |
| Slight | 123 (41.55%) | 9015 (56.21%) | 9138 (55.95%) | 46 (42.59%) | 2993 (56.75%) | 3039 (56.47%) | 12177 (56.08%) | |||
| Mild | 67 (22.64%) | 4343 (27.08%) | 4410 (27%) | 29 (26.85%) | 1374 (26.05%) | 1403 (26.07%) | 5813 (26.77%) | |||
| Mild to moderate | 3 (1.01%) | 88 (0.55%) | 91 (0.56%) | 3 (2.78%) | 31 (0.59%) | 34 (0.63%) | 125 (0.58%) | |||
| Moderate | 8 (2.7%) | 156 (0.97%) | 164 (1%) | 2 (1.85%) | 60 (1.14%) | 62 (1.15%) | 226 (1.04%) | |||
| Moderate to severe | 0 (0%) | 4 (0.02%) | 4 (0.02%) | 1 (0.93%) | 3 (0.06%) | 4 (0.07%) | 8 (0.04%) | |||
| Severe | 0 (0%) | 8 (0.05%) | 8 (0.05%) | 0 (0%) | 2 (0.04%) | 2 (0.04%) | 10 (0.05%) | |||
| TR* | Negative | 10 (2.83%) | 235 (1.45%) | 245 (1.47%) | 0.033 | 5 (4.2%) | 71 (1.33%) | 76 (1.39%) | 0.153 | 321 (1.45%) |
| Slight | 165 (46.74%) | 8606 (52.92%) | 8771 (52.79%) | 55 (46.22%) | 2845 (53.29%) | 2900 (53.13%) | 11671 (52.88%) | |||
| Mild | 128 (36.26%) | 5930 (36.47%) | 6058 (36.46%) | 35 (29.41%) | 1922 (36%) | 1957 (35.86%) | 8015 (36.31%) | |||
| Mild to moderate | 25 (7.08%) | 832 (5.12%) | 857 (5.16%) | 16 (13.45%) | 290 (5.43%) | 306 (5.61%) | 1163 (5.27%) | |||
| Moderate | 15 (4.25%) | 468 (2.88%) | 483 (2.91%) | 7 (5.88%) | 144 (2.7%) | 151 (2.77%) | 634 (2.87%) | |||
| Moderate to severe | 3 (0.85%) | 87 (0.54%) | 90 (0.54%) | 1 (0.84%) | 28 (0.52%) | 29 (0.53%) | 119 (0.54%) | |||
| Severe | 7 (1.98%) | 103 (0.63%) | 110 (0.66%) | 0 (0%) | 39 (0.73%) | 39 (0.71%) | 149 (0.68%) | |||
| White blood cell count* | Normal | 258 (83.23%) | 13271 (93.91%) | 13529 (93.68%) | 101 (84.87%) | 4390 (93.98%) | 4491 (93.76%) | 18020 (93.7%) | ||
| Abnormal | 52 (16.77%) | 861 (6.09%) | 913 (6.32%) | 18 (15.13%) | 281 (6.02%) | 299 (6.24%) | 1212 (6.3%) | |||
| Lymphocyte count | Normal | 93 (30%) | 4199 (29.71%) | 4292 (29.72%) | 0.913 | 35 (29.41%) | 1395 (29.86%) | 1430 (29.85%) | 0.916 | 5722 (29.75%) |
| Abnormal | 217 (70%) | 9933 (70.29%) | 10150 (70.28%) | 84 (70.59%) | 3277 (70.14%) | 3361 (70.15%) | 13511 (70.25%) | |||
| Monocyte count* | Normal | 147 (47.42%) | 9971 (70.56%) | 10118 (70.06%) | 59 (49.58%) | 3240 (69.35%) | 3299 (68.86%) | 13417 (69.76%) | ||
| Abnormal | 163 (52.58%) | 4161 (29.44%) | 4324 (29.94%) | 60 (50.42%) | 1432 (30.65%) | 1492 (31.14%) | 5816 (30.24%) | |||
| Neutrophil count* | Normal | 182 (58.71%) | 10609 (75.07%) | 10791 (74.72%) | 79 (66.39%) | 3498 (74.87%) | 3577 (74.66%) | 0.036 | 14368 (74.7%) | |
| Abnormal | 128 (41.29%) | 3523 (24.93%) | 3651 (25.28%) | 40 (33.61%) | 1174 (25.13%) | 1214 (25.34%) | 4865 (25.3%) | |||
| Eosinophil count* | Normal | 148 (49.33%) | 8182 (59.86%) | 8330 (59.63%) | 56 (48.7%) | 2749 (60.93%) | 2805 (60.62%) | 0.008 | 11135 (59.88%) | |
| Abnormal | 152 (50.67%) | 5487 (40.14%) | 5639 (40.37%) | 59 (51.3%) | 1763 (39.07%) | 1822 (39.38%) | 7461 (40.12%) | |||
| Basophil cell count* | Normal | 259 (86.33%) | 13083 (95.71%) | 13342 (95.51%) | 101 (87.83%) | 4314 (95.61%) | 4415 (95.42%) | 17757 (95.49%) | ||
| Abnormal | 41 (13.67%) | 586 (4.29%) | 627 (4.49%) | 14 (12.17%) | 198 (4.39%) | 212 (4.58%) | 839 (4.51%) | |||
| Lymphocyte ratio* | Normal | 92 (29.68%) | 3539 (25.04%) | 3631 (25.14%) | 0.063 | 41 (34.45%) | 1188 (25.43%) | 1229 (25.65%) | 0.026 | 4860 (25.27%) |
| Abnormal | 218 (70.32%) | 10593 (74.96%) | 10811 (74.86%) | 78 (65.55%) | 3484 (74.57%) | 3562 (74.35%) | 14373 (74.73%) | |||
| Red blood cell count* | Normal | 197 (63.55%) | 11561 (81.81%) | 11758 (81.42%) | 81 (68.07%) | 3825 (81.87%) | 3906 (81.53%) | 15664 (81.44%) | ||
| Abnormal | 113 (36.45%) | 2571 (18.19%) | 2684 (18.58%) | 38 (31.93%) | 847 (18.13%) | 885 (18.47%) | 3569 (18.56%) | |||
| Hemoglobin* | Normal | 197 (63.55%) | 9645 (68.25%) | 9842 (68.15%) | 0.079 | 82 (68.91%) | 3246 (69.48%) | 3328 (69.46%) | 0.894 | 13170 (68.48%) |
| Abnormal | 113 (36.45%) | 4487 (31.75%) | 4600 (31.85%) | 37 (31.09%) | 1426 (30.52%) | 1463 (30.54%) | 6063 (31.52%) | |||
| Hematocrit | Normal | 225 (71.88%) | 9974 (70.54%) | 10199 (70.57%) | 0.606 | 91 (75.83%) | 3317 (70.92%) | 3408 (71.04%) | 0.241 | 13607 (70.69%) |
| Abnormal | 88 (28.12%) | 4165 (29.46%) | 4253 (29.43%) | 29 (24.17%) | 1360 (29.08%) | 1389 (28.96%) | 5642 (29.31%) | |||
| Mean corpuscular volume* | Normal | 230 (74.19%) | 9646 (68.26%) | 9876 (68.38%) | 0.026 | 83 (69.75%) | 3183 (68.13%) | 3266 (68.17%) | 0.708 | 13142 (68.33%) |
| Abnormal | 80 (25.81%) | 4486 (31.74%) | 4566 (31.62%) | 36 (30.25%) | 1489 (31.87%) | 1525 (31.83%) | 6091 (31.67%) | |||
| MHC/MCH (solid mass)* | Normal | 192 (61.94%) | 6948 (49.17%) | 7140 (49.44%) | 72 (60.5%) | 2299 (49.21%) | 2371 (49.49%) | 0.015 | 9511 (49.45%) | |
| Abnormal | 118 (38.06%) | 7184 (50.83%) | 7302 (50.56%) | 47 (39.5%) | 2373 (50.79%) | 2420 (50.51%) | 9722 (50.55%) | |||
| MHC/MCHC (mass concentration)* | Normal | 211 (68.06%) | 10816 (76.54%) | 11027 (76.35%) | 0.001 | 77 (64.71%) | 3589 (76.82%) | 3666 (76.52%) | 0.002 | 14693 (76.39%) |
| Abnormal | 99 (31.94%) | 3316 (23.46%) | 3415 (23.65%) | 42 (35.29%) | 1083 (23.18%) | 1125 (23.48%) | 4540 (23.61%) | |||
| RDW-SD* | Normal | 39 (12.58%) | 6021 (42.61%) | 6060 (41.96%) | 21 (17.65%) | 2028 (43.41%) | 2049 (42.77%) | 8109 (42.16%) | ||
| Abnormal | 271 (87.42%) | 8111 (57.39%) | 8382 (58.04%) | 98 (82.35%) | 2644 (56.59%) | 2742 (57.23%) | 11124 (57.84%) | |||
| Platelet count* | Normal | 235 (75.81%) | 12706 (89.91%) | 12941 (89.61%) | 100 (84.03%) | 4220 (90.33%) | 4320 (90.17%) | 0.023 | 17261 (89.75%) | |
| Abnormal | 75 (24.19%) | 1426 (10.09%) | 1501 (10.39%) | 19 (15.97%) | 452 (9.67%) | 471 (9.83%) | 1972 (10.25%) | |||
| Mean platelet volume* | Normal | 211 (68.06%) | 11008 (77.9%) | 11219 (77.69%) | 81 (68.07%) | 3625 (77.61%) | 3706 (77.37%) | 0.014 | 14925 (77.61%) | |
| Abnormal | 99 (31.94%) | 3123 (22.1%) | 3222 (22.31%) | 38 (31.93%) | 1046 (22.39%) | 1084 (22.63%) | 4306 (22.39%) | |||
| APTT* | Normal | 148 (48.21%) | 9173 (66.12%) | 7211 (83.06%) | 0.019 | 60 (50.42%) | 3065 (66.85%) | 3125 (66.43%) | 12446 (65.9%) | |
| Abnormal | 159 (51.79%) | 4701 (33.88%) | 1471 (16.94%) | 59 (49.58%) | 1520 (33.15%) | 1579 (33.57%) | 6439 (34.1%) | |||
| Prothrombin time* | Normal | 138 (44.81%) | 9721 (70.06%) | 9321 (65.73%) | 47 (39.17%) | 3236 (70.49%) | 3283 (69.69%) | 13142 (69.55%) | ||
| Abnormal | 170 (55.19%) | 4155 (29.94%) | 4860 (34.27%) | 73 (60.83%) | 1355 (29.51%) | 1428 (30.31%) | 5753 (30.45%) | |||
| Total protein* | Normal | 84 (27.54%) | 6555 (47.44%) | 6639 (47.02%) | 34 (28.81%) | 2187 (47.85%) | 2221 (47.37%) | 8860 (47.1%) | ||
| Abnormal | 221 (72.46%) | 7261 (52.56%) | 7482 (52.98%) | 84 (71.19%) | 2384 (52.15%) | 2468 (52.63%) | 9950 (52.9%) | |||
| Serum albumin* | Normal | 205 (66.99%) | 12128 (87.67%) | 12333 (87.22%) | 81 (68.07%) | 3984 (87.12%) | 4065 (86.64%) | 16398 (87.08%) | ||
| Abnormal | 101 (33.01%) | 1706 (12.33%) | 1807 (12.78%) | 38 (31.93%) | 589 (12.88%) | 627 (13.36%) | 2434 (12.92%) | |||
| Serum globulin* | Normal | 188 (61.64%) | 10800 (78.2%) | 10988 (77.84%) | 76 (64.41%) | 3601 (78.8%) | 3677 (78.43%) | 14665 (77.99%) | ||
| Abnormal | 117 (38.36%) | 3011 (21.8%) | 3128 (22.16%) | 42 (35.59%) | 969 (21.2%) | 1011 (21.57%) | 4139 (22.01%) | |||
| Albumin/globulin ratio* | Normal | 205 (67.21%) | 11065 (80.12%) | 11270 (79.84%) | 76 (64.41%) | 3648 (79.82%) | 3724 (79.44%) | 14994 (79.74%) | ||
| Abnormal | 100 (32.79%) | 2746 (19.88%) | 2846 (20.16%) | 42 (35.59%) | 922 (20.18%) | 964 (20.56%) | 3810 (20.26%) | |||
| ALT* | Normal | 234 (76.47%) | 12334 (89.09%) | 12568 (88.82%) | 94 (78.99%) | 4055 (88.61%) | 4149 (88.37%) | 0.001 | 16717 (88.71%) | |
| Abnormal | 72 (23.53%) | 1510 (10.91%) | 1582 (11.18%) | 25 (21.01%) | 521 (11.39%) | 546 (11.63%) | 2128 (11.29%) | |||
| Aspartate aminotransferase* | Normal | 130 (42.62%) | 7806 (56.39%) | 7936 (56.09%) | 53 (44.54%) | 2516 (54.98%) | 2569 (54.72%) | 0.024 | 10505 (55.75%) | |
| Abnormal | 175 (57.38%) | 6038 (43.61%) | 6213 (43.91%) | 66 (55.46%) | 2060 (45.02%) | 2126 (45.28%) | 8339 (44.25%) | |||
| ALP* | Normal | 292 (95.74%) | 13601 (98.44%) | 13893 (98.39%) | 0.001 | 115 (97.46%) | 4497 (98.38%) | 4612 (98.36%) | 0.444 | 18505 (98.38%) |
| Abnormal | 13 (4.26%) | 215 (1.56%) | 228 (1.61%) | 3 (2.54%) | 74 (1.62%) | 77 (1.64%) | 305 (1.62%) | |||
| L- |
Normal | 202 (66.23%) | 9082 (65.74%) | 9284 (65.75%) | 0.857 | 79 (66.95%) | 2924 (63.97%) | 3003 (64.04%) | 0.505 | 12287 (65.32%) |
| Abnormal | 103 (33.77%) | 4734 (34.26%) | 4837 (34.25%) | 39 (33.05%) | 1647 (36.03%) | 1686 (35.96%) | 6523 (34.68%) | |||
| Total bilirubin* | Normal | 140 (48.78%) | 11207 (81.73%) | 11347 (81.05%) | 64 (58.72%) | 3648 (80.44%) | 3712 (79.93%) | 15059 (80.77%) | ||
| Abnormal | 147 (51.22%) | 2506 (18.27%) | 2653 (18.95%) | 45 (41.28%) | 887 (19.56%) | 932 (20.07%) | 3585 (19.23%) | |||
| Direct bilirubin* | Normal | 191 (67.73%) | 11953 (90.28%) | 12144 (89.81%) | 82 (77.36%) | 3946 (90.32%) | 4028 (90.01%) | 16172 (89.86%) | ||
| Abnormal | 91 (32.27%) | 1287 (9.72%) | 1378 (10.19%) | 24 (22.64%) | 423 (9.68%) | 447 (9.99%) | 1825 (10.14%) | |||
| Creatinine* | Normal | 283 (92.48%) | 13682 (98.89%) | 13965 (98.76%) | 109 (91.6%) | 4527 (98.97%) | 4636 (98.79%) | 18601 (98.76%) | ||
| Abnormal | 23 (7.52%) | 153 (1.11%) | 176 (1.24%) | 10 (8.4%) | 47 (1.03%) | 57 (1.21%) | 233 (1.24%) | |||
| Uric acid* | Normal | 150 (49.02%) | 8159 (58.99%) | 8309 (58.77%) | 52 (43.7%) | 2656 (58.07%) | 2708 (57.7%) | 0.002 | 11017 (58.5%) | |
| Abnormal | 156 (50.98%) | 5673 (41.01%) | 5829 (41.23%) | 67 (56.3%) | 1918 (41.93%) | 1985 (42.3%) | 7814 (41.5%) | |||
| Eosinophils/100 leukocytes* | Normal | 194 (64.45%) | 10744 (78.6%) | 10938 (78.29%) | 67 (58.26%) | 3572 (79.15%) | 3639 (78.63%) | 14577 (78.38%) | ||
| Abnormal | 107 (35.55%) | 2926 (21.4%) | 3033 (21.71%) | 48 (41.74%) | 941 (20.85%) | 989 (21.37%) | 4022 (21.62%) | |||
| Monocytes/100 leukocytes* | Normal | 274 (88.39%) | 13121 (92.85%) | 13395 (92.75%) | 0.003 | 104 (87.39%) | 4317 (92.4%) | 4421 (92.28%) | 0.043 | 17816 (92.63%) |
| Abnormal | 36 (11.61%) | 1011 (7.15%) | 1047 (7.25%) | 15 (12.61%) | 355 (7.6%) | 370 (7.72%) | 1417 (7.37%) | |||
| Neutrophils/100 leukocytes | Normal | 72 (23.23%) | 3404 (24.09%) | 3476 (24.07%) | 0.726 | 23 (19.33%) | 1150 (24.61%) | 1173 (24.48%) | 0.185 | 4649 (24.17%) |
| Abnormal | 238 (76.77%) | 10728 (75.91%) | 10966 (75.93%) | 96 (80.67%) | 3522 (75.39%) | 3618 (75.52%) | 14584 (75.83%) | |||
| Basophils/100 leukocytes* | Normal | 239 (79.4%) | 12199 (89.26%) | 12438 (89.05%) | 94 (81.74%) | 4015 (88.98%) | 4109 (88.8%) | 0.015 | 16547 (88.99%) | |
| Abnormal | 62 (20.6%) | 1468 (10.74%) | 1530 (10.95%) | 21 (18.26%) | 497 (11.02%) | 518 (11.2%) | 2048 (11.01%) | |||
| TFIC* | Normal | 249 (80.84%) | 12561 (90.65%) | 12810 (90.44%) | 99 (82.5%) | 4145 (90.4%) | 4244 (90.2%) | 0.004 | 17054 (90.38%) | |
| Abnormal | 59 (19.16%) | 1295 (9.35%) | 1354 (9.56%) | 21 (17.5%) | 440 (9.6%) | 461 (9.8%) | 1815 (9.62%) | |||
| Main defect* | ||||||||||
| TGA | 0 | 405 (91.6%) | 17645 (97.4%) | 18050 (97.3%) | 138 (92.6%) | 5825 (97.3%) | 5963 (97.2%) | 0.003 | 24013 (97.3%) | |
| 1 | 37 (8.4%) | 465 (2.6%) | 502 (2.7%) | 11 (7.4%) | 159 (2.7%) | 170 (2.8%) | 672 (2.7%) | |||
| APVC | 0 | 419 (94.8%) | 17618 (97.3%) | 18037 (97.2%) | 0.002 | 146 (98.0%) | 5833 (97.5%) | 5979 (97.5%) | 1 | 24016 (97.3%) |
| 1 | 23 (5.2%) | 492 (2.7%) | 515 (2.8%) | 3 (2.0%) | 151 (2.5%) | 154 (2.5%) | 669 (2.7%) | |||
| COA | 0 | 431 (97.5%) | 17521 (96.7%) | 17952 (96.8%) | 0.37 | 146 (98.0%) | 5793 (96.8%) | 5939 (96.8%) | 0.632 | 23891 (96.8%) |
| 1 | 11 (2.5%) | 589 (3.3%) | 600 (3.2%) | 3 (2.0%) | 191 (3.2%) | 194 (3.2%) | 794 (3.2%) | |||
| IAA | 0 | 433 (98.0%) | 18023 (99.5%) | 18456 (99.5%) | 145 (97.3%) | 5951 (99.4%) | 6096 (99.4%) | 0.012 | 24552 (99.5%) | |
| 1 | 9 (2.0%) | 87 (0.5%) | 96 (0.5%) | 4 (2.7%) | 33 (0.6%) | 37 (0.6%) | 133 (0.5%) | |||
| AVC | 0 | 433 (98.0%) | 17585 (97.1%) | 18018 (97.1%) | 0.284 | 143 (96.0%) | 5820 (97.3%) | 5963 (97.2%) | 0.309 | 23981 (97.1%) |
| 1 | 9 (2.0%) | 525 (2.9%) | 534 (2.9%) | 6 (4.0%) | 164 (2.7%) | 170 (2.8%) | 704 (2.9%) | |||
| Single ventricle | 0 | 421 (95.2%) | 17844 (98.5%) | 18265 (98.5%) | 144 (96.6%) | 5893 (98.5) | 6037 (98.4%) | 0.084 | 24302 (98.4%) | |
| 1 | 21 (4.8%) | 266 (1.5%) | 287 (1.5%) | 5 (3.4%) | 91 (1.5%) | 96 (1.6%) | 383 (1.6%) | |||
| DORV | 0 | 415 (93.9%) | 17608 (97.2%) | 18023 (97.1%) | 134 (89.9%) | 5821 (97.3%) | 5955 (97.1%) | 23978 (97.1) | ||
| 1 | 27 (6.1%) | 502 (2.8%) | 529 (2.9%) | 15 (10.1%) | 163 (2.7%) | 178 (2.9%) | 707 (2.9%) | |||
| ASD | 0 | 326 (73.8%) | 11528 (63.7%) | 11854 (63.9%) | 105 (70.5%) | 3808 (63.6%) | 3913 (63.8%) | 0.086 | 15767 (63.9%) | |
| 1 | 116 (26.2%) | 6582 (36.3%) | 6698 (36.1%) | 44 (29.5%) | 2176 (36.4%) | 2220 (36.2%) | 8918 (36.1%) | |||
| VSD | 0 | 325 (73.5%) | 10741 (59.3%) | 11066 (59.6%) | 106 (71.1%) | 3555 (59.4%) | 3661 (59.7%) | 0.004 | 14727 (59.7%) | |
| 1 | 117 (26.5%) | 7369 (40.7%) | 7486 (40.4%) | 43 (28.9%) | 2429 (40.6%) | 2472 (40.3%) | 9958 (40.3%) | |||
| PFO | 0 | 420 (95.0%) | 16294 (90.0%) | 16714 (90.1%) | 142 (95.3%) | 5376 (89.8%) | 5518 (90.0%) | 0.028 | 22232 (90.1%) | |
| 1 | 22 (5.0%) | 1816 (10.0%) | 1838 (9.9%) | 7 (4.7%) | 608 (10.2%) | 615 (10.0%) | 2453 (9.9%) | |||
| TOF | 0 | 400 (90.5%) | 16731 (92.4%) | 17131 (92.3%) | 0.14 | 142 (95.3%) | 5508 (92.0%) | 5650 (92.1%) | 0.145 | 22781 (92.3%) |
| 1 | 42 (9.5%) | 1379 (7.6%) | 1421 (7.7%) | 7 (4.7%) | 476 (8.0%) | 483 (7.9%) | 1904 (7.7%) | |||
| PDA | 0 | 355 (80.3%) | 15892 (87.8%) | 16247 (87.6%) | 118 (79.2%) | 5272 (88.1%) | 5390 (87.9%) | 0.001 | 21637 (87.7%) | |
| 1 | 87 (19.7%) | 2218 (12.2%) | 2305 (12.4%) | 31 (20.8%) | 712 (11.9%) | 743 (12.1%) | 3048 (12.3%) | |||
| Pulmonary hypertension | 0 | 391 (88.5%) | 15070 (83.2%) | 15461 (83.3%) | 0.003 | 121 (81.2%) | 5008 (83.7%) | 5129 (83.6%) | 0.419 | 20590 (83.4%) |
| 1 | 51 (11.5%) | 3040 (16.8%) | 3091 (16.7%) | 28 (18.8%) | 976 (16.3%) | 1004 (16.4%) | 4095 (16.6%) | |||
| Numbers of defects* | 0 | 232 (52.5%) | 6418 (35.4%) | 6650 (35.8%) | 74 (49.7%) | 2161 (36.1%) | 2235 (36.4%) | 8885 (36.0%) | ||
| 1 | 33 (7.5%) | 4405 (24.3%) | 4438 (23.9%) | 18 (12.1%) | 1380 (23.1%) | 1398 (22.8%) | 5836 (23.6%) | |||
| 2 | 58 (13.1%) | 3918 (21.6%) | 3976 (21.4%) | 14 (9.4%) | 1350 (22.6%) | 1364 (22.2%) | 5340 (21.6%) | |||
| 3 | 48 (10.9%) | 1700 (9.4%) | 1748 (9.4%) | 17 (11.4%) | 554 (9.3%) | 571 (9.3%) | 2319 (9.4%) | |||
| 4 | 44 (10.0%) | 1059 (5.8%) | 1103 (5.9%) | 15 (10.1%) | 332 (5.5%) | 347 (5.7%) | 1450 (5.9%) | |||
| 5 | 19 (4.3%) | 483 (2.7%) | 502 (2.7%) | 9 (6.0%) | 167 (2.8%) | 176 (2.9%) | 678 (2.7%) | |||
| 6 | 7 (1.6%) | 116 (0.6%) | 123 (0.7%) | 2 (1.3%) | 37 (0.6%) | 39 (0.6%) | 162 (0.7%) | |||
| 7 | 1 (0.2%) | 10 (0.1%) | 11 (0.1%) | 0 (0.0) | 3 (0.1%) | 3 (0.0%) | 14 (0.1%) | |||
| 8 | 0 (0.0%) | 1 (0.0%) | 1 (0.0%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0%) | |||
| Preoperative mechanical ventilation* | 0 | 307 (69.5%) | 16599 (91.7%) | 16906 (91.1%) | 107 (71.8%) | 5473 (91.5%) | 5580 (91.0%) | 22486 (91.1%) | ||
| 1 | 135 (30.5%) | 1511 (8.3%) | 1646 (8.9%) | 42 (28.2%) | 511 (8.5%) | 553 (9.0%) | 2199 (8.9%) | |||
| Categorical variables are described using frequency (%). Continuous variables
are described as the median (range). AAO, Ascending aorta dimension; DAO, Descending aorta dimension; MPA, Main pulmonary artery dimension; MV, Mitral blood flow velocity; TV2, Transtricuspid velocity2; BMI, Body mass index; HCT, Hematocrit; LVDD, Left ventricular end diastolic dimension; LVEF, Left ventricular ejection fraction; LVFS, Left ventricular fraction shortening; LVPWD, Left ventricular posterior wall dimension; AI, Aortic insufficiency; MR, Mitral regurgitation; PI, Pulmonary insufficiency; TR, Tricuspid regurgitation; RDW-SD, Red blood cell volume distribution width-standard deviation; ALP, Alkaline phosphatase; MHC/MCH, Mean hemoglobin content/mean corpuscular hemoglobin; ALT, Alanine aminotransferase; MHC/MCHC, Mean hemoglobin concentration/mean corpuscular hemoglobin concentration; APTT, Activated partial thromboplastin time; TFIC, Tissue factor induced coagulation; TGA, transposition of the great arteries; APVC, anomalous pulmonary venous connection; COA, coarctation of the aorta; IAA, interrupted aortic arch; AVC, atrioventricular canal; DORV, double-outlet right ventricle; ASD, atrial septal defect; PDA, patent ductus arteriosus; PFO, patent foramen ovale; TOF, tetralogy of Fallot; VSD, ventricular septal defect. Note: variables marked with * are included in the XGBoost model. | ||||||||||
Comparative analysis of in-hospital mortality and risk categories for each procedure are listed in Table 2. The most common procedures included ventricular septal defect (VSD) membranous repair, tetralogy repair, and VSD subarterial repair. The RACHS-1 categories consist of six groups labeled 1–6, and the STS-EACTS categories consists of five groups labeled 1–5, a higher number means a higher mortality risk. The risk of mortality associated with each procedure was calculated. The in-hospital mortality rate for each procedure ranged from 0–75%, and no death was recorded in 31 procedures. Mortality rates and risk stratification for specific procedures were also estimated using a Bayesian random effects model.
| Procedure | Cases (n) | Death (n) | Mortality (unadjusted) | Mortality (model* based) | Risk stratification | RACHS-1 Grade | STS-EACTS Grade |
| ASD hybrid repair (off pump) | 87 | 0 | 0% | 0.46% | 1 | 2 | 2 |
| ASD secundum repair | 551 | 1 | 0.18% | 0.13% | 1 | 1 | 1 |
| ASD secundum repair (patch) | 1338 | 1 | 0.07% | 0.14% | 1 | 1 | 1 |
| AVSD repair - depression | 391 | 3 | 0.77% | 0.42% | 1 | 3 | 3 |
| AVSD repair - single patch | 116 | 1 | 0.86% | 0.39% | 1 | 3 | 3 |
| Aortic valvuloplasty | 109 | 1 | 0.92% | 0.40% | 1 | 2 | 2 |
| Coronary art. fistula repair | 78 | 0 | 0% | 0.50% | 1 | 2 | 2 |
| Cortraitriatum repair | 70 | 0 | 0% | 0.50% | 1 | 3 | 2 |
| Mitral valvuloplasty | 461 | 7 | 1.52% | 0.85% | 1 | 3 | 2 |
| PAPVD isolated repair | 115 | 0 | 0% | 0.37% | 1 | 1 | 1 |
| Pulm. Infundibulum resection (indirect) | 178 | 0 | 0% | 0.31% | 1 | 2 | 1 |
| Subaortic fibromyectomy | 155 | 0 | 0% | 0.32% | 1 | 3 | 1 |
| Subaortic myectomy | 80 | 1 | 1.25% | 0.52% | 1 | 3 | 1 |
| Tricuspid valvuloplasty | 540 | 3 | 0.56% | 0.77% | 1 | 3 | 2 |
| VSD canal type repair | 154 | 0 | 0% | 0.33% | 1 | 3 | 1 |
| VSD membranous repair | 7910 | 23 | 0.29% | 0.33% | 1 | 2 | 1 |
| VSD subarterial repair | 1641 | 1 | 0.06% | 0.12% | 1 | 2 | 1 |
| Vascular ring repair | 132 | 0 | 0% | 0.37% | 1 | 2 | 1 |
| A-P window repair | 31 | 1 | 3.23% | 0.79% | 2 | 2 | 2 |
| A-V fistula repair | 6 | 1 | 16.67% | 1.53% | 2 | 2 | 2 |
| ASD common atrium repair | 9 | 0 | 0% | 1.27% | 2 | 2 | 2 |
| ASD repair - minimal invasive & CPB | 29 | 0 | 0% | 0.81% | 2 | 2 | 2 |
| ASD sinus venosus repair | 38 | 0 | 0% | 0.67% | 2 | 1 | 2 |
| Aortic valvotomy | 56 | 0 | 0% | 0.61% | 2 | 2 | 2 |
| Asc. aorta patch aortoplasty | 184 | 6 | 3.26% | 1.97% | 2 | 2 | 2 |
| Coarct repair - bypass or tubular graft | 4 | 0 | 0% | 1.53% | 2 | 1 | 1 |
| Coarct. repair - resection & E to S | 377 | 10 | 2.65% | 1.64% | 2 | 1/2 | 2 |
| Coarct. repair - patch aortoplasty | 253 | 4 | 1.58% | 1.92% | 2 | 1/2 | 3 |
| DORV repair - IVR | 375 | 12 | 3.20% | 3.09% | 2 | 3 | 4 |
| Ebstein anomaly repair | 106 | 1 | 0.94% | 1.17% | 2 | 3 | 4 |
| Excision of cardiac tumor | 96 | 2 | 2.08% | 2.39% | 2 | 3 | 4 |
| Exicion of intracardiac vegetation | 11 | 0 | 0% | 1.22% | 2 | 2 | 2 |
| Fontan operation - I stage | 110 | 4 | 3.64% | 2.97% | 2 | 3 | 2 |
| Hemitruncus repair | 21 | 0 | 0% | 1.02% | 2 | 4 | 2 |
| PDA closure (CPB) | 32 | 0 | 0% | 0.82% | 2 | 1 | 2 |
| PDA closure (off pump) | 386 | 6 | 1.55% | 1.62% | 2 | 1 | 2 |
| Pacemaker - re-implant | 8 | 0 | 0% | 1.34% | 2 | 1 | 1 |
| Pericardectomy | 20 | 0 | 0% | 0.99% | 2 | 1 | 2 |
| Pericardial drainage | 160 | 8 | 5% | 3.26% | 2 | 1 | 4 |
| Pulm. Infundibulum incision & resection | 46 | 1 | 2.17% | 1.99% | 2 | 2 | 1 |
| Pulmonary art. sling repair | 20 | 0 | 0% | 0.96% | 2 | 3 | 3 |
| Pulmonary art. stent | 13 | 0 | 0% | 1.17% | 2 | 2 | 2 |
| Pulmonary arterioplasty | 251 | 8 | 3.19% | 3.42% | 2 | 2 | 2 |
| Pulmonary valvotomy | 200 | 3 | 1.50% | 1.29% | 2 | 2 | 2 |
| Pulmonary valvotomy - hybrid | 5 | 0 | 0% | 1.43% | 2 | 2 | 2 |
| Subaortic septal patch (Konno) | 15 | 0 | 0% | 1.05% | 2 | 4 | 3 |
| Supravalve mitral ring resection | 28 | 0 | 0% | 0.79% | 2 | 3 | 2 |
| Systemic vein repair | 14 | 0 | 0% | 1.12% | 2 | 2 | 3 |
| TAPVD repair - intracardiac | 184 | 2 | 1.09% | 1.32% | 2 | 2/4 | 4 |
| TAPVD repair - mixed type | 34 | 1 | 2.94% | 2.67% | 2 | 2/4 | 4 |
| Tetralogy repair | 2392 | 46 | 1.92% | 1.95% | 2 | 2 | 2 |
| Tricuspid replacement (mech.) | 13 | 0 | 0% | 1.17% | 2 | 3 | 2 |
| VSD Hybrid repair (off pump) | 171 | 1 | 0.58% | 0.84% | 2 | 2 | 2 |
| VSD hybrid repair (CPB) | 21 | 0 | 0% | 0.99% | 2 | 2 | 2 |
| VSD multiple repair | 127 | 2 | 1.57% | 1.75% | 2 | 2 | 2 |
| VSD muscular repair | 105 | 1 | 0.95% | 1.20% | 2 | 2 | 1 |
| VSD repair - minimal invasive & CPB | 45 | 0 | 0% | 0.71% | 2 | 2 | 2 |
| AVSD repair - two patches | 269 | 15 | 5.58% | 5.27% | 3 | 3 | 3 |
| Ao translocation operation | 17 | 2 | 11.76% | 4.60% | 3 | 3 | 3 |
| Aortic arch repair | 70 | 5 | 7.14% | 6.30% | 3 | 4 | 4 |
| Aortic valve replacement (mech.) | 45 | 3 | 6.67% | 4.46% | 3 | 3 | 1 |
| Cavopulmonary shunt - bilateral | 102 | 6 | 5.88% | 4.61% | 3 | 2 | 2 |
| DOLV repair | 4 | 0 | 0% | 2.05% | 3 | 3 | 4 |
| Delayed sternal closure | 891 | 51 | 5.72% | 6.23% | 3 | 1 | 1 |
| Double switch (Senning + Rastelli) | 3 | 0 | 0% | 1.80% | 3 | 4 | 5 |
| Excision of cardiac diverticulum | 4 | 0 | 0% | 1.53% | 3 | 2 | 2 |
| Fontan operation - II stage | 537 | 30 | 5.59% | 5.77% | 3 | 3 | 2 |
| Kawashima procedure | 4 | 0 | 0% | 2.05% | 3 | 3 | 1 |
| Mitral replacement (mech.) | 96 | 11 | 11.46% | 7.86% | 3 | 3 | 4 |
| PA banding | 101 | 12 | 11.88% | 3.78% | 3 | 3 | 4 |
| Pulm. infundibulum resection & patch | 78 | 4 | 5.13% | 4.48% | 3 | 2 | 1 |
| Pulm. infundibulum resection, patch across annulus | 292 | 15 | 5.14% | 6.09% | 3 | 2 | 2 |
| Pulm. vein stenosis repair | 40 | 2 | 5% | 5% | 3 | 4 | 4 |
| Pulmonary atresia/IVS repair | 19 | 2 | 10.53% | 4.87% | 3 | 4 | 3 |
| Pulmonary atresia/VSD repair | 288 | 17 | 5.90% | 6.24% | 3 | 4 | 3 |
| Pulmonary valvotomy (off pump) | 18 | 1 | 5.56% | 4.60% | 3 | 2 | 2 |
| Senning procedure | 19 | 1 | 5.26% | 4.34% | 3 | 3 | 4 |
| TAPVD repair - supracardiac | 238 | 13 | 5.46% | 5.77% | 3 | 2/4 | 4 |
| ALC-PA repair | 58 | 10 | 17.24% | 14.97% | 4 | 3 | 2 |
| Cavopulmonary shunt - left | 83 | 11 | 13.25% | 12.68% | 4 | 2 | 1 |
| Cavopulmonary shunt - right | 359 | 35 | 9.75% | 10.85% | 4 | 2 | 1 |
| Central shunt - with graft | 38 | 8 | 21.05% | 11.02% | 4 | 3 | 4 |
| Conduit RV - PA | 72 | 13 | 18.06% | 13.98% | 4 | 2 | 3 |
| Double Switch (Hemi-Mustard) | 6 | 1 | 16.67% | 9.32% | 4 | 4 | 5 |
| Interrupted aortic arch repair | 77 | 11 | 14.29% | 13.32% | 4 | 5 | 4 |
| Interruption of bronchial collaterals | 8 | 1 | 12.50% | 9.32% | 4 | 1 | 2 |
| Pacemaker - primary implant | 17 | 2 | 11.76% | 11.95% | 4 | 1 | 1 |
| R.E.V. RV - PA connection | 7 | 1 | 14.29% | 8.28% | 4 | 4 | 3 |
| Rastelli operation | 50 | 6 | 12% | 9.44% | 4 | 4 | 3 |
| Rt. or lt. heart assist | 8 | 3 | 37.50% | 9.32% | 4 | 2 | 1 |
| TAPVD repair - infracardiac | 43 | 6 | 13.95% | 14.74% | 4 | 2/4 | 4 |
| Takedown previous shunt | 11 | 1 | 9.09% | 6.80% | 4 | 2 | 3 |
| Arterial switch repair | 456 | 87 | 19.08% | 19.20% | 5 | 3 | 3 |
| Atrial septectomy | 12 | 4 | 33.33% | 27.36% | 5 | 4 | 4 |
| Coronary artery repair | 6 | 2 | 33.33% | 24% | 5 | 3 | 2 |
| DKS connection | 9 | 4 | 44.44% | 30.71% | 5 | 6 | 5 |
| Double switch (Senning + ASO) | 18 | 6 | 33.33% | 18.03% | 5 | 4 | 5 |
| Fontan takedown | 9 | 5 | 55.56% | 41.71% | 5 | 3 | 3 |
| Norwood operation | 4 | 3 | 75% | 50.76% | 5 | 6 | 5 |
| PA debanding | 3 | 1 | 33.33% | 16.53% | 5 | 3 | 4 |
| PA unifocalization | 61 | 11 | 18.03% | 21% | 5 | 4 | 4 |
| Truncus repair | 33 | 7 | 21.21% | 20.44% | 5 | 4 | 4 |
| ASD, Atrial septal defect; AVSD, Atrioventricular septal defect; PAPVD, Partial
anomalous pulmonary venous drainage; VSD, Ventricular septal defect. A-P window, Aorto-pulmonary window; A-V fistula, Arteriovenous fistula; DORV, Double outlet right ventricle; CPB, Cardiopulmonary bypass. PDA, Patent ductus arteriosus; TAPVD, Total anomalous pulmonary venous drainage; ALC-PA, Anomalous left coronary artery from pulmonary artery. RV, Right ventricle; PA, Pulmonary artery; DKS connection, Damus–Kaye–Stansel (DKS) procedure; ASO, Arterial switch operation. *: Bayesian random effect model. | |||||||
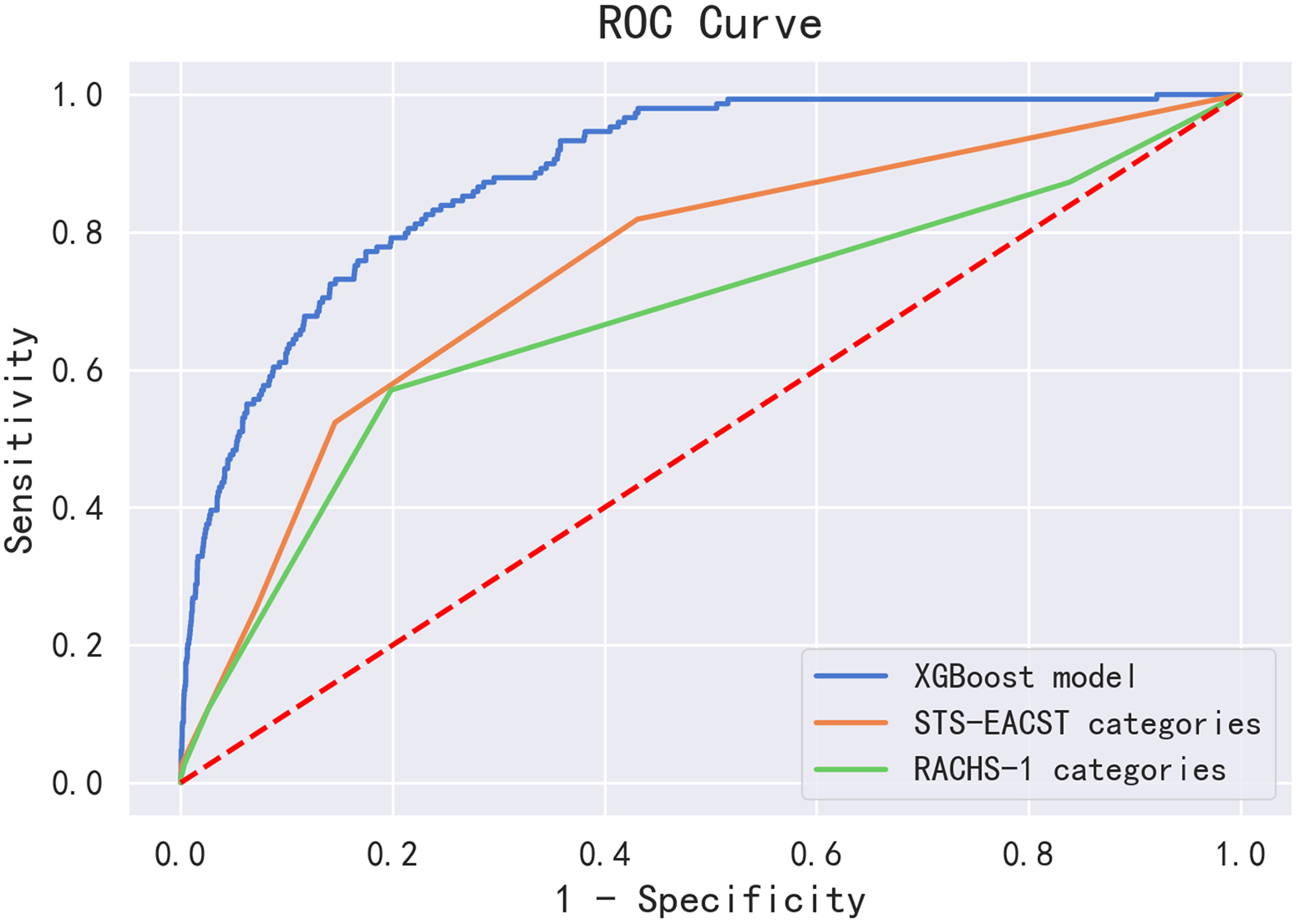
The performance of the XGBoost model, STS- EACTS, and RACHS-1 risk stratification categories in the testing set are shown in Table 3 and Fig. 2. The AUC of the STS-EACTS and RACHS-1 risk stratification categories was 0.748 (95% CI: 0.707–0.789) and 0.677 (95% CI: 0.627–0.728), respectively. Our XGBoost model yielded the best AUC (AUC = 0.887, 95% CI: 0.866–0.907), with a sensitivity and specificity of 0.785 and 0.824, respectively (Table 3).
| Model | AUC | AUC 95% CI | p-value | Sensitivity | Specificity |
| XGBoost model | 0.874 | (0.848, 0.901) | 0.751 | 0.879 | |
| STS-EACTS categories | 0.748 | (0.707, 0.789) | 0.819 | 0.569 | |
| RACHS-1 categories | 0.677 | (0.627, 0.728) | 0.570 | 0.801 |
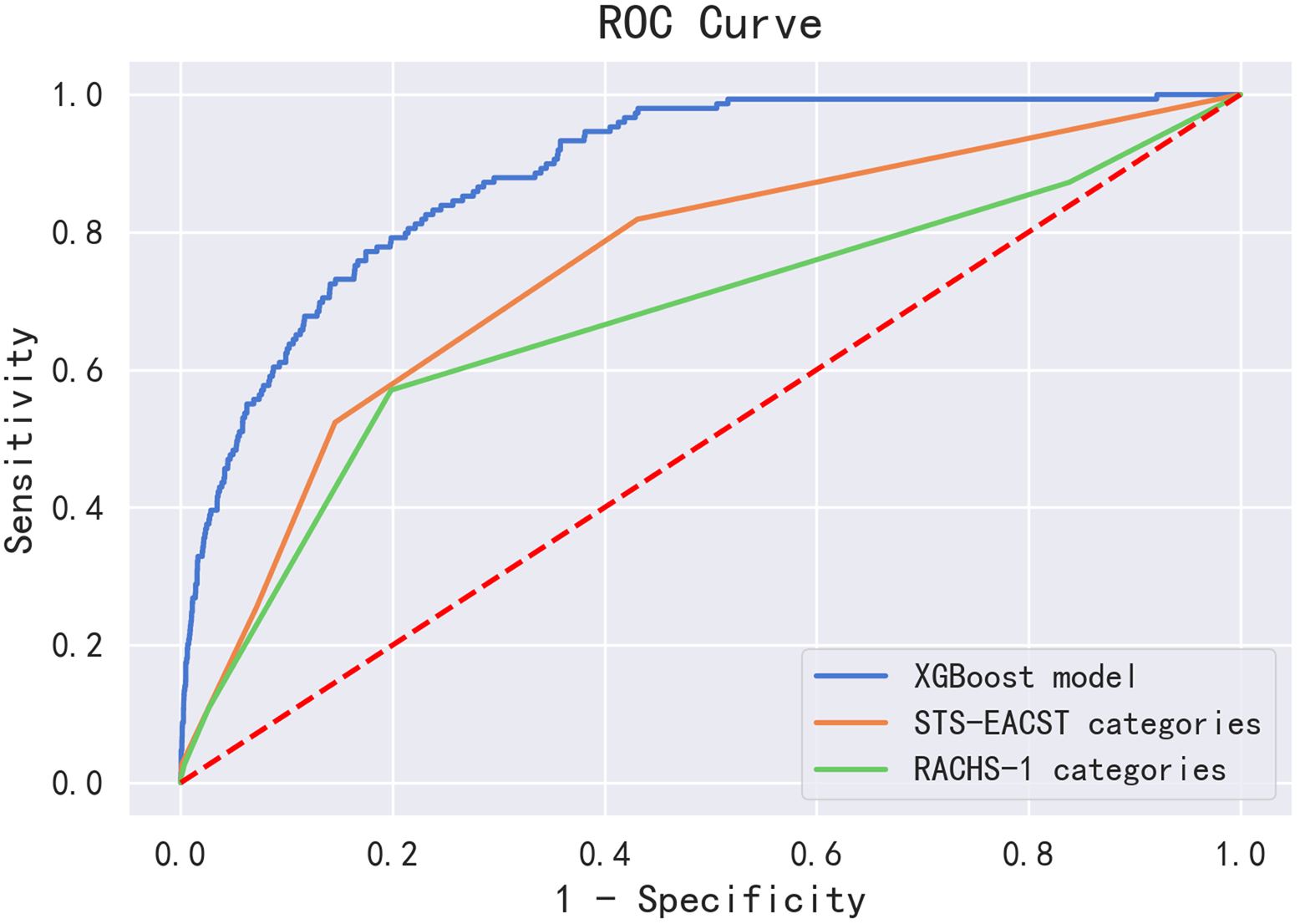 Fig. 2.
Fig. 2.Comparison of the prediction values of the XGBoost model, STS-EACTS categories, and RACHS-1 categories in the testing set.
The top 10 variables that contribute the most to the prediction power of the model are listed in Table 4. The higher the weight coefficient of a feature, the more significant role it plays in the model for outcome classification. The weight coefficient for saturation of pulse oxygen categories, risk categories, age, preoperative mechanical ventilation, atrial shunt, pulmonary insufficiency, ventricular shunt, left atrial dimension, a history of cardiac surgery, numbers of defect were 0.10638574, 0.07759346, 0.07303152, 0.07014898, 0.065226465, 0.05785214, 0.05760804, 0.052233107, 0.051096234, 0.0437589, respectively (Table 4). The excluded variables are listed in Supplementary Table 1.
| Feature | Weight coefficient |
| Saturation of pulse oxygen categories | 0.106386 |
| Risk categories | 0.077593 |
| Age | 0.073032 |
| Preoperative mechanical ventilation | 0.070149 |
| Atrial shunt | 0.065226 |
| Pulmonary insufficiency | 0.057852 |
| Ventricular shunt | 0.057608 |
| Left atrial dimension | 0.052233 |
| A history of cardiac surgery | 0.051096 |
| Number of defects | 0.043759 |
| Weight coefficient: Refer to the extent to which each indicator contributes to the model. | |
Prediction of in-hospital mortality risk is clinically important for directing patient postoperative management. In our study, we compared the XGBoost model with traditional tools for predicting mortality in pediatric CHD surgery. To our knowledge, this is the first study to compare machine learning algorithms with the RACHS-1 and STS-EACTS categories for the prediction of in-hospital mortality risk in pediatric CHD surgery. And we found that in children with CHD of China, the XGBoost model was more accurate in predicting in-hospital mortality for CHD surgery than in the RACHS-1 and STS-EACTS categories.
In our study, the in-hospital mortality rate after CHD surgery was 2.4%, which is consistent with that previously reported in China [5] and in western countries [25, 26, 27], but much lower than that reported in developing countries [28, 29]. Cardiac surgeons use traditional tools such as the RACHS-1 and STS-EACTS to report patient outcomes. The RACHS-1 categories were constructed based on a combination of the opinions of 11 experts and empirical data to predict in-hospital mortality [12, 30]. The RACHS-1 categories classifies procedures into six levels of risk of mortality based on a few clearly defined criteria. In previous studies, the risk of mortality from CHD surgery with different RACHS-1 stratification ranged from 0.26% to 62% [31, 32, 33], which is consistent with the findings of our study. An objective, empirically based tool named STS-EACTS, without the input of an expert panel, has been developed for analyzing in-hospital mortality associated with CHD surgery [14, 34]. However, the RACHS-1 and STS-EACTS categories only consider procedural characteristics and ignore individual patient characteristics. Both categories lack precision when estimating the risk for individual patients. In addition, some procedures (19%) in our cohort could not be classified using the RACHS-1 or STS-EACTS categories. Due to the enormous differences in patient-related variables and CHD surgery, it is difficult to establish a mortality risk prediction model.
Hence, one of the greatest challenges in medicine is how to deal with individuals who have the same disease but with different manifestations. Machine learning algorithms may provide a solution for this problem. Furthermore, previous study further demonstrated that machine-learning methods, especially gradient boosting models, are promising to outperform existing clinical risk scores [35]. Machine learning models have currently been explored as a tool to predict mortality, morbidity, and complications in patients with CHD [22, 36, 37]. A XGBoost model was constructed based on surgical risk stratification and patient preoperative variables in this study. According to previous studies, the AUC of the STS-EACTS and RACHS-1 categories to predict the mortality and complications of CHD surgery in children was 0.68–0.79 [14, 22, 28, 38, 39]. In our study, the AUC of the XGBoost model was 0.887, which was better than that of the STS-EACTS (AUC = 0.748) and RACHS-1 (AUC = 0.677) categories. The results showed that the XGBoost model was able to predict in-hospital mortality with improved predictive power compared to the STS-EACTS and RACHS-1 models.
In addition to surgical risk stratification, patient-related variables also had a significant impact on the performance of the postoperative mortality risk prediction model. The XGBoost model incorporates demographic characteristics, preoperative echocardiography characteristics, and laboratory examination results into the final predictive model. We analyzed the importance of these risk factors in the XGBoost model. Our results showed that saturation of pulse oxygen categories had the greatest impact on the predictive performance of the model. Previous studies have shown that oxygen saturation correlates with mortality in children undergoing CHD surgery [40, 41]. A decrease in oxygen saturation at 24 hours after the operation may increase the mortality rate of newborns with cyanotic cardiopathies [42].
For patients with CHD who have received cardiac intervention, preoperative mechanical ventilation and RACHS categories may affect their mortality during hospitalization [43]. Mechanical ventilation has been shown to be a strong predictor of in-hospital mortality in children with noncardiac surgery [44]. In addition, study has found that newborns with severe CHD may have increased mortality if they need unplanned cardiac reintervention, and according to the results of multifactorial analysis, mechanical ventilation before heart intervention and the larger RACHS-1 category are independent risk factors for unplanned cardiac re-intervention [45]. In this study, we also found that risk categories and preoperative mechanical ventilation are top influencing factors of the predictive performance in XGBoost model. This reminds clinicians to pay more attention to the prognosis of these patients whose surgery is at greater risk category or who require preoperative mechanical ventilation.
Age, as an important factor in the mortality rate of children with CHD, has also been mentioned in several studies. A study in Taiwan Province of China found that the majority (i.e., more than 90%) of CHD deaths occur within the first 5 years of life (mainly in infancy) [46]. The study showed that the mortality rate of CHD patients has a downward trend with the increase of age [47]. Our study also found that age is an influencing factor of in-hospital mortality in children with CHD and made a great contribution to the model. Clinicians should pay more attention to younger CHD patients in practice.
In addition to the above factors, the results of the machine learning model in
this study also show that atrium shunt and ventricular shunt may also be the
factor of in-hospital mortality. The reason may be that these factors affect the
occurrence of postoperative complications in patients. Low
cardiac output syndrome (LCOS) is a common life-threatening postoperative
complication of heart disease that may contributes to postoperative morbidity and
mortality [48, 49, 50, 51]. Atrial shunt and ventricular level shunt were all independent
risk predictors of LCOS [52]. Bangrong Song et al. [51] believed that
more attention should be paid to CHD patients age
In this study, we found that the number of defects influences in-hospital mortality in patients with CHD. The reason may be that if the patient carries multiple CHD at the same time, the prognosis is much worse than that of the patient with a single type of CHD. Presently, the most common types of CHDs include ventricular septal defect (VSD), patent ductus arteriosus (PDA), secundum atrial septal defect (ASDII), pulmonary stenosis (PS) and tetralogy of Fallot (TOF), and the incidence of each CHD is different [54]. Several studies have further divided the CHD population into simple and severe CHD groups [54, 55], and it is found that individuals with simple CHD (e.g., VSD or ASD) have higher survival rates, almost similar to normal populations [47]. However, the prognoses of patients with severe CHD varies widely [47].
Clinicians should focus on the top variables in the model to improve patient outcomes by dealing with variables that can be managed. For example, on the premise of ensuring the treatment effect, surgery with low-risk categories should be selected to improve the postoperative survival rate of patients. For the CHD patients with abnormalities in the above top indicators should be paid closer attention to their postoperative recovery status, which is the important significance of this study to propose this model.
This study has some limitations. First, this study is a single-center retrospective study. However, this is the first study to use a machine learning algorithm to predict mortality in pediatric CHD surgery in a large sample. In addition, our center is the most famous treatment center for children with congenital heart disease in China, with patients from most provinces in China. Second, the in-hospital mortality rates recorded in this study may not include all operation-related deaths, and need to include data from patients after discharge. This needs to be addressed in a more complete data source. Third, there was an imbalance in the number of patients who died and survivors in this study, and we did not perform a 1:N case-control match at the time of patient enrollment. During model building, we try to deal with the imbalance of samples in the training set, we tried to process the unbalanced classes and tuned the parameter ‘scale_pos_weight’, a parameter adjusting the balance of positive and negative weights in the XGBoost package. However, this did not improve the predictive performance of the model.
In conclusion, our single-center study of 24,685 patients demonstrated that using a combination of procedure complexity categories and preoperative patient-level factors, the XGBoost model had higher accuracy in in-hospital mortality prediction than both the RACHS-1 and STS–EACTS categories. In clinical practice, machine learning models can be established based on the surgical database for risk prediction to improve cardiac surgical care.
ZHL and XWD mainly participated in literature search, study design, writing and critical revision. HW, SMW, YH, JHZ, HBZ, ZDH, YWC and ZWX mainly participated in data collection, data analysis and data interpretation. All authors read and approved the final manuscript.
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Ethical Committee of Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiaotong University (approval number: SCMCIRB-W2020026).
We wish to thank all the staff of Shanghai Children’s Medical Center who have contributed to this study. We also thank Shanghai Synyi Medical Technology Co., Ltd. for providing a data analysis and statistical platform.
This research received no external funding.
Zedong Hao and Yiwei Chen are current employees of Shanghai Synyi Medical Technology Co., Ltd. The authors declare no conflict of interest.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.